Abstract
Few studies have examined HIV testing among people who inject drugs (PWID) during the COVID-19 pandemic. This study examines factors associated with PWID who have been recently (past six months) tested for HIV during the COVID-19 pandemic. PWID were recruited between August 2020 and January 2021 from 22 drug treatment and harm reduction programs in nine states and the District of Columbia. We used logistic regression to identify correlates of recent HIV testing among PWID (n = 289). Most (52.9%) PWID reported having been recently tested for HIV. Factors associated with recent HIV testing included: having attended college [adjusted odds ratio (aOR) 2.32, 95% confidence interval (95% CI) 1.32–4.10], weekly hunger (aOR 2.08, 95% CI 1.20–3.60), crystal methamphetamine injection (aOR 2.04, 95% CI 1.05–3.97), and non-metropolitan residence (aOR 0.33, 95% CI 0.13, 0.88). Findings suggest HIV testing initiatives should be expanded during times of crisis, such as global pandemics.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
In the United States (US), HIV diagnoses linked to injection drug use (IDU) increased from 2015 to 2019 [1]. There have also been multiple IDU-associated HIV outbreaks in recent years and people who inject drugs (PWID) accounted for 10% of new HIV diagnoses in the US in 2018, underscoring the need for expanding access to comprehensive HIV prevention services [1,2,3,4,5,6]. Risks for HIV acquisition among PWID extend beyond individual-level risk behaviors (e.g., syringe sharing); for instance, many PWID have limited access to comprehensive syringe services programs (SSPs) and medications for opioid use disorder [7]. The stigmatization of substance use may also deter help-seeking behaviors among PWID [8,9,10].
Throughout the world, the COVID-19 pandemic affected every aspect of public health, including the delivery of HIV prevention services [11,12,13,14]. For example, lockdowns and social distancing practices increased risk for IDU-associated HIV transmission due to reductions in SSP utilization, sterile syringe coverage, and HIV testing [14,15,16,17,18]. Many SSPs were also short-staffed during the COVID-19 pandemic and experienced delays in funding and loss of funding opportunities [19]. A study conducted among PWID in New York (US) during COVID-19 also found higher levels of mental health issues, syringe reuse, and alcohol consumption, as well as reduced buprenorphine utilization, as compared to PWID sampled before the pandemic [15]. Recent analyses similarly found that the COVID-19 pandemic disrupted an increasing trend in preexposure prophylaxis (PrEP) prescriptions for HIV prevention in the US [20].
Given that nearly 40% of new HIV infections are transmitted by persons unaware of their infection, routine HIV testing is vital to ensuring the public health of vulnerable populations [21]. The Centers for Disease Control and Prevention (CDC) recommends that everyone between the ages of 13 and 64 be tested for HIV at least once; however, persons at higher risk, including PWID who recently shared injection equipment, should be tested at least once per year [22]. Despite this recommendation, existing literature demonstrates that PWID experience substantial barriers to HIV testing, such as: missed opportunities for testing during healthcare encounters, not knowing where to get tested, concern persons may be identified as PWID at the testing site, and stigma [5, 23, 24]. Barriers to routine HIV testing among PWID may result in delayed diagnosis, and by extension, lead to suboptimal health outcomes [25,26,27,28]. Existing research that examines HIV testing among PWID is informative, but primarily reflect studies conducted preceding the COVID-19 pandemic. Little work has comprehensively examined HIV testing among PWID during the COVID-19 pandemic. Among the literature that exists, Mistler et al. (2021), for example, found that no changes in access to HIV testing occurred during the pandemic among opioid-dependent individuals enrolled in medication for opioid use disorder treatment [29]. In contrast, a survey of syringe services programs in the US found that HIV testing diminished during the pandemic [18]. This study examines factors associated with having been recently tested for HIV among PWID residing in nine states and the District of Columbia from late 2020 to early 2021.
Methods
Study Context, Design, and Recruitment
Study participants were recruited between August 2020 and January 2021 from 22 drug treatment and harm reduction programs. Programs were primarily recruited from states participating in the Bloomberg Opioid Initiative, a campaign supported by Bloomberg Philanthropies to reduce overdose rates. Programs were geographically diverse, reflecting 9 states (Maine, Maryland, Michigan, New Jersey, New Mexico, New York, Pennsylvania, Tennessee, and West Virginia) and the District of Columbia [30]. Program staff distributed recruitment cards to clients. The recruitment cards included the study logo, a study phone number, study business hours, and a unique study identifier (used to reduce duplicate and non-client participation). Interested individuals called the study phone number listed on the recruitment cards to be screened for eligibility. Eligibile participants were at least 18 years old, currently a client of a participating organization, able to provide informed consent, and able to provide a valid, unused unique study identifier (from the recruitment card). Eligible participants then completed the survey via telephone, which took approximately one hour to complete. Participants received a $40 incentive payment, which was either mailed to an address of their choice or transmitted through the Venmo app. A total of 587 interviews were completed. Given our interest in HIV testing among PWID, we restricted the analytic sample for this analysis to participants who had injected drugs in the past 6 months and who reported both the recency of their last HIV test and not having HIV (n = 289). This research was approved by the Johns Hopkins School of Public Health Institutional Review Board.
Measures
HIV Testing in the Past 6 Months. The main outcome of interest was HIV testing in the past 6 months. Participants were asked when they had last been tested for HIV. Response options included never, in the past 3 months, 4–6 months ago, 7–12 months ago, and more than a year ago. From these responses, we created a binary indicator for being tested in the past 6 months. A 6-month timeframe was selected to best approximate HIV testing during the COVID-19 pandemic given the study recruitment timing. Further, more frequent HIV testing is recommended for persons at increased risk of disease acquisition [22].
Sociodemographic Characteristics. For demographic characteristics, participants reported their age (in years), gender, if they were single (versus in a relationship or married/separated), and their education (less than high school, high school diploma or equivalent, or some college or more). Participants reported their race and ethnicity; given sample size constraints, we combined and dichotomized these measures to non-Hispanic White and racial/ethnic minority. Participants also reported their sexual orientation, which we dichotomized to heterosexual and sexual minority (e.g., gay, lesbian, bisexual). Participants reported several measures of socioeconomic status, including: employment status (full-time, part-time, or not working), if they were currently homeless (yes/no), if they experienced hunger at least once a week since the COVID-19 pandemic (yes/no), and if they traded sex for drugs or money since the pandemic started (yes/no). Participants also reported which county they lived in. We then coded the counties with their associated National Center for Health Statistics Rural Classification Scheme (codes range from 1– large central metro to 6 – non-core). We trichotomized the resulting county designations: large metropolitan (codes 1 and 2), small metropolitan (codes 3 and 4), and non-metropolitan (codes 5 and 6).
Injection Drug Use in the Past 6 Months. Participants reported when they last injected each of 11 drugs/combinations of drugs in the past six months, including: cocaine, heroin, fentanyl, heroin and fentanyl simultaneously, speedball (cocaine and heroin simultaneously), methamphetamine, methamphetamine and heroin simultaneously, prescription opioids, tranquilizers, buprenorphine, and suboxone. Answer options for recency of injection drug use ranged from less than a week ago to never. From these data, we created binary indicators of whether participants reported having injected each drug in the past six months. Participants also reported the number of times they injected per day in the past month. Participants also reported whether they had engaged in receptive and distributive injection equipment sharing in the past six months as well as the number of people they use drugs with (none, one, two, three or more).
Service Utilization. Participants reported whether they had acquired sterile syringes from a syringe services program in the past month (yes/no). We also included two binary measures of drug treatment participation in this analysis. We created an indicator for any treatment for drug use in the past month. We then created a second indicator for if the participant reported receiving medication for opioid use disorder (MOUD; buprenorphine, methadone, or naltrexone).
Analysis
We first estimated the prevalence of being tested for HIV in the past 6 months in our sample. We then used Chi Square tests to assess relationships between each variable and HIV testing. Based on these results, we considered all variables associated with HIV testing at the p < 0.2 level for inclusion in multivariable logistic regression analyses. We excluded two injection drug use variables from the multivariable models due to small cell sizes (tranquilizer and suboxone injection). Standard errors were clustered by the venues participants were recruited from in the multivariable logistic regression model. Statistical analyses were performed using Stata 17 (StataCorp, College Station, TX).
Results
On average, participants were 39.9 years old and approximately half identified as men (Table 1). Most (61.8%) identified as non-Hispanic, White and reported not being employed (85.1%). Less than half reported: being single (46.9%), having completed high school (46.7%), and residing in a large metropolitan area (40.4%). Approximately one in four (27.0%) reported being homeless and nearly one in three (32.9%) reported weekly hunger. Regarding recent injection drug use, heroin was most commonly reported (83.3%), followed by heroin and fentanyl together (61.9%), fentanyl alone (46.7%), and crystal methamphetamine (43.1%).
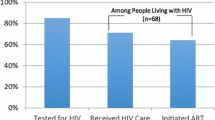
Most (52.9%) PWID reported having been tested for HIV in the past six months. Compared to PWID who had not been tested for HIV in the past six months (Table 1), those who had were significantly (p < 0.05) more likely to report being non-Hispanic White (69.1% vs. 53.7%), experience weekly hunger (41.2% and 23.5%), and having attended college (36.0% vs. 19.9%). Regarding substance use behaviors, PWID who had been tested for HIV in the past six months were more likely than those who had not been tested to report recent crystal methamphetamine injection (49.7% and 35.6%) and less likely to report suboxone injection (5.9% vs. 13.3%). As shown in Table 2, factors associated with greater odds of being tested for HIV in the past months included: having attended college [adjusted odds ratio (aOR) 2.32, 95% confidence interval (95% CI) 1.32–4.10], reporting weekly hunger (aOR 2.08, 95% CI 1.20–3.60), and recent crystal methamphetamine injection (aOR 2.04, 95% CI 1.05–3.97). As compared to residing in a large metropolitan area, living in a non-metropolitan area was associated with decreased odds of having been recently tested for HIV (aOR 0.33, 95% CI 0.13, 0.88).
Discussion
This study examines factors associated with recent HIV testing among a geographically diverse sample of PWID during the early months of the COVID-19 pandemic. Slightly more than half of our sample reported having been tested for HIV in the past six months. The prevalence of recent HIV testing among PWID in our sample underscores the importance of ensuring HIV prevention services are maintained during crises. Research has shown that the COVID-19 pandemic precipitated several consequences (i.e., diminished access to SSPs, sterile injection equipment, PrEP, MOUDs, other essential health and human services) that may increase risks for IDU-associated HIV outbreaks [11,12,13,14,15,16,17,18, 30]. Expanding access to low-threshold (i.e., minimal requirements and barriers for persons to access services) and evidence-based HIV prevention services among PWID populations should be a public health priority in communities throughout the world as diagnosing incident HIV infections is a critical step for interrupting cycles of disease transmission.
Our finding that residing in a non-metropolitan area was associated with lower odds of recent HIV testing aligns with existing research that describes how rural areas may present challenges for accessing HIV prevention services among PWID [7, 23, 31,32,33,34,35]. HIV testing services may be offered at several venues that serve PWID populations, including SSPs, drug treatment programs, homeless shelters, and in healthcare settings. However, many rural communities have limited access to these essential health and social services. Rural communities may also be characterized by substantial sociopolitical barriers that obstruct the implementation of low-threshold and evidence-based response strategies for mitigating the consequences of injection drug use [7, 36,37,38]. Additionally, rural PWID may reside in locations distal to HIV testing sites and experience transportation barriers. Rural communities throughout the US should invest in comprehensive HIV prevention services as doing so may carry substantial public health and economic benefits.
Similar to existing research, we found that greater educational attainment was associated with increased odds of recent HIV testing among PWID [39, 40]. It is plausible that persons with greater education attainment also had increased HIV risk perceptions and, as a result, were more likely to seek HIV testing. This hypothesis is supported by the literature; for example, educational attainment has been shown to have an inverse relationship with several behavioral risk factors for HIV acquisition (e.g., syringe sharing, transactional sex) [41]. Future work should be conducted to better understand how to tailor HIV prevention messaging to PWID populations with varying levels of educational attainment and underlying risk perceptions. Tailored HIV prevention messaging, however, is unlikely to be sufficient to mitigate risks for HIV acquisition unless structural changes are also enacted to ensure PWID have consistent and low-threshold access to the HIV prevention tools that best fit their lives.
Nearly one-third of PWID in our sample reported experiencing weekly hunger. This is a concerning statistic not only because it demonstrates that many PWID do not have sufficient access to a basic requirement for survival, but also because food security plays an important role in HIV prevention [42,43,44]. For example, research has shown that there is an inverse relationship between food security and syringe sharing among PWID [43]. Notably, we found that experiencing weekly hunger was associated with greater odds of recent HIV testing among our sample of PWID. One plausible explanation for this association is that many venues that provide food access also offer HIV prevention services, such as HIV testing. Another potential explanation is that the COVID-19 pandemic may have led to diminished food access, but not decreased access to HIV testing services given that they may be offered at health and social service providers that were deemed essential. This hypothesis may be explored in subsequent research as food insecurity peaked early in the pandemic, but then decreased substantially; however, it is conceivable that PWID may have sustained challenges for food access [45]. Looking ahead, communities should explore implementing complementary interventions that ensure PWID have sufficient access to healthy foods and low-threshold HIV prevention services.
More than half of PWID in our sample reported recently injecting heroin and heroin and fentanyl together, and more than 40% reported injecting fentanyl and methamphetamine. Similar to existing research, these data suggest that polysubstance injection drug use is common [33, 46,47,48,49,50]. In adjusted analyses, we found that crystal methamphetamine injection was associated with greater odds of recent HIV testing. This finding, however, should be interpreted with caution given that crystal methamphetamine injection is likely one component of a much greater profile of substance use and the combinations of substances used may vary in the degree to which they are associated with HIV testing. This idea is supported in the literature; for example, a 2020 study found that the prevalence of HIV risk behaviors and engagement in HIV prevention strategies varied across profiles of injection drug use [33]. Future scientific inquiry is warranted to better understand how to best meet the public health needs of PWID populations with diverse and evolving profiles of injection drug use.
Our finding that non-metropolitan residence was associated with decreased odds of recent HIV testing builds on research that documents diminished HIV testing engagement among persons residing in rural areas by suggesting these inequities continued into the modern era of COVID-19 [51]. Data from 2005 suggest that past-year HIV testing frequencies in urban areas were nearly double that of their rural counterparts [51]. Related analyses similarly found that HIV testing was more common in urban areas at the national, regional, and state level [52]. Studies also indicate that the stigmatization of substance use serves as a substantial impediment to accessing HIV prevention services among rural populations of people who use drugs [23]. Given the persistence of geographical disparities in HIV testing and volume of non-urban areas that are vulnerable to IDU-associated HIV outbreaks, renewed efforts are needed to ensure PWID have access to the myriad of HIV prevention strategies that exist (e.g., home-based HIV tests, PrEP, SSPs) [53]. These actions should be prioritized given that compared to urban areas, rural residence has been shown to be associated with delayed HIV diagnosis [54]. Rural residents are also more likely than their urban coutnerparts to have AIDS at time of HIV diagnosis or within one year of initial HIV diagnosis [55].
Our findings should be interpreted with consideration for relevant limitations. First, our outcome focused on HIV testing in the past six months rather than in the past year, which current HIV testing guidelines suggest for persons at increased risk [22]. Limiting our outcome to past six months allowed us to explore recency of HIV testing during the early months of the COVID-19 pandemic; however, our findings cannot speak to compliance with current HIV testing recommendations. Another limitation is that we had limited sample to explore different dimensions of geographic environment. More nuanced geographical analyses may have been possible with a larger sample. Additionally, our data have a degree of sampling bias given that we recruited persons from a limited number of substance use disorder treatment facilities and harm reduction providers that spanned nine states and the District of Columbia. Our findings may not be reflective of more geographically diverse PWID, nor the experiences of PWID who do not access substance use disorder treatment or harm reduction services. Data were also collected over several months in the early stages of the COVID-19 pandemic; during this time, mitigation strategies rapidly evolved and their implementation may have been inconsistent across communities. As a result, our data may reflect inconsistent exposure to and engagement in COVID-19 mitigation strategies. These limitations notwithstanding, our analyses make a meaningful contribution to the literature by examining factors associated with HIV testing among a geographically diverse sample of PWID during the early months of the COVID-19 pandemic.
This study documents that geographical HIV testing disparities exist among PWID and that several individual-level factors are associated with recent HIV testing. The COVID-19 pandemic affected every aspect of society, including the delivery of HIV prevention services. This study adds to the HIV prevention literature by demonstrating that HIV testing disparities persisted during the early months of the pandemic. During times of interrelated crises, communities should work to ensure essential services, including HIV testing, are preserved. Increasing access to low-threshold HIV testing services among PWID is a public health priority given that diagnosing HIV is one of the first steps of interrupting disease transmission cycles.
Data Availability
Data are available upon reasonable request.
Code Availability
Not applicable.
References
Prevention Cf.D.C.a., Diagnoses of HIV Infection in the United States and Dependent Areas 2019: Special Focus Profiles 2021.
Conrad C, et al. Community Outbreak of HIV Infection Linked to Injection Drug Use of Oxymorphone–Indiana, 2015. MMWR Morb Mortal Wkly Rep. 2015;64(16):443–4.
Rich JD, Adashi EY. Ideological Anachronism Involving Needle and Syringe Exchange Programs: Lessons From the Indiana HIV Outbreak. JAMA. 2015;314(1):23–4.
Atkins A, et al. Notes from the Field: Outbreak of Human Immunodeficiency Virus Infection Among Persons Who Inject Drugs - Cabell County, West Virginia, 2018–2019. MMWR Morb Mortal Wkly Rep. 2020;69(16):499–500.
Hershow RB, et al. Notes from the Field: HIV Outbreak During the COVID-19 Pandemic Among Persons Who Inject Drugs - Kanawha County, West Virginia, 2019–2021. MMWR Morb Mortal Wkly Rep. 2022;71(2):66–8.
Prevention Cf.D.C.a., HIV and People Who Inject Drugs 2022.
Allen ST, et al. Understanding the public health consequences of suspending a rural syringe services program: a qualitative study of the experiences of people who inject drugs. Harm Reduct J. 2019;16(1):33.
Biancarelli DL, et al. Strategies used by people who inject drugs to avoid stigma in healthcare settings. Drug Alcohol Depend. 2019;198:80–6.
Muncan B, et al. “They look at us like junkies”: influences of drug use stigma on the healthcare engagement of people who inject drugs in New York City. Harm Reduct J. 2020;17(1):53.
Paquette CE, Syvertsen JL, Pollini RA. Stigma at every turn: Health services experiences among people who inject drugs. Int J Drug Policy. 2018;57:104–10.
Moitra E, et al. Impact of the COVID-19 pandemic on HIV testing rates across four geographically diverse urban centres in the United States: An observational study. Lancet Reg Health Am. 2022;7:100159.
Menza TW, et al. The Impact of the SARS-CoV-2 Pandemic on Human Immunodeficiency Virus and Bacterial Sexually Transmitted Infection Testing and Diagnosis in Oregon. Sex Transm Dis. 2021;48(5):e59–63.
Braunstein SL, et al. Epidemiology of Reported HIV and Other Sexually Transmitted Infections During the COVID-19 Pandemic, New York City. J Infect Dis. 2021;224(5):798–803.
Hill BJ, Anderson B, Lock L. COVID-19 Pandemic, Pre-exposure Prophylaxis (PrEP) Care, and HIV/STI Testing Among Patients Receiving Care in Three HIV Epidemic Priority States. AIDS Behav. 2021;25(5):1361–5.
Aponte-Melendez Y, et al. The impact of COVID-19 on people who inject drugs in New York City: increased risk and decreased access to services. Harm Reduct J. 2021;18(1):118.
Whitfield M, et al. The impact of COVID-19 restrictions on needle and syringe programme provision and coverage in England. Int J Drug Policy. 2020;83:102851.
Frost MC, et al. Program Adaptations to Provide Harm Reduction Services During the COVID-19 Pandemic: A Qualitative Study of Syringe Services Programs in the U. S AIDS Behav. 2022;26(1):57–68.
Glick SN, et al. The Impact of COVID-19 on Syringe Services Programs in the United States. AIDS Behav. 2020;24(9):2466–8.
Wenger LD, et al. Ingenuity and resiliency of syringe service programs on the front lines of the opioid overdose and COVID-19 crises. Transl Res. 2021;234:159–73.
Huang YA, et al. Impact of COVID-19 on HIV Preexposure Prophylaxis Prescriptions in the United States - A Time Series Analysis. Clin Infect Dis; 2022.
Prevention C.f.D.C.a., HIV Testing 2020.
Prevention Cf.D.C.a., Should I get tested for HIV? 2021.
Basta TB, Stambaugh T, Fisher CB. Efficacy of an Educational Intervention to Increase Consent for HIV Testing in Rural Appalachia. Ethics Behav. 2015;25(2):125–49.
Furukawa NW, et al. Missed Opportunities for Human Immunodeficiency Virus (HIV) Testing During Injection Drug Use-Related Healthcare Encounters Among a Cohort of Persons Who Inject Drugs With HIV Diagnosed During an Outbreak-Cincinnati/Northern Kentucky, 2017–2018. Clin Infect Dis. 2021;72(11):1961–7.
May M, et al. Impact of late diagnosis and treatment on life expectancy in people with HIV-1: UK Collaborative HIV Cohort (UK CHIC) Study. BMJ. 2011;343:d6016.
Tang H, et al. “Late for testing, early for antiretroviral therapy, less likely to die”: results from a large HIV cohort study in China, 2006–2014. BMC Infect Dis. 2018;18(1):272.
Gheibi Z, et al. Determinants of AIDS and non-AIDS related mortality among people living with HIV in Shiraz, southern Iran: a 20-year retrospective follow-up study. BMC Infect Dis. 2019;19(1):1094.
Ang LW, et al. Short-term mortality from HIV-infected persons diagnosed from 2012 to 2016: Impact of late diagnosis of HIV infection. Med (Baltim). 2021;100(26):e26507.
Mistler CB, et al. The Impact of COVID-19 on Access to HIV Prevention Services Among Opioid-Dependent Individuals. J Community Health. 2021;46(5):960–6.
Saloner B, et al. Experiences with substance use disorder treatment during the COVID-19 pandemic: Findings from a multistate survey. Int J Drug Policy. 2021;101:103537.
McKenney J, et al. HIV Risk Behaviors and Utilization of Prevention Services, Urban and Rural Men Who Have Sex with Men in the United States: Results from a National Online Survey. AIDS Behav. 2018;22(7):2127–36.
Fadanelli M, et al. A qualitative study on pharmacy policies toward over-the-counter syringe sales in a rural epicenter of US drug-related epidemics. Harm Reduct J. 2022;19(1):1.
Schneider KE, et al. The Relationship Between Polysubstance Injection Drug Use, HIV Risk Behaviors, and Interest in Pre-Exposure Prophylaxis (PrEP) Among People Who Inject Drugs in Rural West Virginia. J Stud Alcohol Drugs. 2020;81(6):740–9.
Allen ST, et al. Human Immunodeficiency Virus Testing Among People Who Inject Drugs in Rural West Virginia. J Infect Dis. 2020;222(Suppl 5):S346-s353.
Allen ST, et al. Barriers and Facilitators to PrEP Use Among People Who Inject Drugs in Rural Appalachia: A Qualitative Study. AIDS Behav. 2020;24(6):1942–50.
Beachler T, et al. Community Attitudes Toward Opioid Use Disorder and Medication for Opioid Use Disorder in a Rural Appalachian County. J Rural Health. 2021;37(1):29–34.
Zeller TA, et al., Attitudes toward syringe exchange programs in a rural Appalachian community. J Addict Dis, 2021: p. 1–8.
Ibragimov U, et al. Factors that influence enrollment in syringe services programs in rural areas: a qualitative study among program clients in Appalachian Kentucky. Harm Reduct J. 2021;18(1):68.
Bayani A, et al. Factors associated with HIV testing among people who inject drugs: a meta-analysis. J Addict Dis. 2020;38(3):361–74.
Smith MK, et al. Overlap between harm reduction and HIV service utilisation among PWID in India: Implications for HIV combination prevention. Int J Drug Policy. 2018;57:111–8.
Hasnain M, et al. Association of educational attainment with HIV risk in African American active injection drug users. AIDS Care. 2007;19(1):87–91.
Strike C, et al. Frequent food insecurity among injection drug users: correlates and concerns. BMC Public Health. 2012;12:1058.
Rouhani S, et al. Food access among people who inject drugs in West Virginia. Harm Reduct J. 2021;18(1):90.
Shannon K, et al. Severe food insecurity is associated with elevated unprotected sex among HIV-seropositive injection drug users independent of HAART use. Aids. 2011;25(16):2037–42.
America F, The Impact of the Coronavirus on Food Insecurity in 2020 & 2021 2021.
Schneider KE, et al. Patterns of polysubstance use and overdose among people who inject drugs in Baltimore, Maryland: A latent class analysis. Drug Alcohol Depend. 2019;201:71–7.
Schneider KE, et al. Trends in substances involved in polysubstance overdose fatalities in Maryland, USA 2003–2019. Drug Alcohol Depend. 2021;223:108700.
Schneider KE, et al. Polysubstance use in rural West Virginia: Associations between latent classes of drug use, overdose, and take-home naloxone. Int J Drug Policy. 2020;76:102642.
Karamouzian M, et al. Latent patterns of polysubstance use among people who use opioids: A systematic review. Int J Drug Policy. 2022;102:103584.
Rivera Saldana CD, et al. Risk of non-fatal overdose and polysubstance use in a longitudinal study with people who inject drugs in Tijuana, Mexico. Drug Alcohol Rev. 2021;40(7):1340–8.
Ohl ME, Perencevich E. Frequency of human immunodeficiency virus (HIV) testing in urban vs. rural areas of the United States: results from a nationally-representative sample. BMC Public Health. 2011;11:681.
Tran L, Tran P, Tran L. Influence of Rurality on HIV Testing Practices Across the United States, 2012–2017. AIDS Behav. 2020;24(2):404–17.
Van Handel MM, et al. County-Level Vulnerability Assessment for Rapid Dissemination of HIV or HCV Infections Among Persons Who Inject Drugs, United States. J Acquir Immune Defic Syndr. 2016;73(3):323–31.
Weis KE, et al. Associations of rural residence with timing of HIV diagnosis and stage of disease at diagnosis, South Carolina 2001–2005. J Rural Health. 2010;26(2):105–12.
Weissman S, et al. Rural-urban differences in HIV viral loads and progression to AIDS among new HIV cases. South Med J. 2015;108(3):180–8.
Acknowledgements
The authors gratefully acknowledge the assistance of colleagues at Vital Strategies and Pew Charitable Trusts, the study advisory board, and programs that helped distribute client cards. Most importantly, we are grateful to our study participants.
Funding
The study was supported by Bloomberg Philanthropies. STA is also supported by the National Institutes of Health (K01DA046234). The funders were not involved in the collection of study data, the drafting of the manuscript, or the decision to submit the study for publication.
Author information
Authors and Affiliations
Contributions
All authors were involved in the conception of the analyses. All authors were involved in the interpretation of the findings. All authors were involved in drafting the manuscript. All authors reviewed and approved the final manuscript.
Corresponding author
Ethics declarations
Conflicts of interest/Competing Interests
None of the authors have any conflicts of interest.
Ethics Approval
All study procedures were approved by the Johns Hopkins University Bloomberg School of Public Health Institutional Review Board.
Consent to Participate
Eligible participants provided oral consent to participate.
Consent for Publication
We consent to publishing our manuscript.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Allen, S.T., Schneider, K.E., Morris, M. et al. Factors Associated with HIV Testing Among People Who Inject Drugs: Findings from a Multistate Study at the Start of the COVID-19 Pandemic. AIDS Behav 27, 1674–1681 (2023). https://doi.org/10.1007/s10461-022-03899-9
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10461-022-03899-9