Abstract
Health care spending usually contributes to a large part of a developed country’s economy. In 2011, the U.S. consumed about 17.7% of its GDP on health care. As one of the most significant components of the health care industry, the hospital sector plays a key role to provide healthcare services. Healthcare services industry can be affected by many factors, of which economic downturn is a crucial one. As a result, it is worth investigating the condition and state of hospital management when economic downturn occurs. This paper aims to analyze how the Great Recession affects hospital performance in Pennsylvania during the period 2005–2012 by using data envelopment analysis (DEA). Specifically, we measure efficiency for hospitals in Pennsylvania, and use several DEA models to calculate the global Malmquist index (GMI). We find that: (1) 15.4% hospitals are always efficient while 36.9% hospitals are always inefficient for all years in 2005–2012; (2) The relative distance for a group of hospitals to the frontier is almost unchanged post-recession and pre-recession; (3) The average efficiency/GMI decreases by 2.43%/3.07% from pre-recession to post-recession. The analysis indicates that hospital performance slightly decreased due to the economic downturn in Pennsylvania.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
1 Introduction
Business cycles could introduce shocks to both demand and supply sides of health care markets. Hospitals may need time to adjust to these shocks in the short term due to contracts, financial resources, and capacity constraint. Thus, a recession could impact how efficient hospitals utilize input to provide their services (output). For example, an economic downturn could affect hospitals’ demand through the changes in health status and health insurance coverage (Pellegrini et al. 2014; Holahan and Wang 2004). An economic downturn could also affect hospitals’ supply due to increases in bad debt, decreases in funding from public programs, and layoffs (Elliott 2010a, b, 2011).
Most hospitals in Pennsylvania were negatively affected during the Great Recession. More people lost their jobs and health insurance as the unemployment rate in Pennsylvania increased from 4.2% in 2007 to 8.6% in 2010. During this economic downturn, patients who lost coverage faced higher out-of-pocket costs for health care services. In addition, the government spending in Medicaid and Medicare programs also dropped, which meant hospitals received lower reimbursement rate, and faced a higher level of bad debt. Hospitals could also receive fewer donations as an economic downturn could restrict donors’ ability to give (Katz-Stone 2001).
As a result, most hospitals used some cost-cutting measures to tighten budgets to deal with the negative impact of the recession. Many hospitals in Pennsylvania reduced operating costs by laying off workers to tighten budgets in the worsening economic environment. According to a survey conducted by The Hospital & Healthsystem Association of Pennsylvania (HAP) in March 2009, economic downturns worsened most hospitals’ financial conditions. According to a December 2008 survey by HAP, almost half of the hospitals in Pennsylvania reported a decreased number of patients, which forced them to tighten their budgets (Wade 2009). Safety-net hospitals with less financial support had to pay attention to financial issues and implement reforms to earn enough money to survive (Indivero 2014). According to the HealthLeaders Media Industry Survey 2010, in Pennsylvania 19 percent of hospitals implemented permanent layoffs during the Great Recession. Leaders of more than 80 percent of hospitals reported that they saw layoffs as one of the most efficient methods of coping with future economic recessions (Baker et al. 2010). For example, Penn State Milton S. Hershey Medical Center implemented some budget-tightening methods such as hiring fewer workers and avoiding raising salaries (Sholly 2009). At the time of another survey conducted by HAP, almost 90 percent of Pennsylvania’s hospitals had limited their expenditure by holding off on building improvements and medical device updates (Twedt 2009).
The Great Recession has impacted many sectors of the economy. It may also impact hospital efficiency, an important research area in health economics. We propose to investigate how the Great Recession affected hospital operating efficiency in Pennsylvania. In this project, we will combine data from American Hospital Association’s (AHA) annual survey and publically available macro data to conduct a data envelopment analysis (DEA) to assess hospital efficiency from 2005 to 2012. The use of DEA allows us to model multiple factors in a single unified way. With the results obtained from our DEA analysis, we could have more insight on how the Great Recession affects hospital operating efficiency. In other words, is hospital operating efficiency pro-cyclical or counter-cyclical?
DEA is developed by Charnes et al. (1978) for identifying best-practices and measuring efficiency of decision making units (DMUs) when multiple performance metrics are present for organizations such as firms, banks and hospitals (Cook et al. 2014). Up to now, DEA has been applied to many areas such as banking, insurance, energy and auditing (Chen et al. 2015, 2016; An et al. 2015, 2016, 2017; Gong et al. 2016). As shown in a recent survey of DEA applications, health care is among the top-five industries (Liu et al. 2013). Studies on health care benchmarking and performance evaluation by DEA are introduced in Ozcan (2014), which provides us an important guideline. To our best knowledge, Sherman (1984) is the first to evaluate hospital efficiency using DEA even though Nunamaker (1983) publishes the first paper in health care focusing on nursing service efficiency. Since then, a number of studies have been focusing on the efficiency of hospitals. For example, some studies consider the difference of hospital characteristics or components such as teaching and non-teaching hospitals (O’Neill 1998; Grosskopf et al. 2001, 2004), federal hospitals (Harrison et al. 2004), not-for-profit and for-profit hospitals (Harrison and Sexton 2006; Araújo et al. 2014) and hospital’s intensive care units (Tsekouras et al. 2010; Leleu et al. 2012). Other studies explore the cause of the resulting hospital efficiency changes (Harris et al. 2000; Ferrier and Valdmanis 2004; Lee and Wan 2004). Du et al. (2014) incorporate health outcomes in their DEA model and Hu et al. (2012) examine regional hospital efficiency with undesirable output. Using DEA, Miller et al. (2015) investigate the impact of the Massachusetts health care reform on hospital costs and quality of care at the same time. Studies considering hospital efficiency in different countries and/or over different time periods include Chang et al. (2004), Kawaguchi et al. (2014), Chen (2003) and Chowdhury et al. (2014), etc.
In order to measure the productivity changes of hospitals over time, the current study applies a global Malmquist productivity index (Pastor and Lovell 2005). Compared to the traditional Malmquist index (Färe et al. 1994) which is not circular and susceptible to linear programming (LP) infeasibility, the global Malmquist index (GMI) satisfies circularity, generates a single measure of productivity change and is immune to LP infeasibility (Pastor and Lovell 2005).
We compile the input and output metrics for hospital performance and incorporate an important measure of unemployment rate, into our analysis. The unemployment rate is regarded as a non-controllable variable in our model. The global Malmquist index is calculated based upon a non-radial and input-oriented Russell DEA model (Färe and Lovell 1978; Färe et al. 1985) for two reasons. First, non-radial model fully considers the slacks, which helps to improve performance more accurately. Moreover, it is more appropriate and practical to allow all inputs and outputs to change non-proportionally. Second, some outputs may be out of control considering our current study. For example, we cannot expect to arbitrarily increase the number of inpatient surgical operations or emergency room visits in order to improve a hospital’s efficiency. We also wonder if there is any input surplus. So, we choose an input-oriented model. We find that the average efficiency/GMI is a bit fallen off during the time period 2005–2012 under investigation, which implies economic downturn has a minor negative impact on hospital performance.
The rest of this paper is organized as follows. The following section briefly reviews the global Malmquist productivity index and presents our DEA models. In Sect. 3, we discuss the input and output measures, calculate the efficiency and global Malmquist index, and analyze the results. Section 4 concludes.
2 Methodology
In this section, we first review the global Malmquist productivity index. There are a number of ways to calculate Malmquist index, depending on the DEA models used. As shown above, this paper uses non-radial and input-oriented DEA models to calculate the efficiency and the global Malmquist index.
2.1 Global Malmquist productivity index
Assume that there are n DMUs over \(t,t=1,\ldots ,T\) time periods with inputs \(X_j^t =(x_{1j}^t ,x_{2j}^t ...,x_{mj}^t )\) and outputs \(Y_j^t =(y_{1j}^t ,y_{2j}^t ...,y_{sj}^t )\), where \(j=1,2,\ldots ,n\) represents \(DMU_j\) in contemporaneous period t. In this paper, we assume that the data set is positive. The contemporaneous technology in time period t can be defined by a production possibility set (PPS) or technology set:
where L and U are lower and upper bounds for the sum of the intensities. For example, \((L,U)=(0,\infty )\) and \((L,U)=(1,1)\) correspond to constant returns to scale (CRS) and variable returns to scale (VRS) models, respectively. Accordingly, we can define the contemporaneous Malmquist index for \(DMU_k\) between two time periods t and \(t+1\) as:
where \(D^{p}(X_k ,Y_k ),p=t,t+1\) represent the distance functions or the different DEA technologies in a non-parametric framework. For example, the input distance function can be defined as:
The Malmquist index can be decomposed as the product of efficiency change (EC) or catch-up and technical change (TC) or frontier-shift as (Färe et al. 1992, 1994):
Based on the contemporaneous Malmquist index or technology, the global production possibility set or global technology can be defined as (Pastor and Lovell 2005):
Equation (6) shows that \(PPS^{G}\) is the convex envelope of all the contemporaneous technologies. As a result, there is only one global benchmark technology. So, geometric mean convention is never needed to define the global Malmquist index that can be formulated as:
Accordingly, \(D^{G}(X_k ,Y_k )\) can be determined as:
In Pastor and Lovell (2005), the global Malmquist index is decomposed as the product of the usual efficiency change (EC) and the change of the best practice gap or best practice change (BPC) as:
where EC is the same with Eq. (4) and
where \(\frac{D^{G}(X_k^{t+1} ,Y_k^{t+1} )}{D^{t+1}(X_k^{t+1} ,Y_k^{t+1} )}\) and \(\frac{D^{G}(X_k^t ,Y_k^t )}{D^{t}(X_k^t ,Y_k^t )}\) reflect the best practice gap between \(PPS^{G}\) and \(PPS^{p},p=t,t+1\) with respect to \(DMU_k\) in periods t and \(t+1\).
As shown above, the global Malmquist index has three merits: (1) Like any fixed base Malmquist index, \(MI^{G}\) is circular, so is EC and BPC. (2) It generates a single value of productivity change and does not need to take the geometric mean of disparate adjacent period measures. (3) It is immune to the LP infeasibility problem. So we can use a VRS technology without considering the possibility of DEA models’ infeasibility (Seiford and Zhu 1999; Chen 2005; Cook et al. 2009; Chen and Liang 2011; Lee et al. 2011).
2.2 DEA models
We use subscript \(i_{Non}\) to denote the non-controllable inputs \(I_{Non} \subseteq \left\{ { 1,2,\ldots ,m} \right\} \) and the number of the non-controllable inputs is q. For \(D^{G}(X_k^{p^{{\prime }}} ,Y_k^{p^{{\prime }}} ),{p}'=t,t+1\), we use the following model to calculate \(D^{G}(X_k^{p^{{\prime }}} ,Y_k^{p^{{\prime }}} ),{p}'=t,t+1\):
where \(\lambda _j^p\) and \(\theta _i\) are intensive and efficiency variables, respectively. Note that the second constraint is imposed an equality in model (11) for non-controllable inputs (Cooper et al. 2007; Cook and Seiford 2009). And \(D^{p}(X_k^{p^{{\prime }}} ,Y_k^{p^{{\prime }}} ),p,{p}'=t,t+1\) can be calculated by the following linear program:
Note that we also use the traditional input-oriented and non-radial VRS DEA model to calculate hospitals’ efficiency. Our DEA models are based upon the assumption of VRS considering the inputs and outputs used in the current study (see next section). For example, it makes no sense to expect the total number of surgical operations to double as the total number of hospital beds is doubled.
3 Hospital performance in Pennsylvania
In this section, we conduct a DEA analysis on how the Great Recession affects hospital performance in Pennsylvania over 2005–2012. The DEA models and global Malmquist index developed in Sect. 2 are used to calculate efficiency and productivity scores of hospitals. We also examine the performance changes in Pennsylvania hospitals pre-recession and post-recession.
3.1 Input and output measures
Data for the study were obtained from the American Hospital Association’s (AHA) Annual Surveys 2005–2012 and publically available economic data from Federal Reserve Economic Data (FRED).Footnote 1 We combine these two data sources to select our five input variables and five output variables reported in Table 1. Four of the input variables, including the number of total hospital beds, the number of full-time physicians and dentists, the number of full-time registered nurses, and the number of full time equivalent licensed practical or vocational nurses, are taken from the AHA Annual Survey of Hospitals to capture hospitals’ physical inputs. The remaining input variable, PA county-level unemployment rates, is taken from FRED Database. All of the five output variables, namely, total facility admissions, total facility inpatient days, inpatient surgical operations, total surgical operations and emergency room visits, are taken from the AHA Annual Survey of Hospitals to capture hospitals’ physical output.
The five input and five output measures for our DEA models are reported in Table 1.
In order to capture hospital inputs, we first select the total hospital beds, which measures the hospital size. As doctors and nurses are the main staff of hospitals, we include three related variables, i.e. full time equivalent physicians and dentists, full time equivalent registered nurses and full time equivalent licensed practical or vocational nurses. Recognizing the effect of the Great Recession on economy, we use an important variable, county-level unemployment rates, to reflect the overall economic condition facing each hospital. We use the unemployment rate to model the impact macroeconomic environment on resources outside hospitals’ control. However, the unemployment rate must remain fixed as the hospitals have no power to change them. So this variable is non-controllable.
For the output part, we choose five variables to reflect the treatment and care. They are total facility admissions, total facility inpatient days, inpatient surgical operations, total surgical operations and emergency room visits. All of them reflect the healthcare services that a hospital provides. We use these measures to quantify the physical output of hospitals.
3.2 Data
As shown above, the dataset used in this paper was obtained from the American Hospital Association’s (AHA) Annual Surveys and Federal Reserve Economic Data. We gather the data of 65 hospitals from 34 counties in Pennsylvania. Considering that only the data for the counties’ unemployment rates are available, in this paper, we directly use the unemployment rate of a county for each hospital in the county.
Tables 2 shows the summary statistics of input and output measures for all the hospitals. There are 65 hospitals in our sample. The average for some measures (hospbd, admtot, ipdtot, suropip and suroptot) in each year is close to each other while it changes a lot for other measures (ftemd, ftern, ftelpn, unemrat and vem). For hospbd, admtot, ipdtot, suropip and suroptot, the differences between their maximum and minimum of mean are 15.54 (=306.92−291.38), 974.23 (=14922.94−13948.71), 4782.72 (=79161.83−74379.11), 167.18(=4743.31−4576.12) and 415.38(=11988.85−11573.46), respectively. The maximal changes of ratio for the mean of these five variables are 5.33, 6.98, 6.43, 3.65 and 3.59%, respectively. However, the differences between the maximum and minimum of mean for ftemd, ftern, ftelpn, unemrat and vem are 35.98, 107.08, 16.28, 4.16 and 9441.22, respectively. And the maximal changes of ratio for the mean of the five variables are 65.39, 23.10, 58.71, 91.90 and 24.32%, respectively.
Moreover, we further report the tendency of the mean in 2005–2012 for all the input/output variables, which is illustrated in Fig. 1. As shown in Fig. 1, the mean of two variables (ftern and vem) strictly increases monotonically while ftelpn’s mean strictly decreases monotonically. For admtot and ipdtot, the mean first increases and then decreases. For the rest of the variables (hospbd, ftemd, unemrat, suropip and suroptot), the mean increases and decreases interchangeably.
Except for unemrat, all the other variables show a relatively large standard deviation. This information implies that the hospitals included in our smaple vary greatly in hospital size. For some variables (hospbd, unemrat, admtot and vem), the mean is larger than its corresponding standard deviation, while the opposite is foundfor other variables (ftemd, ftern and suropip). For ftelpn, ipdtot and suroptot, the mean is either greater or less than its corresponding standard deviation.
3.3 Results
3.3.1 Hospital efficiency
Hospital efficiency in 2005–2012
Based on the data and models above, this section calculates efficiency scores of all hospitals. First we show the efficiency scores of each hospital in each year. Tables 3 reports the results.
Table 3 shows the efficiency for 65 hospitals in 2005–2012. For each year, the number of efficient hospitals is relatively large even though there are more DMUs (65) as compared with the input/output (5/5) metrics. Basically, the number of efficient hospitals gradually increases from 2005 to 2012. The minimum for the number of efficient hospitals is 18 in 2005, and the maximum reaches 29 in 2012. However, the number of hospitals which are efficient for all years from 2005–2012 is less. There are 10 efficient hospitals for all years, including DMUs 3, 5, 9, 18, 19, 38, 47, 58, 60 and 61. The number of inefficient hospitals across all years is 24, including DMUs 2, 7, 8, 11, 12, 13, 15, 16, 23, 25, 26, 27, 28, 32, 40, 44, 48, 50, 52, 54, 55, 56, 63 and 65. Their efficiency is less than unity for all years. Among the inefficient hospitals across all years, DMU 44 has the maximal efficiency (0.9854) in 2007 and it is almost efficient. Three hospitals (DMUs 6, 10 and 51) are inefficient in one year of 2005–2012 while six hospitals (DMUs 4, 37, 42, 49, 57 and 59) are efficient in only one year of 2005–2012.
The statistics of hospital efficiency for each hospital are shown in Fig. 2, which reflects each hospital’s relative performance/position among all hospitals. For example, there are 10 (15.4%) most efficient hospitals that have equal minimal and maximal efficiency scores, which is also shown above. These 10 hospitals should dominate others for the best performance. Clearly, 24 (36.9%) hospitals are inefficient for all years in 2005–2012 because their maximal efficiency scores are less than unity. DMU 14’s minimal efficiency score is smallest though its average efficiency score is not smallest. In fact, DMU 14 has the largest efficiency difference as its maximal efficiency score is unity. DMU 25’s maximal efficiency score is smallest and its minimal efficiency score is almost the smallest one. Moreover, DMU 25 has the smallest average efficiency score. This result suggests that DMU 25’s performance is worst.
Figure 3 graphically reports the maximal efficiency, minimal efficiency and average efficiency of all hospitals in each year. For the maximal efficiency, all the maximal efficiency scores for all hospitals in each year are unity, which represents an efficient status. For the minimal efficiency, the smallest minimal efficiency score for all hospitals across all years is 0.4449, which corresponds to DMU 14 in 2008. The minimal efficiency curve first decreases until 2008 and later decreases again in 2010. There are three hospitals for which the efficiency score is the smallest among all hospitals in two years. DMUs 14, 21 and 26 are the most inefficient ones in 2008–2009, 2006–2007 and 2011–2012, respectively. Compared with the minimal efficiency, the average efficiency nearly keeps unchanged until 2007, decreases in 2008 and then increases. The average efficiency scores are very high in 2005–2012. Among them, the minimum reaches 0.8266 in 2008 and the maximum (0.8524) is even more than 0.85 in 2012. Moreover, the change of average efficiency is not significant for hospitals in 2005–2012. The maximal difference of average efficiency is only 0.0258. This finding implies that the average efficiency only has minor changes over the years.
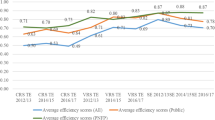
The average efficiency in Fig. 3 reflects the relative distance between the best-practice frontier and the group of hospitals. We call this type of efficiency as average frontier-group efficiency in order to differentiate it from the average efficiency in the next section. As shown in Fig. 4, the mean of average frontier-group efficiency pre-recession and post-recession is 0.8333 and 0.8357, respectively. And the change of ratio for the mean between the frontier-group efficiency is only 0.29%. So the average frontier-group efficiency is almost the same post-recession than pre-recession. It suggests that the relative distance for the group of hospitals to the frontier is almost unchanged post-recession than pre-recession.
In order to examine the correlations among the hospital efficiency scores in each year, we calculate the Pearson correlation coefficients for the efficiency scores in 2005–2012, which are shown in Table 4. The maximal and minimal correlation coefficients are 0.874 and 0.372, respectively. For each year, the maximal correlation coefficient occurs in its adjacent year. For example, the largest correlation coefficient is in Year 2006 for Year 2005 (i.e. 2005 with 2006). Others include 2007 with 2006, 2008 with 2009, 2010 with 2011, and 2011 with 2012. Moreover, for each year in 2006–2011, the first and second largest correlation coefficients are in adjacent year. So, the hospital efficiency scores in these adjacent years are highly correlated.
An interesting finding is that the minimal correlation coefficient occurs in Year 2009 for Years 2005–2007 while it is in Year 2005 for Years 2008–2012. Possible reasons may be (1) for Years 2005–2007 pre-recession, the minimal correlation coefficient is in the year post-recession. The deepest effect of the financial crisis on the relative performance of the hospitals is in Year 2009; (2) for Years 2008–2012 post-recession, the minimal correlation coefficient is in the year pre-recession. And Year 2005 is the furthest (most different) year for Years 2008–2012.
Hospital performance pre-recession and post-recession
In order to figure out the impact of the Great Recession on hospital performance, in this section, we further analyze the average hospital efficiency pre-recession and post-recession. Specifically, we calculate the efficiency of all hospitals in 2005–2012 together. In this case, the total number of DMUs is 520.
First, we show the efficiency distribution for hospitals pre-recession and post-recession due to the large number of hospitals. Figure 5 reports the results. The percentage of efficient hospitals is 14.36% in pre-recession and it is 14.46% in post-recession. So the proportion of efficient hospitals is almost unchanged pre-recession and post-recession. The minimal efficiency is in the interval [0.3, 0.4) in pre-recession while it is in the interval [0.4, 0.5) in post-recession. Besides, the percentage of efficiency in pre-recession is less than that in post-recession for three intervals [0.4, 0.5), [0.5, 0.6) and [0.8, 0.9). However, it is larger than that in post-recession for three intervals [0.6, 0.7), [0.7, 0.8) and [0.9, 1).
Next we quantitatively verify the impact of the Great Recession on hospital performance. Figure 6 reports the average efficiency for hospitals pre-recession and post-recession. As shown in Fig. 6, the average efficiency decreases from 0.7553 to 0.7369 (−2.43%) for hospitals post-recession as compared to pre-recession. It suggests that the Great Recession may have a negative effect on hospital performance. Hence, it supports the argument that the hospital performance slightly decreases due to the Great Recession.
3.3.2 Productivity changes over time
Section 3.3.1 shows the efficiency that only reflects the performance in each single year. To measure the productivity change of hospitals over time, we next calculate the global Malmquist index of the hospitals during 2005–2012. Table 5 reports the results.
In Table 5, there is only one hospital (DMU 5) whose productivity keeps the same all the periods in 2005–2012, and its global Malmquist index is unity. For all the other hospitals, each hospital’s productivity changes differently. And the global Malmquist index increases and decreases interchangeably. It indicates that these hospitals experience progress and regress in the total factor productivity at different points during 2005–2012.
The statistics of global Malmquist index for each hospital are shown in Fig. 7, which partly reflects each hospital’s productivity change. Except for DMU 5, the minimal (maximal) GMI is less (larger) than unity for all the other DMUs. Only one DMU’s minimal/maximal GMI is less/larger than 0.5/2.4, i.e. DMU 14. And seven DMUs’ maximal GMIs are larger than 1.5, including DMUs 4, 14, 20, 24, 37, 46 and 57. In comparison with the minimal/maximal GMI, the average GMI for each DMU is closer to each other. And all the DMUs’ average GMIs falls in the interval [0.9270, 1.1034].
Similar to the efficiency results above, DMU 14 has the smallest minimal GMI (0.3872) and the largest maximal GMI (2.4709), which shows a massive change of productivity during 2005–2012. In fact, DMU 14’s minimal GMI is from period 2008/2007, which is just the time when the economic crisis occurred. Different from its efficiency results, DMU 14 has the largest average GMI. This result may imply that the economic downturn had the greatest impact on DMU 14’s hospital performance. DMU 25’s GMI is almost the same during 2005–2012, which also behaves differently from its efficiency shown in Fig. 2.
Figure 8 further reports the maximal, minimal and average GMIs of all hospitals in each period of 2005–2012. The minimal (maximal) GMI is less (larger) than unity for all periods of 2005–2012. For the maximal GMI, the curve increases smoothly before period 2008/2007 but changes sharply after the period. The largest maximal GMI is 2.4709, which corresponds to period 2011/2010. For the minimal GMI, the smallest minimal GMI for all hospitals across all years is 0.3872, which corresponds to period 2008/2007. So, the largest increase and decrease of productivity are from different periods.
As for the average GMI, five average GMIs are larger than unity, which indicates progress in the total factor productivity. And two are less than unity, which indicates regress in the total factor productivity. Moreover, the average GMI for period 2010/2009 is almost unity (0.9988). The curve has a same increasing/decreasing tendency with the minimal GMI’s, but it is smoother. The maximal difference of average GMIs is 0.0969. Except for period 2008/2007, the average GMI only changes slightly between periods.
In fact, if we focus on the quantitative change of the average GMI in 2005–2012, we find that the average GMI increases and decreases interchangeably. The average GMI for period 2008/2007 is smallest and less than unity (0.9512). So it indicates regress in the total factor productivity in 2008. And the average GMI for period 2009/2008 is larger than unity. So it indicates progress in the total factor productivity in 2009. Note that year 2008 is the worst of the recession. The V-shape change of the average GMI partly reflects the situation of the economic crisis.
Next, we examine the change of GMI pre-recession and post-recession to further show the impact of the Great Recession on hospital performance. As shown in Fig. 9, the mean of the average GMI pre-recession and post-recession is 1.0350 and 1.0033, respectively. And the ratio of change is −3.07%. There is a decrease in the average GMI post-recession compared to pre-recession during 2005–2012. It implies that the economic downturn has a minor negative impact on hospital productivity. Namely, the hospital productivity slightly regresses due to the economic downturn.
Other than the global Malmquist index, we can also obtain the results for efficiency change and best practice change. Considering the goal of this paper, the detailed results are not presented in this paper. And we only report the average EC/BPC over periods in 2005–2012. Figure 10 shows the results for the average GMI/EC/BPC by both bar diagram (including data label) and line graph. Compared with the GMI curve in Fig. 8, the relative magnitude for the average GMI in Fig. 10 is clearer and obvious (it is almost a horizontal line in Fig. 8). By doing this, we can find/compare the tendency for these three indices more easily.
Six values of average ECs are larger than unity. The average EC in period 2007/2006 is 1.0016, which is very close to unity. It suggests that there is almost no efficiency change in period 2007/2006. So only the other five periods undergo progress in the efficiency change. And only one average EC is less than unity, which corresponds to period 2008/2007. However, the smallest average EC is 0.9992 and also almost equals unity. In other words, there is nearly no efficiency change in period 2008/2007. The average efficiency changes (increase/decrease) are consistent with the results in Fig. 3 except for period 2007/2006. In fact, if we calculate the ratio of change of average efficiency in Fig. 3, it is almost the same with the average EC in Fig. 10 for each period. Compared with the change of the average GMI, the change for the average EC is small.
Four values of average BPC are larger than unity, which indicates progress in the frontier technology. The average BPC in period 2010/2009 is 0.9994, which is also very close to unity. So there is almost no change in the frontier technology in this period. It is interesting that the tendency for the average BPC is similar to that for the average GMI. The maximal difference of average BPCs is 0.0968, which approximately equals the maximal difference of average GMIs. Similarly, except for period 2008/2007, the average BPC shifts slight between periods. This finding means that significant changes doe not occur in the frontier technology for hospitals in Pennsylvania during 2005–2012.
4 Conclusions
In general, the status of economy can have a strong impact on the development of firms and organizations, human’s life and healthcare services, etc. For example, many financial crises were associated with banking panics and many downturns cohered with these panics. The 2008 financial crisis directly triggers the global economic recession and has been regarded as the worst financial crisis since the Great Depression of the 1930s. As a result, the real GDP in the United States decreases 2.8% in 2009. The objective of this paper is to examine the impact of the Great Recession on hospital performance in Pennsylvania. We consider a period 2005–2012 where the global economic crisis occurs in the middle of period. And we use several DEA models to measure the hospital efficiency and calculate the global Malmquist index (GMI) for hospitals. The results suggest that the economic downturn or the Great Recession only has a minor impact on hospital operating efficiency. Hospitals could adapt different strategies to navigate through economic downturns. For example, hospitals could downsize operations, layoff some staffs, offer fewer services, set collaborative relationships, expand geographic areas to reach more well-insured patients, align with physicians more closely, and increase healthcare service innovations. As such, our findings provide some useful information for hospital administrators and have potential implications for hospital management.
Note that models (11) and (12) rely on the positive assumption of the data set. Namely, no hospital shows input variables with zeros. Otherwise the average efficiency score in the objective function is incorrect. Future research could develop new models to evaluate efficiency when non-negative data or input variables with zeros exists.
In this paper, we use several inputs where only one input is explicitly related to the economy and there is no measure about hospital operating costs. Also, except for the main staff, no other personnel are considered in the inputs. Moreover, no output is considered for outpatient’s visits except emergency room visits due to the data availability. A potential effect of the Great Depression can be a substitution between inpatients and outpatients to reduce costs, which needs to be further investigated. At the same time, no quality metrics (process measure and/or output measure) are included in our analysis and in the current paper. But the provision of high quality standards is also an important goal of hospitals (and other health services). Besides, new DEA models could be developed when undesirable quality data exists. To fully capture the composition of inputs/outputs and precisely examine the effect of the Great Recession on hospital performance, future research could include other inputs considering hospital operating costs and other output measures. Although we do not find that the economic downturn has a significant impact on hospital performance in Pennsylvania, we cannot claim that the downturn has no impact on hospital performance in other states. Hence, further research can investigate how the Great Recession affected hospital performance in other states. Meanwhile, more research is needed to examine the longer term impact of the Great Recession on hospital operating efficiency.
Notes
Data Accessed on June 25, 20014. Available at http://research.stlouisfed.org/fred2/categories/29613.
References
An, Q., Chen, H., Wu, J., & Liang, L. (2015). Measuring slacks-based efficiency for commercial banks in China by using a two-stage DEA model with undesirable output. Annals of Operations Research. doi:10.1007/s10479-015-1987-1.
An, Q., Chen, H., Xiong, B., Wu, J., & Liang, L. (2016). Target intermediate products setting in a two-stage system with fairness concern. Omega. doi:10.1016/j.omega.2016.12.005.
An, Q., Wen, Y., Xiong, B., Yang, M., & Chen, X. (2017). Allocation of carbon dioxide emission permits with the minimum cost for Chinese provinces in big data environment. Journal of Cleaner Production, 142, 886–893.
Araújo, C., Barros, C. P., & Wanke, P. (2014). Efficiency determinants and capacity issues in Brazilian for-profit hospitals. Health Care Management Science, 17, 126–138.
Baker, R. M., Dixon, D. R., & Passmore, D. (2010). Role of hospitals in the Pennsylvania economy. Social science research network, February 23, 2010. http://ssrn.com/abstract=1557864. Accessed 31 March, 2015.
Chang, H., Cheng, M. A., & Das, S. (2004). Hospital ownership and operating efficiency: Evidence from Taiwan. European Journal of Operational Research, 159, 513–527.
Charnes, A., Cooper, W. W., & Rhodes, E. (1978). Measuring the efficiency of decision making units. European Journal of Operational Research, 2, 429–444.
Chen, Y. (2003). A non-radial Malmquist productivity index with an illustrative application to Chinese major industries. International Journal of Production Economics, 83, 27–35.
Chen, Y. (2005). Measuring super-efficiency in DEA in the presence of infeasibility. European Journal of Operational Research, 161, 545–551.
Chen, Y., Cook, W. D., Du, J., Hu, H. H., & Zhu, J. (2015). Bounded and discrete data and Likert scales in data envelopment analysis: Application to regional energy efficiency in China. Annals of Operations Research. doi:10.1007/s10479-015-1827-3.
Chen, Y., & Liang, L. (2011). Super-efficiency DEA in the presence of infeasibility: One model approach. European Journal of Operational Research, 213, 359–360.
Chen, Y., Li, Y. J., Liang, L., Salo, A., & Wu, H. Q. (2016). Frontier projection and efficiency decomposition in two-stage processes with slacks-based measures. European Journal of Operational Research, 250(2), 543–554.
Chowdhury, H., Zelenyuk, V., Laporte, A., & Wodchis, W. P. (2014). Analysis of productivity, efficiency and technological changes in hospital services in Ontario: How does case-mix matter? International Journal of Production Economics, 150, 74–82.
Cook, W. D., Liang, L., Zha, Y., & Zhu, J. (2009). A modified super-efficiency DEA model for infeasibility. Journal of Operational Research Society, 69, 276–281.
Cook, W. D., & Seiford, L. (2009). Data envelopment analysis (DEA)—Thirty years on. European Journal of Operational Research, 192, 1–17.
Cook, W. D., Tone, K., & Zhu, J. (2014). Data envelopment analysis: Prior to choosing a model. Omega, 44, 1–4.
Cooper, W. W., Seiford, L., & Tone, K. (2007). Data envelopment analysis: A comprehensive text with models, applications, references, and dea-solver software. Berlin: Springer.
Du, J., Wang, J., Chen, Y., Chou, S.-Y., & Zhu, J. (2014). Incorporating health outcomes in Pennsylvania hospital efficiency: An additive super-efficiency DEA approach. Annals of Operations Research, 221, 161–172.
Elliott, V. S. (2010a). Hospital mass layoffs matching last year’s record levels: Health systems say the economic downturn continues to take its toll. American Medical News, American Medical Association, April 5, 2010. http://www.amednews.com/article/20100405/business/304059962/7/. Accessed 17 March, 2015.
Elliott, V. S. (2010b). Recession hitting health system harder this time around: Patients are having trouble paying medical bills, a New Study Finds. American Medical News, American Medical Association, May 12, 2010. http://www.amednews.com/article/20100512/business/305129997/8/. Accessed 17 March, 2015.
Elliott, V. S. (2011). 2010 the second-worst year for hospital mass layoffs in 15 years: The highest number of layoffs occurred in April, when almost 2,000 employees filed for unemployment benefits. American Medical News, American Medical Association, Feb. 9, 2011. http://www.amednews.com/article/20110209/business/302099997/8/. Accessed 17 March, 2015.
Färe, R., Grosskopf, S., Lindgren, B., & Roos, P. (1992). Productivity developments in Swedish pharmacies: A non-parametric Malmquist approach. Journal of Productivity Analysis, 3, 85–101.
Färe, R., Grosskopf, S., & Lovell, C. A. K. (1985). The measurement of efficiency of production. Dordrecht: Kluwer-Nijhoff Publishing.
Färe, R., Grosskopf, S., Norris, M., & Zhang, Z. (1994). Productivity growth technical progress and efficiency changes in industrialized countries. American Economic Review, 84, 66–83.
Färe, R., & Lovell, C. A. K. (1978). Measuring the technical efficiency of production. Journal of Economic Theory, 19, 150–162.
Ferrier, G. D., & Valdmanis, V. (2004). Do mergers improve hospital productivity? Journal of the Operational Research Society, 55(10), 1071–1080.
Gong, Y. D., Zhu, J., Chen, Y., & Cook, W. D. (2016). DEA as a tool for auditing: Application to Chinese manufacturing industry with parallel network structures. Annals of Operations Research. doi:10.1007/s10479-016-2197-1.
Grosskopf, S., Margaritis, D., & Valdmanis, V. (2001). The effects of teaching on hospital productivity. Socio-Economic Planning Sciences, 35(3), 189–204.
Grosskopf, S., Margaritis, D., & Valdmanis, V. (2004). Competitive effects on teaching hospitals. European Journal of Operational Research, 154(2), 515–525.
Harrison, J. P., Coppola, M. N., & Wakefield, M. (2004). Efficiency of federal hospitals in the United States. Journal of Medical Systems, 28(5), 411–422.
Harrison, J. P., & Sexton, C. (2006). The improving efficiency frontier of religious not-for-profit hospitals. Hospital Topics, 84(1), 2–10.
Harris, J. M., Ozgen, H., & Ozcan, Y. A. (2000). Do mergers enhance the performance of hospital efficiency? Journal of the Operational Research Society, 51, 801–811.
Holahan, J., & Wang, M. (2004). Changes in health insurance coverage during the economic downturn: 2000–2002. Health Affairs. doi:10.1377/hlthaff.w4.31.
Hu, H. H., Qi, Q., & Yang, C. H. (2012). Evaluation of China’s regional hospital efficiency: DEA approach with undesirable output. Journal of the Operational Research Society, 63, 715–725.
Indivero, V. M. (2014). Hospitals recover from recession, some financial issues remain, Penn State News, Penn State University. May 12, 2014. http://news.psu.edu/story/315594/2014/05/12/research/hospitals-recover-recession-some-financial-issues-remain. Accessed 17 March, 2015.
Katz-Stone, A. (2001). Downturn adds to hospitals’ fundraising woes. Philadelphia Business Journal, 20(9), 17.
Kawaguchi, H., Tone, K., & Tsutsui, M. (2014). Estimation of the efficiency of Japanese hospitals using a dynamic and network data envelopment analysis model. Health Care Management Science, 17, 101–112.
Lee, H. S., Chu, C. W., & Zhu, J. (2011). Super-efficiency DEA in the presence of infeasibility. European Journal of Operational Research, 212, 141–147.
Lee, K., & Wan, T. T. H. (2004). Information system integration and technical efficiency in urban hospitals. International Journal of Healthcare Technology and Management, 1(3/4), 452.
Leleu, H., Moises, J., & Valdmanis, V. (2012). Optimal productive size of hospital’s intensive care units. International Journal of Production Economics, 136(2), 297–305.
Liu, J. S., Lu, L. Y. Y., Lu, W. M., & Lin, B. J. Y. (2013). A survey of DEA applications. Omega, 41, 893–902.
Miller, F., Wang, J., Zhu, J., Chen, Y., & Hockenberry, J. (2015). Investigation of the impact of the Massachusetts health care reform on hospital costs and quality of care. Annals of Operations Research. doi:10.1007/s10479-015-1856-y.
Nunamaker, T. R. (1983). Measuring routine nursing service efficiency: A comparison of cost per patient day and data envelopment analysis models. Health Services Research, 18, 183–208.
O’Neill, L. (1998). Multifactor efficiency in data envelopment analysis with an application to urban hospitals. Health Care Management Science, 1(1), 19–27.
Ozcan, Y. A. (2014). Health care benchmarking and performance evaluation: An assessment using data envelopment analysis (DEA) (2nd ed.). Berlin: Springer.
Pastor, J. T., & Lovell, C. A. K. (2005). A global Malmquist productivity index. Economics Letters, 88, 266–271.
Pellegrini, L. C., Rodriguez-monguio, R., & Qian, J. (2014). The US healthcare workforce and the labor market effect on healthcare spending and health outcomes. International Journal of Health Care Finance and Economics, 14(2), 127–141.
Seiford, L. M., & Zhu, J. (1999). Infeasibility of super-efficiency data envelopment analysis models. INFOR, 37, 174–187.
Sherman, H. D. (1984). Hospital efficiency measurement and evaluation: Empirical test of a new technique. Medical Care, 22(10), 922–938.
Sholly, C. (2009). Despite recession, HMC in black. Lebanon Daily News, June 28, 2009. http://www.ldnews.com/ci_12710336. Accessed 31 March, 2015.
Tsekouras, K., Papathanassopoulos, F., Kounetas, K., & Pappous, G. (2010). Does the adoption of new technology boost productive efficiency in the public sector? The case of ICUs system. International Journal of Production Economics, 128(1), 427–433.
Twedt, S. (2009). Survey: 80 percent of PA. hospitals weigh layoffs. Pittsburgh Post-Gazette, March 13, 2009. http://www.post-gazette.com/business/businessnews/2009/03/13/Survey-80-percent-of-Pa-hospitals-weigh-layoffs/stories/200903130144. Accessed 31 March, 2015.
Wade, M. (2009). Area hospitals forced to tighten budgets. Northeast Pennsylvania Business Journal, 24(3), 25.
Acknowledgements
The authors are grateful for the comments and suggestions from two anonymous reviewers on an earlier version of this paper. Dr. Ya Chen thanks the support by the National Natural Science Foundation of China (Grant No. 71601064) and Natural Science Foundation of Anhui Province (Grant No. 1708085QG161). Support from the Priority Academic Program Development of the Jiangsu Higher Education Institutions (China) is acknowledged.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Chen, Y., Wang, J., Zhu, J. et al. How the Great Recession affects performance: a case of Pennsylvania hospitals using DEA. Ann Oper Res 278, 77–99 (2019). https://doi.org/10.1007/s10479-017-2516-1
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10479-017-2516-1