Abstract
Background
Depression consistently predicts nonadherence to human immunodeficiency virus antiretroviral therapy, but which aspects of depression are most influential are unknown. Such knowledge could inform assessments of adherence readiness and the type of depression treatment to utilize.
Purpose
We examined how depression severity, symptom type, and change over time relate to adherence.
Methods
Microelectronic adherence and self-reported depression data from 1,374 participants across merged studies were examined with cross-sectional and longitudinal analyses. Depression variables included a continuous measure, categorical measure of severity, cognitive and vegetative subscales, and individual symptoms.
Results
At baseline, mean adherence was 69%, and 25% had mild/moderate and 18% had severe depression. In cross-sectional multivariate analyses, continuous depression, cognitive depressive symptoms, and severe depression were associated with lower adherence. In longitudinal analysis, reductions in both continuous and categorical depression predicted increased adherence.
Conclusions
The relationship between global continuous depression and nonadherence was statistically significant, but relatively weak compared to that of cognitive depressive symptoms and severe depression, which appear to pose strong challenges to adherence and call for the need for early detection and treatment of depression.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Depressive symptoms are highly prevalent in individuals infected with the human immunodeficiency virus (HIV). In a large nationally representative probability sample of persons living with HIV in the USA, 37% screened positive for depression using a self-report [1]. Rates of current clinical depression are much lower when diagnosed by clinical structured interviews [2], but nonetheless are roughly two times greater in people living with HIV than the general population (approximately 10% versus 5%), as determined by a meta-analysis of published studies [3].
Depression has been associated with a threefold increase in nonadherence with medical treatment recommendations in general [4], and HIV research has consistently shown depression to be an impediment to HIV antiretroviral therapy (ART) adherence [5–9]. Depression is also associated with missed clinic appointments [6], failure to initiate ART [10–12] or to enter into HIV care [13], virologic treatment failure [14], and provider reluctance to prescribe ART for fear of it interfering with adherence [15–17]. However, studies to date have mostly examined the cross-sectional association between global measures of depression and nonadherence in relatively small samples. Research on the specific aspects of depression (e.g., type and severity of depressive symptoms) that drive its effect on objectively measured adherence over time and in large samples is scarce. Greater understanding of how these aspects of depression affect adherence can inform adherence interventions that integrate depression treatment and decisions regarding ART initiation among depressed patients [18].
There has been speculation, but little data, concerning whether specific types of depressive symptoms are more or less associated with lapses in medication adherence. Both cognitive and vegetative symptoms of depression may present challenges to adherence. For example, cognitive symptoms such as low mood and loss of interest can result in loss of motivation for daily activities, including taking one’s medication on schedule [19, 20]. Poor concentration can manifest as forgetfulness, which is the most frequently cited reason patients give for missing doses of ART [7, 9, 20, 21]. Vegetative symptoms such as sleep disturbance and fatigue can wreak havoc with structured daily routines including dosing regimens [22]. Loss of appetite can make it a challenge to eat the food needed to properly absorb medication and lead to patients skipping doses in an attempt to mitigate side effects intensified by poor dietary intake. If either vegetative or cognitive depressive symptoms are more strongly related to adherence, this can inform the nature of both the assessment and treatment of depression that clinicians utilize to improve adherence.
For both assessment and intervention purposes, it is also important to understand whether severity of depression is associated with nonadherence. Standardized depression rating scales and diagnostic interviews provide a range of diagnostic levels of depression severity based on diagnostic criteria or validated cutoff scores, from mild to moderate to severe depression, and it is possible that these severity levels of depression may differentially influence adherence. Yet we are unaware of published data that have carefully examined this potentially important distinction. Some providers are reluctant to prescribe ART to depressed patients, fearing that depression prevents a patient from being able to adhere well enough to ward off developing drug resistance [15–17]; knowing whether any level of depression, or only severe levels of depression, are associated with poor adherence could thus inform decisions regarding adherence readiness and treatment initiation.
Longitudinal studies can shed further light on the relationship between depression and nonadherence; however, few studies have adequate statistical power, longitudinal data, or precision of adherence measurement. While depression is commonly thought of as an antecedent to nonadherence, the relationship between depression and adherence may be bidirectional; depression may impede adherence and other health behaviors, and poor adherence and associated effects on physical health may increase the risk for depression [23]. Studies of interventions targeting both depression and ART nonadherence have resulted in mixed findings regarding whether changes in depression correspond to changes in adherence over time. Safren et al. conducted a small pilot study of cognitive-behavioral counseling for depression and ART nonadherence and found that intervention patients experienced a significant decrease in depression and increase in adherence over time [18]. In contrast, Antoni et al. found that beneficial effects of a cognitive-behavioral stress management program on depressed mood were not associated with improved ART adherence [24]. Other studies have found that those receiving psychiatric care, including antidepressants, and who presumably experience reduced depression, are more likely to be prescribed ART and to be adherent to it [25–28].
In this paper, we report findings from a secondary analysis of data merged from longitudinal studies that measured ART adherence with electronic monitoring devices, considered to be one of the most accurate, objective methods currently available [29]. We examined multiple measures of depression to assess whether the relationship between depression and nonadherence differs by diagnostic levels of depressive severity, types of symptoms (cognitive vs. vegetative), and specific individual depressive symptoms. We also examined the relationship between changes in adherence and depression over time. Our hypotheses included the following: (1) adherence will be significantly lower among individuals with severe or moderate depressive symptoms as compared to those evidencing no depressive symptoms, (2) cognitive depressive symptoms will be more strongly negatively correlated with adherence compared to vegetative depressive symptoms, and (3) reduced depressive symptoms over time will be associated with improved adherence.
Methods
Data Source
Data are from the Multi-site Adherence Collaboration on HIV (MACH14), a project of pooled data from 16 longitudinal studies that examined electronically monitored ART adherence across 14 research sites in the USA. All studies received IRB approval for their protocols and obtained written informed consent. The samples for these studies were recruited between 1997 and 2009, and 12 evaluated an adherence intervention, while the other four were observational studies. The analysis for this paper was performed with data from the ten studies included in the MACH14 dataset that had measures of depression. From this dataset, 1,374 participants (out of 2,860 participants in the entire dataset) had both depression and adherence measures available, and thus constituted the sample for this analysis. The eligibility criteria varied across these studies, but eight of the ten studies were performed with general HIV clinic populations (the other two consisted of drug users and homeless or marginally housed); none specifically enrolled depressed patients. A more detailed description of MACH14 is published elsewhere (Liu et al., submitted for publication).
Measures
Background Characteristics
These included age, gender, race/ethnicity, education, employment, sexual orientation, whether or not illicit drugs had ever been used in the past, and CD4 count at study entry.
ART Adherence
Electronic data monitoring caps were used to measure adherence in all of the studies from which the data were drawn. These caps house an electronic chip that records the exact time that the cap is unscrewed from the bottle. Participants were instructed to remove the cap from the bottle at the time that they planned to ingest the medication and to only remove one dose at a time. Adherence was operationalized as the percentage of prescribed doses taken during the 2 weeks prior to the assessment (continuous variable), and whether or not the participants had taken at least 90% of their prescribed doses (“good” adherence) during this time period (dichotomous variable)—a cutoff that is commonly used in research and that represents a level of adherence needed to achieve sustained virologic response [30, 31]. The timing of when the doses were taken (i.e., cap removed from the bottle) is not accounted for in these variables. The 2-week observation period matches the time frame used in the depression measures in half of the ten studies, with the other half using past week as the time frame.
Depression
Four different depression measures were used across the ten studies: four used the Beck Depression Inventory version II (BDI-II) [32], one used the original version of the BDI [33], three used the Center for Epidemiological Studies Depression Scale (CES-D) [34], and two used the depression subscale of the Brief Symptom Inventory (BSI) [35]. In order to merge the depression data from all studies, we devised methods to compute a single continuous measure, a single categorical measure that reflects established diagnostic levels of depression, and single items for each depression symptom that was assessed.
The continuous measure of depression was created by converting data from each of the different depression scales into standardized Z scores. The categorical measure of depression severity was aggregated using published, previously validated ranges for each depression scale. Both versions of the BDI have four validated score ranges that reflect severity of depression (minimal, mild, moderate, severe), as does the CES-D (none, mild to moderate, clinical depression, major depression). Level of depressive severity was collapsed into three categories for each measure: the first level in the original classification of each scale was labeled “none/minimal,” the second and third levels were combined to represent “mild/moderate,” and the fourth level was labeled “severe.” Data from the two studies that used the BSI (n = 238) were not included when creating this variable because the BSI does not have validated cutoff scores for establishing severity levels.
Finally, to combine data with regard to individual depression symptoms, we compared the response formats representing the frequency of each item or symptom of each measure: the BDI-I, BDI-II, and CES-D use four-point response scales, while the BSI uses a five-point response scale, but in all cases, the range is from “not at all/not present” to “all of the time/very present.” The individual symptom data were converted to four-point response scales from 0 “not present” to 3 “present most or all of the time”; for the BSI, the last two response levels (“quite a bit” and “extremely”) were combined to represent “present most or all of the time” in the new response format. If a scale had multiple items that represented a specific symptom (e.g., items “loss of energy” and “tiredness or fatigue” from the BDI-II), an average of these items was used to represent the symptom score. Finally, with the converted single item scores, mean vegetative and cognitive subscales were calculated, which is a common categorization of depression symptom type [36–39]. Symptoms included in the vegetative subscale were fatigue, loss of appetite or weight, sleep disturbance, and psychomotor agitation; cognitive symptoms included depressed mood, loss of interest, suicidality, irritability, hopelessness, indecisiveness, poor concentration, worthlessness, and guilt. The depression scales varied on the number of vegetative and cognitive symptoms that were represented; therefore, the subscale scores represented the mean of the number of items or symptoms that were measured.
Statistical Analysis
Baseline was defined as the first assessment in which data were collected for both adherence and depression. Along with the baseline measures, data from the subsequent two follow-up assessments (if available) that measured both constructs were used in the longitudinal analysis. Descriptive statistics were calculated to examine the distributions of depression, adherence, and demographic characteristics. Bivariate analyses [Pearson correlation, two-tailed t test, analysis of variance, and Chi-Square] were used to examine the relationships between the continuous (percentage of prescribed doses taken) and categorical [good (>=90% adherence) versus poor adherence] measures of adherence and the depression variables. Multiple linear (continuous measure of adherence) and logistic (dichotomous measure of adherence) regressions were used to model the associations with depression at baseline, controlling for background characteristics; separate analyses were conducted for the continuous measure of depression, the categorical measure of diagnostic depressive severity, and the vegetative and cognitive subscales (which were placed in a single model together).
To examine the longitudinal relationship between depression and adherence, repeated measure mixed effects models [40, 41] were fitted to assess whether depression is associated with adherence over time, controlling for the number of weeks between the first and the third time points, and background characteristics that were significantly associated with adherence in any of the cross-sectional regression analyses. Separate models were fitted for the continuous and categorical measures of depression.
Results
Sample Description
The sample of 1,374 participants had the following demographic and background characteristics: mean age was 42.0 years (SD = 8.1; range, 18–70), 67% were male, 42% self-identified as heterosexual, 71% were ethnic minorities (including 48% African American and 13% Hispanic), 22% did not graduate from high school, and 32% had a history of illicit drug use. Average length of time since HIV diagnosis was 7.9 years (SD = 5.6), and mean CD4 count was 372 cells/mm3 (SD = 296). Mean ART adherence at baseline was 69% (SD = 34%), with 593 (43%) having “good” adherence (defined as taking at least 90% of prescribed doses).
With regard to depression at baseline, the mean Z-score on the standardized continuous depression measure was 0.87 (SD = 1.64), with a range of −1.31 to 7.72. Among the subgroup of 1,128 participants who were from studies that used a depression rating scale with established diagnostic cutoff scores, 639 (57%) had none or minimal signs of depression, 284 (25%) had mild to moderate depression, and 205 (18%) had severe depressive symptomatology.
Bivariate Analysis of the Relationship Between Depression and Adherence
We first examined the relationship between nonadherence and the standardized continuous measure of depression. Adherence was negatively correlated with depression, r (1365) = −0.08, p < 0.01, and those with good adherence had significantly lower depression (mean = 0.63, SD = 1.47) than those with poor adherence (mean = 1.06, SD = 1.73), t (1,346) = 4.9, p < 0.001.
We then assessed whether each specific depressive symptom, as well as vegetative and cognitive symptom subscales, was related to nonadherence. Good adherence was associated with lower levels of nearly every individual depression symptom (only irritability did not differ between good and poor adherers), as well as lower vegetative and cognitive subscale scores (see Table 1). However, while both the cognitive and vegetative subscales were negatively correlated with the continuous measure of adherence, analysis of each specific depressive symptom revealed that most of the cognitive symptoms (depressed mood, loss of interest, hopelessness, guilt, poor concentration, and worthlessness) were significantly correlated with nonadherence, whereas fatigue was the only vegetative symptom that was significantly correlated with nonadherence (see Table 1).
When examining the categorical variable of depression, mean adherence was equivalent between those with no depression (mean = 68%, SD = 34%) and mild to moderate depression (mean = 68%, SD = 35%), but both of these levels were significantly higher than what was measured in those with severe depression (mean = 57%, SD = 38%), F(2,1125) = 8.79, p < 0.001. Similarly, only 28% of those with severe depression had “good” adherence, compared to 40% and 44% of those with no and mild to moderate depression, respectively, χ 2(2,1128) = 15.0, p < 0.001.
Cross-Sectional Multivariate Analysis of the Relationship Between Depression and Adherence
Linear regression analysis was used to examine the relationship between depression and the continuous measure of adherence, with a separate model for the [1] continuous measure of depression, [2] cognitive and vegetative symptom subscales, and [3] categorical measure of depressive severity. In each model, background covariates included age, gender, employment, race/ethnicity, sexual orientation, history of illicit drug use, and baseline CD4 count. Table 2 lists the results of each model.
In the model with the continuous measure of depression, greater depression was significantly associated with lower adherence, beta (SE) = −0.012 (0.006), p < 0.05. In the model with both vegetative and cognitive symptom subscales, greater cognitive depressive symptoms were associated with lower adherence, beta (SE) = −0.052 (0.027), p < 0.05, but not vegetative symptoms. In the third model, which included the categorical measure of depression (with “none/minimal” depression as the referent), only severe depression, beta (SE) = −0.090 (0.038), p < 0.01, was associated with lower adherence.
Logistic regression analysis was then used to examine the relationship between depression and “good” versus “poor” adherence, again with separate models for each of the depression measures and inclusion of the background covariates (see Table 3). The same three measures of depression were significantly associated with the categorical adherence measure as were associated with the continuous adherence measure: continuous depression, cognitive depressive symptoms, and severe depression. In the model with the continuous measure of depression, greater depression was associated with poor adherence, odds ratio (OR) confidence interval (CI) = 0.86 (0.79, 0.93), p < 0.001. In the model with vegetative and cognitive symptom subscale scores, greater cognitive depressive symptoms but not vegetative symptoms were associated with poor adherence, OR (CI) = 0.74 (0.55, 0.99), p < 0.05. The model with the categorical measure of depression showed that severe depression, OR (CI) = 0.51 (0.34, 0.78), p < 0.05, was associated with poor adherence, but not mild to moderate depression.
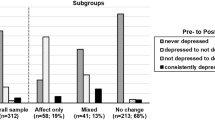
Longitudinal Multivariate Analysis of the Relationship Between Changes in Depression and Adherence
Repeated measures mixed effect models were fitted to examine whether the continuous measure of depression was associated with nonadherence over time. Adherence levels at the three time periods was the dependent variable, and the independent variables included the measures of depression at the same time periods, the number of weeks from time one to time three (average of 27 weeks; range, 8–36 weeks), and the background characteristics that were found to be predictive of adherence in any of the cross-sectional regression models described above (age, gender, race/ethnicity, sexual orientation, history of drug use, CD4 count). Results indicate that change in depression over time was significantly associated with change in adherence, beta (SE) = −0.015 (0.005), p < 0.01, such that for every unit of increase in depression, adherence decreased by 1.5%; the maximum effect of depression on adherence was approximately 12% change in adherence, as eight was the highest depression score (see Table 4).
In the model with categorical depression measure, we converted the three-level measure of depressive severity into a binary variable—high (severe) versus low (no or mild/moderate) depression—because no and mild/moderate depression were associated with equivalent levels of adherence in the bivariate analysis. Greater depression over time was associated with reduced adherence, beta (SE) = −0.089 (0.018), p < 0.001, with depression associated with about a 9% reduction in adherence (see Table 4).
Discussion
This study is one of the few to examine the relationship between depression and ART nonadherence using specific types of depressive symptoms, a finer analysis of depressive severity, and objective, electronically monitored longitudinal adherence data. Like other studies, our data show that global depression is associated with lower adherence [5–9], but our findings also suggest that cognitive depressive symptoms affect adherence more than vegetative symptoms, that severe depression impedes adherence whereas mild to moderate depression appears not to, and that reduced depression over time is associated with improved adherence.
While the relationship between the global continuous measure of depression and nonadherence was statistically significant, the magnitude was relatively weak compared to that of cognitive depressive symptoms and especially severe depression. This highlights the value of a more nuanced measurement of depression. Researchers and clinicians who are assessing the relationship between depression and ART adherence, or examining whether a patient’s depressive symptoms may pose a challenge to adherence, should use measures of depression that go beyond a global impression and reflect both symptom type and severity.
Both cognitive and vegetative symptoms were associated with lower adherence when assessed globally in the bivariate analyses, but analyses involving individual symptoms showed that most cognitive symptoms were correlated with nonadherence, while fatigue was the only vegetative symptom associated with adherence. Consistent with our hypothesis that cognitive symptoms would be more strongly associated with nonadherence, the multivariate analysis, which controlled for covariates including CD4 count, showed that the cognitive symptom subscale was associated with nonadherence but not the vegetative symptom subscale. Most vegetative depressive symptoms overlap with those of medical illness and are common among persons living with HIV (e.g., poor appetite, insomnia, fatigue) [42]; therefore, the presence of such physical symptoms may be due to HIV (and possibly higher viral load resulting from nonadherence) or antiretroviral side effects (which may be related to greater adherence) and thus relate to nonadherence differently and less robustly than cognitive symptoms of depression, and may be related to nonadherence independent of depression [43].
We hypothesized that patients with either severe or mild to moderate depression would have lower adherence compared to non-depressed patients, but our data revealed that only severe depression was associated with nonadherence. This finding has implications for HIV clinical management and ART access, as providers have shown a reluctance to prescribe ART to patients with mental illness for fear that such patients will not be able to adhere well enough and thus develop drug resistance [15–17]. While patients with mild to moderate depressive symptoms may need mental health treatment for their depression, our data suggest that these patients are able to adhere as well to ART as patients without depression, and that it is only when depressive symptoms become relatively severe, and presumably disruptive to overall functioning, that adherence is negatively affected. Accordingly, measures of depression in routine clinical practice must assess not only the presence of symptoms but also symptom severity and frequency, and include a sufficient representation of cognitive depressive symptoms. Routine screening of depression can be implemented with little need for limited clinic resources as several self-administered depression measures have been validated and successfully used with HIV patients [44].
As we had hypothesized, longitudinal analysis showed that changes in depression correspond with changes in adherence. This finding suggests that depression treatment could have indirect benefits on adherence. Only recently have studies examined the effects of depression treatment on adherence, but there is some evidence that antidepressant treatment [25, 28, 45] and cognitive behavioral therapy for depression [18] improve adherence among depressed patients. It would be informative to know whether such benefits accrue even more among patients who had more severe depression or patients whose cognitive symptoms of depression are relieved. Similarly, interventions to improve adherence may indirectly lead to improve mood and psychological well-being, and this warrants examination.
Limitations of the study include the reliance on self-report measures of depression that were not uniform across studies. Although the BDI and CES-D depression scales have established scoring cutoffs for determining diagnostic levels of depression, self-reports overestimate psychopathology, and hence, our data would be strengthened if depression diagnoses had been derived from diagnostic interviews [44]. The use of data from several different scales also introduces added variance into the analyses, although the content of the different measures is very similar. It is worth noting that the ranges of depression scores were relatively similar across the studies that comprised that dataset for this analysis, suggesting that none of the studies was an outlier that may have disproportionately influenced the study findings. Also, the depression measures do not screen for bipolar depression, which may affect adherence differently than unipolar depression.
In conclusion, these findings provide further confirmation of the relationship between depression and poor ART adherence, as well as evidence that severe levels of depression and cognitive depression symptoms pose particular challenges to adherence. Furthermore, changes in depression over time were associated with corresponding changes in adherence. Our findings, together with the cited evidence that depression treatment mitigates the harmful effects of depression on adherence, support the importance of integrating mental health care into HIV programs, routine periodic screening and early detection of depression, and aggressive treatment of depression in people living with HIV.
References
Bing EG, Burnam MA, Longshore D, et al. Psychiatric disorders and drug use among human immunodeficiency virus-infected adults in the United States. Arch Gen Psychiatry. 2001; 58(8): 721–8.
Orlando M, Burnam MA, Beckman R, et al. Re-estimating the prevalence of psychiatric disorders in a nationally representative sample of persons receiving care for HIV: Results from the HIV Cost and Services Utilization Study. Int J Methods Psychiatr Res. 2002;11:75–82.
Ciesla JA, Roberts JE. Meta-analysis of the relationship between HIV infection and risk for depressive disorders. Am J Psychiatry. 2001;158:725–730.
DiMatteo MR, Lepper HS, Croghan TW. Depression is a risk factor for noncompliance with medical treatment: Meta-analysis of the effects of anxiety and depression on patient adherence. Arch Inter Med. 2000; 160(14): 2101–7.
Starace F, Ammassari A, Trotta MP, et al. Depression is a risk factor for suboptimal adherence to highly active antiretroviral therapy. J Acquir Immune Defic Syndr. 2002; 31: S136–9.
Holzemer WL, Corless IB, Nokes KM, et al. Predictors of self-reported adherence in persons living with HIV disease. AIDS Patient Care and STDs. 1999; 13(3): 185–97.
Ammassari A, Antinori A, Aloisi MS, et al. Depressive symptoms, neurocognitive impairment, and adherence to highly active antiretroviral therapy among HIV-infected persons. Psychosomatics. 2004; 45(5): 394–402.
Vranceanu AM, Safren SA, Lu M, Coady WM, Skolnik PR, Rogers WH, Wilson IB. The relationship of post-traumatic stress disorder and depression to antiretroviral medication adherence in persons with HIV. AIDS Patient Care and STDs. 2007; 22: 313–21.
Wagner GJ, Kanouse DE, Koegel P, Sullivan G. Correlates of HIV antiretroviral adherence in persons with serious mental illness. AIDS Care. 2004; 16(4): 501–6.
Tegger MK, Crane HM, Tapia KA, Uldall KK, Holte SE, Kitahata MM. The effect of mental illness, substance use, and treatment for depression on the initiation of highly active antiretroviral therapy among HIV-infected individuals. AIDS Patient Care and STDs. 2008; 22: 231–41.
Kalichman SC, Graham J, Luke W, Austin J. Perceptions of health care among persons living with HIV/AIDS who are not receiving antiretroviral medications. AIDS Patient Care and STDs. 2002; 16(5): 233–40.
Fairfield KM, Libman H, Davis RB, Eisenberg DM, Phillips RS. Delays in protease inhibitor use in clinical practice. J Gen Intern Med. 1999; 14: 446–8.
Bhatia R, Hartman C, Kallen MA, Graham J, Giordano TP. Persons newly diagnosed with HIV infection are at high risk for depression and poor linkage to care: Results from the Steps Study. AIDS Behav. 2011; 15(6):1161–1170
Hartzell JD, Spooner K, Howard R, Wegner S, Wortmann G. Race and mental health diagnosis are risk factors for highly active antiretroviral therapy failure in a military cohort despite equal access to care. J Acquir Immune Defic Syndr. 2007; 44(4): 411–6.
Bogart LM, Kelly JA, Catz SL, Sosman JM. Impact of medical and nonmedical factors on physician decision making for HIV/AIDS antiretroviral treatment. J Acquir Immune Defic Syndr. 2000; 23(5): 396–404.
Bassetti S, Battegay M, Furrer H, et al. Why is highly active antiretroviral therapy (HAART) not prescribed or discontinued? Swiss HIV Cohort Study. J Acquir Immune Defic Syndr. 1999; 21(2): 114–9.
Wood E, Montaner JS, Bangsberg DR, et al. Expanding access to HIV antiretroviral therapy among marginalized populations in the developed world. AIDS. 2003; 17(17): 2419–27.
Safren SA, O’Cleirigh CO, Tan JY, et al. A randomized controlled trial of cognitive behavioral therapy for adherence and depression (CBT-AD) in HIV-infected individuals. Health Psychol. 2009; 28: 1–10.
Wagner GJ. Placebo practice trials: the best predictor of adherence readiness for HAART among drug users? HIV Clinical Trials. 2003; 4(4): 269–81.
Wagner GJ. Predictors of antiretroviral adherence as measured by self-report, electronic monitoring, and medication diaries. AIDS Patient Care and STDs. 2002; 16(12): 599–608.
Weidle PJ, Ganea CE, Irwin KL, et al. Adherence to antiretroviral medications in an inner-city population. J Acquir Immune Defic Syndr. 1999; 22(5): 498–502.
Wagner GJ, Ryan GW. Relationship between routinization of daily behaviors and medication adherence in HIV-positive drug users. AIDS Patient Care and STDs. 2004; 18(7): 385–93.
Wing RR, Phelan S, Tate D. The role of adherence in mediating the relationship between depression and health outcomes. J Psychosom Res. 2002; 53(4): 877–81.
Antoni MH, Carrico AW, Duran RE, et al. Randomized clinical trial of cognitive behavioral stress management on human immunodeficiency virus viral load in gay men treated with highly active antiretroviral therapy. Psychosom Med. 2006; 68(1): 143–51.
Yun LW, Maravi M, Kobayashi JS, Barton PL, Davidson AJ. Antidepressant treatment improves adherence to antiretroviral therapy among depressed HIV-infected patients. J Acquir Immune Defic Syndr. 2005; 38(4): 432–8.
Turner BJ, Fleishman JA, Wenger N, et al. Effects of drug abuse and mental disorders on use and type of antiretroviral therapy in HIV-infected persons. J Gen Intern Med. 2001; 16(9): 625–33.
Walkup J, Wei W, Sambamoorthi U, Crystal S. Antidepressant treatment and adherence to combination antiretroviral therapy among patients with AIDS and diagnosed depression. Psychiatr Q. 2008; 79(1): 43–53.
Horberg MA, Silverberg MJ, Hurley LB, et al. Effects of depression and selective serotonin reuptake inhibitor use on adherence to highly active antiretroviral therapy and on clinical outcomes in HIV-infected patients. J Acquir Immune Defic Syndr. 2008; 47(3): 384–90.
Pearson CR, Simoni JM, Hoff P, Kurth AE, Martin DP. Assessing antiretroviral adherence via electronic drug monitoring and self-report: An examination of key methodological issues. AIDS Behav. 2007; 11:161–73.
Wagner GJ, Kanouse DE, Golinelli D, et al. Cognitive-behavioral intervention to enhance adherence to ART: A randomized controlled trial (CCTG 578). AIDS. 2006; 20:1295–1302.
Finocchario-Kessler S, Catley D, Berkley-Patton J, et al. Baseline predictors of ninety percent or higher antiretroviral therapy adherence in a diverse urban sample: The role of patient autonomy and fatalistic religious beliefs. AIDS Patient Care STDs. 2011;25:103–111.
Beck AT, Steer RA, Brown GK (1996) BDI-II manual. The Psychological Corporation Harcourt Brace & Company, San Antonio
Beck AT, Steer RA, Garbin MG. Psychometric properties of the Beck Depression Inventory: Twenty-five years of evaluation. Clin Psychol Rev. 1988; 8: 77–100.
Radloff LS. The CES-D scale: A self report depression scale for research in the general population. Applied Psychological Measurement. 1977; 1: 385–401.
Derogatis LR. Brief Symptom Inventory 18: Administration, scoring, and procedures manual. Minneapolis, MN: NCS Pearson, Inc. 2001.
Wichers MC, Koek GH, Robaeys G, Praamstra AJ, Maes M. Early increase in vegetative symptoms predicts IFN-α-induced cognitive-depressive changes. Psychological Med. 2005; 35:433–441.
Sunnil SB, Gelfand LA, Schmid SP, et al. Sequence of improvement in depressive symptoms across cognitive therapy and pharmacotherapy. J Affective Dis. 2008; 110:161–6.
Faustman WO, Faull KF, Whiteford HA, Borchert C, Csernansky JG. CSF 5-HIAA, serum cortisol, and age differentially predict vegetative and cognitive symptoms in depression. Biological Psychiatry. 1990; 27:311–8.
Spitznagel MB, Tremont G, Brown LB, Gunstad J. Cognitive reserve and the relationship between depressive symptoms and awareness of deficits in dementia. J Neuropsychiatry Clin Neurosci. 2006; 18:186–190.
Laird NM, Ware JH. Random-effects models for longitudinal data. Biometrics. 1982; 38: 963–974.
Diggle PJ, Liang KY, Zeger SL. The analysis of longitudinal data. Oxford University Press, Oxford, 1994.
Treisman G, Lyketsos CG, Fishman M, Hanson AL, Rosenblatt A, McHugh PR. Psychiatric care for patients with HIV infection: The varying perspectives. Psychosomatics. 1993; 34(5): 432–9.
Duran S, Spire B, Raffi F, et al. Self-reported symptoms after initiation of protease inhibitors in HIV-infected patients and their impact on adherence to HAART. HIV Clin Trials. 2001; 2:38–45.
Simoni JM, Safren SA, Manhart LE, et al. Challenges in addressing depression in HIV research: Assessment, cultural context, and methods. AIDS & Behavior. 2011; 15(2):376–388.
Tsai AC, Weiser SD, Petersen ML, Ragland K, Kushel MB, Bangsberg DR. A marginal structural model to estimate the causal effect of antidepressant medication treatment on viral suppression among homeless and marginally housed persons with HIV. Arch Gen Psychiatry. 2010; 67: 1–9.
Acknowledgments
This research was supported by the Multi-site Adherence Collaboration in HIV (MACH14) grant R01MH078773 from the National Institute of Mental Health (NIMH), Office on AIDS. The original grants of individual participating studies are: R01DA11869, R01MH54907, R01NR04749, R01NR04749, R01MH68197, R01DA13826, K23MH01862, R01MH01584, R01AI41413, R01 MH61173, NIH/NIAID AI38858, AI069419, K02DA017277, R01DA15215, NIMH P01MH49548, R01MH58986, R01MH61695, CC99-SD003, CC02-SD-003 and R01DA015679. We would like to thank all the patients who participated in each of the individual studies. The content of the paper is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Conflict of interest statement
The authors have no conflict of interest to disclose.
Author information
Authors and Affiliations
Consortia
Corresponding author
About this article
Cite this article
Wagner, G.J., Goggin, K., Remien, R.H. et al. A Closer Look at Depression and Its Relationship to HIV Antiretroviral Adherence. ann. behav. med. 42, 352–360 (2011). https://doi.org/10.1007/s12160-011-9295-8
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12160-011-9295-8