Abstract
As the number of individuals diagnosed with autism increases, there is an increase in demand to provide support throughout their lifespan. This study aimed to: (1) estimate trends in the prevalence of autism diagnoses and medical services use in adults with autism diagnoses; (2) assess predictors of healthcare utilization and costs among adults with autism diagnoses enrolled in Medicaid. A retrospective analysis of 2006–2008 Medicaid claims for 39 states was conducted. There was a 38% increase in the prevalence of autism diagnoses from 2006 to 2008. Total expenditures and outpatient and ER visits varied significantly by demographic variables.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Autism spectrum disorders are neurodevelopmental disorders characterized by repetitive and restrictive behavior and limited social and communication skills (American Psychiatric Association 2013). The Center for disease control and prevention’s autism and developmental disabilities monitoring network, which includes data from 11 sites in the United States (US) found that one in 42 boys and one in 189 girls aged 8 years were diagnosed with autism in 2010 (Wingate et al. 2014). Prevalence data on adults with autism in the US is not currently available; however, a study conducted in England by Brugha et al. (2011) reported the prevalence among adults to be ~ 1%. Children with autism have higher healthcare utilization and costs in terms of outpatient visits, physician visits, medication use, emergency department encounters, and inpatient hospitalizations compared to children without autism (Croen et al. 2006; Liptak et al. 2006). The lifetime cost of supporting an adult with autism with intellectual disability (ID) in the US is estimated to be $2.4 million, while for those without ID it is estimated to be $1.4 million (Buescher et al. 2014). Housing, direct medical, and indirect costs (e.g., lost productivity) constitute the largest portion of this cost. In general, adults with autism have been found to have higher medical cost than children with autism (Buescher et al. 2014).
A few studies have described the healthcare utilization and cost burden associated with a diagnosis of autism among adults. A study conducted by Nicolaidis et al. (2012) highlighted several healthcare disparities experienced by autistic adults in comparison with adults without autism, including significantly more unmet needs in mental health, physical health and prescription medication. This study also found that adults with autism were less likely to receive preventive care services such as tetanus vaccination, blood pressure measurement and Pap smear testing compared to adults without autism. In terms of healthcare utilization, the authors found that adults with autism had higher emergency room (ER) visits compared to adults without autism. Similar findings were reported by Iannuzzi et al. (2014) based on their analysis of the 2010 Nationwide Emergency Department Sample (NEDS) data. Adults with autism were found to have significantly higher emergency department visits compared to children with autism. In their analysis of the 2003 commercial payer MarketScan data, Shimabukuro et al. (2008) found ~ 4 times higher cost per year among privately insured adults with autism (18–21 years) compared to adults without autism. The authors further reported that adults with autism had median annual costs that were ~ $3930 more (~ 9.3 times higher) than adults without the disorder.
Although these studies provide useful information, they do not provide insight into the impact of this disorder among adults in the Medicaid population. Funded jointly by federal and state governments, Medicaid provides healthcare coverage to the indigent population in the US. Data on autism prevalence and healthcare utilization and costs among adults with autism enrolled in the Medicaid program are not currently available. The specific objectives of this study were to: (1) estimate the trends in the prevalence of autism diagnoses in adults and all-cause medical services utilization in these individuals; and (2) study the predictors of medical services utilization and costs among adults diagnosed with autism enrolled in the Medicaid program.
Method
Data Source and Study Design
A retrospective descriptive analysis of 2006–2008 Medicaid administrative claims data for 39 states (Alabama, Arizona, Arkansas, California, Colorado, Connecticut, Delaware, Florida, Georgia, Idaho, Illinois, Indiana, Iowa, Kansas, Kentucky, Louisiana, Maryland, Massachusetts, Michigan, Minnesota, Mississippi, Nebraska, Nevada, New Hampshire, New Jersey, New Mexico, New York, North Carolina, Ohio, Oklahoma, Oregon, Rhode Island, South Carolina, Tennessee, Texas, Vermont, Virginia, Washington, and West Virginia) was conducted. The Medicaid Analytic Extract (MAX) data contains: (1) person summary file (demographic information and eligibility periods for the recipients), (2) other services file (outpatient hospital, physician office, and ER visits), and (3) inpatient services file (information on admission and discharge dates, diagnoses, and amount paid). Encrypted unique identification numbers for individual recipients protected patient identity and were utilized to link study data files. The University of Mississippi Institutional Review Board (UM IRB) approved the study under exempt status.
Sample Selection
The analytic samples for the first objective (annual prevalence and medical services utilization) were developed for each individual year. To be included recipients had to be ≥ 18 years of age and < 65 years of age as of December 31st of the year, and continuously enrolled in Medicaid throughout the year. For the second objective, predictors of medical services utilization and costs, only recipients who met the previous criteria and were continuously enrolled for the entire study period (2006–2008) were included. For all analyses, recipients with long-term care claims were excluded due to the possibility of incomplete medical services use information for such individuals. Recipients with a diagnosis of autism were identified using International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) code 299.xx.
Measures
The prevalence of autism diagnosis among adults was calculated by dividing the number of unique recipients with a claim with a primary or secondary diagnosis of autism by the number of Medicaid recipients meeting the inclusion criteria per year. The prevalence was stratified based on demographic variables (by age, gender, race, and location of residence) for each calendar year. Prevalence was reported as diagnosed cases per 1000 Medicaid recipients.
All-cause medical services use (outpatient, inpatient, and emergency room visits) rates for each year were calculated by dividing the number of recipients with an autism diagnosis who used that service by the number of Medicaid recipients meeting the inclusion criteria per year. Use rates were reported per 10,000 Medicaid recipients and were stratified for demographic variables (age, gender, race, and location of residence) for each calendar year. The mean number of outpatient, inpatient, and emergency room visits was also calculated for those adults with an autism diagnosis; this was done for each calendar year.
To examine predictors of medical services use, co-morbidities and other covariates were calculated from 2006 data and costs and utilization were computed for 2007 and 2008 individually. The MAX inpatient and other therapy files were used to identify healthcare utilization and costs. The total cost of every paid claim in the year is included in the cost measure. Costs were calculated from Medicaid’s perspective.
Three measures were coded to control for co-morbid conditions: disease severity (yes/no), Charlson Co-morbidity Index (CCI), and mental health conditions (yes/no). Disease severity was based on whether a recipient with autism had a hospitalization or an ER visit with a primary diagnosis of autism or not. The co-morbidity profile of recipients was calculated using the Deyo modification of CCI (Deyo et al. 1992). A proxy measure for mental health conditions was also created indicating if an individual had a diagnosis of any of the following conditions: schizophrenia, attention deficit hyperactivity disorder (ADHD), bipolar disorder, depression, anxiety, and intellectual disability.
Age was computed as of December 31st of each year (2006–2008) in order to determine eligibility for inclusion each year, and was categorized into five groups: 18–24 years, 25–35 years, 36–45 years, 46–55 years and 56–64 years. Race was categorized as White, Black/African American, Hispanic or Latino or Other (including American Indian or Alaska Native, Asian, Native Hawaiian or Other Pacific Islander, multiracial, or unknown race). Location of residence was classified as urban or rural based on Rural Urban Commuting Area (RUCA) codes (RUCA Data 2013).
Analysis
Means and standard deviations or frequencies and percentages were used to describe the characteristics of the study sample, as appropriate. All analyses were conducted using SAS version 9.3 (SAS Institute Inc, Cary, NC).
Logistic regression was used to assess trends from 2006 to 2008 in the proportion of adults with an autism diagnosis (prevalence) with year as a predictor variable. Medical services (inpatient visits, ER visits, and outpatient visits) utilization rates stratified by demographic variable were also reported. The mean medical services utilization among adults with an autism diagnosis was also reported for each year individually.
In order to determine the predictors of all-cause inpatient, ER, and outpatient visits and the total all-cause cost among adults diagnosed with autism, generalized linear mixed modeling (GLMM) with an appropriate distribution and a log link was conducted. To determine the appropriate distribution for GLMM (i.e., Gaussian, Poisson, Gamma, and Inverse Gaussian), the modified Park test was used. GLMM was utilized as it can account for correlated observations within clusters. A two-level model with patient at the first level and states at the second level was utilized. All models were computed with age, race/ethnicity, gender and location of residence as predictor variables and a random intercept. Fee-for-service, CCI, presence of any mental health diagnoses, and disease severity were added as possible confounders. The Poisson distribution with a log link was selected as the most appropriate for all the models based on the modified Park test. Results were reported using incidence rate ratios. The demographic and co-morbid variables were calculated for 2006. Total healthcare utilization and costs were calculated by summing all visits or costs reimbursed by Medicaid for calendar years 2007–2008. The multilevel analysis was conducted by using PROC GLIMMIX in SAS version 9.3 (SAS Institute Inc, Cary, NC).
Results
Prevalence
The annual prevalence of autism diagnoses among adult recipients in the Medicaid program was 2.66 per 1000 in 2006, 3.25 per 1000 in 2007, and 3.66 per 1000 in 2008 (Table 1). Based on the logistic regression results, the prevalence of autism diagnoses among adults increased significantly from 2006 to 2008 (p < 0.001). Across all years, prevalence was higher among adults aged 18–25 years (5.8/1000 in 2006, 7.1/1000 in 2007 and 8.2/1000 in 2008), males (6.8/1000 in 2006, 8.2/1000 in 2007 and 9.2/1000 in 2008) and Whites (3.8/1000 in 2006, 4.5/1000 in 2007 and 5.1/1000 in 2008). Prevalence by the location of residence (urban vs. rural) remained stable for all 3 years.
Trends in Medical Services Users and Utilization
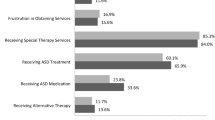
Medical services use rates per 10,000 adult Medicaid recipients were reported for outpatient, inpatient, and ER visits (Table 2) and were stratified by age, gender, race, and location of residence. Similar to the prevalence results, use rates for outpatient, inpatient, and ER visits were higher for 18–25 year olds, males and Whites, relative to comparison groups. For all 3 years, adults diagnosed with autism had an average of ~ 1 inpatient visit per year (1.21 [± 1.99] in 2006, 1.28 [± 2.05] in 2007 and an average of 1.34 [± 2.03] in 2008) and ~ 3 ER room visits (2.52 [± 3.54] in 2006, 2.54 [± 3.49] in 2007 and 2.60 [± 3.71] in 2008) per year (Table 3). On average, individuals diagnosed with autism had approximately 37 outpatient visits in 2006, 35 outpatient visits in 2007, and 36 outpatient visits in 2008.
Predictors of Healthcare Utilization and Costs
GLMM was conducted to study the predictors of outpatient, inpatient, and ER visits for adults diagnosed with autism who had a claim for one of these services (Table 4). None of the demographic variables were found to be significant in the GLMM analyses for inpatient visits. Race was found to be a significant predictor of ER visits. After controlling for all the variables, Whites had fewer ER visits than Blacks (IRR = 0.889; p = 0.04) and others (IRR = 0.848; p = 0.01). Adults diagnosed with autism aged 18–25 years had significantly fewer outpatient visits by a factor of 0.773 compared to adults aged 46–65 years (IRR = 0.773; p < 0.01) after controlling for other variables. Significantly fewer outpatient visits were found among Whites compared to Blacks (IRR = 0.909; p < 0.001) after controlling for other variables. Adults diagnosed with autism residing in urban areas had ~ 1.6 times more outpatient visits compared to those in rural areas (IRR = 1.641; p < 0.001).
Predictors of all-cause healthcare costs for adults diagnosed with autism were also evaluated (Table 5). For all-cause costs, all variables were found to be significant predictors among adults with autism. Adults diagnosed with autism aged 18–25 years (IRR = 0.82; p < 0.001) had lower total costs, while adults aged 26–35 years (IRR = 1.084; p < 0.001) and 36–45 years (IRR = 1.055; p < 0.001) had higher total costs than those aged 46–55 years. Overall, higher costs were found for males compared to females (IRR = 1.024; p < 0.001), Whites compared to Blacks (IRR = 1.084; p < 0.001), and adults located in urban areas compared to those in rural areas (IRR = 1.415; p < 0.001).
Discussion
This study reported the prevalence, all-cause medical utilization, and predictors of all-cause healthcare utilization and costs of adults diagnosed with autism using multi-state Medicaid claims data. The prevalence of autism diagnoses among Medicaid recipients increased approximately 38% from 2.7 per 1000 in 2006 to 3.7 per 1000 in 2008. Despite this increase, the prevalence of autism diagnoses observed in our study was lower than the ~ 1% prevalence reported among adults in a study in England (Brugha et al. 2011). The lower prevalence observed in this analysis may be attributed to factors including methodological differences, age distribution, and geographic variation. Importantly, Brugha et al. assessed prevalence in a community setting by using the ADOS-4 survey, while we used retrospective Medicaid claims data. Additionally, Brugha et al. calculated prevalence among individuals aged 16 years and above, whereas in our study we only included those aged 18 years and above. It is reasonable to assume that adults with autism covered under other insurance systems in the US or those who were uninsured were not represented in our sample. We identified adults with autism based on medical services utilization using autism diagnosis codes; therefore, those adults who did not have such a claim in the study period would have been excluded from our calculation. In a previous study of autism prevalence among adults in the US, Shimabukuro et al. (2008) reported autism prevalence based on administrative data of 1.2/1000 in 2003 among privately insured adults aged 18–24 years of age. As the prevalence of autism increases among children, it is expected that the prevalence for adults will rise over time, which may explain the higher prevalence observed in our study as compared to those reported by Shimabukuro et al. (2008).
To date, only one study has reported trends in prevalence among US adults, where the adult cases with autism were reported to increase by 121.4% from 2002 to 2006 in vocational rehabilitation (VR) programs in the US (Cimera and Cowan 2009). Similar to the general demographic distribution among individuals with autism in other studies (Boyle et al. 2011; Brugha et al. 2011; Mandell et al. 2009), we also found higher prevalence among White, male adults. In our study, males were approximately seven times more likely to have a diagnosis of autism compared to females across all age groups. In addition, we also found higher prevalence among younger adults aged 18–25 years compared to other age groups. Autism diagnoses are more prevalent among children than among adults (Buescher et al. 2014; Cidav et al. 2012). Therefore, it is possible that with more people transitioning from childhood to adulthood, a higher prevalence among younger adults is observed. However, this alone is unlikely to be the cause of the increased prevalence observed in the current study as the increase was evident across all age strata. This suggests that other factors are involved in the increased prevalence. For example, as provider awareness of autism and its influence on health increases, coding for autism in claims may be increasing. It may also be that more adults with autism are becoming eligible for and therefore enrolled in Medicaid over time. Further research is needed to explore these and other factors.
Information on healthcare utilization and costs among adults with autism is currently limited in the US. Adults with an autism diagnosis had on average approximately 1 inpatient visit, 3 ER visits, and 36 outpatient visits during a year. Medical service use rates among this sample of Medicaid recipients were higher among young adults (18–25), males, and Whites. As the prevalence of adults diagnosed with autism increases, there is likely to be an increase in the healthcare burden associated with this disorder. State policy makers will need to consider the rising medical resource use and costs of autism in making Medicaid budget allocation decisions.
Despite greater incidence of medical services usage among young adults with an autism diagnosis, outpatient visits were significantly higher among older adults with an autism diagnosis, after controlling for other demographic and co-morbid conditions. This could be related to gradual progression in age leading to higher office-related visits in this population. In this study, we created three proxy variables to control for co-morbid conditions, including a proxy variable for the presence of any common mental co-morbid conditions such as schizophrenia, ADHD, bipolar disorder, depression, anxiety, or intellectual disability in this population. However, it is also possible that older adults have other co-morbid conditions, contributing to higher outpatient visits. Prior research has found that adults with autism are more likely to have co-morbid conditions such as intellectual disability, bowel disorders, epilepsy, autoimmune disease, and sleep disorders compared to children with autism (Buck et al. 2014; Kohane et al. 2012). A recent study found a higher occurrence of seizures disorders, allergies and depression among adults with autism compared to the general population (Fortuna et al. 2015). Therefore, general progression of age as well as occurrence of co-morbid conditions may lead to higher outpatient visits among older adults. Although prevalence was higher among Whites, Black adults with an autism diagnosis had significantly more ER and outpatient visits. Racial differences have been reported among children with autism, with Black children having a delayed diagnosis and being less likely to receive early treatment and intervention compared to White children (Mandell et al. 2002, 2009). This delay in diagnosis and treatment provision early in childhood may eventually translate to higher resource use as these individuals transition to adulthood. Research has also found that Black children have difficulties in receiving quality healthcare compared to white children with autism (Magana et al. 2012). Adults diagnosed with autism in urban locations compared to rural locations had higher outpatient visits. Better access to support services and resources in urban locations could have contributed to the higher visits observed among adults located in those areas.
The average all-cause cost among adults diagnosed with autism was estimated to be $106,163 over the two-year period. Total costs were significantly higher among older adults diagnosed with autism compared to the other age groups. This finding is consistent with Cidav et al. (2012), who reported an increase in costs with age among Medicaid recipients with autism. Males had higher medical services costs compared to females. Contrary to differences in resource utilization (outpatient visits and ER visits), higher costs were found among Whites compared to Blacks. Adults diagnosed with autism in urban locations had higher average costs than those in rural locations. Variation in disease severity, treatment intensity, and availability of resources may explain these differences. Racial differences have been reported among children with autism with black children having a delayed diagnosis and being less likely to receive early treatment and intervention than white children (Mandell et al. 2002, 2009). This delay in diagnosis and treatment provision early in childhood may eventually translate to higher resource use as they transition to adulthood. Further research is needed to fully understand the underlying reasons contributing to cost differential among adults diagnosed with autism.
Limitations
The identification of autism cases was based on diagnostic codes (ICD-9-CM). Misclassification or coding errors during claims processing could affect study results. Considering that we used Medicaid managed care data, we could not estimate specific autism-related costs in this study. The all-cause medical services utilization and costs reported in this study may not reflect the true healthcare burden of autism and may have led to an overestimation of care utilization and cost. Medicaid coverage varies by state, which may have affected the results of this study. However, to account for this variation, states were treated as random effects in multilevel modeling. The disease severity measure, utilized as covariate in the utilization model, could be subject to measurement error based on variations in access to emergency care and/or availability of alternatives to emergency care. Other differential factors could exist that were not addressed, including potential differential rates of diagnoses for subgroups.
Conclusions
This study evaluated the trends in prevalence of autism diagnosis in adults, health care utilization and predictors of health care use and costs among these individuals enrolled across many state Medicaid programs. The results of this study demonstrated significant increase in the prevalence rate among Medicaid adults with an autism diagnosis over the 3-year study period, which mirror the increasing prevalence trends observed among children over the past few years. We also observed an increase in medical services utilization in terms of inpatient visits, ER visits, and outpatient visits over the study period. Our results suggest significant variation in medical services utilization and costs by demographic characteristics among adults with a diagnosis of autism. With rising prevalence of adults diagnosed with autism in the Medicaid population, state Medicaid programs need to consider the resource impact of this rising trend and make appropriate budgetary decisions to address the needs of this growing population. Future research should examine whether the prevalence trend observed in this study continues. Additionally, more study is needed to examine how the medical services utilization and costs among adults with autism compare with the general population.
References
American Psychiatric Association. (2013). Diagnostic criteria for 299.00 Autistic Disorder. Diagnostic and Statistical Manual of Mental Disorders (5th ed ed.). Washington DC: American Psychiatric Association.
Boyle, C. A., Boulet, S., Schieve, L. A., Cohen, R. A., Blumberg, S. J., Yeargin-Allsopp, M., et al. (2011). Trends in the prevalence of developmental disabilities in US children, 1997–2008. Pediatrics, 127, 1034–1042.
Brugha, T. S., McManus, S., Bankart, J., Scott, F., Purdon, S., Smith, J., et al. (2011). Epidemiology of autism spectrum disorders in adults in the community in England. Archives of General Psychiatry, 68, 459–465.
Buck, T. R., Viskochil, J., Farley, M., Coon, H., McMahon, W. M., Morgan, J., et al. (2014). Psychiatric comorbidity and medication use in adults with autism spectrum disorder. Journal of Autism and Developmental Disorders, 44, 3063–3071.
Buescher, A. V. S., Cidav, Z., Knapp, M., & Mandell, D. S. (2014). Costs of autism spectrum disorders in the United Kingdom and the United States. JAMA Pediatrics, 168(8), 721.
Cidav, Z., Lawer, L., Marcus, S. C., & Mandell, D. S. (2012). Age-related variation in health service use and associated expenditures among children with autism. Journal of Autism and Developmental Disorders, 43, 924–931.
Cimera, R. E., & Cowan, R. J. (2009). The costs of services and employment outcomes achieved by adults with autism in the US. Autism, 13, 285–302.
Croen, L. A., Najjar, D. V., Ray, G. T., Lotspeich, L., & Bernal, P. (2006). A comparison of health care utilization and costs of children with and without autism spectrum disorders in a large group-model health plan. Pediatrics, 118, e1203–e1211.
Deyo, R. A., Cherkin, D. C., & Ciol, M. A. (1992). Adapting a clinical comorbidity index for use with ICD-9-CM administrative databases. Journal of Clinical Epidemiology, 45, 613–619.
Fortuna, R. J., Robins, L., Smith, T. H., Meccarello, J., Bullen, B., Nobis, K., et al. (2015). Health conditions and functional status in adults with autism: A cross-sectional evaluation. Journal of General Internal Medicine, 31(1), 77–84.
Iannuzzi, D. A., Cheng, E. R., Broder-Fingert, S., & Bauman, M. L. (2014). Brief report: Emergency department utilization by individuals with autism. Journal of Autism and Developmental Disorders, 45, 1096–1102.
Kohane, I. S., McMurry, A., Weber, G., MacFadden, D., Rappaport, L., Kunkel, L., et al. (2012). The co-morbidity burden of children and young adults with autism spectrum disorders. PLoS ONE, 7(4), e33224–e33224.
Liptak, G. S., Stuart, T., & Auinger, P. (2006). Health care utilization and expenditures for children with autism: Data from U.S. national samples. Journal of Autism and Developmental Disorders, 36(7), 871–879.
Magana, S., Parish, S. L., Rose, R. A., Timberlake, M., & Swaine, J. G. (2012). Racial and ethnic disparities in quality of health care among children with autism and other developmental disabilities. Journal of Intellectual and Developmental Disability, 50, 287–299.
Mandell, D. S., Listerud, J., Levy, S. E., & Pinto-Martin, J. A. (2002). Race differences in the age at diagnosis among medicaid-eligible children with autism. Journal of the American Academy of Child and Adolescent Psychiatry, 41, 1447–1453.
Mandell, D. S., Wiggins, L. D., Carpenter, L. A., Daniels, J., DiGuiseppi, C., Durkin, M. S., et al. (2009). Racial/ethnic disparities in the identification of children with autism spectrum disorders. American Journal of Public Health, 99, 493–498.
Nicolaidis, C., Raymaker, D., McDonald, K., Dern, S., Boisclair, W. C., Ashkenazy, E., et al. (2012). Comparison of healthcare experiences in autistic and non-autistic adults: A cross-sectional online survey facilitated by an academic-community partnership. Journal of General Internal Medicine, 28, 761–769.
RUCA Data. (2013). Rural-urban commuting area codes (RUCAs). Retrieved June 9th, 2015, from www. http://depts.washington.edu/uwruca/.
Shimabukuro, T. T., Grosse, S. D., & Rice, C. (2008). Medical expenditures for children with an autism spectrum disorder in a privately insured population. Journal of Autism and Developmental Disorders, 38(3), 546–552.
Wingate, M., Kirby, R. S., Pettygrove, S., Cunniff, C., Schulz, E., Ghosh, T., et al. (2014). Prevalence of autism spectrum disorder among children aged 8 years-autism and developmental disabilities monitoring network, 11 sites, United States, 2010. MMWR Surveillance Summaries, 63, 1–21.
Funding
This study was part of a larger project funded by the Organization for Autism Research and a University of Mississippi Graduate School Council Research Grant. The study was presented as a poster at the 2014 Annual Research Meeting (ARM), AcademyHealth, June 8–10, San Diego, CA.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors declare that they have no conflict of interest.
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. For this type of study formal consent is not required.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Jariwala-Parikh, K., Barnard, M., Holmes, E.R. et al. Autism Prevalence in the Medicaid Program and Healthcare Utilization and Costs Among Adult Enrollees Diagnosed with Autism. Adm Policy Ment Health 46, 768–776 (2019). https://doi.org/10.1007/s10488-019-00960-z
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10488-019-00960-z