Abstract
In the US, HIV testing has been key in the identification of new HIV cases, allowing for the initiation of antiretroviral treatment and a reduction in disease transmission. We consider the influence of living in a rural area (rurality) on HIV testing between different US regions and states as existing work in this area is limited. Using the 2012–2017 Behavioral Risk Factor Surveillance Systems surveys, we explored the independent role of rurality on having ever been tested for HIV and having a recent HIV test at the national, regional, and state levels by calculating average adjusted predictions (AAPs) and average marginal effects (AMEs). Suburban and urban areas had higher odds and AAPs of having ever been tested for HIV and having a recent HIV test compared to rural areas across the US. The Midwest had the lowest AAPs for both having ever been tested for HIV (17.57–20.32%) and having a recent HIV test (37.65–41.14%) compared to other regions. For both questions on HIV testing, regions with the highest AAPs had the greatest rural–urban differences in probabilities and regions with the lowest AAPs had the smallest rural–urban difference in probabilities. The highest rural–urban testing disparities were observed in states with high AAPs for HIV testing. HIV testing estimates were higher in urban compared to rural areas at the national, regional, and state level. This study examines the isolated influence of rurality on HIV testing and identifies specific US areas where future efforts to increase HIV testing should be directed to.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
In the US, over 1.1 million adults and adolescents currently live with HIV and an estimated 40,000–50,000 new HIV infections occur annually [1,2,3,4,5]. About 1 in 7 individuals infected with HIV do not know that they carry the virus [1, 6]. HIV infected individuals who are unaware of their status and continue to engage in risky sexual activity contribute to 93% of new HIV infections each year [7,8,9]. Early HIV detection allows people to start antiretroviral treatment (ART) while their CD4 counts are still high, which has led to dramatically improved long-term outcomes and similar life expectancies to individuals without HIV [10,11,12,13,14]. Thus, it is crucial for sexually active individuals to undergo routine HIV testing in order to start ART as soon as possible after they are infected with HIV [15,16,17,18].
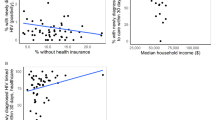
Despite slowly rising rates of HIV testing and a decrease in new infections each year among the general population, HIV testing remains disproportionately low among certain subgroups such as adolescents, older adults, and rural residents [19,20,21,22,23]. Lack of healthcare access, fears about HIV risk and stigma, misconceptions about treatment, and the exclusion of HIV testing from routine medical care have been identified as the four key barriers that result in less than half of Americans getting tested in their lifetime [2, 24,25,26]. Existing research on the impact of living in a rural area (rurality) on HIV testing at the national and state level indicates that rural–urban differences in high HIV-transmission risk behaviors and access to HIV prevention and treatment may contribute to differences in HIV testing rates between rural and urban areas that range from 5.4 to 15.4% [27,28,29,30,31,32,33,34,35,36]. However, these works have been limited by non-contemporaneous data that is not indicative of current HIV prevalence, examination of testing at only a single geographic scale within a study, and the inability to directly compare HIV testing rates between US regions and states [27,28,29,30,31].
Our study extensively examined differences in HIV testing between rural and urban residents at the state, regional, and national scale by using contemporary nationally representative HIV data [27,28,29,30,31]. We isolated the independent role of rurality on HIV testing while controlling for sociodemographic, clinical, and health seeking behavioral factors through marginal effects. Keeping in line with previous studies on the influence of rurality on HIV testing, we hypothesized that rural residents would have lower rates of HIV testing at the state, regional, and national level compared to urban residents [27,28,29,30,31]. The results of this study allowed us to identify specific rural/urban areas with HIV testing disparities across the US and make direct comparisons of HIV testing estimates at the state, regional, and national level which can be used to guide development of future public health interventions.
Methods
Study Sample
We used the Centers for Disease Control and Prevention’s (CDC) nationally representative Behavioral Risk Factor Surveillance System (BRFSS) surveys from 2012 to 2017 [37,38,39,40,41,42]. The BRFSS is a landline and cell phone conducted survey that collects information on the health behaviors and chronic conditions of residents in all 50 states and the District of Columbia [37,38,39,40,41,42]. Potential survey participants are contacted through commercially available phone lists from Genesys, Inc. [43]. As some minority groups and rural residents are less likely to have access to telephones and cell phones, oversampling and raking adjustments are carried out in the BRFSS to ensure these groups are well represented [43, 44].
We combined data from the six most recent BRFSS surveys to maximize the sample size and increase the power of our analyses. BRFSS surveys from 2010 and earlier were not included because they used post stratification weighting, which is incompatible with the iterative proportional fitting of the 2012-2017 surveys [45,46,47]. The datasets are publicly available for download at the CDC’s website (https://www.cdc.gov/brfss/annual_data/annual_data.htm) [38].
Our study was comprised of survey participants ≥ 18 year who responded to two questions in the HIV/AIDS section of the BRFSS (section 18 in the 2012 and 2014 surveys, section 16 in the 2013 and 2017 surveys, section 15 in the 2015 survey, section 19 in the 2016 survey) [45,46,47]. Specifically, we included individuals in our study who responded to, “Have you ever been tested for HIV? Do not count tests you may have had as part of a blood donation. Include testing fluid from your mouth.” (n = 2,509,103), and “Not including blood donations, in what month and year was your last HIV test?” (n = 399,067 out of 755,726 who answered “Yes” to the previous question) [45,46,47]. Given that the median delay from infection to diagnosis was 3 years, we classified anyone who had received an HIV test in the last 3 years at the time of survey as “recent”, while those who had not were labeled “not recent” [48]. Responses to these two questions allowed us to separate the sample of respondents into those who had never received HIV testing (n = 1,753,377), those who had received HIV testing but have not kept up regular screenings (last screening more than 3 years ago) (n = 185,629), and those who maintain a regular screening schedule (n = 213,438). For both questions, we excluded respondents who answered “don’t know/not sure” or refused to answer.
Covariates
We included multiple sociodemographic, clinical, and health seeking behavioral factors in our analyses that have either been shown to be associated with HIV in numerous studies or are associated with testing [49,50,51,52,53,54,55,56,57,58,59,60,61,62,63,64,65,66,67,68,69,70,71,72,73]. By including these factors as covariates in our analyses, we are able to control to a large degree any confounding that could bias the association between rurality and HIV testing [74, 75]. We finely categorized all the sociodemographic, clinical, and health seeking behavioral covariates in our study to minimize any residual confounding due to coarse categorization, an issue that has arisen in previous studies on rurality and HIV testing [31, 74, 76, 77]. All covariates in the study were categorical and consisted of age, household income, educational attainment, self-reported race, general health status, body mass index (BMI) categories, health care coverage, personal doctor/health care provider, and marital status [45,46,47].
We used the Metropolitan Status Codes (MSCODE) in each survey to classify respondents as either rural, suburban, or urban residents [45,46,47]. Rural residents were those who do not live in a metropolitan statistical area (MSA) (MSCODE 5), suburban residents were those who live inside a suburban county of the MSA (MSCODE 3), and urban residents were those who live in the center city of an MSA (MSCODE 1) or outside the center city of an MSA but inside the county containing the center city (MSCODE 2) [45,46,47]. Living in an MSA that has no center city (MSCODE 4) was only available in the 2012 and 2013 BRFSS surveys and was very small compared to other categories in the same survey and the overall study sample [37, 45]. Due to the small number of MSCODE 4 individuals (n = 3629 for “Have you ever been tested for HIV?”, n = 507 for “How recent is your last HIV test?”) we do not discuss results pertaining to MSCODE 4, although it was included in our analysis.
Statistical Models
We accounted for the complex survey design and unequal weighting using survey weights in logistic regression models that evaluated the relationship between HIV testing and rurality (MSCODE) while controlling for the sociodemographic, clinical, and health seeking behavioral factors mentioned earlier. Two logistic regression models were run in this study, one for “Have you ever been tested for HIV?” (HIVTST) with “Yes” as the outcome and the other for “How recent is your last HIV test?” (WHENLAST) with “3 years or less” as the outcome [78]. The two logistic models controlled for the same covariates but had different sample sizes (as only respondents who had ever been tested for HIV could answer about its recency). The sample sizes for these two models were 2,509,103 and 399,067 individuals respectively. All logistic models were run in SAS 9.4 [79].
No subgroup analyses were conducted for groups that are at high risk for HIV infection such as Men who have Sex with Men (MSM) and injection drug users due to the manner the BRFSS is structured and administered [40, 41, 44, 80,81,82,83]. For instance, we would not be able to capture heterosexual men who have sex with men in MSM and it would be impossible to figure out which individuals actually are injection drug users as the BRFSS question on drug use is a composite question on a variety of high risk HIV situations [40, 41, 44, 84, 85]. Additionally, the ability to carry out subgroup analyses is hindered by the already small sample size of MSM in BRFSS surveys before data cleaning (MSM: ~ 1.5% of survey population) [40, 41, 44, 80,81,82,83, 85].
Marginal Probabilities
After fitting the two logistic regression models, we calculated Average Adjusted Predictions (AAPs), a type of marginal probability, for the two questions on HIV testing (HIVTST and WHENLAST) [86, 87]. In this case, AAPs attempt to control for the other sociodemographic, clinical, and health seeking behavioral factors by considering a hypothetical respondent population with no variation in these factors [87]. For example, the rural AAP is the predicted marginal probability of either having ever been tested for HIV or a recent last HIV test where the survey population was hypothetically all residing in rural areas [87]. We chose to calculate AAPs in addition to odds ratios due to the values of AAPs being given in absolute numerical values, allowing for the presentation of our actual estimated testing probabilities and more practical interpretation of state-by-state testing differences [87]. Essentially, marginal probabilities can be thought of as odds ratios, where all the covariates have been held constant. AAPs allow us to isolate the association between rurality, each sociodemographic, clinical, and health seeking behavioral factor, and HIVTST or WHENLAST when all other factors are held constant in the logistic regression models for rural, suburban, and urban areas in each of the 50 states [86, 87]. Furthermore, we also calculated the urban/suburban versus rural AAP differences, known as average marginal effects (AMEs), with respect to HIVTST and WHENLAST in each state [86, 87]. In this study, an AME is the difference in the probability of people who have ever been tested for HIV or had a recent last HIV test between a hypothetically all suburban or urban survey population and a hypothetically all rural one [87]. Stata 15 was used to calculate both AAPs and AMEs [88].
Regional and National Level Analyses
We used the same US Census regions in our study as used by other studies on the influence of rurality on HIV testing [31, 89]. The four regions were the Northeast (Connecticut, Maine, Massachusetts, New Hampshire, New Jersey, New York, Pennsylvania, Rhode Island, Vermont), the Midwest (Illinois, Indiana, Iowa, Kansas, Michigan, Minnesota, Missouri, Nebraska, North Dakota, Ohio, South Dakota, Wisconsin), the South (Alabama, Arkansas, Delaware, District of Columbia, Florida, Georgia, Kentucky, Louisiana, Maryland, Mississippi, North Carolina, Oklahoma, South Carolina, Tennessee, Texas, Virginia, West Virginia), and the West (Alaska, Arizona, California, Colorado, Hawaii, Idaho, Montana, Nevada, New Mexico, Oregon, Utah, Washington, Wyoming) [89]. In order to obtain regional level estimates of HIV testing for each MSCODE, we averaged together the marginal probabilities for each of the states in the respective region. National level estimates of HIV testing for rural, suburban, and urban areas were calculated by using all study participants who met the study’s eligibility criteria from 2012 to 2017 BRFSS surveys.
Results
The people who responded to having ever been tested for HIV were predominantly ≥ 45 years (73.0%), female (58.2%), had an income ≥ $25,000 (61.7%), White (76.7%), had at least a high-school education (92%), reported that they felt good to excellent about their general health (81%), had healthcare coverage (90.9%), and a personal doctor (84.5%) (Table 1). BMI was roughly evenly split between normal weight (32.4%), overweight (36.1%), and obese (29.8%). The majority of these people reported either living in the center city of an MSA (33.6%) or not in an MSA at all (33.7%). People who responded to the recency of their last HIV test were mainly 25–54 years (67.0%), female (56.7%), had an income ≥ $25,000 (72.9%), had at least a high-school education (93.5%), reported that they felt good to excellent about their general health (81.8%), had healthcare coverage (87.4%), and a personal doctor (79.7%).
In national level results of both having ever been tested for HIV and having a last HIV test ≤ 3 years ago; men had higher odds compared to women, those earning < $15,000 had the highest odds compared to those earning ≥ $50,000, Blacks had the highest odds compared to Whites, those with poor health had the highest odds compared to those with excellent health, those with more than one personal doctor/health care provider had the highest odds compared to those with only one, and current smokers had higher odds compared to non-smokers (Table 2). Except for smoking status, all of these associations were statistically significant with p values < 0.05. Overall, we observed that the odds of having ever been tested for HIV and having a last HIV test ≤ 3 years ago tended to decrease as reported income increased, while the odds of having a last HIV test ≤ 3 years ago declined with increasing education level. Blacks, Hispanics, and those who reported other races all had higher odds of both having ever been tested for HIV and a last HIV test ≤ 3 years ago compared to Whites. In addition, suburban and urban residents had higher odds of having ever been tested for HIV and a last HIV test ≤ 3 than rural residents across the US.
At the national level, people who lived in urban (MSCODE 1 and 2) and suburban (MSCODE 3) areas had a higher probability of having ever been tested for HIV [AAPs: MSCODE 1: 28.26% (95% CI 28.04–28.49%); MSCODE 2: 26.52 (95% CI 26.23–26.82%); and MSCODE 3: 25.82% (95% CI 25.46–26.18%)] compared with residents in rural area (AAP MSCODE 5: 24.92% (95% CI 24.64–25.21%)). Urban and suburban residents also had a higher probability of having a recent HIV test [AAPs: MSCODE 1: 47.81% (95% CI 47.15–48.48%); MSCODE 2: 46.29% (95% CI 45.38–47.21%); and MSCODE 3: 45.83% (95% CI 44.72–46.94%)] compared to those residing in rural areas [AAP MSCODE 5: 44.28% (95% CI: 43.34–45.21%)]. There was the greatest difference in probability of having ever been tested for HIV between those living In the center city of an MSA (MSCODE 1) and those not living in an MSA (MSCODE 5) (AME: 3.34%) and the smallest difference between those living inside a suburban county of the MSA (MSCODE 3) and those not living in an MSA (MSCODE 5) (AME: 0.9%) (Table 3). For recency of last HIV test, the largest difference in probability was between those living in the center city of an MSA (MSCODE 1) and those not living in an MSA (MSCODE 5) (AME: 3.54%) and the smallest between those living inside a suburban county of the MSA (MSCODE 3) and those not living in an MSA (MSCODE 5) (AME: 1.55%).
Regionally, the Northeast had the highest probability of people having ever been tested for HIV for all MSCODE areas (AAP: 25.65–29.12%) and the Midwest had the lowest (AAP: 17.57–20.32%) (Table 4). The region with the highest probability of people having a recent HIV test was the South for all MSCODE areas (AAP: 49.71–53.32%) and the region with the lowest probability was the Midwest (AAP: 37.65–41.14%). The states with the greatest probability of people having ever been tested for HIV are Alaska (AAP: 35.19–39.32%), Maryland (AAP: 34.37–38.27%), and New York (AAP: 34.28–38.21%) while South Dakotas (AAP: 14.74–17.18%), North Dakota (AAP: 14.72–17.19%), and Utah (AAP: 14.75–17.26%) are the states with the smallest probability. Mississippi (AAP: 61.55–64.9%), Louisiana (AAP: 57.45–60.91%), and North Carolina (AAP: 56.14–59.67%) had the greatest probability of people having a recent HIV test while Wisconsin (AAP: 28.05–31.16%), Maine (AAP: 29.21–32.45%), and Idaho (AAP: 29.34–32.52%) had the smallest probability.
Discussion
We conducted a nationally representative study using 2012–2017 BRFSS to examine the influence of rurality on HIV testing. At the national level, suburban and urban areas had higher odds and AAPs of having ever been tested for HIV and having a recent HIV test compared to rural areas across the US. Compared to other regions, the Midwest had the lowest AAPs for both having ever been tested for HIV (17.57–20.32%) and a recent HIV test (37.65–41.14%). For both having ever been tested for HIV and having a recent HIV test, regions with the highest probabilities had the greatest difference in probabilities between rural and urban areas and regions with the lowest probabilities had the smallest difference in probabilities between rural and urban areas. In addition, the highest rural–urban testing disparities were observed in states with high AAPs for having ever been tested for HIV and having a recent HIV test. HIV testing odds ratios and AAPs, with regard to having ever been tested for HIV and having a recent HIV test, were higher in urban compared to rural areas at the national level and in all regions and states.
Past work on the influence of rurality on HIV testing has tended to focus on this research question at one geographic scale [28,29,30,31]. A Texas study of 9744 people in 2010 found that Whites who did not live in a MSA were less likely to have ever been tested for HIV compared to those who lived in the central city of a MSA [28, 29]. In two national level studies, one using the 2005 and 2009 BRFSS and the other the 2015 BRFSS, rural residents were found to be significantly less likely than urban residents to have ever been tested for HIV and for their last HIV test to have been recent [30, 31]. While our results are consistent with past research highlighting rural–urban disparities in HIV testing, the magnitude of our differences in HIV testing rates between rural and urban areas, AME: 3.4 and 1.6%, are smaller than those reported in previous studies [27,28,29,30,31]. This study’s lower differences in HIV testing rates between rural and urban areas may be attributed to our ability to adjust extensively for sociodemographic, clinical, and health seeking behavioral factors compared to other studies, reducing the impact of these factors’ bias on study estimates [27,28,29,30,31]. Our results also bring to light exceptionally high HIV testing rates in states such as Alaska which could be explained by the state’s high chlamydia (highest in the US) and gonorrhea (2nd highest in the US) incidence rates [90]. The behaviors that lead to chlamydia and gonorrhea infections and the lesions and sores that are a product of these diseases are associated with a higher risk of becoming HIV infected [90,91,92,93].
We believe that the rural–urban HIV testing disparity observed in our study centers on two distinct points: (1), differences in high HIV-transmission risk behaviors between rural and urban areas and (2) differences in access to HIV prevention and treatment resources between rural and urban areas [32]. In Florida, adolescent rural residents were more likely to report that they intended to have sex without a condom in the future than urban residents [34]. Rural men who use the internet to meet partners online were more likely to report unprotected anal intercourse in their last sexual episode compared to urban men [33]. Although the prevalence of illicit drug use is consistently higher in urban compared to rural areas, urban residents tend to have greater access to treatment facilities, in terms of availability and standard of care, than rural residents [35, 36]. Regarding differences in access to HIV prevention and treatment resources between rural and urban areas, a study of US rural and urban individuals with HIV found that not only did many rural residents with HIV have to travel to urban medical centers in order to receive Highly Active Antiretroviral Therapy (HAART), but that on average rural residents with HIV had fewer outpatient visits for HIV care compared to urban residents with HIV [32]. In addition, this same study observed that rural injection drug users were more likely to have fewer visits for HIV care compared to their urban counterparts [32]. However, pinpointing whether differences in high HIV-transmission risk behaviors between rural and urban areas, differences in access to HIV prevention and treatment resources between rural and urban areas, or both are behind the rural–urban HIV testing disparity is beyond the scope of the BRFSS data and this issue warrants further study.
It is important to distinguish between the statistical and clinical significance of our results and establish what they mean in practical terms, especially because their magnitude is less than that found in earlier and smaller-scale studies [27,28,29,30,31, 94]. Although it is true that the calculated differences in AAPs between the most urban and most rural areas for both having ever had a HIV test having had a recent HIV test are relatively small in magnitude, they are consistent in their strength and direction across multiple levels of granularity [27,28,29,30,31]. Furthermore, keeping in mind that even the finest scale we considered, the state, still encompasses millions of adult individuals, the approximate 3–4% difference in AAPs still corresponds to tens, if not hundreds of thousands of people [95]. For example, a 3.66% (MSCODE 1 and 5) and 1.76% (MSCODE 2 and 5) difference in AAP for having ever had a HIV test between rural and urban areas in Georgia, the state with the highest HIV infection rate and with a rural population of 2,415,502 in the 2010 Census, translates into approximately 88,000 and 42,500 more rural residents who would receive HIV tests if they had lived in urban and suburban areas, respectively [95, 96].
Our study has several limitations that need to be considered. Data in the BRFSS is obtained through self-report, so it is likely that some misclassification of health status, race, ethnicity, education, age, and income exists [37,38,39]. While there is no way of ascertaining the accuracy of the entire self-reported BRFSS dataset, several studies have shown that the correlations between in person measurements of clinical factors (obesity, smoking, diabetes) and BRFSS responses ranged from 74 to 82% [97]. In addition, a study comparing Massachusetts electronic health records (EHR) to Massachusetts BRFSS responses found that prevalence of diabetes (EHR: 9.4%, BRFSS: 9.7%), smoking (EHR: 13.5%, BRFSS: 14.7%), hypertension (EHR: 26.3%, BRFSS: 29.6%), and obesity (EHR: 22.8%, BRFSS: 23.8%) was very similar between the two data sources [98]. Another BRFSS validation study that examined the correlation between self-reported BMI with in clinic BMI measurements found that among men the correlation was R2 = 0.89 and among women R2 = 0.92 [99]. Therefore, we feel any issues concerning accuracy of self-report to be minor, if not negligible. Minor loss of accuracy due to self-report will likely result in minimal non-differential misclassification bias [100]. Although we controlled for a large array of sociodemographic and clinical covariates in our analysis, it is possible some residual confounding remains. However, we included all of the covariates included in other studies on rurality and HIV testing in our analyses except for whether an individual was a member of a sexual minority group, as this information was not available in the 2012 BRFSS [27, 28, 30, 31, 72]. While we did not include this covariate in our analysis, sensitivity analyses conducted by Henderson et al. in their work on the influence of rurality on HIV testing indicated there was negligible differences in results between models that included whether an individual was a member of a sexual minority group and those that did not [31]. We are unable to conduct subgroup analyses for high risk HIV groups such as MSM and injection drug users. This is largely inherent to the nature of how BRFSS survey questions are structured and conducted as well as the small sample size of these subgroups [40, 41, 44, 85].
We would also like to note the limitations in our usage of two operational definitions integral to our model, that of what constitutes “recent” and what constitutes the cutoffs between “urban, rural, and suburban”. It is possible that using alternative definitions (such as reducing the cutoff for recency or using USDA Rural–Urban Continuum Codes) may change study findings, but our usage of these definitions in this study is well justified. Although it is true that sexually active individuals have possibly engaged in intercourse later than the 3 year cutoff that we have defined for “recent HIV test”, 3 years corresponds with how the CDC defines “recency” within this survey, and accounts for any further or continuing testing within this timeframe [40, 41, 85]. With respect to our choice of Metropolitan Status Codes, the division of the codes clearly delineates the cutoff between urban versus suburban versus rural, whereas the choice is not as immediately apparent with Rural–Urban Continuum codes (for example, many urban populations in nonmetro counties have higher populations than metro counties in continuum codes) [40, 41, 85, 101].
Compared with previous research that examines the influence of rurality on HIV testing, our large nationwide study allows us to isolate the association between rurality and HIV testing practices at multiple geographic scales after taking major sociodemographic and clinical factors that influence HIV risk and health seeking behaviors into account [27,28,29,30,31, 72]. Combining the 2012–2017 BRFSS surveys gives us a large study population and adequate power for our analyses. By using survey weights and oversampling in the study population, we are able to obtain more precise estimation within the subpopulations of interest (different MSCODEs at regional and state level). Additionally, the use of marginal effects allows for easier direct comparisons of HIV testing probabilities, especially for the factors where the choice of level that odds ratios are computed against is arbitrary or not immediately clear, as with state or region. Finally, the use of MSCODE as the classification for rural, suburban, and urban areas allows for an ordinal scale that distinctly separates places by degree of rurality.
Conclusion
This study sought to determine if there are disparities in HIV testing between suburban/urban and rural residents and whether they vary across the US. Our results indicated the existence of suburban/urban–rural disparities in HIV testing at the national, regional, and state levels. Regions and states where HIV testing estimates were far below the national average can use this study’s findings to motivate the implementation of HIV testing initiatives that well-performing states already have in place. This will increase the number of HIV cases that can be detected early, improve the lives of the already infected via prompt antiretroviral treatment, and ultimately reduce future HIV cases.
References
CDC. Estimated HIV incidence and prevalence in the United States, 2010–2015. HIV Surveill Suppl Rep. 2018;23(1):1.
CDC. Estimates of new HIV infections in the United States: CDC HIV/AIDS Facts. 2016; http://www.cdc.gov/hiv/topics/surveillance/resources/factsheets/pdf/incidence.pdf. Accessed 2 April 2018.
Kaiser Family Foundation. The HIV/AIDS epidemic in the United States: the basics. 2018; https://www.kff.org/hivaids/fact-sheet/the-hivaids-epidemic-in-the-united-states-the-basics/. Accessed 27 Aug 2018.
Secretary’s Minority AIDS Initiative Fund U.S. Statistics; 2018. https://www.hiv.gov/hiv-basics/overview/data-and-trends/statistics. Accessed 27 Aug 2018.
CDC. HIV in the United States: at a glance. 2018; https://www.cdc.gov/hiv/statistics/overview/ataglance.html. Accessed 27 Aug 2018.
Campsmith ML, Rhodes PH, Hall HI, Green TA. Undiagnosed HIV prevalence among adults and adolescents in the United States at the end of 2006. J Acquir Immune Defic Syndr. 2010;53(5):619–24.
CDC. Monitoring selected national HIV prevention and care objectives by using HIV surveillance data—United States and 6 dependent areas, 2016. HIV Surveill Suppl Rep. 2018;23(4).
CDC. HIV surveillance report, 2016. 2017; http://www.cdc.gov/hiv/library/reports/hiv-surveillance.html.
Marks G, Crepaz N, Janssen RS. Estimating sexual transmission of HIV from persons aware and unaware that they are infected with the virus in the USA. AIDS. 2006;20(10):1447–50.
Rutstein SE, Ananworanich J, Fidler S, et al. Clinical and public health implications of acute and early HIV detection and treatment: a scoping review. J Int AIDS Soc. 2017;20(1):21579.
Eaton LA, Kalichman SC. Changes in transmission risk behaviors across stages of HIV disease among people living with HIV. J Assoc Nurses AIDS Care. 2009;20(1):39–49.
Rosenberg NE, Pilcher CD, Busch MP, Cohen MS. How can we better identify early HIV infections? Curr Opin HIV AIDS. 2015;10(1):61–8.
Smith MK, Rutstein SE, Powers KA, et al. The detection and management of early HIV infection: a clinical and public health emergency. J Acquir Immune Defic Syndr. 2013;63(2):S187–99.
Teeraananchai S, Kerr SJ, Amin J, Ruxrungtham K, Law MG. Life expectancy of HIV-positive people after starting combination antiretroviral therapy: a meta-analysis. HIV Med. 2016;18(4):256–66.
Dieffenbach CW, Fauci AS. Universal voluntary testing and treatment for prevention of HIV transmission. JAMA. 2009;301(22):2380–2.
Granich RM, Gilks CF, Dye C, De Cock KM, Williams BG. Universal voluntary HIV testing with immediate antiretroviral therapy as a strategy for elimination of HIV transmission: a mathematical model. Lancet. 2009;373(9657):48–57.
Holtgrave D. Potential and limitations of a “test and treat” strategy as HIV prevention in the United States. Int J Clin Prac. 2010;64(6):678–84.
Selik RM, Mokotoff ED, Branson B, Owen SM, Whitmore S, Hall HI. Revised surveillance case definition for HIV infection & United States, 2014. Morb Mortal Wkly Rep. 2014;63(3):1–10.
Takahashi TA, Johnson KM, Bradley KA. A population-based study of HIV testing practices and perceptions in 4 U.S. states. J Gen Intern Med. 2005;20(7):618–22.
Kaiser Family Foundation. Views and Experiences with HIV testing in the U.S.: survey brief. 2009; https://kaiserfamilyfoundation.files.wordpress.com/2013/01/7926.pdf.
Ford CL, Godette DC, Mulatu MS, Gaines TL. Recent HIV testing prevalence, determinants, and disparities among US older adult respondents to the behavioral risk factor surveillance system. Sex Transm Dis. 2015;42(8):405–10.
Ansa BE, White S, Chung Y, Smith SA. Trends in HIV testing among adults in Georgia: analysis of the 2011–2015 BRFSS data. Int J Environ Res Public Health. 2016;13(11):1126.
Van Handel MM, Rose CE, Hallisey EJ, et al. County-level vulnerability assessment for rapid dissemination of HIV or HCV infections among persons who inject drugs, United States. J Acquir Immune Defic Syndr. 2016;73(3):323–31.
Government Accountability Office. Federal and State efforts to identify infected individuals and connect them to care. GAO-09-985 2009; GAO-09-985. https://www.gao.gov/products/GAO-09-985.
Mahajan AP, Sayles JN, Patel VA, et al. Stigma in the HIV/AIDS epidemic: a review of the literature and recommendations for the way forward. AIDS. 2008;22(Suppl 2):S67–79.
CAA Test. HIV testing in the United States. 2016; https://www.cdc.gov/nchhstp/newsroom/docs/factsheets/hiv-testing-us-508.pdf.
Forrest KYZ, Lin Y. Comparison of health-related factors between rural and urban Pennsylvania residents using behavioral risk factor surveillance system (BRFSS) data. 2010; http://www.rural.palegislature.us/brfss_2010.pdf.
Benavides-Torres RA, Wall KM, Núñez Rocha GM, Onofre Rodríguez DJ, Hopson L. Factors associated with lifetime HIV testing in Texas by race/ethnicity. Open AIDS J. 2012;6:232–8.
Hall HI, Li J, McKenna MT. HIV in predominantly rural areas of the United States. J Rural Health. 2005;21(3):245–53.
Ohl ME, Perencevich E. Frequency of human immunodeficiency virus (HIV) testing in urban vs. rural areas of the United States: results from a nationally-representative sample. BMC Public Health. 2011;11:681.
Henderson ER, Subramaniam DS, Chen J. Rural–urban differences in HIV testing among US adults: findings from the behavioral risk factor surveillance system. Sex Transm Dis. 2018; Publish Ahead of Print.
Wilson LE, Korthuis T, Fleishman JA, et al. HIV-related medical service use by rural/urban residents: a multistate perspective. AIDS Care. 2011;23(8):971–9.
Kakietek J, Sullivan PS, Heffelfinger JD. You’ve got male: internet use, rural residence, and risky sex in men who have sex with men recruited in 12 U.S. cities. AIDS Educ Prev. 2011;23(2):118–27.
Thompson EL, Mahony H, Noble C, et al. Rural and urban differences in sexual behaviors among adolescents in Florida. J Community Health. 2018;43(2):268–72.
Oser CB, Leukefeld CG, Tindall MS, et al. Rural drug users: factors associated with substance abuse treatment utilization. Int J Offender Ther Comp Criminol. 2011;55(4):567–86.
Pullen E, Oser C. Barriers to substance abuse treatment in rural and urban communities: counselor perspectives. Subst Use Misuse. 2014;49(7):891–901.
CDC. Behavioral risk factor surveillance system survey data. In: Services USDoHaH, ed. Atlanta: Centers for Disease Control and Prevention; 2012.
CDC. Behavioral risk factor surveillance system survey data. In: Services USDoHaH, ed. Atlanta: Centers for Disease Control and Prevention; 2014.
CDC. Behavioral risk factor surveillance system survey data. In: Services USDoHaH, ed. Atlanta: Centers for Disease Control and Prevention; 2016.
CDC. Behavioral risk factor surveillance system 2013 codebook report land-line and cell-phone data. 2014.
CDC. Behavioral risk factor surveillance system 2015 codebook report land-line and cell-phone data. 2016; https://www.cdc.gov/brfss/annual_data/2015/pdf/codebook15_llcp.pdf.
CDC. LLCP 2017 codebook report overall version data weighted with _LLCPWT behavioral risk factor surveillance system. 2018; https://www.cdc.gov/brfss/annual_data/2017/pdf/codebook17_llcp-v2-508.pdf.
Judd SE, Gutierrez OM, Newby PK, et al. Dietary patterns are associated with incident stroke and contribute to excess risk of stroke in black Americans. Stroke. 2013;44(12):3305–11.
CDC. Behavioral risk factor surveillance system comparability of data BRFSS 2017. 2018; https://www.cdc.gov/brfss/annual_data/2017/pdf/compare-2017-508.pdf.
CDC. Behavioral risk factor surveillance system survey questionnaire. In: Services USDoHaH, ed. Atlanta: Centers for Disease Control and Prevention; 2012.
CDC. Behavioral risk factor surveillance system survey questionnaire. In: Services DoHaH, ed. Atlanta: Centers for Disease Control and Prevention; 2014.
CDC. Behavioral risk factor surveillance system survey questionnaire. In: Services USDoHaH, ed. Atlanta: Centers for Disease Control and Prevention; 2016.
Dailey AF, Hoots BE, Hall HI, et al. Vital signs: human immunodeficiency virus testing and diagnosis delays—United States. Morb Mortal Wkly Rep. 2017;66:1300–6.
Patel P, Borkowf CB, Brooks JT, Lasry A, Lansky A, Mermin J. Estimating per-act HIV transmission risk: a systematic review. AIDS. 2014;28(10):1509–19.
Koblin BA, Husnik MJ, Colfax G, et al. Risk factors for HIV infection among men who have sex with men. AIDS. 2006;20(5):731–9.
Kwan CK, Rose CE, Brooks JT, Marks G, Sionean C. HIV testing among men at risk for acquiring HIV infection before and after the 2006 CDC recommendations. Public Health Rep. 2016;131(2):311–9.
Purcell DW, Johnson CH, Lansky A, et al. Estimating the population size of men who have sex with men in the United States to obtain HIV and syphilis rates. Open AIDS J. 2012;6:98–107.
Wejnert C, Le B, Rose CE, Oster AM, Smith AJ, Zhu J. HIV infection and awareness among men who have sex with men-20 cities, United States, 2008 and 2011. PLoS ONE. 2013;8(10):e76878.
Bauer HM, Gibson P, Hernandez M, Kent C, Klausner J, Bolan G. Intimate partner violence and high-risk sexual behaviors among female patients with sexually transmitted diseases. Sex Transm Dis. 2002;29(7):411–6.
Cavanaugh CE, Hansen NB, Sullivan TP. HIV sexual risk behavior among low-income women experiencing intimate partner violence: the role of posttraumatic stress disorder. AIDS Behav. 2010;14(2):318–27.
Crosby RA, DiClemente RJ, Wingood GM, et al. Sexual agency versus relational factors: a study of condom use antecedents among high-risk young African American women. Sex Health. 2008;5(1):41–7.
Coker AL. Does physical intimate partner violence affect sexual health? A systematic review. Trauma Violence Abuse. 2007;8(2):149–77.
Dinenno EA, Oster AM, Sionean C, Denning P, Lansky A. Piloting a system for behavioral surveillance among heterosexuals at increased risk of HIV in the United States. Open AIDS J. 2012;6:169–76.
Herbenick D, Reece M, Schick V, Sanders SA, Dodge B, Fortenberry JD. Sexual behavior in the United States: results from a national probability sample of men and women ages 14–94. J Sex Med. 2010;7(Suppl 5):255–65.
Moreno CL. The relationship between culture, gender, structural factors, abuse, trauma, and HIV/AIDS for Latinas. Qual Health Res. 2007;17(3):340–52.
Mosack KE, Randolph ME, Dickson-Gomez J, Abbott M, Smith E, Weeks MR. Sexual risk-taking among high-risk urban women with and without histories of childhood sexual abuse: mediating effects of contextual factors. J Child Sex Abuse. 2010;19(1):43–61.
Simoni JM, Sehgal S, Walters KL. Triangle of risk: urban American Indian women’s sexual trauma, injection drug use, and HIV sexual risk behaviors. AIDS Behav. 2004;8(1):33–45.
Tross S, Hanner J, Hu MC, Pavlicova M, Campbell A, Nunes EV. Substance use and high risk sexual behaviors among women in psychosocial outpatient and methadone maintenance treatment programs. Am J Drug Alcohol Abuse. 2009;35(5):368–74.
Reisen CA, Zea MC, Bianchi FT, Poppen PJ, Shedlin MG, Penha MM. Latino gay and bisexual men’s relationships with non-gay-identified men who have sex with men. J Homosex. 2010;57(8):1004–21.
Albarracin J, Plambeck CR. Demographic factors and sexist beliefs as predictors of condom use among Latinos in the USA. AIDS Care. 2010;22(8):1021–8.
Shedlin MG, Decena CU, Oliver-Velez D. Initial acculturation and HIV risk among new Hispanic immigrants. J Natl Med Assoc. 2005;97(7 Suppl):32S–7S.
Duran D, Usman HR, Beltrami J, Alvarez ME, Valleroy L, Lyles CM. HIV counseling and testing among hispanics at CDC-funded sites in the United States, 2007. Am J Public Health. 2010;100(Suppl 1):S152–8.
del Rio C. Latinos and HIV care in the Southeastern United States: new challenges complicating longstanding problems. Clin Infect Dis. 2011;53(5):488–9.
Beer L, Mattson CL, Bradley H, Shouse RL. Trends in ART prescription and viral suppression among HIV-positive young adults in care in the United States, 2009–2013. J Acquir Immune Defic Syndr. 2017;76(1):e1–6.
Kann L, Olsen EO, McManus T, et al. Sexual identity, sex of sexual contacts, and health-risk behaviors among students in grades 9–12-youth risk behavior surveillance, selected sites, United States, 2001–2009. Morb Mortal Wkly Rep. 2011;60(7):1–133.
Althoff KN, Gebo KA, Gange SJ, et al. CD4 count at presentation for HIV care in the United States and Canada: are those over 50 years more likely to have a delayed presentation? AIDS Res Ther. 2010;7:45
Brooks JT, Buchacz K, Gebo KA, Mermin J. HIV infection and older Americans: the public health perspective. Am J Public Health. 2012;102(8):1516–26.
Oberoi S, Chaudhary N, Patnaik S, Singh A. Understanding health seeking behavior. J Fam Med Prim Care. 2016;5(2):463–4.
McNamee R. Regression modelling and other methods to control confounding. Occup Environ Med. 2005;62(7):500.
Geng Z, Guo J, Fung W-K. Criteria for confounders in epidemiological studies. J R Stat Soc Ser B. 2002;64(1):3–15.
LaMorte WW. Residual confounding, confounding by indication, & reverse causality. 2016; http://sphweb.bumc.bu.edu/otlt/MPH-Modules/BS/BS704-EP713_Confounding-EM/BS704-EP713_Confounding-EM4.html.
Becher H. The concept of residual confounding in regression models and some applications. Stat Med. 1992;11(13):1747–58.
Wang F, Shin H-C. SAS® model selection macros for complex survey data using PROC SURVEYLOGISTIC/SURVEYREG. Midwest SAS Users Group, Kansas City, KS; 2011. http://www.mwsug.org/proceedings/2011/stats/MWSUG-2011-SA02.pdf.
SAS 9.4 [computer program]. Cary, North Carolina 2017.
NIDA. Who is at risk for HIV infection and which populations are most affected? 2012; https://www.drugabuse.gov/publications/research-reports/hivaids/who-risk-hiv-infection-which-populations-are-most-affected.
NICHD. Who is at risk of HIV/AIDS? 2016; https://www.nichd.nih.gov/health/topics/hiv/conditioninfo/risk.
CDC. Populations at greatest risk. 2015; https://www.cdc.gov/hiv/policies/hip/risk.html.
Molina J-M, Capitant C, Spire B, et al. On-demand preexposure prophylaxis in men at high risk for HIV-1 infection. N Engl J Med. 2015;373(23):2237–46.
WHO. Men who have sex with men. 2018; https://www.who.int/hiv/topics/msm/en/.
CDC. Behavioral risk factor surveillance system 2012 codebook report land-line and cell-phone data. 2013; https://www.cdc.gov/brfss/annual_data/2012/pdf/codebook12_llcp.pdf.
Jann B. Predictive margins and marginal effects in Stata. 2013.
Williams R. Using stata’s margins command to estimate and interpret adjusted predictions and marginal effects. Stata J. 2012;12(2):308–31.
Stata Statistical Software. Release 15 [computer program]. College Station: StataCorp LLC; 2017.
U.S. Census Bureau. Census Bureau Regions and Divisions with State FIPS Codes; 2015. https://www2.census.gov/geo/docs/maps-data/maps/reg_div.txt.
CDC. Sexually transmitted disease surveillance 2017. 2018; https://www.cdc.gov/std/stats17/2017-STD-Surveillance-Report_CDC-clearance-9.10.18.pdf.
Nusbaum MR, Wallace RR, Slatt LM, Kondrad EC. Sexually transmitted infections and increased risk of co-infection with human immunodeficiency virus. J Am Osteopath Assoc. 2004;104(12):527–35.
Peterman TA, Newman DR, Maddox L, Schmitt K, Shiver S. Risk for HIV following a diagnosis of syphilis, gonorrhoea or chlamydia: 328,456 women in Florida, 2000–2011. Int J STD AIDS. 2015;26(2):113–9.
Pathela P, Braunstein SL, Blank S, Schillinger JA. HIV incidence among men with and those without sexually transmitted rectal infections: estimates from matching against an HIV case registry. Clin Infect Dis. 2013;57(8):1203–9.
Page P. Beyond statistical significance: clinical interpretation of rehabilitation research literature. Int J Sports Phys Ther. 2014;9(5):726–36.
US Census. Georgia: 2010 population and housing Unit counts. 2012; https://www2.census.gov/library/publications/decennial/2010/cph-2/cph-2-12.pdf.
CDC. HIV in the United States by region. 2018; https://www.cdc.gov/hiv/statistics/overview/geographicdistribution.html.
Bowlin SJ, Morrill BD, Nafziger AN, Jenkins PL, Lewis C, Pearson TA. Validity of cardiovascular disease risk factors assessed by telephone survey: the behavioral risk factor survey. J Clin Epidemiol. 1993;46(6):561–71.
Klompas M, Cocoros NM, Menchaca JT, et al. State and local chronic disease surveillance using electronic health record systems. Am J Public Health. 2017;107(9):1406–12.
Scribani M, Shelton J, Chapel D, Krupa N, Wyckoff L, Jenkins P. Comparison of bias resulting from two methods of self-reporting height and weight: a validation study. RSM Open. 2014;5(6):1–7.
Schneider KL, Clark MA, Rakowski W, Lapane KL. Evaluating the impact of non-response bias in the behavioral risk factor surveillance system (BRFSS). J Epidemiol Community Health. 2012;66(4):290–5.
USDA. Rural–urban continuum codes. 2016; https://www.ers.usda.gov/data-products/rural-urban-continuum-codes/.
Funding
There was no funding for this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical Approval
This article does not contain any studies with human or animals participants performed by any of the authors. All data that was used is publicly available and anonymized.
Informed Consent
This is not applicable to the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Tran, L., Tran, P. & Tran, L. Influence of Rurality on HIV Testing Practices Across the United States, 2012–2017. AIDS Behav 24, 404–417 (2020). https://doi.org/10.1007/s10461-019-02436-5
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10461-019-02436-5