Abstract
With global warming, extreme environmental heat is becoming a social issue of concern, which can cause adverse health results including heatstroke (HS). Severe heat stress is characterized by cell death of direct heat damage, excessive inflammatory responses, and coagulation disorders that can lead to multiple organ dysfunction (MODS) and even death. However, the significant pathophysiological mechanism and treatment of HS are still not fully clear. Various modes of cell death, including apoptosis, pyroptosis, ferroptosis, necroptosis and PANoptosis are involved in MODS induced by heatstroke. In this review, we summarized molecular mechanism, key transcriptional regulation as for HSF1, NRF2, NF-κB and PARP-1, and potential therapies of cell death resulting in CNS, liver, intestine, reproductive system and kidney injury induced by heat stress. Understanding the mechanism of cell death provides new targets to protect multi-organ function in HS.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Epidemiology of heatstroke
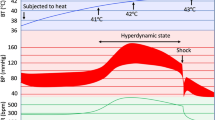
Extreme heat events are becoming permanent features of summer seasons worldwide, causing many excess deaths. Heat-related morbidity and mortality are increasing further as climate change progresses [1]. Exposure to extremely high temperatures causes heatstroke which could lead to needless suffering and death. In high-income countries, heat is one of the largest weather-related causes of death [1]. In addition to mortality, hot weather and heat extremes are associated with increased emergency room visits and hospital admittance [2,3,4], increased deaths from cardiorespiratory and other diseases [5], mental health issues [6], adverse pregnancy and birth outcomes, and increased health-care costs [7] (Fig. 1).
Pathogenesis and pathophysiology of heatstroke
Heatstroke is a severe life-threatening disease, typically characterized by an increase in core body temperature more than 40° C and convulsion, delirium, or coma which lead by central nervous system (CNS) dysfunction [8]. According to the main classification method, heatstroke is divided into two types, namely, classic heatstroke (CHS) and exertional heatstroke (EHS) [9]. Our review focuses on the pathogenesis and pathophysiology of CHS, especially induced by key transcription factors and the associated major organ injuries induced by CHS [10]. The original pathogenic and pathophysiologic mechanisms of heatstroke could be described as two stages which change from a compensable thermoregulatory stage to a non-compensable stage. Our group puts forward the theory of second strike of heat stroke. The body first receives damage due to direct heat stress, and then secondary damage due to immune disorders and blood clotting disorders. The HS-induced damage appears in major organs, such as brain, lung, intestine, liver, kidney, and reproductive system. We elaborate the main factors and mechanisms of pathogenesis and pathophysiology below.
Key transcription factors in heat stress regulation
HSF1
During the response to heat stress, heat shock proteins (HSPs) are induced, which correct protein misfolding. The heat shock factor family includes HSF1, HSF2, HSF3, HSF4, HSFX and HSFY [13]. HSF1 binds to the promoter of heat shock proteins and is involved in the transcriptional regulation of many heat shock proteins including HSP70, HSP90, HSP110, HSP40 and small HSPs [14]. HSF1 is also involved in the regulation of cell death. HSF1 inhibits endogenous and exogenous apoptosis by directly regulating HSP [15]. HSP70 inhibits activation of Bax and down-regulation of the anti-apoptotic protein MCL-1 [16]. In addition, HSP70 plays an important role in the caspase-independent apoptotic pathway. It can inhibit apoptosis by interacting with apoptosis-inducing factor (AIF). Conversely, apoptosis-associated proteins also inhibit the activation of HSF1. HSF1 and scaffold attachment factor B (SAFB) can form stress granules that up-regulate HSP27 and HSP70, which are involved in heat stress-induced apoptosis [17].
HSF1 binds to the promoter region of ATG7, a key enzyme in autophagy, and upregulates ATG7 expression, thereby promoting protective autophagy in cells [18]. Another important target gene of HSF1 is p62/SQSTM1, which is involved in the formation of autophagic vesicles. p62/SQSTM1 is involved in the phosphorylation of key residues S349 and S403 for its activation in an HSF1-dependent manner, and HSF1 can induce autophagy to enhance cell survival by regulating the activity of p62/SQSTM1 [19].
Erastin upregulates the expression of HSP27, which regulates iron uptake by stabilizing the cytoskeleton and downregulates iron taken up by transferrin receptor 1 (TFR1), in an hsf1-dependent manner. Meanwhile, HSF1 contributes to nuclear translocation and stabilization of p53, and many studies have shown that p53 promotes ferroptosis by regulating SLC7A11 [20]. However, the mechanisms of HSF1 regulating ferroptosis have not been fully elucidated and deserve further study.
NRF2
Nrf2 is a key transcription factor that regulates oxidative stress response and is involved in a variety of biological processes such as neuroinflammation, mitochondrial dysfunction, autophagy, ferroptosis, etc. [21]. Dysregulation of the Nrf2 may lead to a range of disease progression. Studies have shown that Nrf2 upregulates hsp70, hsp90, hsp110 and the superoxide dismutase (SOD), glutathione peroxidase (GPX), to increase heat tolerance in Drosophila [22]. Meanwhile, in the liver of heat-stressed mice, the expression of Nrf2 and macrophage migration inhibitory factor (MIF) is up-regulated, which was involved in the regulation of oxidative stress, mitochondrial dysfunction, and inflammatory pathways [22]. Nrf2 is also involved in oxidative stress and apoptosis in mammary epithelium of cows under heat stress [23]. Camel whey protein could reduce hepatic HMGB1 release and attenuate heat stress-induced oxidative stress injury by up-regulating Nrf2 in hepatocytes [24].
NF-κB
Heat stress affects NF-κB-regulated signal transduction involved in the regulation of cell death and inflammatory response [25]. Heat stress reduces the immune response in the ileal region of chickens induced by Salmonella infection through the NF-κB/NLRP3 [26]. Meanwhile, activation of the TLR4/NF-κB and NLRP3 pathways induced hepatic inflammation in broiler chickens [27]. Heat stress induced aseptic inflammatory responses in the mouse hippocampus, including microglia and astrocyte activated and producing pro-inflammatory cytokines. β-Hydroxybutyric acid (BHBA) suppressed heat stress-induced inflammation by inhibiting the activation of the TLR4/p38 MAPK and NF-κB pathways [28]. Meanwhile, heat stress significantly up-regulated necroptosis-related molecules RIP1 and MLKL in rat lung microvascular endothelial cells (PMVECs) in a time-dependent manner, whereas RIP3 was not significantly up-regulated [29]. It is also involved in the generation of ROS in PMVEC [30].
PARP-1
Poly (adp-ribose) polymerase-1 (PARP-1) is a dna-binding protein which play an important role in inflammation. HS promotes nuclear translocation of AIF and leads to PARP-1 dependent neuron death, whereas Xuebijing injection inhibits oxidative stress via PARP-1/AIF pathway in rats brain under HS [31]. The ubiquitin ligase RNF4 ubiquitinates PARP-1 and affects its stability, which regulates HSP70 and participates in the heat stress response. It has been shown that inhibition of PARP activity increases the expression of HSPs and decreases cytokine levels, thereby improving survival. PARP1 inhibitors may have potential therapeutic value in HS [32] (Fig. 2) (Table 1).
Mechanisms of heatstroke-induced cell death
The pathogenesis of heatstroke-induced cell death involves multiple mechanisms. In addition to typical apoptosis, heat stress due to cell death via pyroptosis, necroptosis, ferroptosis and PANoptosis. These modes of cell death regulate heat stress and further development of heatstroke in different level.
HS & apoptosis
In the previous studies, apoptosis is referred to as the only mechanism of cell death, which has been the main subject of studying for the past three decades. The damage of nuclear membrane by caspase-6, the damage of genomic DNA into nucleosomal structures, the cleavage of intracellular proteins, the membrane blebbing, and the phosphatidylserine (PS) molecules exposing on the outer surface of the plasma membrane, which are the symbol of apoptosis and are widely used to identify the cell death pathway. The essential feature of apoptosis is related to two major pathways, the internal and external pathways. The internal pathway is regulated by the oligomerization of the B-cell lymphoma-2 (BCL-2) family proteins (eg. BAK and BAX), which also lead to the release of cytochrome c from mitochondria to cytosol and balance the promoting and demoting of apoptosis. The promoting and demoting proteins of the BCL-2 family involve initiator caspases (caspase-8, -9 and -10) and effector caspases (caspase-3, -6 and -7). The external pathway is regulated by the membrane receptors, for instance Death Receptors, Toll Like Receptor 4 (TLR4), or Tumor necrosis factor receptor 1 (TNFR1), involving Fas-associated death domain protein (FADD) or Tumor necrosis factor receptor 1-associated death domain protein (TRADD), receptor-interacting serine/threonine protein kinase 1 (RIPK1) and caspase-8. These proteins activate the progress of apoptosis through the crucial effector caspases (caspase-3 and -7), and subsequent activating caspases (caspase-2, -6, -8, and -10) [33].
According to F. Zhao et al. researching, their studies have shown that one of the well-documented mechanisms of heat stress-induced human spermatozoa’s cell death is apoptosis and melatonin shows dramatically potential in protecting sperm from heat stress and oxidative damage [36]. There is a large number of reactive oxygen species (ROS) generation with the development of heat stress and affects human spermatozoa’s viability and motility via doing harm to the intracellular homeostasis and leading to apoptosis in human spermatozoa. When heat stress happens in human spermatozoa, melatonin can alleviate the damage by suppressing ROS generation and apoptosis in human spermatozoa, increasing mitochondrial membrane potential, reducing sperm DNA damage, reducing the lipid peroxidation product and 4-HNE formation. The role of melatonin is similar to that of antioxidant [37].
Besides, J. Zhu et al. previous studies, their findings indicate that neuronal apoptosis is a vital basis of heat stress-induced brain injury and microglia in heat stress actively induce apoptosis of hippocampal neurons by means of a transwell coculture system. MiR-466i-5p which was screened by high-throughput sequencing and further conducted gene ontology (GO) pathway analysis is considered as the mostly upregulated microRNAs in heat stress exosomes and may regulate apoptosis through the Bcl-2/caspase-3 pathway [38, 39]. By qRT-PCR, histopathological analysis, immunohistochemistry, statistical analysis, and another basic experiments, J. Zhu et al. explored the function of miR-466i-5p and its effect on neuron apoptosis and further brain injury. MiR-466i-5p antagomir, a treatment for HS apoptosis-induced brain injury. Heatstroke patients with brain injury have a poor prognosis because it is primarily due to heat-stress-induced neuronal apoptosis, which is now understood to be a new crosstalk mechanism among cells that involves microglial exosomal miR-466i-5p. This mechanism promotes hippocampal neuron apoptosis and contributes to brain injury in heatstroke patients. In t J. Zhu et al. studying, a potential treatment was found that nasal delivery of miR-466i-5p antagomir reversed HS neuron apoptosis and relatived brain injury [38, 40].
HS & pyroptosis
Pyroptosis is a classical type of programmed cell death which could be described with the loss of plasma membrane damage inducing by inflammasome sensors activation [33]. Furthermore, the essential requirement of pyroptosis could be described with both active caspase-1 and PI positivity [41]. In addition, caspases have been identified as mediators of pyroptosis [42, 43]. Once activated, caspase-1 and caspase-11 mediate the cleavage of gasdermin D (GSDMD), eliminating an autoinhibitory carboxy-terminal domain from GSDMD. This action enables the N-terminal fragment to form pores on the plasma membrane, finally inducing pyroptosis [43, 44]. Such as mature IL-1β, mediated by the release of cytokines as well as necroptosis in living cells, without signal peptides [45, 46].
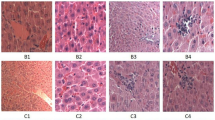
Yan Geng et al. discuss that heat stress-induced hepatocyte pyroptosis in vivo and in vitro by mediating High mobility group box-1 protein (HMGB1) signaling activation [47]. Most of HS patients who had significantly high mortality always increased HMGB1 levels in a certain extent [48]. To further confirm the role of HMGB1, Wang et al. used HMGB1 monoclonal antibody to specifically block the effect of HMGB1 to explore the key role of HMGB1 in heat stress-induced ALI [49]. Meanwhile, HMGB1 is the most strongly associated inflammasome sensor in the development of pyroptosis and uncontrolled inflammation [50]. Additionally, the proteomic analysis demonstrated that the pathway primarily affected by heat stress was programmed cell death regulation [51]. Activation of the inflammasome accompanies HS-induced liver injury, effectively initiating the activation of IL-1β and pyroptosis in hepatocytes, leading to severe liver damage [47].
Taken all together, these findings suggest that HMGB1 is necessary for hepatocyte pyroptosis and subsequent heat stress-induced liver injury amplification [47, 52, 53].
HS & necroptosis
Necroptosis, as known as one of the traditional three programmed cell death (PCD), medicates cell death by four important factors, RIPK1, RIPK3, MLKL and ZBP1. As a caspase-dependent PCD, caspase-8 is vital to medicate. Caspase-8 suppresses the kinase activation of RIPK1 and mediates the cleavage of RIPK1. Active RIPK1, the main pathway to medicate necroptosis, forms necrosome (complex IIb) also includes PIPK3 and MLKL under apoptosis-deficient condition [54]. Additionally, Caspase-8 has the capability to cleave RIPK3. Meanwhile, RIPK1 is activated under heat stress, metabolic and hypoxia [55,56,57]. Independent of these typical pathways, Z-DNA binding protein 1 (ZBP1) medicates necroptosis in research in recent years [45, 58].
Heat stress elevated the necrotic cell rate and expression levels of RIPK1, RIPK3, and phosphorylated MLKL in IEC-6 cells [59]. The heightened expression levels facilitated increased formation of the RIPK1-RIPK3 complex, leading to necrosome formation. As a cellular consequence, HS induced necroptosis, oxidative stress response, and mitochondrial damage, eventually resulting in small intestinal tissue injury. The ROS scavenger N-acetyl-L-cysteine (NAC) pretreatment notably inhibited HS-induced RIPK1/RIPK3-dependent necroptosis formation. Consistent with our findings, Nec-1 or GSK’872 pretreatment reduced HS-induced intestinal injury in vivo. Scavenging ROS production also inhibited HS-induced RIPK1/RIPK3-dependent necroptosis activation both in vivo and in vitro [60]. These results suggest that preventing necroptosis through scavenging ROS production may cell death induced by HS and alleviate small intestinal tissue injury [61].
Moreover, Fangfang Yuan et al. found a Z–nucleic acid receptor, ZBP1, which appears to mediate heatstroke via necroptosis by triggering a key receptor, receptor interacting protein kinase 3 (RIPK3)-dependent cell death. Meanwhile, deleting the ZBP1, RIPK3, caspase-8, and mixed lineage kinase domain-like (MLKL) can decrease heat stress–induced injury, such as cell death, circulatory failure, and organ injury [62,63,64,65]. Their study identifies the key role of ZBP1 in promoting the pathologic pathway of heat stress through RIPK3-dependent cell death [66, 67].
HS & ferroptosis
Ferroptosis, a distinctive form of cell death propelled by iron-dependent phospholipid peroxidation, is under the control of several cellular metabolic pathways. These pathways include redox homeostasis, iron handling, mitochondrial activity and metabolism of amino acids, lipids and sugars, alongside diverse signaling cascades implicated in pathological conditions [68]. The regulation of reactive oxygen species (ROS) levels and cellular metabolism can influence ferroptosis, impacted by intracellular and intercellular signaling events as well as environmental stresses. Moreover, nutrient supply control the cell metabolic state. The metabolic regulation is crucial in understanding the connection between ferroptosis and pathologies linked to tissue damage, where ferroptotic cell death plays a key role in cell loss [69]. Therefore, inhibiting ferroptosis emerges as a potential therapeutic strategy for these pathologies.
The discovery of ferroptosis also enables advances in the treatment of cancer [70]. Manipulating cell action rather than indiscriminately activating or restraining immune response could avoid unnecessary systemic inflammatory response and accurately regulate autoimmune diseases [71]. Especially, heat stress-induced metabolic control, ferroptosis, is active in cancer cell. S. Xie et al. finding that heat stress disrupts the redox homeostasis of tumor cells by inhibiting the synthesis of GSH, resulting in the production of a large amount of LPO through lipid metabolic reprogramming and redox, which eventually induces tumor ferroptosis [72]. Furthermore, the discovery of the key regulator ACSBG1, as an acyl-CoA synthetase, allows for the transformation of prostate cancer cell death from ferroptosis to non-ferroptotic death. This metabolic reprogramming might to be an effective treatment of plastic tumors and be able to avoid damage to normal tissues. Consequently, knockout ACSBG1 in this process could determine which type of cell death to tumor is more sensitive and have a potential treatment in prostate cancer [73].
In Yingyi Luan et al. studying, they found that baicalein may protect HK-2 cell from endoplasmic reticulum stress (ERS)-associated ferroptosis under heat stress, which induced by high myoglobin, associated with acute kidney injury (AKI) [74]. Serum myoglobin, related with incident rhabdomyolysis (RM)-induced AKI after exertional heatstroke (EHS), was predicting the occurrence and prognosis of AKI that serum myoglobin ≥ 1000 ng/mL in EHS. Consistent with their findings, the experimental models they used also indicated that after heat stress, the effect of myoglobin on human kidney proximal tubular cells includes exacerbating cell ferroptosis and inducing the ERS response.
HS & PANoptosis
PANoptosis, is first known as a pathogen infection model in current studying, originally characterized as an inflammatory cell death modulated by PANoptosome. The key features of PANoptosis includes apoptosis, necroptosis, and pyroptosis [75]. According to the recent research, PANoptosis predominantly relates to the formation of PANoptosome, namely, a certain kind of polyprotein complexes. The composition of PANoptosome varies depending on the triggering factors, but it consistently incorporates with ZBP1, absent in melanoma 2 (AIM2), RIPK3, RIPK1, apoptosis-associated speck-like protein containing a caspase recruitment domain (ASC), Fas-associated protein with death domain (FADD), CASP8, along with key components responsible for performing pyroptosis, apoptosis, and necroptosis [77].
Gasdermin family proteins (e.g., gasdermin D) or MLKL mediate programmed necrosis in vertebrates. When these proteins are activated, pores are formed on intracellular or cytoplasmic membranes [78,79,80,81]. MLKL is activated by RIPK3-dependent phosphorylation and produce a type of programmed cell death, namely, necroptosis [80, 81]. Moreover, activation of gasdermin D (GSDMD) triggers other the type of programmed cell death, namely, pyroptosis, which is also closely related with PANoptosis associated ZBP1 [78, 79]. In sepsis, immoderate activation of GSDMD causes multiple organ dysfunctions and disseminated intravascular coagulation (DIC), which is an infection-induced severe disease as same as heatstroke in clinical signs [8, 82, 83]. They systematically elaborated the possible pathogenesis and mechanisms of heat stress-induced programmed cell death and It is found that ZBP1, a Z–nucleic acid sensor [63,64,65], induces the pathological features of heat stress by triggering the activation of RIPK3-induced MLKL-dependent cell death and caspase-8 (casp8)-dependent cell death in a lesser extent.
Yuan F et al. found that heat shock transcription factor 1 (HSF1) promoted the expression of Z-DNA binding protein 1 (ZBP1) and primarily activated ZBP1 through the RHIM domain under heat stress, thereby mediating RIPK3 dependent programmed cell death, including PANoptosis [62]. In the latest research, M. Zheng et al. have also found that ZBP1 regulates PANoptosis through RIPK3, RIPK1, and CASPs during influenza virus infection [84]. PANoptosis is a regulated cell death mechanism coordinated by the PANoptosome, a multi-protein complex. This pathway fostered co-regulation and crosstalk among cellular processes [62]. In addition, heat stress stimulated ZBP1 transcription in the liver, lung, kidney, and intestine [64, 66]. Due to the presence of many key proteins and their related molecules in the process of PANoptosis, these molecules are expected to serve as drug targets for the development of specific therapeutic drugs for heat stroke, thereby bringing significant improvements to the prognosis of heat stroke [62, 85, 86] (Fig. 3).
HS & autophagy
Autophagy is a cellular process for degrading and recycling proteins and organelles to maintain intracellular homeostasis. Though the autophagy mechanisms or excessive autophagic flux often result in cell death, consistent with our findings, it still serves a protective function in cells [87, 88]. SZ Liu et al. explore the augmentation of autophagy in disease therapy and propose a novel viewpoint emphasizing its utilization for various functional transitions, including both autophagy and different modes of autophagy-mediated cell death to treat heat stress-induced organ injuries in clinic [89].
Previous research has shown that autophagy is inhibited by AKT and ameliorated by AMPK. [90] By labelling autophagy-associated markers [91], Hu, J.M. et al. find that autophagy is triggered to eliminate damaged organelles and proteins, serving as pivotal regulators of cellular homeostasis during heat stress [92]. Ethyl pyruvate (EP), a derivative of pyruvic acid, effects with antioxidant and anti-inflammatory [93]. By inducing stress proteins and activating autophagy in rats, EP mitigates heat stress-induced multi-organ dysfunction and inflammatory responses. Their study examines the impact of EP on multiple organ dysfunction (MOD) in HS rats and elucidate potential mechanisms, finding that EP might hinder the dysfunction of autophagosome degradation induced by HS [89]. According to Quentin Willot et al. research, they find that heat stress would induce an upregulation of autophagy in the tissues of flies and exposure to rapamycin would elicit a measurable autophagic response in adult flies, consequently enhancing their heat tolerance [94, 95]. These findings provide compelling evidence for a significant protection role of autophagy in the mechanisms heat stress-induced organs damage.
Based on our theory of heatstroke, different from sepsis and tumors, human body first receives damage due to direct heat stress, as a physical stimulus, and then secondary damage due to immune disorders and blood clotting disorders. As for the cell death induced by tumors and sepsis, human body is damage by tumor cells and inflammatory factors directly at first time, which included complex biochemical stimulus, then causes multi-organs injuries as same as the heat stress induced. Furthermore, different from previous widely known research on heat stress-induced organ injuries, heat stress with specifically temperature even has objective effects on the treatments of some type of tumors. Also, autophagy, a special type of cell death, play an important role in protecting organ’s function form heat stress-induced damage.
The therapy of cell death in heatstroke and clinical perspective
Traditional views suggested that heatstroke may mainly originate from simple physical injury. Clinical interventions currently mainly included cooling and supportive treatment, without suitable specific therapeutic drugs available. However, there are some potential treatments for different organs that deserve further investigation.
Melatonin
Melatonin, a treatment for HS apoptosis-induced spermatozoa injury. The quality of human spermatozoa is the important factor to the outcome of pregnancy [96]. However, heat stress-induced oxidative damage reduces the reproductive capacity of spermatozoa. Based on F. Zhao et al. finding, it is melatonin that could be a potential clinical treatment and reproductive technology for male spermatozoa injury, especially in heat stress-induced oxidative stress injury [37].
Dexmedetomidine
Dexmedetomidine (DEX), as a selective α2-adrenergic agonist, in addition to its well-known threapy, there is a hotspot with DEX in the research of protecting organs injury and improving survival with increasingly clinical applications in recent years [97,98,99]. Several clinical and fundamental investigations have validated that DEX is able to diminish inflammatory reactions by modulating the immune system, trigger anti-apoptotic pathways for cellular protection against damage, and confer protective effects on diverse organs such as the brain, intestine, lung, and kidney. Remarkably, clinical trials have demonstrated that DEX can mitigate the systemic inflammatory response and multiple HS-induced organs injury [100].
In the study of P. Li et al., DEX showed its ability to reduce neuron apoptosis and neuroinfammation in the progression of CNS diseases caused by heatstroke [101]. Their research has revealed that DEX has the ability to decrease neuroinflammation by stimulating the transformation of microglial cells into a phenotype with no nerve-damaging functions [102]. In summary, these discoveries suggest that DEX may be a potential therapeutic strategy for ameliorating HS-induced brain injury and neuroinflammation by activation of the PI3K/Akt signaling pathway through TREM2 [103].
In Y. Geng et al. research, they found that heatstroke induced acute lung injury (ALI) and pulmonary dysfunction, but DEX treatment can effectively inhibit lung injury and improve respiratory dysfunction. HS also leads to a significant upregulation of the Toll-like receptor 4 (TLR4)/MyD88/NFκB signaling pathway in lung tissue,which effects could be counteracted by the treatment of DEX. Additionally, DEX treatment can restore the downregulated expression of caveolin 1 caused by HS, thus contributing to the inhibition of the TLR4/MyD88/NFκB signaling pathway [104]. By inhibiting the inflammatory response, DEX may potentially provide effective protection against HS-induced ALI. Consequently, it is suggested that DEX holds promise as a viable and efficient threapy for heatstroke [105].
In present investigation, DEX showed its administration of the significant reduction in systemic inflammatory response and the protective effects against intestinal dysfunction. This was achieved by inhibiting intestinal apoptosis and preserving the integrity of the intestinal barrier during heatstroke [106, 107]. In Z. N. Xia, et al. studying, comparable findings were identified in HS mice, represented as structural damage to intestine. DEX could simultaneously decrease the level of serum inflammatory cytokines through inhibiting the activation of intestinal NF-kB [108]. Their results also showed that DEX decreased HS-induced TUNEL-positive cells in a Bax/Bcl-2-related manner [109]. Taken together, their results indicate that DEX treatment significantly prevented intestinal injury, maintained the structure of intestine, increased the expression of the main tight junction proteins, occludin and ZO-1, and decreased apoptosis in intestine [100].
Heatstroke also leads to systemic inflammation, resulting in vascular endothelial damage. Endothelial glycocalyx (EGCX) coats the normal vascular endothelium [110]. DEX not only preserved EGCX but also improved survival in rats model [111].
Thrombomodulin
The treatments for heat stress-induced liver damage included supportive therapy and liver transplantation. The emphasis is primarily on supportive therapy, which includes thrombomodulin (TM) intervention, early oxygen supply, cooling treatment, continuous blood purification, anti-inflammatory treatment, anticoagulant therapy. For patients with irreversible liver damage, liver transplantation is a possible option. Especially, TM had been shown to reduce plasma HMGB1 levels even when treatment was delayed [112]. Besides ameliorating heat stress-induced liver injury by improving the coagulation state systemically, these findings also suggested that excessive inflammatory reactions effectively inhibited by TM in heat stress. In conclusion, TM supplementation is ought to be a crucial treatment strategy for patients with HS as it effectively improves heat stress-induced liver injury, potentially through various mechanisms. Y. Geng et al. conducted a systematic analysis of the potential mechanisms and treatment strategies associated with heat stress-induced liver injury. This comprehensive investigation has laid the groundwork for a theoretical understanding and identified future research direction in the field of heat stress-induced liver injury [47].
Mesenchymal stem cell
Mesenchymal stem cells (MSCs) can arrive brain tissue that needs treatment, crossing the blood–brain barrier. Multidirectional differentiation can be one way for them to achieve therapeutic goals [113]. MSCs have the ability to differentiate into various adult cells, including chondrocytes, osteoblasts, neural progenitor cells, and others so that MSCs can be used in brain injury treatment [114]. However, on the other hand, the powerful repair function also carries the risk of causing cancer. There is still an unclear risk of the host immune system's immune response to it. In addition, research has shown that another way to exert its effect is through paracrine mechanisms [113]. Some research evidence suggests that it achieves therapeutic effects more through paracrine mechanisms rather than differentiated cell replacement mechanisms [114]. The secretion of nutritional factors including MCP-1, IL-6, growth factors-β, and others enable the control of inflammation in the damaged brain area, while promoting the formation of new blood vessels. Meanwhile, the remaining undamaged brain cells were also protected [113]. The released exosomes may play a crucial role in achieving their therapeutic effects. These exosomes are mostly vesicles containing miRNAs, RNAs, proteins, or long noncoding RNAs. Although various experimental data indicate the feasibility of using MSCs in the treatment of brain injury, clinical applications usually consider safety issues, making it difficult to evaluate the efficacy [115].
High pressure oxygen
In Ni, X. X. et al. studying [116], it was observed that high pressure oxygen (HBO) attenuated cytotoxicity, oxidative injury (measured by malondialdehyde levels), reactive oxygen species (ROS) generation, and decreased SOD activity and apoptosis in HS. Treatment with the Drp1 inhibitor (Mdivi-1) yielded similar effects and showed a tendency to reduce oxidative injury [117]. Both HBO and Mdivi-1 reduced the phosphorylation of DrpSer616 induced by HS, and HBO also decreased the phosphorylation of protein kinase C (PKC) induced by HS. Furthermore, both PKC inhibitor and ROS scavenger suppressed p-DrpSer616 in HS.
Building on previous findings [118, 119], excessive heat stress in body and scrotum, surpassing the normal physiological temperature range, may result in a reduction in germ cells within the testes, potentially leading to male infertility. Hsieh, K. L. et al. findings suggested that HBO preconditioning (HBOP) effectively mitigated hyperthermia in the body core and scrotum, as well as mitigating decreases in sperm count and motility, abnormalities in the testes/prostate/bladder, erectile dysfunction, and neurological impairments in adult male rats subjected to EHS [120]. Reducing expression levels of tight junctions (TJs) proteins induced by EHS and the increased apoptosis of Sertoli-Leydig cells, scrotal temperature, sperm quality, testicular structure, and erectile function can be alleviated by HBOP in rats experiments [121].
N-acetylcysteine
Intestinal damage is recognized as a pivotal factor in several critical illnesses in heatstroke [122]. Because of a diminished blood flow to the small intestine, prioritizing to brain and heart, the small intestinal epithelial tissue undergoes ischemia in hypoxic conditions, potentially leading to permanent tissue damage [123]. Heat stress caused damage to both the small intestine and intestinal epithelial cells, according to Li Li et al. Scavenging ROS production can alleviate this damage by significantly reducing RIPK1/RIPK3-dependent necroptosis, which mediates heat stress-induced intestinal damage. This sequence of events significantly hampers the functionality of small intestinal villus epithelial cells, triggering excessive cell death and increasing the risk of mortality. Remarkably, there was a significant reversal of HS-induced oxidative stress injury in intestine observed in both animals and cells that had been pre-treated with ROS scavenger N-acetylcysteine (NAC). In both in vitro and in vivo, NAC pretreatment led to a dramatic inhibition of necrosome formation in HS. Their finding suggest that future therapeutic strategies for patients diagnosed with heat stress-induced intestinal injury could focus on targeting this mechanism [59].
Baicalein
Baicalein is a treatment for HS ferroptosis-induced kidney injury. The data based on an clinical experiment involving about 200 patients in Y. Luan et al. research, showed that baicalein is likely to be a targeted therapeutic medication to reduce AKI patients with high myoglobin according to both the outcomes and baseline characteristics of serum biomarkers of RM in patients who underwent EHS stratified according to the incidence of AKI, and the association of myoglobin and AKI and 90-day mortality following EHS [74].
Ulinastatin
Ulinastatin (UTI), which found extensive application in treating diverse ailments, is a wide-ranging serine protease inhibitor derived from human urine, possessing potent anti-inflammatory and cytoprotective properties [124,125,126]. The current study of Tao Zhen et al. represents that UTI may confer protection against heat stress-induced brain injury and inflammatory responses by inhibiting cellular apoptosis and blocking the NF-κB/COX-2 pathway in rats. This study offers fresh insights into the mechanism through which UTI mitigates heatstroke-induced brain injury. Consequently, UTI could present a promising therapeutic approach for heat stress-induced brain injury [127, 128]. According to Peng Na et al. research, UTI may be an effective medication for early treatment of SHS-induced kidney damage. UTI inhibits the decline in superoxide dismutase (SOD) and glutathione peroxidase (GPx) activity, thereby reducing the level of malondialdehyde (MDA) in the kidneys of SHS rats, alleviating renal oxidative stress levels. Meanwhile, pathological damage to the kidneys and renal function parameters are improved [129]. Other previous research also showed that UTI has protective effects to against heat stress-induced acute lung injury by reducing the inflammatory exudation and pulmonary edema in mice [130].
Probiotics
Probiotics, comprising bacteria and yeast, are viable microorganisms that are beneficial to human health. It has been documented through animal experiments and clinical trials that probiotics have the potential to modulate intestinal microbiota, thereby controlling various gastrointestinal diseases and promoting overall well-being [131, 132]. Lei Li et al. results demonstrated that bacillus licheniformis (BL), a kind of probiotics, maintaining the function of intestinal barrier and modulating gut microbiota (GM), by pre-administration of BL for 7 days which prevented the onset of HS induced multi-organ injuries and mitigated its progression [122, 133, 134]. H. Cai, et al. find that probiotics can remodel GM by ameliorating heat stress-induced necroptosis in male germ cells [135]. During prolonged systemic heat stress, based on probiotic modification of GM decreases the expansion of aberrant bacteria and mitigates the dissemination of gut-derived inflammatory mediators into bloodstream, thereby alleviating inflammation in germ cells [136]. Overall, to gain a better understand of the therapy of HS-induced intestinal diseases even multi-organ injuries, we need further future directions and research in the area of beneficial effects of probiotics (Table 2).
Conclusion and prospect
Cell death is necessary for growth and development under tight regulation by the organism. Excessive cell death when regulation is impaired leads to the progress of a variety of diseases. Many molecular markers of death are now defined, for example, RIPK, MLKL are involved in the regulation of necroptosis, caspase-1, GSDMD are involved in the regulation of pyroptosis, and iron ion overdeposition is involved in the regulation of ferroptosis. Different patterns of cell death exist at different stages of injury to different organs under heatstroke. A comprehensive understanding of how cell die can help counteract aberrant under heatstroke. Heat-induced cell death can lead to the release of large amounts of DAMPs, which further activates the immune response and creating positive feedback. Use of specific cell death inhibitors may attenuate heat-induced organ damage. However, there are often multiple modes of cell death coexisting. Key molecules may be involved in regulating multiple modes of death, such as ZBP1, but the real situation is more complicated than we think. Targeting cell death inhibition process promises future translation into clinical rescue of heatstroke.
Data availability
No datasets were generated or analysed during the current study.
References
Ebi KL et al (2021) Hot weather and heat extremes: health risks. Lancet 398(10301):698–708
Onozuka D, Hagihara A (2015) All-cause and cause-specific risk of emergency transport attributable to temperature: a nationwide study. Medicine (Baltimore) 94(51):e2259
Liss A, Naumova EN (2019) Heatwaves and hospitalizations due to hyperthermia in defined climate regions in the conterminous USA. Environ Monit Assess 191(Suppl 2):394
Cheng YT, Lung SC, Hwang JS (2019) New approach to identifying proper thresholds for a heat warning system using health risk increments. Environ Res 170:282–292
Cheng J et al (2019) Cardiorespiratory effects of heatwaves: A systematic review and meta-analysis of global epidemiological evidence. Environ Res 177:108610
Thompson R et al (2018) Associations between high ambient temperatures and heat waves with mental health outcomes: a systematic review. Public Health 161:171–191
Liu Y et al (2019) Degrees and dollars – Health costs associated with suboptimal ambient temperature exposure. Sci Total Environ 678:702–711
Epstein Y, Yanovich R (2019) Heatstroke. N Engl J Med 380(25):2449–2459
Bouchama A et al (2022) Classic and exertional heatstroke. Nat Rev Dis Primers 8(1):8
Leon LR, Bouchama A (2015) Heat stroke. Compr Physiol 5(2):611–647
Bouchama A, Knochel JP (2002) Heat stroke. N Engl J Med 346(1978–1988):2002
González-Alonso J, Quistorff B, Krustrup P, Bangsbo J, Saltin B (2000) Heat production in human skeletal muscle at the onset of intense dynamic exercise. J Physiol 524:603–615
Dong Q, Xiu Y, Wang Y et al (2022) HSF1 is a driver of leukemia stem cell self-renewal in acute myeloid leukemia. Nat Commun 13(1):6107
Dong Q et al (2022) HSF1 is a driver of leukemia stem cell self-renewal in acute myeloid leukemia. Nat Commun 13(1):6107
Zhang B et al (2021) Multifaceted roles of HSF1 in cell death: A state-of-the-art review. Biochim Biophys Acta Rev Cancer 1876(2):188591
Park SH et al (2020) Evaluation of the interaction between Bax and Hsp70 in cells by using a FRET system consisting of a fluorescent amino acid and YFP as a FRET pair. ChemBioChem 21(1–2):59–63
Watanabe K, Ohtsuki T (2021) Inhibition of HSF1 and SAFB granule formation enhances apoptosis induced by heat stress. Int J Mol Sci 22(9):4982
Li W et al (2023) MicroRNA-217 aggravates breast cancer through activation of NF1-mediated HSF1/ATG7 axis and c-Jun/ATF3/MMP13 axis. Hum Cell 36(1):377–392
Granato M, Gilardini Montani MS, Angiolillo C, D'Orazi G, Faggioni A, Cirone M (2018) Cytotoxic Drugs Activate KSHV Lytic Cycle in Latently Infected PEL Cells by Inducing a Moderate ROS Increase Controlled by HSF1, NRF2 and p62/SQSTM1. Viruses 11(1):8
Wang B et al (2022) Ferroptosis-related biomarkers for Alzheimer’s disease: Identification by bioinformatic analysis in hippocampus. Front Cell Neurosci 16:1023947
Zuo C et al (2022) Nrf2: An all-rounder in depression. Redox Biol 58:102522
Mahanty A, Mohanty S, Mohanty BP (2017) Dietary supplementation of curcumin augments heat stress tolerance through upregulation of nrf-2-mediated antioxidative enzymes and hsps in Puntius sophore. Fish Physiol Biochem 43(4):1131–1141
Wang Y et al (2021) S-allyl cysteine ameliorates heat stress-induced oxidative stress by activating Nrf2/HO-1 signaling pathway in BMECs. Toxicol Appl Pharmacol 416:115469
Du D et al (2022) Camel whey protein alleviates heat stress-induced liver injury by activating the Nrf2/HO-1 signaling pathway and inhibiting HMGB1 release. Cell Stress Chaperones 27(4):449–460
Paszek A et al (2020) Heat shock response regulates stimulus-specificity and sensitivity of the pro-inflammatory NF-kappaB signalling. Cell Commun Signal 18(1):77
Tang LP et al (2021) Heat stress inhibits expression of the cytokines, and NF-kappaB-NLRP3 signaling pathway in broiler chickens infected with salmonella typhimurium. J Therm Biol 98:102945
Liu YL et al (2022) Chronic heat stress promotes liver inflammation in broilers via enhancing NF-kappaB and NLRP3 signaling pathway. BMC Vet Res 18(1):289
Huang J et al (2022) beta-Hydroxybutyric acid attenuates heat stress-induced neuroinflammation via inhibiting TLR4/p38 MAPK and NF-kappaB pathways in the hippocampus. FASEB J 36(4):e22264
Huang W et al (2020) Heat stress induces RIP1/RIP3-dependent necroptosis through the MAPK, NF-kappaB, and c-Jun signaling pathways in pulmonary vascular endothelial cells. Biochem Biophys Res Commun 528(1):206–212
Xie W, Huang W, Cai S, Chen H, Fu W, Chen Z, Liu Y (2021) NF‑κB/IκBα signaling pathways are essential for resistance to heat stress‑induced ROS production in pulmonary microvascular endothelial cells. Mol Med Rep 24(5):814
Wang L et al (2023) Xuebijing injection attenuates heat stroke-induced brain injury through oxidative stress blockage and parthanatos modulation via PARP-1/AIF signaling. ACS Omega 8(37):33392–33402
Mota RA et al (2008) Poly(ADP-ribose) polymerase-1 inhibition increases expression of heat shock proteins and attenuates heat stroke-induced liver injury. Crit Care Med 36(2):526–534
Bertheloot D, Latz E, Franklin BS (2021) Necroptosis, pyroptosis and apoptosis: an intricate game of cell death. Cell Mol Immunol 18(5):1106–1121
O’Donnell MA et al (2007) Ubiquitination of RIP1 regulates an NF-kappaB-independent cell-death switch in TNF signaling. Curr Biol 17(5):418–424
Medema JP, Scaffidi C, Kischkel FC, Shevchenko A, Mann M, Krammer PH, Peter ME (1997) FLICE is activated by association with the CD95 death-inducing signaling complex (DISC). EMBO J 16(10):2794–2804. https://doi.org/10.1093/emboj/16.10.2794
Li Y et al (2019) Mitochondrial OXPHOS is involved in the protective effects of L-arginine against heat-induced low sperm motility of boar. J Therm Biol 84:236–244
Zhao F et al (2021) Melatonin alleviates heat stress-induced oxidative stress and apoptosis in human spermatozoa. Free Radic Biol Med 164:410–416
Zhu J et al (2022) Microglial exosomal miR-466i-5p induces brain injury via promoting hippocampal neuron apoptosis in heatstroke. Front Immunol 13:968520
Chen Y et al (2022) The role of microglial exosomes in brain injury. Front Cell Neurosci 16:1003809
King MA et al (2017) Unique cytokine and chemokine responses to exertional heat stroke in mice. J Appl Physiol (1985) 122(2):296–306
Yan W et al (2012) High-mobility group box 1 activates caspase-1 and promotes hepatocellular carcinoma invasiveness and metastases. Hepatology 55(6):1863–1875
Rathinam VAK, Zhao Y, Shao F (2019) Innate immunity to intracellular LPS. Nat Immunol 20(5):527–533
Newton K, Dixit VM, Kayagaki N (2021) Dying cells fan the flames of inflammation. Science 374(6571):1076–1080
Broz P, Pelegrin P, Shao F (2020) The gasdermins, a protein family executing cell death and inflammation. Nat Rev Immunol 20(3):143–157
Yuan J, Ofengeim D (2024) A guide to cell death pathways. Nat Rev Mol Cell Biol 25(5):379–395
Ding J et al (2016) Pore-forming activity and structural autoinhibition of the gasdermin family. Nature 535(7610):111–116
Geng Y et al (2015) Heatstroke induces liver injury via IL-1beta and HMGB1-induced pyroptosis. J Hepatol 63(3):622–633
Tong HS et al (2011) Early elevated HMGB1 level predicting the outcome in exertional heatstroke. J Trauma 71(4):808–814
Tong H et al (2013) HMGB1 activity inhibition alleviating liver injury in heatstroke. J Trauma Acute Care Surg 74(3):801–807
Pei Y et al (2023) Mesenchymal stem cell-derived exosomal miR-548x-3p inhibits pyroptosis of vascular endothelial cells through HMGB1 in heat stroke. Genomics 115(6):110719
Li Y et al (2020) Proteomic analysis of extracellular vesicles released from heat-stroked hepatocytes reveals promotion of programmed cell death pathway. Biomed Pharmacother 129:110489
Sims GP et al (2010) HMGB1 and RAGE in inflammation and cancer. Annu Rev Immunol 28:367–388
Lamkanfi M (2011) Emerging inflammasome effector mechanisms. Nat Rev Immunol 11(3):213–220
Newton K (2020) Multitasking kinase RIPK1 regulates cell death and inflammation. Cold Spring Harb Perspect Biol 12(3):a036368
Newton K et al (2019) Cleavage of RIPK1 by caspase-8 is crucial for limiting apoptosis and necroptosis. Nature 574(7778):428–431
Lalaoui N et al (2020) Mutations that prevent caspase cleavage of RIPK1 cause autoinflammatory disease. Nature 577(7788):103–108
Tao P et al (2020) A dominant autoinflammatory disease caused by non-cleavable variants of RIPK1. Nature 577(7788):109–114
Ai Y et al (2024) The biochemical pathways of apoptotic, necroptotic, pyroptotic, and ferroptotic cell death. Mol Cell 84(1):170–179
Li L, Tan H, Zou Z, Gong J, Zhou J, Peng N, Su L, Maegele M, Cai D, Gu Z (2020) Preventing necroptosis by scavenging ROS production alleviates heat stress-induced intestinal injury. Int J Hyperthermia 37(1):517–530. https://doi.org/10.1080/02656736.2020.1763483
Li L et al (2019) Ser46 phosphorylation of p53 is an essential event in prolyl-isomerase Pin1-mediated p53-independent apoptosis in response to heat stress. Cell Death Dis 10(2):96
He S et al (2019) Ferulic acid protects against heat stress-induced intestinal epithelial barrier dysfunction in IEC-6 cells via the PI3K/Akt-mediated Nrf2/HO-1 signaling pathway. Int J Hyperthermia 35(1):112–121
Yuan F, Cai J, Wu J, Tang Y, Zhao K, Liang F, Li F, Yang X, He Z, Billiar TR, Wang H, Su L, Lu B (2022) Z-DNA binding protein 1 promotes heatstroke-induced cell death. Science 376(6593):609–615. https://doi.org/10.1126/science.abg5251
Wang R et al (2020) Gut stem cell necroptosis by genome instability triggers bowel inflammation. Nature 580(7803):386–390
Zhang T et al (2020) Influenza virus Z-RNAs induce ZBP1-mediated necroptosis. Cell 180(6):1115-1129 e13
Jiao H et al (2020) Z-nucleic-acid sensing triggers ZBP1-dependent necroptosis and inflammation. Nature 580(7803):391–395
Kuriakose T, Kanneganti TD (2018) ZBP1: innate sensor regulating cell death and inflammation. Trends Immunol 39(2):123–134
Devos M, Tanghe G, Gilbert B, Dierick E, Verheirstraeten M, Nemegeer J, de Reuver R, Lefebvre S, De Munck J, Rehwinkel J, Vandenabeele P, Declercq W, Maelfait J (2020) Sensing of endogenous nucleic acids by ZBP1 induces keratinocyte necroptosis and skin inflammation. J Exp Med 217(7):e20191913
Jiang X, Stockwell BR, Conrad M (2021) Ferroptosis: mechanisms, biology and role in disease. Nat Rev Mol Cell Biol 22(4):266–282
Jenkins NL, James SA, Salim A, Sumardy F, Speed TP, Conrad M, Richardson DR, Bush AI, McColl G (2020) Changes in ferrous iron and glutathione promote ferroptosis and frailty in aging Caenorhabditis elegans. Elife 9:e56580
Chen X et al (2021) Broadening horizons: the role of ferroptosis in cancer. Nat Rev Clin Oncol 18(5):280–296
Carneiro BA, El-Deiry WS (2020) Targeting apoptosis in cancer therapy. Nat Rev Clin Oncol 17(7):395–417
Xie S et al (2021) Metabolic control by heat stress determining cell fate to ferroptosis for effective cancer therapy. ACS Nano 15(4):7179–7194
Kanno T et al (2021) Acsbg1-dependent mitochondrial fitness is a metabolic checkpoint for tissue T(reg) cell homeostasis. Cell Rep 37(6):109921
Luan Y et al (2023) Serum myoglobin modulates kidney injury via inducing ferroptosis after exertional heatstroke. J Transl Int Med 11(2):178–188
Karki R et al (2021) ADAR1 restricts ZBP1-mediated immune response and PANoptosis to promote tumorigenesis. Cell Rep 37(3):109858
Pandian N, Kanneganti TD (2022) PANoptosis: a unique innate immune inflammatory cell death modality. J Immunol 209(9):1625–1633
Zhu P et al (2023) Advances in mechanism and regulation of PANoptosis: Prospects in disease treatment. Front Immunol 14:1120034
Kayagaki N et al (2015) Caspase-11 cleaves gasdermin D for non-canonical inflammasome signalling. Nature 526(7575):666–671
Shi J et al (2015) Cleavage of GSDMD by inflammatory caspases determines pyroptotic cell death. Nature 526(7575):660–665
Sun L et al (2012) Mixed lineage kinase domain-like protein mediates necrosis signaling downstream of RIP3 kinase. Cell 148(1–2):213–227
Chen X et al (2014) Translocation of mixed lineage kinase domain-like protein to plasma membrane leads to necrotic cell death. Cell Res 24(1):105–121
Wu C et al (2019) Inflammasome activation triggers blood clotting and host death through pyroptosis. Immunity 50(6):1401-1411 e4
Yang X et al (2019) Bacterial endotoxin activates the coagulation cascade through gasdermin D-dependent phosphatidylserine exposure. Immunity 51(6):983-996 e6
Zheng M, Kanneganti TD (2020) The regulation of the ZBP1-NLRP3 inflammasome and its implications in pyroptosis, apoptosis, and necroptosis (PANoptosis). Immunol Rev 297(1):26–38
Zheng M et al (2020) Caspase-6 is a key regulator of innate immunity, inflammasome activation, and host defense. Cell 181(3):674-687 e13
Kayagaki N et al (2021) NINJ1 mediates plasma membrane rupture during lytic cell death. Nature 591(7848):131–136
Yamamoto K et al (2020) Autophagy promotes immune evasion of pancreatic cancer by degrading MHC-I. Nature 581(7806):100–105
Green DR (2019) The coming decade of cell death research: five riddles. Cell 177(5):1094–1107
Liu S et al (2023) Autophagy: Regulator of cell death. Cell Death Dis 14(10):648
Dokladny K, Myers OB, Moseley PL (2015) Heat shock response and autophagy–cooperation and control. Autophagy 11(2):200–213
Glick D, Barth S, Macleod KF (2010) Autophagy: cellular and molecular mechanisms. J Pathol 221(1):3–12
Hu JM et al (2021) Ethyl pyruvate ameliorates heat stroke-induced multiple organ dysfunction and inflammatory responses by induction of stress proteins and activation of autophagy in rats. Int J Hyperthermia 38(1):862–874
Kuo NC, Huang SY, Yang CY, Shen HH, Lee YM (2020) Involvement of HO-1 and autophagy in the protective effect of magnolol in hepatic steatosis-induced NLRP3 inflammasome activation in vivo and in vitro. Antioxidants (Basel) 9(10):924
Willot Q et al (2006) Exploring the connection between autophagy and heat-stress tolerance in Drosophila melanogaster. Proc Biol Sci 2023(290):20231305
Gohel R et al (2020) Molecular mechanisms of selective autophagy in Drosophila. Int Rev Cell Mol Biol 354:63–105
Zhao F et al (2016) Semen preparation methods and sperm telomere length: density gradient centrifugation versus the swim up procedure. Sci Rep 6:39051
Venn RM et al (1999) Preliminary UK experience of dexmedetomidine, a novel agent for postoperative sedation in the intensive care unit. Anaesthesia 54(12):1136–1142
Li B et al (2015) Anti-inflammatory effects of perioperative dexmedetomidine administered as an adjunct to general anesthesia: a meta-analysis. Sci Rep 5:12342
Zamani MM et al (2016) Survival benefits of dexmedetomidine used for sedating septic patients in intensive care setting: A systematic review. J Crit Care 32:93–100
Xia ZN et al (2017) Dexmedetomidine protects against multi-organ dysfunction induced by heatstroke via sustaining the intestinal integrity. Shock 48(2):260–269
Zhang J et al (2015) The effect of dexmedetomidine on inflammatory response of septic rats. BMC Anesthesiol 15:68
Zhang P et al (2017) Dexmedetomidine regulates 6-hydroxydopamine-induced microglial polarization. Neurochem Res 42(5):1524–1532
Li P et al (2021) Modulation of microglial phenotypes by dexmedetomidine through TREM2 reduces neuroinflammation in heatstroke. Sci Rep 11(1):13345
Zhang Y et al (2017) Dexmedetomidine may upregulate the expression of caveolin-1 in lung tissues of rats with sepsis and improve the short-term outcome. Mol Med Rep 15(2):635–642
Geng Y et al (2019) Dexmedetomidine attenuates acute lung injury induced by heatstroke and improve outcome. Shock 52(5):532–539
Klingensmith NJ, Coopersmith CM (2016) The gut as the motor of multiple organ dysfunction in critical illness. Crit Care Clin 32(2):203–212
Leon LR, Helwig BG (2010) Role of endotoxin and cytokines in the systemic inflammatory response to heat injury. Front Biosci (Schol Ed) 2(3):916–938. https://doi.org/10.2741/s111
Chi X et al (2015) Dexmedetomidine ameliorates acute lung injury following orthotopic autologous liver transplantation in rats probably by inhibiting Toll-like receptor 4-nuclear factor kappa B signaling. J Transl Med 13:190
Zhang X et al (2016) Sarcolemmal ATP-sensitive potassium channel protects cardiac myocytes against lipopolysaccharide-induced apoptosis. Int J Mol Med 38(3):758–766
Kataoka H et al (2017) Structural behavior of the endothelial glycocalyx is associated with pathophysiologic status in septic mice: an integrated approach to analyzing the behavior and function of the glycocalyx using both electron and fluorescence intravital microscopy. Anesth Analg 125(3):874–883
Kobayashi K et al (2018) Dexmedetomidine preserves the endothelial glycocalyx and improves survival in a rat heatstroke model. J Anesth 32(6):880–885
Kawasaki T et al (2014) Thrombomodulin improved liver injury, coagulopathy, and mortality in an experimental heatstroke model in mice. Anesth Analg 118(5):956–963
Zhang K et al (2022) Mesenchymal stem cell therapy: a potential treatment targeting pathological manifestations of traumatic brain injury. Oxid Med Cell Longev 2022:4645021
Das M et al (2019) Mesenchymal stem cell therapy for the treatment of traumatic brain injury: progress and prospects. Rev Neurosci 30(8):839–855
Brooks B, Ebedes D, Usmani A, Gonzales-Portillo JV, Gonzales-Portillo D, Borlongan CV (2022) Mesenchymal stromal cells in ischemic brain injury. Cells 11(6):1013
Ni XX et al (2020) Protective effects of hyperbaric oxygen therapy on brain injury by regulating the phosphorylation of Drp1 through ROS/PKC pathway in heatstroke rats. Cell Mol Neurobiol 40(8):1253–1269
Wu Q et al (2018) Mdivi-1 alleviates blood-brain barrier disruption and cell death in experimental traumatic brain injury by mitigating autophagy dysfunction and mitophagy activation. Int J Biochem Cell Biol 94:44–55
Lin PH et al (2021) Exertional heat stroke on fertility, erectile function, and testicular morphology in male rats. Sci Rep 11(1):3539
Chao CM et al (2023) Myocardial structure and functional alterations in a preclinical model of exertional heat stroke. Life Sci 323:121640
Hsieh KL et al (2024) Hyperbaric oxygen preconditioning normalizes scrotal temperature, sperm quality, testicular structure, and erectile function in adult male rats subjected to exertional heat injury. Mol Cell Endocrinol 584:112175
Luaces JP et al (2023) What do we know about blood-testis barrier? current understanding of its structure and physiology. Front Cell Dev Biol 11:1114769
Lian P, Braber S, Garssen J, Wichers HJ, Folkerts G, Fink-Gremmels J, Varasteh S (2020) Beyond heat stress: Intestinal integrity disruption and mechanism-based intervention strategies. Nutrients 12(3):734
Ortega ADSV, Szabó C (2021) Adverse effects of heat stress on the intestinal integrity and function of pigs and the mitigation capacity of dietary antioxidants: A review. Animals (Basel) 11(4):1135
Li ST et al (2018) Ulinastatin attenuates LPS-induced inflammation in mouse macrophage RAW264.7 cells by inhibiting the JNK/NF-kappaB signaling pathway and activating the PI3K/Akt/Nrf2 pathway. Acta Pharmacol Sin 39(8):1294–1304
Zhang H et al (2016) Preventive effects of ulinastatin on complications related to pancreaticoduodenectomy: A Consort-prospective, randomized, double-blind, placebo-controlled trial. Medicine (Baltimore) 95(24):e3731
Pan Y et al (2017) Ulinastatin ameliorates tissue damage of severe acute pancreatitis through modulating regulatory T cells. J Inflamm (Lond) 14:7
Tao Z et al (2017) Effect of ulinastatin, a human urinary protease inhibitor, on heatstroke-induced apoptosis and inflammatory responses in rats. Exp Ther Med 13(1):335–341
Tong Y et al (2014) Ulinastatin preconditioning attenuates inflammatory reaction of hepatic ischemia reperfusion injury in rats via high mobility group box 1(HMGB1) inhibition. Int J Med Sci 11(4):337–343
Na P, Yan G, Zhang S, Tang Y-Q, Qiang W, Yun-song L, Lei S (2015) Effects of ulinastatin on oxidative stress and renal injury in rats with severe heatstroke. Med J Chin PLA 05:354–357 (CNKI:SUN:JFJY.0.2015-05-004)
Zhou G, Xu Q, Liu Y, Wang Z, Su L, Guo X (2015) Protective effects of ulinastatin against acute lung injury induced by heatstroke in mice. Nan Fang Yi Ke Da Xue Xue Bao 35(9):1277–1282 (Chinese)
Kim SK et al (2019) Role of probiotics in human gut microbiome-associated diseases. J Microbiol Biotechnol 29(9):1335–1340
Bae JY et al (2018) Effects of Lactobacillus plantarum and Leuconostoc mesenteroides Probiotics on Human Seasonal and Avian Influenza Viruses. J Microbiol Biotechnol 28(6):893–901
Li L et al (2021) Preventive effects of Bacillus licheniformis on heat stroke in rats by sustaining intestinal barrier function and modulating gut microbiota. Front Microbiol 12:630841
Ogden HB, Child RB, Fallowfield JL, Delves SK, Westwood CS, Layden JD (2020) The gastrointestinal exertional heat stroke paradigm: Pathophysiology, assessment, severity, aetiology and nutritional countermeasures. Nutrients 12(2):537
Cai H et al (2023) Remodeling of gut microbiota by probiotics alleviated heat stroke-induced necroptosis in male germ cells. Mol Nutr Food Res 67(18):e2300291
Ding N et al (2020) Impairment of spermatogenesis and sperm motility by the high-fat diet-induced dysbiosis of gut microbes. Gut 69(9):1608–1619
Funding
This work was supported by grants from the Medical Science and Technology Projects in Guangdong [A2023269] and Science and Technology Projects in Guangzhou [2024A03J0640].
Author information
Ethics declarations
Ethic declaration
Not applicable.
Consent for publication
All authors reviewed the manuscript and approved the publication.
Competing interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Wang, Z., Zhu, J., Zhang, D. et al. The significant mechanism and treatments of cell death in heatstroke. Apoptosis 29, 967–980 (2024). https://doi.org/10.1007/s10495-024-01979-w
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10495-024-01979-w