Abstract
As a basic biological phenomenon of cells, regulated cell death (RCD) has irreplaceable influence on the occurrence and development of many processes of life and diseases. RCD plays an important role in the stability of the homeostasis, the development of multiple systems and the evolution of organisms. Thus comprehensively understanding of RCD is undoubtedly helpful in the innovation of disease treatment. Recently, research on the underlying mechanisms of the major forms of RCD, such as apoptosis, autophagy, necroptosis, pyroptosis, paraptosis and neutrophils NETosis has made significant breakthroughs. In addition, the interconnections among them have attracted increasing attention from global scholars in the field of life sciences. Here, recent advances in RCD research field are discussed.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
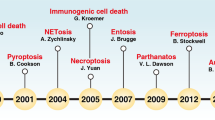
Regulated cell death (RCD) is an updated term for programmed cell death (PCD) recommended by the Nomenclature Committee on Cell Death (NCCD) in 2018 [1]. The concept of PCD was previously applied to all types of physiological cell death, including developmental and non-developmental processes needed to maintain health. When RCD occurs in strictly physiological conditions, it is also called as PCD. RCD is an important part of maintaining a stable intracellular environment and the survival of multicellular organisms. From the host's immune defense to the shaping of organs and tissues, RCD is the key to a series of important cellular processes during embryonic development. Researches on the RCD mechanisms have identified a large number of genes and pathways that positively or negatively control and influence RCD processes, thereby altering the course of life change to some extent. The terms apoptosis and PCD were once used interchangeably. However, it is well known that apoptosis is only one type of RCD along with the discovery of more and more forms of cell death. The major forms of RCD including apoptosis, pyroptosis, NETosis, necroptosis, autophagy, etc. are different in characteristics but they are inextricably linked. The insight into the network among them may become a breakthrough in the field of life science research.
Association between apoptotic and non-apoptotic regulated cell death
Apoptosis, the first PCD to be identified, is thought to be a non-inflammatory form of cell death and usually manifested as immunologically silent. Apoptosis is traditionally considered as a form of cell death independent of pyroptosis and autophagy etc. However, with the in-depth research on RCD, the connection between apoptosis and other forms of cell death was discovered. Previous studies have often focused on a single type of RCD, but many key proteins have been proven to trigger various RCDs under diverse regulation. People slowly began to realize that the interconnection between different kinds of RCD is very important because cell death is no longer an isolated process.
The caspase family links apoptosis and pyroptosis
Apoptosis, a mechanism that allows cells to self-destruct, is an active process which involves a series of gene activation, expression, regulation, etc. These genes which are very conservative among species strictly control the process of apoptosis. Inflammasome, a multiprotein cytoplasmic complex, is an innate immune mechanism that promotes inflammation by activating protease caspase-1. Activated caspase-1 can induce pyroptosis and promote the release of intracellular pro-inflammatory factors, including the cytokine IL-1 family. Recent studies have identified mediators of cell death related to inflammatory bodies and suggest that NLRP3 and AIM2 inflammasomes are not only involved in pyroptosis, but also in apoptosis [2]. Caspase-1, the key to the canonical inflammasome pathway of cell pyroptosis, has been reported to have the potential to induce apoptosis [3, 4]. Val-boroPro, a dipeptidyl peptidase (DPP) inhibitor, can induce caspase-1-dependent cell death and promote apoptosis in GSDMD-deficient cells RAW264.7 and THP-1 cells with accompanying caspase-3/-7 activation [3]. Pyroptosis is dominant in LPS plus nigericin- or Salmonella typhimurium-treated J774 cells and bone marrow-derived macrophages. However, apoptosis became obvious in gsdmd−/− cells [5]. In the absence of GSDMD, caspase-1 can activate caspase-3/-7 and cause apoptosis. Caspase-1 is involved in the activation of Bid while GSDMD has nothing to do with it in many disease models, which suggested caspase-1-induced apoptosis involves the Bid-caspase-9-caspase-3 axis. However, the rapid release of LDH was observed after the apoptosis of gsdmd-KO CL26-iCasp1 cells triggered by caspase-1. Caspase-3 can cleave Gasdermin E (GSDME, DFNA5) and mediate pyroptosis but this situation only exists in cell lines that highly express GSDME [4]. A study has done the opposite, observing the changes of GSDMD during apoptosis. It is found that caspase-3/-7 can also cleave GSDMD at a different site from inflammatory caspase that inactivates the protein, thereby specifically blocks the pyroptosis [3]. Caspase-3-induced cleavage of GSDME can promote pyroptosis of certain cancer cells expressing GSDME after chemotherapy. It is further confirmed that GSDME can convert caspase-3 mediated apoptosis induced by TNF or chemotherapy drugs into pyroptosis because GSDME can be specifically cleaved by caspase-3 in its connexin to generate GSDME-N fragments and perforate cell membrane, thereby inducing pyroptosis [6].
Caspase-8 may be involved in activating inflammasome during apoptosis. The genetic or pharmacological inactivation of endogenous apoptotic inhibitors (cIAP1, 2, XIAP, TAK1, IKK protein, etc.) sensitizes myeloid cells including macrophages, dendritic cells, and neutrophils to induce caspase-8 activation, promote cell lysis and activate NLRP3 inflammasomes in vitro, which results in an inflammatory response [7,8,9,10,11,12]. Emerging studies demonstrate that GSDMD played an important role in caspase-8-induced inflammation. GSDMD is processed into cleaved p30 fragments by two pathways. The first pathway involves directly cleavage of caspase-8-dependent GSDMD but can only be observed when caspase-8 is strongly activated [13]. The second pathway leading to the activation of GSDMD occurs through potassium efflux and the activation of NLRP3 inflammasome. However, the mechanism of caspase-8 driving NLRP3 inflammasome activation is still controversial [14]. The activation of caspase-8-dependent NLRP3 inflammasome requires pannexin-1, a channel-forming transmembrane glycoprotein. Caspase-8 promotes the activation of downstream executor caspase-3/-7, cleaves and activates pannexin-1 channel activity, membrane permeability and NLRP3 inflammasome activation and promotes cell lysis and inflammation [15] (Fig. 1).
Histone modification and ROS are associated with apoptosis and NETosis
The different forms of NETosis and their common terminal structure have been revealed recently. The formation of neutrophil extracelluar traps (NETs) is thought to be important in defending against microbial invasion. NETs usually contain DNA, modified histones and cytotoxic enzymes. Post-translational modifications (PTMs) of neutrophil histones play a key role in regulating neutrophil death. Histone citrullination has been shown to promote a form of NETs that does not depend on NADPH oxidase (NOX) but depends on calcium influx. Histone acetylation has a double-edged sword effect on NETosis. Histone deacetylase (HDAC) inhibitors, such as low concentrations of HDAC inhibitors (HDACis): belinostat (0.25 M) and panobinostat (0.04 M), can promote Histone acetylation (eg AcH4) and NOX-dependent or -independent NETosis. However, the increased levels of histone acetylation can inhibit NETosis and transform the neutrophil death into apoptosis [16, 17]. The histone-modified methods in NETs may play a two-way role because they can change many types of neutrophil death and affect lots of NETs-mediated diseases.
It is well established that increased levels of reactive oxygen species (ROS) will reduce the expression of anti-autophagic factor mTOR and anti-apoptotic gene Bcl-2, and increase the pro-autophagic genes (Dynein, Beclin-1 and LC3B) and pro-apoptotic factors (BAX, Fas, FasL, Caspase-3, Caspase-8 and Caspase-9) expression, thus promoting cell autophagy and apoptosis [18]. The detection of neutrophils in human peripheral blood and mouse abdominal cavity found that PRAK (p38-regulated/activated protein kinase) dysfunction leads to a significant reduction in the formation of NETs and an increase in the rate of apoptosis, and may lead to impaired antibacterial activity of NETs. The overproduction of ROS plays a central role in this process. In a low-oxygen environment, treatment with low-dose ROS will make the generation of NETs and the occurrence of apoptosis more uneven [19].
RIPK1 and caspase-8 are involved in the regulation of apoptosis, pyroptosis and necroptosis
Necroptosis was classically described as an unregulated cell death. However, genetic, biochemical, and functional evidence, as well as the discovery of caspase inhibitors, have redefined necroptosis as a form of molecularly controlled cell death. Necroptosis is a RCD induced by receptor interacting protein kinase 3 (RIPK3) and mixed lineage kinase domain like pseudokinase (MLKL). RIPK3 is activated in the upstream pathway through RIPK1, TRIF and ZBP1/DAI [20]. Necroptosis requires the implementation of RIPK3-dependent phosphorylated MLKL, which will subsequently cause cell death and destruction of the plasma membrane.
The investigations of genetically modified mouse model, clinical investigation as well as genetic and pharmacological inhibition revealed that RIPK1 is the hub of apoptosis and necroptosis signaling pathways and has kinase-dependent or kinase-independent functions. These functions are all very important for regulation of cell survival, regulated cell death and inflammation [21,22,23,24,25]. Numerous studies have shown that ubiquitination of RIPK1 with lysine 11 (K11), M1(linear), K63 and K48 ubiquitin chains regulates its function by preventing the formation of death-inducing protein complexes and promoting its pro-survival effect in TNFR1 signaling complex [20]. In addition to ubiquitination, various phosphorylation pathways are also involved in the regulation of RIPK1 function. RIPK1 can be phosphorylated by MK2, TAK1 and IKKs [9, 26, 27]. The activation of RIPK1 kinase is inhibited by mutating serine 25 of RIPK1 to glutamic acid to simulate phosphorylation, which protects cells from TNFR1-mediated cell death and inflammation. RIPK1 ubiquitination and phosphorylation can inhibit the activation of RIPK1 kinase activity, which will prevent apoptosis and necroptosis [20]. There may also be a link between cell pyroptosis and necroptosis. NLRP3 plays a major role in pyroptosis while RIPK3 and its substrate MLKL are essential for necroptosis. There is a link between RIPK3-MLKL-induced necroptosis and NLRP3 inflammasome activation. After LPS treatment of bone marrow-derived macrophages (BMDM) or LPS-induced necroptosis, the TLR adapter protein TRIF and apoptotic inhibitor protein XIAPs can regulate RIPK3 and MLKL ubiquitination. The addition of LPS or TNF to BMDM lacking IAPs will promote the formation of ripoptosome and the activation of RIPK3-dependent caspase-8 after treatment with IAP antagonist compounds or genetic deletion, which activates NLRP3 inflammasome and produce strong pro-inflammatory factors IL-1β [28]. Lack of caspase-8 in the presence or absence of RIPK3 will inhibit the process of NLRP3 inflammasome activating caspase-1 and caspase-11 but will not inhibit NLRC4 inflammasome, which indicates that caspase-8 can mediate the initiation and activation of NLRP3 inflammasome in both the canonical and the non-canonical inflammasome pathways of pyroptosis. Treatment of caspase-8−/− mice with LPS or Citrobacter rodentium will impair the production of IL-1β, which suggests caspase-8 plays a role in necroptosis and pyroptosis [29].
Caspase-8 has been reported that can mediate the switching between different modes of RCD. Catalytically inactivate caspase-8 is the nucleation signal of ASC spot formation and activation of caspase-1. Caspase-8 eventually leads to premature death of mice when necroptosis is blocked, which reveals the enzymatic activity of caspase-8 and scaffold function have previously unknown and unanticipated effects, including the activation of inflammasome and induction of pyroptosis under situations in which apoptosis and necroptosis are suppressed. The ability of caspase-8 scaffolds to induce pyroptosis is limited to specific cell types, such as bone marrow cells and IECs. Caspase-8 is often reported to interact with the caspase-1 ASC adapter complex and promote the self-assembly of ASC, especially during bacterial infections. Virus is heavily dependent on the fate of infected cells and has evolved to encode apoptosis inhibitors that suppress caspase-8 and necroptosis inhibitors that suppress RHIM-containing proteins (such as RIPK1 and RIPK3) [30].
Co-regulation of apoptosis and autophagy
Autophagy and apoptosis are thought to jointly regulate the process of cell death. Autophagy promotes apoptosis by degrading anti-apoptotic factors and cell survival factors. In rat hippocampal astrocytes, degradation of caveolin-1 by autophagy can lead to apoptosis induced by palmitic acid [31]. Fap-1 is a fas-mediated apoptosis inhibitor. Type I cells become sensitive to fas-induced apoptosis when Fap-1 is degraded by autophagy [32]. Atg12 and Atg3 are important components of the ubiquitin-like binding mechanism necessary for the formation of autophagy. However, the binding of Atg12 to Atg3 neither occur in the process of starvation-induced autophagy, nor occur in Atg8 lipidation. It occurs in the process of mitochondrial-mediated apoptosis [33]. The Atg12-5 conjugate is required for autophagy. Atg5 is cleaved by caplains, cystein proteases activated by cellular stress, and plays a key role in the initiation of apoptosis. After Atg5 is cleaved, the N-terminus of Atg5 is translocated to mitochondria, where it interacts with Bcl-XL to mediate the release of cytochrome C and promote apoptosis [34].
Bcl-2 and Beclin-1 are considered to be related components of apoptosis and autophagy. Under normal physiological conditions, the interaction of Bcl-2 with Beclin-1 and Bax inhibits autophagy and apoptosis [35] (Fig. 2). Beclin-1 is necessary in macrophages and fibroblasts to promote the synthesis of actin and membrane phospholipids during the phagocytosis of apoptotic cells. Beclin-1 knockdown will lead to a decrease in the internalization of apoptotic cells. Under the conditions of autophagy induction, BH3 protein (whether Bik, Bad or Nova) competitively binds to Bcl-2 and replaces Beclin-1 [36]. This substitution is enhanced by JNK1 phosphorylation of Bcl-2, thereby promoting cell autophagy. Since Bcl-2 has a higher affinity for Bax than Beclin-1, the low level of phosphorylation of Bcl-2 is insufficient to separate it from mitochondrial Bax. The pressure signal will promote apoptosis when it becomes very strong and requires Bcl-2 hyperphosphorylation [37]. Caspases-3 and caspase-8 are also involved. They cleave PI3K members (Vps34 and Beclin-1) and Atg3 respectively, change the homeostasis of the cell and promote autophagy to apoptosis [34]. However, Bcl-2 family members have also been reported to affect autophagy indirectly by inhibiting BAX and BAK1 activation only. This is a controversial and challenging issue that will further our understanding of PCD [36, 38]. Autophagy activated by Rapamycin (Rapa) can inhibit apoptosis while chloroquine inhibiting autophagy can significantly enhance the apoptosis induced by T-2 toxin, a mycotoxin generated by Fusarium species [39].
MAPK and p53 may connect apoptosis and paraptosis
Paraptosis, a caspase-independent regulated cell death, is mainly characterized by extensive cytoplasmic vacuolization, swelling of endoplasmic reticulum (ER) and mitochondrial swelling [40]. MAPK and p53 may have a relationship between apoptosis and paraptosis. p53 is a tumor suppressor that controls cell proliferation and apoptosis as well as involving in non-apoptotic cell death. p53 influences non-canonical forms of cell death through transcriptional regulation of its downstream targets and direct interactions with key factors involved in these mechanisms, in a cell-type or tissue-environment dependent manner [41]. Ginsenoside Rh2, one of the active components of ginseng, possesses a p53-dependent pathway for apoptosis and paraptosis to induce cell death [42].
Paratosis is generally believed to be mediated by ROS-mediated endoplasmic reticulum stress and MAPK activation. The MAPK signaling pathway will be activated to promote paraptosis when p53 is lacking. Apoptosis and paraptosis often occur together during MAPK activation. The formation of paraptosis is even more obvious when apoptosis is inhibited. Fusaric acid (FA), a kind of food-derived mycotoxin, had been used to treat human peripheral blood mononuclear cells (PMBCs) and THP-1 cells. FA induced paraptosis in PMBCs, but induced apoptosis in THP-1 cells. In PBMCs, FA significantly up-regulated the MAPK protein expression of p-ERK and p-JNK while down-regulated the expression of p-p38. In THP-1 cells, FA up-regulated the MAPK protein expression of p-ERK and down-regulated the expression of p-JNK and p-p38. It is speculated that there may be a switch for regulating paraptosis and apoptosis but it still needs to be further verified [43].
Association between different kinds of non-apoptotic regulated cell death
After apoptosis, a large number of kinds of non-apoptotic RCD were found, such as pyroptosis, NETosis and autophagy. Non-apoptotic RCD has specific characteristics in regulating cell death and play an important role in the process. Cell death seems to be a basic process regulated by a variety of interrelated RCDs, therefore, the interaction between different kinds of non-apoptotic RCD has also garnered much attention.
GSDMD links pyroptosis and NETosis
Macrophages and neutrophils are important components of host innate immunity. When neutrophils quickly move into the site of infection or tissue damage, they remain in the blood for only 6–12 h. After remaining in the blood for several days, monocytes migrate to tissues and differentiate into wandering or stationary macrophages. Phagocytes can engulf and kill most kinds of pathogens, release a variety of cytokines and trigger an inflammatory response, which is closely related to the RCD processes. Pyroptosis, a highly inflammatory form of RCD, occurs most frequently upon infection with intracellular pathogens. It is characterized by the continuous expansion of cells until the cell membrane ruptures, which eventually leads to the release of cell contents and a large number of pro-inflammatory factors closely related to inflammation. NETosis is a special form of neutrophil death characterized by the release of chromatin and granular material into the extracellular space, a structure that can capture and kill a variety of bacterial, fungal and protozoan pathogens. NETosis is critical for the host's defense against extracellular pathogens while pyroptosis provides efficient and effective defense against intracellular pathogens. Several studies found that pyroptosis and NETosis are interlinked by Gasdermin D (GSDMD) [44, 45]. GSDMD, the substrate of inflammasome-associated caspase, has the ability to induce PCD and inflammation during the inflammasome signal transduction and pyroptosis. When GSDMD is cleaved by caspase, the N-terminal domain of GSDMD which has the ability to form pores in cell membrane is activated and promotes the release of NETs or inflammatory cytokines [46, 47]. GSDMD can not only make intracellular sodium–potassium concentration lose balance, but also induce the release of cytokines. In addition, GSDMD is related to the activation of inflammasome-associated caspase [48, 49]. The causation of pyroptosis mainly includes canonical inflammasome pathway and non-canonical inflammasome pathway and GSDMD plays a key role in both of them. There are reports indicating that neutrophils exposure to lipopolysaccharide (LPS) or Gram-negative bacteria (Salmonella and Citrobacter rodentium) activate non-canonical (caspase-4/-11) inflammasome signaling pathways and trigger GSDMD-dependent cell death. This way of cell death will induce neutrophils to release NETs and promote the process of NETosis [44]. Neutrophil elastase (NE), myeloperoxidase (MPO) and PAD4, three key enzymes in the formation of NETosis, are associated with histone inactivation and chromatin depolymerization in the early stages of NETosis caused by specific stimuli [50,51,52]. However, NE, MPO and PAD4 are dispensable in the formation of caspase-11-dependent NETs, which suggests that caspase-11 and GSDMD may directly induce the formation of NETosis [15, 44]. The N-terminal of caspase-cleaved GSDMD perforates the membrane fraction of macrophages and that it causes pyroptosis. However, the cleavage and activation of GSDMD can also be mediated by a neutrophil-specific serine protease in neutrophils [45, 53]. It has been well documented that a high concentration of neutrophil serine protease is transferred from neutrophilic cyan granules to the nucleus in the early stages of NETosis, which causes nuclear membrane damage prior to cell rupture. In such a case, the cleaved GSDMD may preferently destroy the nuclear membrane and that cause NETosis [45, 50, 54] (Fig. 3).
Pyroptosis is negatively regulated by autophagy
Autophagy is a process in which cells use lysosomes to degrade their damaged organelles and foreign bodies under the control of autophagy-related genes (Atgs). The pro-inflammatory cytokine IL-1β has been shown to have at least two secretion mechanisms. One is secretory autophagy and the other is pore formation mediated by the gasdermin family [55]. Extremely hungry macrophages secrete IL-1β in an autophagy-dependent manner when inflammation is activated [56]. Autophagy caused by starvation or pharmacological effects can promote the secretion of inflammasome-dependent IL-1β, IL-18 and HMGB1. Lysosomal damage may also be involved in the secretion of IL-1β. Lysosomal damage can be caused by silica, monosodium urate crystal and polymer precursor, which accumulate in lysosomes, destroy lysosomal membranes as well as activate autophagy and inflammasome [57, 58]. Due to the close relationship between autophagy and inflammatory response, the gasdermin pore-dependent release of IL-1β may be correlated with secretory autophagy pathway [55].
Treatment of human umbilical vein endothelial cells (HUVECs) with acrolein can induce ROS generation, autophagy, pyroptosis and reduce cell migration. Acrolein treatment of HUVECs activates NLRP3 inflammasome, promotes caspase-1 activation and induces downstream mature IL-1β and IL-18 secretion. 3-methyladenine (3-MA), an autophagy inhibitor, can make the above phenomenon more obvious. Rapa, an autophagy agonist, will have a reverse effect under acrolein stress. Knockdown of NLRP3 using siRNA can significantly inhibit acrolein-induced pyroptosis and increase cell migration rate. Removal of ROS will inhibit the activation of NLRP3 inflammasome and reduce apoptosis and pyroptosis [59]. ROS can also induce pyroptosis of nucleus pulposus cells (NPCs). However, with the increase of ROS level, the autophagy of NPCs increases and inhibits pyroptosis [60]. The authors speculate that pyroptosis is negatively regulated by autophagy.
The key role of NLRP3 inflammasome in autophagy of HCC cells was found by the study of 17β-estradiol (E2)-induced activation of NLRP3 inflammasome. NLRP3 inflammasome inhibited autophagy through e2-ERβ-AMPK-mTOR pathway and the positive changes of caspase-1 and PI were detected by flow cytometry, which confirmed to the interaction between pyroptosis and autophagy. E2-induced pyroptosis was significantly increased by 3-MA treatment while treatment with caspase-1 inhibitor YVAD-cmk prevented the phenomenon after 3-MA treatment, which indicates that caspase-1-dependent pyroptosis was negatively regulated by autophagy. In conclusion, E2-induced activation of NLRP3 inflammasome can be used as an inhibitor of HCC cell cycle processes because it triggers pyroptosis and inhibits autophagy [61].
Autophagy induces the generation of NETosis
Autophagy and NETosis were thought to be independent biological processes. When wortmannin, a PI3K inhibitor, was found to inhibit neutrophil autophagy and impair the formation of NETs, the association between autophagy and NETs was formally noticed [62]. Selective autophagy is indirect evidence for the cause of NETosis because the lack of an important regulator of selective autophagy Wdfy3 significantly decreased ROS and NETs in neutrophils [63]. Both ROS and autophagy have a role in NETosis [62]. NETosis caused by near infrared laser irradiation can also be mediated by oxidative stress and autophagy. The key to PMA-induced NETosis is ROS and autophagy [64, 65]. Selective autophagy is the main cause of NETosis because neutrophils which lack Wdfy3 (an important regulator of selective autophagy) result in a significant decrease in intracellular ROS and NETs [63]. mTOR regulates NETosis driven by autophagy because it can promote the formation of NETs through post-transcriptional control of hypoxia-inducible factor 1α (HIF-1α) [66]. However, subsequent studies have shown that activation of the mTOR pathway will down-regulate the formation of NETs [67]. The inhibition of NETosis may be caused by the interruption of the autophagy process of histone citrullination. Rapa, a pharmacological inhibitor of mTOR, has been shown to promote NETosis and induce the release of HIF-1α by inhibiting the mTOR pathway to activate autophagy. Rapa can increase autophagy activity and accelerate the release of NETs [68]. Treatment of peripheral blood neutrophils (PBNs) with IL-8 can strongly induce autophagy and the generation of NETs in PBNs, but the mechanism remains to be studied [69]. Neutrophils from patients with systemic lupus erythematosus (SLE) showed an increase in autophagy levels, which was accompanied by an increase in the release of NETs. The production of NETosis of neutrophils in patients with SLE is related to the increased expression of the stress response protein REDD1. Endothelin-1 (ET-1) and HIF-1α are the key to REDD1 driving NETs [70]. However, excessive inhibition or activation of autophagy can lead to its original dysfunction and loss, which needs further independent studies to verify [71].
Conclusion
RCD, a mechanism of living organisms, has multiple uses in the body and can cause defective and potentially harmful cells to self-destruct. There are still a lot of exploreable parts in the connection between several distinct RCD mechanisms. It has always been a subject that people desperately hope to solve. The connections among the major forms of RCD, whether they are mutual promotion/antagonism, unidirectional promotion/antagonism, or promotion of antagonistic coexistence, have played a vital role in the life process. With the in-depth exploration of the interconnections among RCD, deciphering the secrets of RCD will help to broaden effective therapies and yield many new surprises.
References
Galluzzi L, Vitale I, Aaronson SA et al (2018) Molecular mechanisms of cell death: recommendations of the Nomenclature Committee on Cell Death 2018. Cell Death Differ 25(3):486–541. https://doi.org/10.1038/s41418-017-0012-4
Tsuchiya K (2020) Inflammasome-associated cell death: pyroptosis, apoptosis, and physiological implications. Microbiol Immunol 64(4):252–269. https://doi.org/10.1111/1348-0421.12771
Taabazuing CY, Okondo MC, Bachovchin DA (2017) Pyroptosis and apoptosis pathways engage in bidirectional crosstalk in monocytes and macrophages. Cell Chem Biol 24(4):507–514. https://doi.org/10.1016/j.chembiol.2017.03.009
Tsuchiya K, Nakajima S, Hosojima S et al (2019) Caspase-1 initiates apoptosis in the absence of gasdermin D. Nat Commun 10(1):2091. https://doi.org/10.1038/s41467-019-09753-2
He WT, Wan H, Hu L et al (2015) Gasdermin D is an executor of pyroptosis and required for interleukin-1β secretion. Cell Res 25(12):1285–1298. https://doi.org/10.1038/cr.2015.139
Wang Y, Gao W, Shi X et al (2017) Chemotherapy drugs induce pyroptosis through caspase-3 cleavage of a gasdermin. Nature 547(7661):99–103. https://doi.org/10.1038/nature22393
Vince JE, Wong WW, Gentle I et al (2012) Inhibitor of apoptosis proteins limit RIP3 kinase-dependent interleukin-1 activation. Immunity 36(2):215–227. https://doi.org/10.1016/j.immuni.2012.01.012
Yabal M, Müller N, Adler H et al (2014) XIAP restricts TNF- and RIP3-dependent cell death and inflammasome activation. Cell Rep 7(6):1796–1808. https://doi.org/10.1016/j.celrep.2014.05.008
Dondelinger Y, Jouan-Lanhouet S, Divert T et al (2015) NF-κB-independent role of IKKα/IKKβ in preventing RIPK1 kinase-dependent apoptotic and necroptotic cell death during TNF signaling. Mol Cell 60(1):63–76. https://doi.org/10.1016/j.molcel.2015.07.032
Lawlor KE, Feltham R, Yabal M et al (2017) XIAP loss triggers RIPK3- and caspase-8-driven IL-1β activation and cell death as a consequence of TLR-MyD88-induced cIAP1-TRAF2 degradation. Cell Rep 20(3):668–682. https://doi.org/10.1016/j.celrep.2017.06.073
Chen KW, Lawlor KE, von Pein JB et al (2018) Cutting edge: blockade of inhibitor of apoptosis proteins sensitizes neutrophils to TNF- but not lipopolysaccharide-mediated cell death and IL-1β secretion. J Immunol 200(10):3341–3346. https://doi.org/10.4049/jimmunol.1701620
Wicki S, Gurzeler U, Wei-Lynn Wong W, Jost PJ, Bachmann D, Kaufmann T (2016) Loss of XIAP facilitates switch to TNFα-induced necroptosis in mouse neutrophils. Cell Death Dis 7(10):e2422. https://doi.org/10.1038/cddis.2016.311
Chen KW, Demarco B, Heilig R et al (2019) Extrinsic and intrinsic apoptosis activate pannexin-1 to drive NLRP3 inflammasome assembly. EMBO J 38(10):e101638
Conos SA, Chen KW, De Nardo D et al (2017) Active MLKL triggers the NLRP3 inflammasome in a cell-intrinsic manner. Proc Natl Acad Sci USA 114(6):E961–E969. https://doi.org/10.1073/pnas.1613305114
Chen KW, Demarco B, Broz P (2020) Beyond inflammasomes: emerging function of gasdermins during apoptosis and NETosis. EMBO J 39(2):e103397
Hamam HJ, Palaniyar N (2019) Post-translational modifications in NETosis and NETs-mediated diseases. Biomolecules 9(8):369. https://doi.org/10.3390/biom9080369
Hamam HJ, Palaniyar N (2019) Histone deacetylase inhibitors dose-dependently switch neutrophil death from NETosis to apoptosis. Biomolecules 9(5):184. https://doi.org/10.3390/biom9050184
Yirong C, Shengchen W, Jiaxin S, Shuting W, Ziwei Z (2020) DEHP induces neutrophil extracellular traps formation and apoptosis in carp isolated from carp blood via promotion of ROS burst and autophagy. Environ Pollut 262:114295. https://doi.org/10.1016/j.envpol.2020.114295
Wang Y, Wang Y, Wu J et al (2019) PRAK is required for the formation of neutrophil extracellular traps. Front Immunol 10:1252. https://doi.org/10.3389/fimmu.2019.01252
Schwarzer R, Laurien L, Pasparakis M (2020) New insights into the regulation of apoptosis, necroptosis, and pyroptosis by receptor interacting protein kinase 1 and caspase-8. Curr Opin Cell Biol 63:186–193. https://doi.org/10.1016/j.ceb.2020.02.004
O'Donnell JA, Lehman J, Roderick JE et al (2018) Dendritic cell RIPK1 maintains immune homeostasis by preventing inflammation and autoimmunity. J Immunol 200(2):737–748. https://doi.org/10.4049/jimmunol.1701229
Newton K, Wickliffe KE, Maltzman A et al (2016) RIPK1 inhibits ZBP1-driven necroptosis during development. Nature 540(7631):129–133. https://doi.org/10.1038/nature20559
Lin J, Kumari S, Kim C et al (2016) RIPK1 counteracts ZBP1-mediated necroptosis to inhibit inflammation. Nature 540(7631):124–128. https://doi.org/10.1038/nature20558
Takahashi N, Vereecke L, Bertrand MJ et al (2014) RIPK1 ensures intestinal homeostasis by protecting the epithelium against apoptosis. Nature 513(7516):95–99. https://doi.org/10.1038/nature13706
Rickard JA, O'Donnell JA, Evans JM et al (2014) RIPK1 regulates RIPK3-MLKL-driven systemic inflammation and emergency hematopoiesis. Cell 157(5):1175–1188. https://doi.org/10.1016/j.cell.2014.04.019
Dondelinger Y, Delanghe T, Rojas-Rivera D et al (2017) MK2 phosphorylation of RIPK1 regulates TNF-mediated cell death. Nat Cell Biol 19(10):1237–1247. https://doi.org/10.1038/ncb3608
Geng J, Ito Y, Shi L et al (2017) Regulation of RIPK1 activation by TAK1-mediated phosphorylation dictates apoptosis and necroptosis. Nat Commun 8(1):359. https://doi.org/10.1038/s41467-017-00406-w
Lawlor KE, Khan N, Mildenhall A et al (2015) RIPK3 promotes cell death and NLRP3 inflammasome activation in the absence of MLKL. Nat Commun 6:6282. https://doi.org/10.1038/ncomms7282
Gurung P, Anand PK, Malireddi RK et al (2014) FADD and caspase-8 mediate priming and activation of the canonical and noncanonical Nlrp3 inflammasomes. J Immunol 192(4):1835–1846. https://doi.org/10.4049/jimmunol.1302839
Fritsch M, Günther SD, Schwarzer R et al (2019) Caspase-8 is the molecular switch for apoptosis, necroptosis and pyroptosis. Nature 575(7784):683–687. https://doi.org/10.1038/s41586-019-1770-6
Chen Z, Nie SD, Qu ML et al (2018) The autophagic degradation of Cav-1 contributes to PA-induced apoptosis and inflammation of astrocytes. Cell Death Dis 9(7):771. https://doi.org/10.1038/s41419-018-0795-3
Gump JM, Staskiewicz L, Morgan MJ, Bamberg A, Riches DW, Thorburn A (2014) Autophagy variation within a cell population determines cell fate through selective degradation of Fap-1. Nat Cell Biol 16(1):47–54. https://doi.org/10.1038/ncb2886
Doherty J, Baehrecke EH (2018) Life, death and autophagy. Nat Cell Biol 20(10):1110–1117. https://doi.org/10.1038/s41556-018-0201-5
Cooper KF (2018) Till death do us part: the marriage of autophagy and apoptosis. Oxid Med Cell Longev 2018:4701275. https://doi.org/10.1155/2018/4701275
Maiuri MC, Criollo A, Kroemer G (2010) Crosstalk between apoptosis and autophagy within the Beclin 1 interactome. EMBO J 29(3):515–516. https://doi.org/10.1038/emboj.2009.377
Lindqvist LM, Heinlein M, Huang DC, Vaux DL (2014) Prosurvival Bcl-2 family members affect autophagy only indirectly, by inhibiting Bax and Bak. Proc Natl Acad Sci U S A 111(23):8512–8517. https://doi.org/10.1073/pnas.1406425111
Bassik MC, Scorrano L, Oakes SA, Pozzan T, Korsmeyer SJ (2004) Phosphorylation of BCL-2 regulates ER Ca2+ homeostasis and apoptosis. EMBO J 23(5):1207–1216. https://doi.org/10.1038/sj.emboj.7600104
Lindqvist LM, Vaux DL (2014) BCL2 and related prosurvival proteins require BAK1 and BAX to affect autophagy. Autophagy 10(8):1474–1475. https://doi.org/10.4161/auto.29639
Wu J, Zhou Y, Yuan Z et al (2019) Autophagy and apoptosis interact to modulate T-2 toxin-induced toxicity in liver cells. Toxins (Basel) 11(1):45. https://doi.org/10.3390/toxins11010045
Kroemer G, Galluzzi L, Vandenabeele P, Abrams J et al (2009) Classification of cell death: recommendations of the nomenclature committee on cell death 2009. Cell Death Differ 16(1):3–11. https://doi.org/10.1038/cdd.2008.150
Sodrul IMD, Wang C, Chen X, Du J, Sun H (2017) Role of ginsenosides in reactive oxygen species-mediated anticancer therapy. Oncotarget 9(2):2931–2950
Ranjan A, Iwakuma T (2016) Non-canonical cell death induced by p53. Int J Mol Sci 17(12):2068. https://doi.org/10.3390/ijms17122068
Dhani S, Nagiah S, Naidoo DB, Chuturgoon AA (2017) Fusaric acid immunotoxicity and MAPK activation in normal peripheral blood mononuclear cells and Thp-1 cells. Sci Rep 7(1):3051. https://doi.org/10.1038/s41598-017-03183-0
Chen KW, Monteleone M, Boucher D et al (2018) Noncanonical inflammasome signaling elicits gasdermin D-dependent neutrophil extracellular traps. Sci Immunol 3(26):eaar6676. https://doi.org/10.1126/sciimmunol.aar6676
Sollberger G, Choidas A, Burn GL et al (2018) Gasdermin D plays a vital role in the generation of neutrophil extracellular traps. Sci Immunol 3(26):eaar6689. https://doi.org/10.1126/sciimmunol.aar6689
Kuang S, Zheng J, Yang H et al (2017) Structure insight of GSDMD reveals the basis of GSDMD autoinhibition in cell pyroptosis. Proc Natl Acad Sci USA 114(40):10642–10647. https://doi.org/10.1073/pnas.1708194114
Shi J, Gao W, Shao F (2017) Pyroptosis: gasdermin-mediated programmed necrotic cell death. Trends Biochem Sci 42(4):245–254. https://doi.org/10.1016/j.tibs.2016.10.004
Feng S, Fox D, Man SM (2018) Mechanisms of gasdermin family members in inflammasome signaling and cell death. J Mol Biol 430(18PtB):3068–3080. https://doi.org/10.1016/j.jmb.2018.07.002
Kovacs SB, Miao EA (2017) Gasdermins: effectors of pyroptosis. Trends Cell Biol 27(9):673–684. https://doi.org/10.1016/j.tcb.2017.05.005
Papayannopoulos V, Metzler KD, Hakkim A, Zychlinsky A (2010) Neutrophil elastase and myeloperoxidase regulate the formation of neutrophil extracellular traps. J Cell Biol 191(3):677–691. https://doi.org/10.1083/jcb.201006052
Li P, Li M, Lindberg MR, Kennett MJ, Xiong N, Wang Y (2010) PAD4 is essential for antibacterial innate immunity mediated by neutrophil extracellular traps. J Exp Med 207(9):1853–1862. https://doi.org/10.1084/jem.20100239
Kenny EF, Herzig A, Krüger R et al (2017) Diverse stimuli engage different neutrophil extracellular trap pathways. Elife 6:e24437. https://doi.org/10.7554/eLife.24437
Kambara H, Liu F, Zhang X et al (2018) Gasdermin D exerts anti-inflammatory effects by promoting neutrophil death. Cell Rep 22(11):2924–2936. https://doi.org/10.1016/j.celrep.2018.02.067
Metzler KD, Goosmann C, Lubojemska A, Zychlinsky A, Papayannopoulos V (2014) A myeloperoxidase-containing complex regulates neutrophil elastase release and actin dynamics during NETosis. Cell Rep 8(3):883–896. https://doi.org/10.1016/j.celrep.2014.06.044
Claude-Taupin A, Bissa B, Jia J, Gu Y, Deretic V (2018) Role of autophagy in IL-1β export and release from cells. Semin Cell Dev Biol 83:36–41. https://doi.org/10.1016/j.semcdb.2018.03.012
Dupont N, Jiang S, Pilli M, Ornatowski W, Bhattacharya D, Deretic V (2011) Autophagy-based unconventional secretory pathway for extracellular delivery of IL-1β. EMBO J 30(23):4701–4711. https://doi.org/10.1038/emboj.2011.398
Ito M, Shichita T, Okada M et al (2015) Bruton's tyrosine kinase is essential for NLRP3 inflammasome activation and contributes to ischaemic brain injury. Nat Commun 6:7360. https://doi.org/10.1038/ncomms8360
Maejima I, Takahashi A, Omori H et al (2013) Autophagy sequesters damaged lysosomes to control lysosomal biogenesis and kidney injury. EMBO J 32(17):2336–2347. https://doi.org/10.1038/emboj.2013.171
Jiang C, Jiang L, Li Q et al (2018) Acrolein induces NLRP3 inflammasome-mediated pyroptosis and suppresses migration via ROS-dependent autophagy in vascular endothelial cells. Toxicology 410:26–40. https://doi.org/10.1016/j.tox.2018.09.002
Bai Z, Liu W, He D et al (2020) Protective effects of autophagy and NFE2L2 on reactive oxygen species-induced pyroptosis of human nucleus pulposus cells. Aging (Albany NY) 12(8):7534–7548
Wei Q, Zhu R, Zhu J, Zhao R, Li M (2019) E2-induced activation of the NLRP3 inflammasome triggers pyroptosis and inhibits autophagy in HCC cells. Oncol Res 27(7):827–834. https://doi.org/10.3727/096504018X15462920753012
Remijsen Q, Vanden Berghe T, Wirawan E et al (2011) Neutrophil extracellular trap cell death requires both autophagy and superoxide generation. Cell Res 21(2):290–304. https://doi.org/10.1038/cr.2010.150
Suzuki E, Maverakis E, Sarin R et al (2016) T cell-independent mechanisms associated with neutrophil extracellular trap formation and selective autophagy in IL-17A-mediated epidermal hyperplasia. J Immunol 197(11):4403–4412. https://doi.org/10.4049/jimmunol.1600383
Migliario M, Tonello S, Rocchetti V, Rizzi M, Renò F (2018) Near infrared laser irradiation induces NETosis via oxidative stress and autophagy. Lasers Med Sci 33(9):1919–1924. https://doi.org/10.1007/s10103-018-2556-z
Cheng ML, Ho HY, Lin HY, Lai YC, Chiu DT (2013) Effective NET formation in neutrophils from individuals with G6PD Taiwan-Hakka is associated with enhanced NADP(+) biosynthesis. Free Radic Res 47(9):699–709. https://doi.org/10.3109/10715762.2013.816420
McInturff AM, Cody MJ, Elliott EA et al (2012) Mammalian target of rapamycin regulates neutrophil extracellular trap formation via induction of hypoxia-inducible factor 1 α. Blood 120(15):3118–3125. https://doi.org/10.1182/blood-2012-01-405993
Itakura A, McCarty OJ (2013) Pivotal role for the mTOR pathway in the formation of neutrophil extracellular traps via regulation of autophagy. Am J Physiol Cell Physiol 305(3):C348–C354. https://doi.org/10.1152/ajpcell.00108.2013
Chicca IJ, Milward MR, Chapple ILC et al (2018) Development and application of high-content biological screening for modulators of NET production. Front Immunol 9:337. https://doi.org/10.3389/fimmu.2018.00337
Pham DL, Ban GY, Kim SH et al (2017) Neutrophil autophagy and extracellular DNA traps contribute to airway inflammation in severe asthma. Clin Exp Allergy 47(1):57–70. https://doi.org/10.1111/cea.12859
Frangou E, Chrysanthopoulou A, Mitsios A et al (2019) REDD1/autophagy pathway promotes thromboinflammation and fibrosis in human systemic lupus erythematosus (SLE) through NETs decorated with tissue factor (TF) and interleukin-17A (IL-17A). Ann Rheum Dis 78(2):238–248. https://doi.org/10.1136/annrheumdis-2018-213181
Pyo JO, Nah J, Jung YK (2012) Molecules and their functions in autophagy. Exp Mol Med 44(2):73–80. https://doi.org/10.3858/emm.2012.44.2.029
Funding
The Natural Science Foundation of China (NSFC, No. 81671976, 31970132), the Priority Academic Program Development of Jiangsu Higher Education Institutions (PAPD).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflicts of interest to declare.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Wu, C., Zhou, L., Yuan, H. et al. Interconnections among major forms of regulated cell death. Apoptosis 25, 616–624 (2020). https://doi.org/10.1007/s10495-020-01632-2
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10495-020-01632-2