Abstract
We studied schizophrenia liability in a Danish population-based sample of 44 twin pairs (13 MZ, 31 DZ, SS plus OS) in order to replicate previous twin study findings using contemporary diagnostic criteria, to examine genetic liability shared between schizophrenia and other disorders, and to explore whether variance in schizophrenia liability attributable to environmental factors may have decreased with successive cohorts exposed to improvements in public health. ICD-10 diagnoses were determined by clinical interview. Although the best-fitting, most parsimonious biometric model of schizophrenia liability specified variance attributable to additive genetic and non-shared environmental factors, this model did not differ significantly from a model that also included non-additive genetic factors, consistent with recent interview-based twin studies. Schizophrenia showed strong genetic links to other psychotic disorders but much less so for the broader category of psychiatric disorders in general. We also observed a marginally significant decline in schizophrenia variance attributable to environmental factors over successive Western European cohorts, consistent perhaps with improvements in diagnosis and in prenatal and perinatal care and with a secular decline in the prevalence of schizophrenia in that region.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Over the course of the twentieth century, twin, family, and adoption studies demonstrated substantial genetic influences on schizophrenia liability (Ritsner and Gottesman 2009, 2011) with a polygenic mode of inheritance and probabilistic, multifactorial threshold effects (Gottesman and Shields, 1967). Genetic factors generally have accounted for an estimated 81–85 % of the variance in liability to developing schizophrenia (Cardno and Gottesman 2000; Purcell et al. 2009, Sullivan et al. 2003) as an upper bound and, omitting twin studies, a lower bound of 64–67 % (Lichtenstein et al. 2009; Wray and Gottesman 2012). Molecular genetic studies have identified many common schizophrenia-related SNPs with odds ratios (OR) of 1.1–1.2 and some very rare structural variations with OR of ~2 to 20 for individuals but no single genes of major effect at the population level to date (Sullivan et al. 2012). Genome-wide complex trait analyses (GCTA) are beginning to account for the “missing heritability” in phenotypes (Yang et al. 2011). For example, simultaneous combination of common SNPs has accounted for about one-third of the genetic variance in schizophrenia (Lee et al. 2012). In addition, some very rare copy number variants confer greatly increased liability to schizophrenia at an individual level (Lee et al. 2012; Kirov 2010; Kirov et al. 2009; Lencz et al. 2013). Twin studies, our focus here, provide a benchmark estimate of heritability by which molecular genetic studies can estimate the magnitude of the contributions from either a particular polymorphism or a GCTA combination to the overall genetic variance in schizophrenia liability (VanDongen et al. 2013; Lee et al. 2012).
Twin studies also offer evidence of the degree to which schizophrenia and other psychotic disorders may be co-heritable (Lichtenstein et al. 2009; Cardno et al. 2012). A recent case report, in which bipolar disorder developed in the previously well, monozygotic twin of a proband with schizophrenia may illustrate this phenomenon (O’Reilly et al. 2013). Symptoms shared between schizophrenia and the psychotic manifestations of bipolar and depressive disorders may represent a general vulnerability to psychotic symptoms/cognitive slippage, evident in family pedigrees populated by both schizophrenia and bipolar disorder probands (Meehl 1972; Lenzenweger 2010). Exclusion criteria typically prohibit, a priori, the co-occurring diagnoses of psychotic bipolar affective and schizophrenia in research protocols. However, both affective and non-affective psychotic disorders co-exist in some individuals over time, prompting the logical diagnosis of schizoaffective disorder. Current taxonomic initiatives like the Research Domain Criteria (RDoC; Cuthbert and Insel 2013; Insel et al. 2010; NIH 2014) may further clarify the associations among the various psychotic disorders through their examinations of psychiatric symptom domains and of endophenotypic vulnerability markers shared across diagnostic groups (Gottesman and Gould 2003; Gottesman and McGue 2014; Insel and Cuthbert 2009; Glahn et al. 2014). Evidence of molecular relationships between schizophrenia and other psychotic disorders are already emerging, as GWAS identified SNPs associated with schizophrenia also have been associated with liability to schizoaffective, bipolar, and psychotic depressive disorders (Geschwind and Flint 2015; Lencz et al. 2013; Lee et al. 2012).
Even as technology improves our capacity to examine molecular mechanisms for schizophrenia in the pathways between genotypes and phenotypes, the environmental contributions to the disorder also may be changing. Although meta-analyses of twin studies of schizophrenia typically assume cross-cohort stability in variance attributable to genetic and environmental factors in order to obtain meta-estimates for these sources of liability (Sullivan et al. 2003), it still may be wise to test this assumption periodically. The historical and epidemiological evidence that famine (Susser et al. 1996), obstetrical complications (Geddes et al. 1999), and other adverse environmental factors may increase secular rates of schizophrenia (Murray et al. 2003; Matheson et al. 2011) also suggests that changes in these conditions may change both the incidence of schizophrenia and also the relative influences of environmental and genetic factors on population risk for schizophrenia. Sufficient food supplies, better diet, and improved public health and obstetrical health care corresponded with a decline in Denmark’s perinatal mortality rates from 12 % in 1900 to 2.5 % in 1953 (Copenhagen Statistical Department 1967), with further declines evident through the 1980s and early 1990s (Vallgarda 1995). Insofar as these perinatal risk factors also contribute to schizophrenia risk, one would expect a decline both in schizophrenia incidence and in the proportion of schizophrenia risk attributable to environmental factors. Indeed, evidence suggests that the incidence of schizophrenia has declined with successive cohorts both in Denmark (Munk-Jorgensen 1986; Munk-Jorgensen and Jorgensen 1986) and, more broadly, in the West (Warner 1995). Any corresponding temporal changes in the relative contributions of environmental factors to overall schizophrenia liability may be tested, in part, through pan-generational comparisons of twin study data.
We estimated the heritability of ICD-10 schizophrenia and its co-heritability with other disorders, based on probands’ schizophrenia concordance with their co-twins’ diagnoses, respectively, of schizophrenia, of schizophrenia-related or other psychotic disorder, and of any psychiatric disorder. We also examined the current twin data in light of earlier Western European twin studies to explore a possible secular decline in environmental influences on schizophrenia liability across historical cohorts.
Methods
Sample and diagnoses
The data for this Twin Study, approved by the Danish National Scientific Ethics Committee, were collected in 1992–1995 for the first author’s PhD dissertation (Kläning 1996), based on The Young Cohort of The Danish Twin Register (Kyvik et al. 1996) and The Danish Psychiatric Central Register (Munk-Jorgensen and Mortensen 1997). The Young Cohort of The Danish Twin Register was established in 1991 by Kyvik et al. (1996; cf., Hauge et al. 1968) and consists of a total of 42,182 individuals from twin and triplet sets born 1953–1982 in Denmark, including individuals from broken sets (in which one member has died). The identification of the twins was performed by means of the Danish Civil Registration System (Pedersen et al. 2006) and was independent of their health status. The Danish Psychiatric Central Register (Munk-Jorgensen and Mortensen, 1997; Mors et al. 2011) includes computerized information about all admissions after April 1, 1969 to every hospital in Denmark providing psychiatric in-patient treatment and was used to identify all twin register members who were ever psychiatric in-patients in Denmark, using the citizen’s identity registration number, which ensures reliable identification. Early psychiatric register diagnoses were based on the ICD-8 (World Health Organization (WHO) 1967, 1974) and, beginning on January 1, 1994, on the ICD-10 (WHO 1992, 1993).
The first author performed a nationwide record-linkage to select a sample for the ascertainment of ICD-10 schizophrenia probands. She examined the medical records of twins who received a discharge diagnosis of functional psychosis (ICD-8: 295–299, ICD-10: F2 and F3) or schizoid, paranoid, and ‘other’ personality disorder (ICD-8: 301.0–.2 and .8 (with Danish sub-specifications), ICD-10: F 60.0 and F60.2) to select twins with schizophrenia symptoms for clinical interviews. Twin pairs in which one or both twins had a discharge diagnosis of schizophrenia or records describing non-affective psychotic symptoms for 1 week or more were selected, provided that both twins were alive and living in Denmark (excluding 4 counties to adjust to the scope of the available resources). After giving informed consent, those pairs available for examination were interviewed in Danish with the semi-structured Schedules for Clinical Assessment in Neuropsychiatry (SCAN; Wing et al. 1990). Ten genetic markers from blood samples were used to determine the zygosity of same-sex twins in this interview sample. If either twin did not agree to give a blood sample, zygosity was inferred from a mailed questionnaire, previously validated against serological zygosity determination (Kyvik et al. 1995). In 108 pairs, at least one twin had a chart diagnosis consistent with selection criteria. In 74 pairs, twins meeting these criteria consented to a clinical interview for proband ascertainment. This rate of interview, although nominally lower than historically high levels of participation in the mid-twentieth century, remains somewhat higher than is typical of recent Danish register cohorts, estimated at about 60 % by the turn of the current century (Bertelsen 2004). The 34 pairs who declined interviews showed no substantial differences from the 74 interviewed pairs in gender, mean age at first admission, or mean time between first admission and interview, suggesting that participants were reasonably representative of the population. Among the 74 participant pairs, the twins in 22 pairs ultimately did not fulfill diagnostic criteria for schizophrenia, and 8 pairs were discarded because of missing cotwin information, leaving 44 twin pairs with at least one twin meeting the diagnostic criteria for research with ICD-10 schizophrenia for the ascertainment of the probands, the ascertainment being of the incomplete ascertainment type.
All the probands and 4 cotwins were interviewed with SCAN by the first author, and the non-proband co-twins who had agreed to a personal examination were interviewed with SCAN and the Personality disorder examination (PDE; Loranger, 1988) by another psychiatrist (CS) blind to zygosity. For the cotwins who agreed to participate but did not want a personal interview, a case summary was prepared solely on the basis of medical records and information from the interviewed proband and/or the twin pair’s mother. Summaries of the interviews and case records were conferenced with and confirmed by our senior psychiatrist (AB), blind to zygosity. All ICD-10 diagnosed probands also met threshold criteria for DSM-IV diagnoses of schizophrenia.
Data analysis
Concordance for ICD-10 schizophrenia F20.x was termed C1. Cotwin concordance for schizophrenia-related and other psychotic disorders was termed C2, and included F21–29 (schizotypal, delusional, brief psychotic, shared psychotic, schizoaffective, or other psychotic disorder, or unspecified psychosis not due to a substance or known physiological condition), F30.2 (manic episode, severe with psychotic symptoms), F31.2and .5 [bipolar disorder, severe with psychotic features, current episode specified as manic (F31.2) and depressed (F31.5)], F32.3 and F33.3 (major depressive disorder severe with psychotic features, single episode or recurrent, respectively). In order to consider an even broader concordance for psychopathology, cotwin concordance for any other psychiatric disorder was termed C3. (Raw concordance data appear in Supplementary Appendix A.) We computed probandwise concordance rates for these three levels of concordance–proband C1 with cotwin C1, with cotwin C1 or C2, and with cotwin C1 or C2 or C3. Probandwise concordance rates, with pairs based on each independently ascertained proband, typically produce higher and more consistent heritability estimates with incomplete ascertainment than do pairwise rates, which ignore ascertainment (McGue 1992).
Using Mx software (Neale 2004), we estimated tetrachoric correlations based on pairwise similarity in schizophrenia liability by zygosity, imputing the number of unaffected pairs based on schizophrenia prevalence rates. We then fitted biometric models to our original contingency tables of probandwise concordance frequencies using incomplete ascertainment models (Neale 2004, p 70). Our models assumed that the liabilities to the three concordance phenotypes (C1 schizophrenia, C2 schizophrenia and schizophrenia-related or other psychotic disorders, and C3 any psychiatric disorder) are normally distributed, and that only those individuals whose liability exceeds a specified threshold manifest the disorder (Rijsdijk and Sham, 2002). Thresholds for schizophrenia liability (C1) were based on an estimated population risk of 1 % for schizophrenia diagnosis; for psychotic disorder liability (C1 or C2 diagnoses), based on an estimated population risk of 2 % for any psychotic disorder in the cotwin; and for “any psychiatric disorder” (C1 or C2 or C3 diagnoses) in the cotwin, based on an estimated population risk of 22 % (from Pedersen et al. 2014 Danish incidence and risk study), all assuming incomplete ascertainment. Minor changes in the population risk threshold produced negligible changes in model-fitting results.
Our biometric models estimated the contributions of additive (A) and non-additive (D) genetic and of common/shared (C) and unique/nonshared (E) environmental factors to variance in schizophrenia liability, psychosis liability, and schizophrenia/affective disorder liability, limited by degrees of freedom to no more than three parameters at a time (ACE or ADE model). Given the theoretical problems associated with a DE model that assumes non-additive apart from additive genetic factors, we also compared the relative fit of ADE and AE models to test the significance of non-additive genetic variance. Our limited sample size provided insufficient statistical power for testing more complex models, such as a sex-effects, multiple thresholds, or gene by environment interaction models. Models’ goodness-of-fit to the data were determined using the root mean square error of approximation (RMSEA) and the Akaike Information Criterion (AIC; Akaike, 1987), which balances goodness-of-fit and parsimony of the model by subtracting twice the model’s degrees of freedom from its χ 2 value: AIC = χ2−2df.
We computed MZ/DZ concordance ratios for the three primary levels of concordance (proband C1 with cotwin C1, with cotwin C1 or C2, and with cotwin C1 or C2 or C3), reflecting evidence of long-observed diminishing continuity among these diagnoses (Farmer et al. 1987). We also computed concordance rates of proband schizophrenia with two more discrete cotwin phenotypes, that is, cotwin diagnoses of C2 only and of C3 only. For these latter two sets of analyses, we first removed pairs meeting more stringent concordance from consideration: we excluded pairs strictly concordant for schizophrenia to examine the concordance of proband schizophrenia (C1) with cotwin non-schizophrenia psychosis (C2 only) and excluded pairs concordant for strict schizophrenia or for any cotwin psychosis to examine the concordance of proband schizophrenia (C1) with any non-psychotic disorder in the cotwin (C3 only). We then computed MZ/DZ concordance ratios and tetrachoric correlations for these two additional concordance types.
We compared our study’s results for strict schizophrenia concordance with those of other twin studies of schizophrenia that also were based on epidemiological sampling and clinical interviews, including Fischer’s (1973) Danish Twin Study, as well as studies by Kringlen (1967, Norway), Tienari (1975, Finland), Gottesman and Shields (1972, UK), Cardno et al. (1999, UK), Onstad et al. (1991, Norway), Cannon et al. (1998, Finland), and Franzek and Beckmann (1998, Germany), focusing on concordance rates for a strict schizophrenia diagnosis. Specifically, we fitted biometric models for schizophrenia based on probandwise frequencies reported in the studies, comparing ACE, ADE, and AE models to find the biometric model of best fit to each sample’s data.
We recorded the mid-range birth year for each sample. When birth years were not indicated directly (Franzek and Beckmann, 1998), we imputed an estimated range of birth years from participants’ ages at the time of the study. Where initial raw data were available (the current sample, Fischer 1973; Gottesman and Shields, 1972), we computed the median birth year directly from case-level information and, for other studies, used the middle year of the cohort range as a best estimate of median birth year. We then fitted a regression equation to predict, from mid-range year of birth, the proportion of variance in schizophrenia liability attributable to environmental factors. Cardno et al.’s (1999) study used more than one diagnostic system, so we selected the ICD-10 diagnoses to represent this sample. This diagnostic system most closely resembles those used in the current and other comparison studies and, in Cardno’s sample, produced the least extreme parameter estimates.
We also conducted a more rigorous test of invariance of genetic and environmental contributions to schizophrenia liability over time by comparing ACE, ADE, and AE models that constrained parameters to be equal across all cohorts to the same models in which parameters for two early-cohort, low-heritability outlier samples (Fischer 1973; Tienari 1975), were set equal to each other and free to vary from the other samples, still constrained as a group to produce equal parameter estimates.
Results
Supplementary Appendix A contains pairwise data for individual proband status, zygosity determination, sex, year of birth, age at onset, age at first admission, and at last observation, as well as ICD-10 and DSM-IV diagnostic codes for each twin for ease of others’ future data mining. Among the 44 twin pairs included for concordance evaluation were 47 individual probands, 22 males and 25 females, 16 from MZ, 15 from same-sex DZ (SS-DZ), and 16 from opposite-sex DZ (OS-DZ) pairs. The mean age of probands was 33.2 at interview, with a range of 20–42 years (MZ, 31.1, 20–38 years; combined SS- and OS-DZ, 34.3, 23–42 years), and the mean number of years from onset of illness until interview was 12.7 with a range of 1–24 years (MZ 10.7, range 1–20; combined DZ 13.8, range 3–24). There was no substantial age difference between MZ and DZ twins, and with no evidence of temporal bias, the analyses were conducted without age-correction, which also allowed comparison with other twin studies of schizophrenia. For concordant pairs, the onset of illness in the cotwin followed within 1–4 years of the proband in MZ pairs and within 6 years in the one concordant DZ pair.
With increasingly broad definitions of the affected phenotype, concordance rates and tetrachoric correlations increased accordingly. The “narrow” (C1) probandwise concordance rate for schizophrenia was 44 % (se p = .12) in the 13 MZ pairs, which included 16 independently-ascertained probands with 9 discordant and 7 concordant cotwins (6 proband cotwins plus one concordant cotwin not ascertained independently). C1 concordance for the 31 DZ pairs was 3 % (se p = .03), with 31 probands, only one of whom had a concordant cotwin. None of the 15 SS-DZ pairs (0 %) and only one and of the 16 OS-DZ pairs (6 %, se p = .06) was concordant. For this narrowly defined schizophrenia phenotype (C1 only), tetrachoric correlations based on pairwise concordance were .74 (.45, .92) for 4/13 MZ and .19 (−.20, .51) for 1/31 DZ concordant pairs.
For a proband twin’s schizophrenia (C1) and a cotwin’s more broadly defined psychotic disorder (C1 or C2 diagnosis), the probandwise concordance was 50 % (se p = .13) in MZ pairs (16 probands with 8 discordant and 8 concordant cotwins) and 16 % (se p = .05) in DZ pairs (31 probands with 26 discordant and 5 concordant cotwins). Within DZs, concordance was 20 % (se p = .07) in SS pairs (15 probands with 12 discordant and 3 concordant cotwins) and 13 % (se p = .08) in OS pairs (16 probands with 14 discordant and 2 concordant cotwins). The one MZ cotwin diagnosed with non-schizophrenia psychosis received a diagnosis of bipolar disorder, single manic episode, and the four DZs, with major depressive disorder. Tetrachoric correlations for proband schizophrenia (C1) with cotwin schizophrenia or other psychotic disorder (C1 or C2) were .77 (.48, .93) for 5/13 MZ and .49 (.22, .70) for 5/31 DZ concordant pairs.
For proband schizophrenia and cotwin concordant for any psychiatric disorder (C1, C2, or C3), probandwise concordance was 75 % (se p = .11) for MZ (16 independently ascertained schizophrenia probands with 4 additional concordant cotwins, for a total of 4 discordant and 12 concordant cotwins) and 58 % (se p = .09) for DZ pairs, with 53 % (se p = .13) for SSDZ (15 probands, 7 discordant and 8 concordant cotwins) and 62.5 % (se p = .12) for OSDZ (16 probands, 6 discordant and 10 concordant cotwins). The majority of the C3 concordant cotwins were diagnosed with nonpsychotic affective disorders (3 of 4 MZs, 6 of 7 SSDZs, and 3 of 8 OSDZs), mainly with moderate depression. For concordance of proband C1 with cotwin C1, C2, or C3, tetrachoric correlations were .84 (.44, .98) for 9/13 MZ and .70 (.41, .89) for 18/31 DZ concordant pairs.
For proband schizophrenia with the more discrete phenotypes of non-schizophrenia psychosis only and of non-psychotic disorder only in cotwins, concordance rates reflected the removal of more highly concordant pairs. After removal of pairs already concordant for schizophrenia (C1), concordance rates of proband schizophrenia with cotwin’s non-schizophrenia psychosis (C2 only) were .11 for MZ (1/9) and .13 for DZ (4/30) pairs, with tetrachoric correlations of .38 (−.16, .79) for MZ and .43 (.15, .67) for DZ pairs. After additional removal of these non-schizophrenia psychosis concordant pairs, concordance rates of proband schizophrenia with cotwin’s non-psychotic disorder (C3 only) were .50 for both MZ and DZ twins (4/8 and 13/26, respectively), with tetrachoric correlations of .58 (−.07, .94) for MZ and .58 (.22, .83) for DZ pairs.
MZ/DZ probandwise concordance ratios declined with increasingly broad cotwin phenotypes for the three diagnostic groups considered in combination. Concordance ratios for cotwin C1, cotwin C1 or C2, and cotwin C1, C2, or C3 produced ratios of 13.56 (MZ = 7/16; DZ = 1/31), 3.1 (MZ = 8/16; DZ = 5/31), and 1.29 (MZ = 12/16; DZ = 18/31), respectively. The MZ/DZ concordance ratios further declined with the removal of more highly concordant pairs. Concordance for proband schizophrenia (C1) with cotwin non-schizophrenia psychosis only (C2 only) produced an MZ/DZ ratio of only .83 (MZ .11 (1/9) and DZ .13 (4/30) concordance). For proband schizophrenia (C1) with cotwin non-psychotic disorder (C3 only), the MZ/DZ concordance ratio was 1.0 (MZ .50 (4/8) and DZ .50 (13/26). The severely restricted range of cotwin similarity created by the exclusion of more fully concordant pairs accounts for these small ratios.
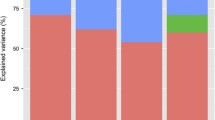
Details of biometric model-fitting can be found in Supplementary Appendix B. Although, theoretically, a perfect fit of three-parameter ACE and ADE models is expected, the less than perfect model fit for some of these models was likely a result of the parameter estimates converging with the boundary value of zero. Table 1 presents parameter estimates from the best-fitting biometric models applied to contingency tables of probandwise concordance for schizophrenia only (C1), for proband schizophrenia (C1) with any psychotic disorder in the cotwin (C1 or C2), and for proband schizophrenia (C1) with any psychiatric disorder in the cotwin (C1 or C2 or C3). As model parameters are eliminated from models for parsimony’s sake, the remaining parameter estimates may be biased, so where parameters have been dropped, we also include the full model (ACE or ADE) with the lower χ 2.
The best-fitting, most parsimonious biometric model for schizophrenia in the full sample was an AE model, in which additive genetic plus unique environmental factors accounted for population variance in schizophrenia. With the same χ 2 as the ACE model, the AE model shows no decrement in fit due to dropping the common environmental variance factor. The situation was somewhat different for the ADE model, over which the AE model showed a non-significant increase in χ 2. Although ADE was not the most parsimonious model, its relatively lower χ 2 suggests potential, non-zero contributions of non-additive genetic variance. The zero frequency of SS DZ concordant pairs for strict schizophrenia led us to add a (hypothetical) concordant pair to fit models, and the AE model, of additive genetic plus unique environmental factors, showed the best, most parsimonious fit for strict schizophrenia diagnosis in SS pairs. For the broader (C1 + C2) phenotype of schizophrenia or other non-schizophrenia psychosis and for the broadest (C1 + C2 + C3) phenotype, “any psychiatric disorder,” the AE model also showed the most parsimonious, best fit to both the full sample and SS subsample. Of course, sample size limited our statistical power, and none of the AE models showed a significant χ 2 difference from the ACE and ADE models in which they were nested.
Table 2 summarizes the cohorts’ range of birth years and probandwise concordance rates for a sample of current and past twin studies of schizophrenia diagnosed through clinical interviews, with diagnostic systems noted. Table 3 shows the midrange birth year for each sample, the results of the best-fitting biometric model based on probandwise frequency data, and the estimate of broad heritability (phenotypic variance attributable to all genetic factors, additive and non-additive combined), with most estimates in the low to mid .80s and some in the .90s. Across all samples, estimates of variance attributable to environments shared within-pair ranged from zero to .41, and to nonshared environments, from .01 to .31. Within-country, we see increasing heritability and a decreasing proportion of phenotypic variance attributable to environmental factors across the Danish and Finnish samples (with 56.5 and 24 years’ difference in mid-birth years—a half to a quarter century) and no significant changes across the Norwegian or UK cohorts (with 32 and 4 years’ difference, respectively), except that ADE models showed a relatively better χ 2 fit to the later cohort data for both countries. Across all samples, a linear regression that used mid-range birth year to predict the proportion of non-genetic variance in schizophrenia (c2 + e2) yielded a slope of b = −.47and β = −.47 (standardized), r = −.47, r 2 = .22 (p = .09). Because of the limited number of historic twin studies using population-based samples with interview-based diagnoses, this moderate decline with later cohorts in the proportion of schizophrenia variance attributable to non-genetic factors misses standard statistical significance. Nevertheless, median year of birth accounts for over one-fifth of the (unmeasured) environmental variance in schizophrenia liability. These data seem consistent with an historical pattern of increasing heritability of schizophrenia liability.
When we fitted the samples in one large analysis, constraining parameters to be equal across all samples, the χ2 goodness-of-fit measures for the combined model were 28.21 (16 df, ACE), 28.22 (16df, ADE), and 28.22 (17df, AE), respectively. When we freed parameters in the two early-cohort, low-heritability outlier samples (Fischer 1973; Tienari 1975), to be equal to each other and free to vary from the other samples’ still equality-constrained parameter estimates, the χ2 goodness-of-fit improved: 20.71 (13 df, ACE), 26.08 (13df, ADE), 26.08 (15df, AE). However, in light of the difference in degrees of freedom, these χ2 differences between the more and the less constrained models failed to reach statistical significance.
Discussion
Statistical power was limited by sample size and by the small number, historically, of population-based twin studies of schizophrenia that used clinical interview methods for diagnosis. Given the relative rarity of twins diagnosed with schizophrenia (about .02 % of the population, as approximately 2 % of people are twins and roughly 1 % of people have schizophrenia diagnoses), univariate twin studies of schizophrenia are often under-powered for complex analyses, but nevertheless generate useful information across multiple populations and historical cohorts for testing data-based hypotheses. Our reliance on population-based samples in which schizophrenia was diagnosed through clinical interview helped to ensure both optimal representativeness and reliable diagnosis.
For this study’s first objective, to replicate previous twin study findings using contemporary diagnostic criteria (WHO 1993), the data showed both continuity with and change from much of the earlier literature. The current study replicated the high MZ: DZ ratio of schizophrenia concordance observed across decades of twin research. Additionally, the difference between MZ/DZ concordance ratios for strict schizophrenia diagnosis (13.6) and for probands’ strict schizophrenia diagnoses with the cotwins’ broader diagnoses of either schizophrenia or other psychotic disorders (3.1) lends support to the discriminant validity of the ICD-10 schizophrenia diagnosis (See Farmer et al. 1987). Left-censored twins already deceased and right-censored, late-onset cases emerging post-study represent unmeasured censoring and potential under-estimates of schizophrenia incidence, but the current study’s biometric models remain consistent with those of other samples.
In light of our second objective, to examine genetic liability shared between schizophrenia and other disorders,—we observed a much stronger genetic association of schizophrenia with psychotic than with non-psychotic disorders when these disorders were considered as part of a continuum of phenotypic similarity to schizophrenia. Consistent with GWAS discoveries of partially shared genetic liability to bipolar disorder and schizophrenia (Lee et al. 2013; Cardno and Owen, 2014), the heritability of “narrow” (C1) schizophrenia was virtually indistinguishable from the broadened phenotype that included other psychotic disorders (all affective psychotic disorders in our study). The stronger genetic association of schizophrenia with psychotic than with non-psychotic (mainly affective) disorders seems consistent with the centrality of “psychosis-proneness” to the shared genetic etiology between schizophrenia and other psychotic disorders (Gottesman et al. 2010). Such evidence of shared vulnerabilities across disorders has led researchers recently to re-envision psychiatric constructs less exclusively in terms of diagnostic category and more broadly in the context of dynamical systems, whether as mechanistic property clusters (Kendler et al. 2011), network constructs (Schmittmann et al. 2013), or the psychopathology domains posited by Insel in the National Institutes of Health for Research Domain Criteria (RDoC; Cuthbert and Insel, 2013; Insel et al. 2010; NIH, 2014). Of course, recent evidence that symptom covariation in a large sample produced separate higher-order dimensions for affective and non-affective psychosis maintains some differentiation between schizophrenia and other psychotic disorders (Russo et al. 2014). We observed a similar differentiation in the lower MZ/DZ concordance ratios produced for probands’ schizophrenia with non-schizophrenia disorders in cotwins, after excluding from our analyses pairs already concordant for schizophrenia.
The third objective of the study, to explore, in a preliminary way, whether the last century’s changes in the frequency or magnitude of environmental risk factors for schizophrenia have also decreased the relative importance of environmental relative to genetic factors in schizophrenia liability (indexed by increasing heritability), yielded ambiguous results. Of course, statistical variability and variation in sample size, circumstances, and diagnostic guidelines or criteria may contribute to fluctuating heritability estimates across studies. Censoring also presents potential limitations for cross-cohort examinations; it is unknowable whether the very high mortality rates for twin births in the late 1800s and early 1900s were randomly or non-randomly associated with schizophrenia liability. In biometric modeling, epigenetic effects may be confounded statistically with either genetic or environmental effects, depending on whether the epigenetics were stable from fertilization, changed similarly with shared environments, or diverged with the effects of unique environmental factors (Petronis 2010). Finally, when twin studies produce higher estimates of heritability (lower environmental variance) than non-twin family studies do, it may indicate either epigenetic or non-additive genetic inheritance, or both.
Our estimates across interviewed, population-based Western European twin samples showed marginal evidence of a cohort-related increase in heritability of schizophrenia liability and a corresponding decline overall in the degree to which its variance could be attributed to environmental factors. Within-country, variance in schizophrenia liability attributable to environmental factors either declined or remained stable (no significant increase). Participant overlap accounts for some of the observed stability, as Cardno’s (2000) UK sample built on that of Gottesman and Shields’ (1972) study, with only a four-year difference in the overall median year of birth.
By restricting our analysis to population-based samples subjected to clinical interviews, our study reveals somewhat stronger evidence for declining environmental variance in schizophrenia than was seen in earlier studies (see Sullivan et al., 2012 for a review). When diagnosis becomes more exacting and strong environmental risks for schizophrenia diminish (as with a secular decline in prenatal and perinatal complications), population variance attributable to environmental factors may be expected to decrease proportionally.
The attenuation, over time, of environmental variance in schizophrenia liability may yield new patterns of twin similarity with later cohorts. An earlier Danish study (Fischer 1973) showed patterns of within-pair phenotypic similarity such that MZ correlations were no more than twice the size of DZ correlations, so ACE models typically best fit the data. Limited to three degrees of freedom, ACE models do not include an estimate of non-additive genetic variance. In the presence of epistatic or dominance effects, however, where MZ twins typically show more than twice the phenotypic similarity of DZ twins, the ADE model, with the capacity to estimate the relative proportions of both additive and non-additive genetic variance, yields a better fit. This ADE model seemed to fit Cardno’s (1999) data, and yet, Cardno et al. (1999) correctly interpreted such evidence conservatively, as potentially attributable to low DZ concordance rates, and by adding one (hypothetical) concordant DZ pair to the analyses of DSM-III diagnoses, found evidence more consistent with an AE model. However, a low rate of DZ concordance can be expected under conditions of epistasis, so the possibility of non-additive genetic variance cannot be ruled out. Alternatively, an AE model may best fit the data in the absence of variance due to shared environments. Despite the large MZ/DZ ratio in probandwise concordance, for example, Franzek and Beckmann’s (1998) data for strict schizophrenia diagnosis fit the AE better than it did the ADE model. Our sample, with limited statistical power and similar to Onstad et al.’s (1991) sample, could not fully resolve the question of non-additive genetic variance. Evidence of non-additive genetic effects on schizophrenia has been observed at an endophenotypic level, accounting for significant variance in ocular motor functioning (Clementz et al., 1992) and at a molecular level, with specific epistatic effects of polymorphisms of the dopamine transporter (DAT) and catecholomethyltransferase (COMT) genes on cortical function in schizophrenia during executive processing (Prata et al. 2009).
The current Danish twin sample, like other recent samples, showed no evidence of shared environmental effects on ICD-10 schizophrenia, except when we limited our analysis to same-sex twins and added a hypothetical concordant DZ pair. Historically, though, other twin samples with somewhat lower MZ: DZ concordance ratios indicated some variance attributable to shared environments (Fischer 1973; Sullivan et al. 2012). These differences could be due to chance, less precision in some older diagnostic systems, and other sources of variation.
Gottesman and Shields’ (1972) high estimates of schizophrenia heritability seem anomalous when compared with other studies of its era, more similar to current studies. This difference may stem, in part, from the rigor of the study’s diagnostic methods, with higher priority given to diagnoses arrived at through the consensus review of six judges. This high standard of reliable inter-rater diagnosis may have overcome some of the diagnostic unreliability that, historically, prompted the eventual widespread adoption of criterion-based diagnosis. Measurement unreliability, however, is theoretically uncorrelated within twin pairs, and would most likely affect the estimate of non-shared, rather than shared, environmental variance.
Evidence of shared environmental variance typically emerged from studies of earlier cohorts, when certain environmental risks were more common, whereas studies of more recent cohorts found no evidence of shared environmental variance and produced higher heritability estimates for schizophrenia liability. This temporal effect of increasing heritability with improved health care seems analogous to the socioeconomic status effect Turkheimer et al. observed for heritability of children’s IQ (Turkheimer et al. 2003). In impoverished families, where environmental risks were more common, individual differences in children’s IQ were attributable to environmental factors alone. In more affluent families, buffered from those environmental risks, children’s IQ was more prototypically heritable. Limited access to individual-level data across the full range of samples limited the scope of this portion of our investigation, as the decades-wide definition of some sample cohorts potentially obscured any covariation between birth year and heritability estimates.
A decline across more than a century in the proportion of schizophrenia liability attributable to environmental factors would be consistent with improvements in public health. Of course, the number of twin studies of schizophrenia is relatively small, with the regression and more rigorous model-fitting falling short of nominal statistical significance. If no cohort-related decrease in the variance in schizophrenia liability associated with environmental factors has occurred, then either public health improvements did not appreciably affect environmental contributions to schizophrenia liability at the population level, or their positive effects may have been counterbalanced by the survival of more environmentally “at risk” individuals to the age of schizophrenia onset and/or by the introduction of new environmental risks for schizophrenia, such as increasing exposure to drugs associated with psychosis risk (McGrath et al. 2010) or secular increases in paternal age (Matheson et al. 2011; D’Onofrio et al. 2014). Alternatively, the observed correlation, albeit under-powered, could represent an actual decline in environmental influences on schizophrenia liability with successive cohorts. If this is the case, then improved public health may have made a difference. As previously noted, improved diagnostics reduce measurement error (one source of nonshared environmental variance), which decreases non-shared environmental variance and, proportionally, increases variance attributable to other factors. However, more accurate diagnosis would not explain the reduction in schizophrenia liability attributable to environments shared within-pair. Any reduction in measurement error and in actual environmental variability may increase the capacity of some twin studies to detect evidence of both additive and non-additive genetic influences on schizophrenia. These estimates of genetic variance, in turn, may provide a reference point from which to appraise how much any particular additive or non-additive genetic (or similarly-acting epigenetic) effect identified in molecular genetic studies may contribute to the overall genetic liability to schizophrenia (Van Dongen et al. 2012).
References
Akaike H (1987) Factor analysis and AIC. Psychometrika 52:317–332
Bertelsen A (2004) Contributions of Danish registers to understanding psychopathology: Thirty years of collaboration with Irving I. Gottesman. In: Dilalla LF (ed) Behavior Genetics Principles: Perspectives in Development, Personality, and Psychoapthology. American Psychological Association, Washington, DC
Cannon TD, Kaprio J, Lönnqvist J, Huttunen M, Koskenvuo M (1998) The genetic epidemiology of schizophrenia in a Finnish twin cohort. A population -based mode1ing study. Arch Gen Psychiatry 55:67–74
Cardno AG (2000) The quantitative genetics of clinical variation in psychotic illnesses. Unpub. Ph.D. Dissertation, University of Wales College of Medicine, Cardiff, Wales
Cardno AG, Gottesman II (2000) Twin studies of schizophrenia: From bow-and-arrow concordances to star wars Mx and functional genomics. Am J Medical Genet 97:12–17
Cardno AG, Owen MJ (2014) Genetic relationships between schizophrenia, bipolar disorder, and schizoaffective disorder. Schizophr Bull 40:504–515
Cardno AG, Marshall EJ, Coid B, Macdonald AM, Ribchester TR, Davies NJ, Venturi P, Jones LA, Lewis SW, Sham PC, Gottesman II, Farmer AE, McGuffin P, Reveley AM, Murray RM (1999) Heritability estimates for psychotic disorders: the Maudsley twin psychosis series. Arch Gen Psychiatry 56:162–168
Cardno AG, Rijsdijk FV, West RM, Gottesman II, Craddock N, Murray RM, McGuffin P (2012) A twin study of schizoaffective-mania, schizoaffective-depression, and other psychotic syndromes. Am J Med Genet B Neuropsychiatr Genet 159B:172–182
Clementz BA, Grove WM, Iacono WG, Sweeney JA (1992) Smooth-pursuit eye movement dysfunction and liability for schizophrenia: Implications for genetic modeling. J Abn Psychology 101(1), 117–129. www.scopus.com
Copenhagen Statistical Department (1967) Population development and health conditions 1901–1960. Statistical Department, Copenhagen
Cuthbert BN, Insel TR (2013) Toward the future of psychiatric diagnosis: the seven pillars of RDoC. BMC Med 11, 126. http://www.bimoedcentral.com/1741-7015/11/126
D’Onofrio B, Rickert ME, Frans E et al (2014) Paternal age at childbearing and offspring psychiatric and academic morbidity. JAMA Psychiatry 71:432–438
Farmer AE, McGuffin P, Gottesman II (1987) Twin concordance for DSM-III schizophrenia: scrutinizing the validity of the definition. Arch Gen Psychiatry 44:634–641
Fischer M (1973) Genetic and environmental factors in schizophrenia: A study of schizophrenic twins and their families. Acta Psychiatr Scand Supp1 238:1–158
Franzek E, Beckmann H (1998) Different genetic background of schizophrenia spectrum psychoses: a twin study. Am J Psychiatry 155:76–83
Geddes JR, Verdoux H, Takei N et al (1999) Schizophrenia and complications of pregnancy and labor: an individual patient data meta-analysis. Schizophr Bull 25:413–423
Geschwind DH, Flint J (2015) Genetics and genomics of psychiatric disease. Science 349:1489–1494
Glahn DC, Knowles EEM, McKay DR et al (2014) Arguments for the sake of endophenotypes: examining common misconceptions about the use of endophenotypes in psychiatric genetics. Am J Med Genet B Neuropsychiatr Genet 165B:122–130
Gottesman II, Gould TD (2003) The endophenotype concept in psychiatry: etymology and strategic intentions. Am J Psychiatry 160:636–645
Gottesman II, McGue M (2014) Endophenotype. In: Cautin RL, Lilienfeld SO (eds) Wiley-Blackwell encyclopedia of clinical psychology. Wiley, New York
Gottesman II, Shields J (1967) A polygenic theory of schizophrenia. Science 156,53–538. (Abstract) Proc Natl Acad Sci USA 58, 199–205. [Reprinted in Int J Ment Health 1972,1,107–115]
Gottesman II, Shields J (1972) Schizophrenia and Genetics, a Twin Vantage Point. Academic Press, New York, London
Gottesman II, Laursen TM, Bertelsen A, Mortensen PB (2010) Severe mental disorders in offspring with 2 psychiatrically ill parents. Arch Gen Psychiatry 67:252–257
Hauge M, Harvald B, Fischer M et al (1968) The Danish twin register. Acta Genet Med Gemellol 17(2):315–332
Insel TR, Cuthbert BN (2009) Endophenotypes: bridging genomic complexity and disorder heterogeneity. Biol Psychiatry 66:988–989
Insel T, Cuthbert B, Garvey M, Heinssen R, Pine DS, Quinn K, Sanislow C, Wang P (2010) Research Domain Criteria (RDoC): toward a new classification framework for research on mental disorders. Am J Psychiatry 167:748–751
Kendler KS, Zachar P, Craver C (2011) What kinds of things are psychiatric disorders? Psychol Med 41:1143–1150
Kirov G (2010) The role of copy number variation in schizophrenia. Expert Rev Neurotherapeutics 10:25–32
Kirov G, Grozeva D, Norton N, Ivanov D, Mantripragada KK, Holmans P, Craddock N, Owen MJ, O’Donovan MC (2009) Support for the involvement of large copy number variants in the pathogenesis of schizophrenia. Hum Mol Genet 18(8):1497–1503
Kläning, U. (1996). Schizophrenia in twins: Incidence and risk factors. Unpub.Ph.D. Dissertation. University of Aarhus, Aarhus, Denmark
Kringlen E (1967) Heredity and Environment in the Functional Psychoses. An Epidemiological - Clinical Twin Study. Universitetsforlaget, Oslo
Kyvik KO, Green A, Nielsen HB (1995) The New Danish Twin Register: establishment and analysis of twinning rates. Int J Epidemiol 24:589–596
Kyvik KO, Christensen K, Skytthe A et al (1996) The Danish Twin Register. Dan Med Bull 43:467–470
Lee SH, Decandia TR, Ripke S, Yang J, Sullivan PF, Goddard ME, Keller MC, Visscher PM, Wray NR (2012) Estimating the proportion of variation in susceptibility to schizophrenia captured by common SNPs. Nat Genet 44:247–250
Lee SH, Ripke S, Neale BM, Faraone SV, Purcell SM, Perlis RH et al (2013) Genetic relationship between five psychiatric disorders estimated from genome-wide SNPs. Nat Genet 45(9):984–994
Lencz T, Liu C, Rosenfeld J, Mukherjee S, DeRosse P et al (2013) Genome-wide association study implicates NDST3 in schizophrenia and bipolar disorder. Nat Commun 4:2739. doi:10.1038/ncomms3739
Lenzenweger MF (2010) Schizotypy and schizophrenia-the view from experimental psychopathology. Guilford, New York
Lichtenstein P, Yip BH, Björk C et al (2009) Common genetic determinants of schizophrenia and bipolar disorder in Swedish families: a population-based study. Lancet 373(9659):234–239
Loranger AM (1988) Personality disorder examination. Yonkers, New York
Matheson SL, Shepherd AM, Laurens KR, Carr VJ (2011) A systematic meta-review grading the evidence for non-genetic risk factors and putative antecedents of schizophrenia. Schizophr Res 133:133–142
McGrath J, Welham J, Scott J, Varghese D, Degenhardt L, Hayatbakhsh MR et al (2010) Association between cannabis use and psychosis-related outcomes using sibling pair analysis in a cohort of young adults. Arch Gen Psychiatry 67:440–447
McGue M (1992) When assessing twin concordance, use the probandwise and not the pairwise rate. Schizophr Bull 18:171–176
Meehl PE (1972) A critical afterword. In: Gottesman II, Shields J (eds) Schizophrenia and Genetics: A Twin Study Vantage Point. Academic Press, New York, London, pp 367–415
Mors O, Perto GP, Mortensen PB (2011) The Danish Psychiatric Central Research Register. Scand J Pub Health 39:54–57
Munk-Jorgensen P (1986) Decreasing first-admission rates of schizophrenia among males in Denmark from 1970 to 1984. Acta Psychiatr Scand 23:645–650
Munk-Jorgensen P, Jorgensen P (1986) Decreasing rates of first-admission diagnoses of schizophrenia among females in Denmark from 1970 to 1984. Acta Psychiatr Scand 74:379–383
Munk-Jorgensen P, Mortensen PB (1997) The Danish Psychiatric Central Register. Dan Med Bull 44:82–84
Murray RM, Jones PB, Susser E, Van Os J, Cannon M (eds) (2003) The Epidemiology of Schizophrenia. Cambridge University Press, Cambridge
National Institute of Mental Health (2014) Research Domain Criteria (RDoC). http://www.nimh.nih.gov/research-priorities/rdoc/index.shtml
Neale MC (2004) Mx Statistical Modeling. 6th Edition. http://www.vipbg.vcu.edu/~vipbg/software/mxmanual.pdf
O’Reilly R, Torrey EF, Rao J, Singh S (2013) Monozygotic twins with early-onset schizophrenia and late-onset bipolar disorder: a case report. J Med Case Reports 7:134
Onstad S, Skre I, Torgersen S, Kringlen E (1991) Twin concordance for DSM-III-R schizophrenia. Acta Psychiatr Scand 83:395–401
Pedersen CB, Gøtzsche H, Møller JØ, Mortensen PB (2006) The Danish civil registration system. Dan Med Bull 53(4):441–449
Pedersen CB, Mors O, Bertelsen A, Lindum Waltoft B, Agerbo E, McGrath JJ, Mortensen PB, Eaton W (2014) A comprehensive nationwide study of the incidence rate and lifetime risk for treated mental disorders. JAMA Psychiatry 71:573–581
Petronis A (2010) Twin studies in schizophrenia with special emphasis on concordance figures. Nature 465:721–727
Prata DP, Mechelli A, Fu CHY, Picchioni M, Toulopoulou T, Bramon E, Walshe M, Murray RM, Collier DA, McGuire P (2009) Epistasis between the DAT 3′ UTR VNTR and the COMT Val158Met SNP on cortical function in healthy subjects and patients with schizophrenia. Proc Natl Acad Sci USA 106(32), 13600–13605. www.scopus.com
Purcell SM, Wray NR, Stone JL, Visscher PM, O’Donovan MC, Sullivan PF et al (2009) Common polygenic variation contributes to risk of schizophrenia and bipolar disorder. Nature 460:748–752
Rijsdijk FV, Sham PC (2002) Analytic approaches to twin data using structural equation models. Brief Bioform 3:119–133
Ritsner MS, Gottesman II (2009) Where do we stand in the quest for neuropsychiatric biomarkers and endophenotypes and what next? In: Ritsner MS (ed) The handbook of neuropsychiatric biomarkers, endophenotypes, and genes, neuropsychological endophenotypes and biomarkers, vol 1. Springer, New York, pp 3–22
Ritsner MS, Gottesman II (2011) The schizophrenia construct after 100 years of challenges. In: Ritsner MS (ed) Handbook of schizophrenia spectrum disorders, conceptual issues and neurobiological advances, vol 1. Springer, New York, pp 1–44
Russo M, Levine SZ, Demjaha A, DiForti M, Bonaccorso S, Fearon P et al (2014) Association between symptom dimensions and categorical diagnoses of psychosis: a cross-sectional and longitudinal investigation. Schizophr Bull 40:111–119
Schmittmann VD, Cramer AOJ, Waldorp LJ, Epskamp S, Kievit RA, Borsboom D (2013) Deconstructing the construct: a network perspective on psychological phenomena. New Ideas Psychol 31(1):43–53
Sullivan PF, Kendler KS, Neale MC (2003) Schizophrenia as a complex trait, Evidence from a meta-analysis of twin studies. Arch Gen Psychiatry 60:1187–1192
Sullivan PF, Daly MJ, O’Donovan M (2012) Genetic architectures of psychiatric disorders. The emerging picture and its implications. Nat Rev Genet 13:537–551
Susser E, Neugebauer R, Hoek HW, Brown AS, Lin S, Labovitz D, Gorman JM (1996) Schizophrenia after prenatal famine: further evidence. Arch Gen Psychiatry 53:25–31
Tienari P (1975) Schizophrenia in Finnish male twins. In: Lader MH (ed) Studies of Schizophrenia. Kent, Ashford, pp 29–35
Turkheimer E, Haley A, Waldron M, D’Onofrio B, Gottesman II (2003) Socioeconomic status modifies heritability of IQ in young children. Psychol Sci 14:623–628
Vallgarda S (1995) Trends in perinatal death rates in Denmark and Sweden, 1915–1990. Paediatr Perinat Epidemiol 9:201–218
VanDongen J, Slagboom PE, Draisma HHM, Martin NG, Boomsma DJ (2013) The continuing value of twin studies in the omics era. Nat Rev Genet 13:640–653
Warner R (1995) Time trends in schizophrenia: changes in obstetric risk factors with industrialization. Schizophr Bull 21:483–500
Wing JK, Babor T, Brugha T, Burke J, Cooper JE, Giel R, Jablenski A, Regier D, Sartorius N (1990) SCAN. Schedules for Clinical assessment in Neuropsychiatry. Arch Gen Psychiatry 47:589–593
World Health Organization (1967) Manual of the international statistical classification of diseases, injuries, and causes of death. based on the recommendations of the eighth revision conference, 1965, and adopted by the nineteenth world health assembly, World Health Organization, Geneva
World Health Organization (1974) Glossary of mental disorders and guide to their c1assification for use in conjunction with the International Classification of Diseases, 8th Revision. World Health Organization, Geneva
World Health Organization (1992) The lCD-10 c1assification of mental and behavioural disorders. Clinical descriptions and diagnostic guidelines. World Health Organization, Geneva
World Health Organization (1993) The ICD-10 classification of mental and behavioural disorders. Diagnostic criteria for research. World Health Organization, Geneva
Wray NR, Gottesman II (2012). Using summary data from the Danish National Registers to estimate heritabilities for schizophrenia, bipolar disorder and major depressive disorder. Front Genet, 3, Article 118
Yang J, Lee SH, Goddard ME, Visscher PM (2011) GCTA: a tool for genome-wide complex trait analysis. Am J Hum Genet 88:76–82
Acknowledgments
The authors wish to thank Christin Sindballe,, M.D, Psychiatric Center Bispebjerg, Copenhagen, for interviewing the cotwins. We are grateful for the helpful comments on earlier versions of this report from Alastair Cardno and Nick Martin and on the current version from Michael Lyons, Greg Carey, Matt McGue, and anonymous reviewers.
Funding
This work was supported by Sygekassernes Helsefond, Forskerakademiet, Forskningsinitiativet under Århus University; the Theodore and Vada Stanley Foundation, Fonden til Forskning af Sindslidelse, Fonden til Psykiatriens Fremme (Petra & Cris Andersens Fond) and Eli Lilly Denmark AIS; and a Vassar College study leave to SLT. IIG was supported by the Lieber Prize for Schizophrenia Research and the University of Louisville Grawemeyer Award in Psychology.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Ulla Kläning, Susan L. Trumbetta, Irving I. Gottesman, Axel Skytthe, Kirsten O. Kyvik, and Aksel Bertelsen declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2000 (5). Informed consent was obtained from all patients for being included in the study.
Additional information
Edited by Michael Lyons.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Kläning, U., Trumbetta, S.L., Gottesman, I.I. et al. A Danish Twin Study of Schizophrenia Liability: Investigation from Interviewed Twins for Genetic Links to Affective Psychoses and for Cross-Cohort Comparisons. Behav Genet 46, 193–204 (2016). https://doi.org/10.1007/s10519-015-9765-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10519-015-9765-z