Abstract
Globally, transgender women have higher risk for HIV than the general population and men who have sex with men, but there is little data on this population in Vietnam. In 2015 we conducted a biological and behavioral survey of 205 transgender women in Ho Chi Minh City, Vietnam. Factors associated with HIV and syphilis infection were assessed through multivariable logistic regression models. Median age was 25 years (range 18–64). Overall prevalence was 18.0 % for HIV and 17.6 % for syphilis. Factors independently associated with HIV infection included risky alcohol use [adjusted Odds Ratio (aOR) 3.55, 95 % confidence interval (CI) 1.53–8.21], amphetamine stimulant use (aOR 2.90, 95 % CI 1.27–6.61), sex with male sex workers (aOR 4.73, 95 % CI 1.72–13.0), and history of sex with an adult before the age of 18 years (aOR 2.97, 95 % CI 1.06–8.34). Two factors associated with syphilis infection were HIV infection (aOR 2.37, 95 % CI 1.03–5.45) and condomless anal sex with casual partners (aOR 2.27, 95 % CI 1.03–5.00). In order to address the HIV and syphilis epidemics in Vietnamese transgender women, interventions are needed to make HIV and sexually transmitted infection screening and treatment more accessible.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
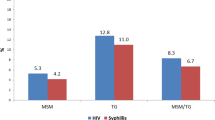
Throughout the world, transgender women have a higher risk for HIV infection than men who sex with men (MSM) and men in the general population [1]. In a meta-analysis of ten low-income and middle-income countries, the pooled HIV prevalence for transgender women was 17.7 %, an odds ratio (OR) of 50 times over the general male populations in the same countries [1].
In Thailand, the HIV prevalence in transgender women was 12.7 % in 2014, whereas prevalence was lower among MSM (9.2 %) and male military recruits (0.5 %) [2]. Transgender women in Indonesia commonly engaged in sex work and had an HIV prevalence of 24.4 %, syphilis prevalence of 26.8 %, and rectal sexually transmitted infection (STI) prevalence of 47.0 % [3]. Hijras, the local term for transgender women in India, are more likely than MSM to sell sex and have HIV prevalence reported at 45.2 % [4].
There is little data on the prevalence of HIV or STI among transgender women in Vietnam. There have been no targeted studies of transgender women in the country; the data that does exist was gathered from the minority of transgender women who were recruited within larger studies of MSM. In 2004, HIV prevalence was 6.8 % among 75 transgender women in Ho Chi Minh City [5]. In the Mekong Delta province of An Giang in 2009, HIV prevalence was 7.9 % among 72 transgender women [6]. By contract, HIV prevalence among MSM in Ho Chi Minh City in 2009 was 14.8 % [7].
We report on the results of the TransVN study, the first survey of HIV prevalence and risk behavior to be completed exclusively among transgender women in Vietnam.
Methods
The TransVN study was a cross-sectional survey of transgender women in Ho Chi Minh City conducted March–April 2015. Inclusion criteria were age ≥18 years, biological male at birth, self-identified as female gender, resident of Ho Chi Minh City, and Vietnamese citizenship. A community advisory board (CAB) consisting of five transgender women was established to provide guidance to the study and to assist with recruitment. The CAB members were chosen to represent diversity in terms of age and economic status. They provided feedback to the investigators on the study protocol and pre-tested the study questionnaire for applicability and ease of understanding.
The CAB members identified transgender women in the community using their social networks and the snowball method to produce a convenience sample. Potentially eligible women were referred to a central location for screening and enrollment. Study staff provided information about the study procedures, provided potential participants with a written information sheet about the study, and obtained verbal informed consent. Participants received 200,000 Vietnam dong (about US$10) to compensate for travel expenses. Pre-test and post-test counseling for HIV was provided and participants were given a subject number that they could use to receive their test results. Treatment for syphilis was provided by the study and those testing positive for HIV were referred to public clinics that provide free antiretroviral treatment.
The study was implemented by the Centre for Applied Research on Men and Community Health (CARMAH), a Vietnamese non-governmental organization that focuses on health issues for MSM and transgender women, and was approved by the Institutional Review Boards at the Hanoi School of Public Health in Vietnam and the University of Pittsburgh in the USA.
Data Collection
Demographic and behavioral data were collected using a standardized questionnaire. Participants completed the questionnaire on their own in the presence of one study staff member who could help answer any questions that participants had about the questionnaire or study procedures. Data was collected on demographics, sexual and condom use behavior, hormone use, history of surgical procedures, substance use, knowledge about HIV infection and prevention, and experiences with sexual abuse as a child and as an adult. Alcohol use was assessed by the 3-item AUDIT-3 scale, with a score of ≥5 defined as risky alcohol use [8]. Substance use was classified as stimulants (ecstasy and crystal methamphetamine), injecting heroin, and smoking opium, and was further categorized as ever used and use within the previous 30 days. Psychological measures utilizing standardized scales included the Primary Care Post-Traumatic Stress Disorder (PTSD) screening tool [9], the Rosenberg self-esteem scale [10], and the shortened Center for Epidemiologic Studies Depression Scale (CESD-10) tool for depression [11].
Sexual behavior was categorized by partner type. For male partners, this included regular partners (boyfriend or husband), clients who paid money for sex, male sex workers, and casual partners. Female partners were classified as regular partners (wife or girlfriend) or non-regular (all others). Condom use for anal or vaginal sex with each partner type was reported on a 4-item Likert scale of never, sometimes, usually, or always. The questionnaire did not differentiate between insertive or receptive sex. Based on post hoc review of the data, consistent condom use was defined as usually or always using condoms; condomless sex (CLS) was defined as reporting either never or sometimes condom use for anal or vaginal sex in the previous 30 days.
Blood was taken for HIV screening using a rapid antibody test (Alere Determine™ HIV 1/2, Alere Inc., Waltham, Massachusetts, USA); positive test results were confirmed by an additional two HIV antibody tests at the Pasteur Institute in Ho Chi Minh City following Vietnam Ministry of Health regulations. Syphilis testing was performed using the Alere Determine™ Syphilis TP rapid test. Positive results were confirmed using a rapid plasma regain test (RPR, Biorad, UK).
Data Analysis
Descriptive characteristics were calculated for the study sample using proportions for categorical variables and medians and interquartile ranges (IQR) for continuous variables. Variables of interest were evaluated for associations with the outcomes of HIV infection and syphilis using χ2 or Fisher’s exact test for categorical variables and Student’s t test for continuous variables. For each outcome variable, a multivariable model using backward stepwise logistic regression was produced that incorporated all variables associated with the outcome with p < 0.20 on bivariate testing. All p values were two-sided and p < 0.05 was considered significant. Data analysis was performed using SPSS version 22 (IBM, Armonk, New York, USA).
Results
Demographics of the study population are presented in Table 1. The median age was 25 years (range 18–64) and the median income was 3–5 million Vietnam Dong (US$141-235) per month. None had ever been married and only 2 (1 %) had children.
The majority of feminizing oral hormones used were birth control pills (94 %) and were purchased at a pharmacy (85 %), obtained from friends (13 %), or prescribed by a physician (2 %). Injectable hormones were obtained through informal networks (68 %), foreign countries (21 %), direct purchase at a pharmacy (10 %), or by a physician prescription (2 %). Injections were most commonly performed by nonmedical persons (59 %), followed by health care workers (33 %), and self-injection (8 %). Silicone injections for cosmetic enhancement were used by 39 %, most commonly to the buttocks, face, and breasts. A minority of transgender women (n = 48, 23 %) had already undergone surgical procedures and 150 (73 %) intended to have procedures in the future (Table 1).
The majority (n = 121, 59 %) had ever been tested for HIV, and 45 % reported testing within the previous year. Of those tested, 89 % reported receiving the test result and only one participant reported a previously positive HIV test. Reasons given for not testing were low perception of risk (60 %), fear of a positive result (14 %), not knowing where to test (13 %), and confidentiality concerns (10 %).
Sexual Behavior
Sexual and substance use behavior is reported in Table 2. First sex with males was at a median of 17 years old (IQR 16-19). There was no difference in mean age at first sex for those HIV positive (16.7 years) or HIV negative (17.3 years) (p = 0.15). Although 71 % reported having sex with an adult before they reached 18 years of age, only 32 (22 %) of these considered it to be sexual abuse. Partner types and condom use are noted in Table 3.
HIV and Syphilis Prevalence
HIV prevalence was 18.0 % (37/205). Factors associated with HIV infection on bivariate and multivariable analyses are presented in Table 4. In the multivariable analysis, risky alcohol use, stimulant use in the previous 30 days, sex with male sex workers, and history of sex with adults before the age of 18 were independently associated with HIV infection.
Syphilis prevalence was 17.6 % (36/205). Co-infection with both syphilis and HIV was found in 11 participants (5.4 %). On multivariable analysis, HIV infection and CLS with casual partners were the only two factors significantly associated with syphilis infection (Table 5).
Discussion
The HIV prevalence in this sample of transgender women in Vietnam was 18 %. This is higher than the estimate of 14.8 % for HIV prevalence among MSM in HCMC [7] but very close to the 17.7 % reported pooled prevalence for transgender women worldwide [1]. Other countries in South and Southeast Asia have reported HIV prevalence rates among transgender women of 12.7–45.2 % [2–4].
Previous studies have reported a lower HIV prevalence of 6.8–7.9 % among transgender women in southern Vietnam [5, 6]. However, those studies were completed 6–11 years earlier, had smaller sample sizes of transgender women, used different recruiting methods, and were primarily studies targeting MSM that included a minority of transgender women participants. The higher HIV prevalence found in the current study may be explained by rising HIV prevalence over time and by the targeted sampling methodology. The Vietnam Ministry of Health reports a “worrisome” increase in HIV prevalence for MSM from 2005 to 2013 [12]. Our study indicates that HIV prevalence is also rising rapidly among transgender women and may in fact be higher than among MSM.
HIV infection was significantly associated with risky alcohol use, recent stimulant use, sex with male sex workers, and history of sex with adults before the age of 18 years. Although 35 % of the transgender women in the survey reported having sex for money in the previous month, selling sex was not associated with HIV or syphilis infection. Nor was any measure of recent condom use associated with HIV infection. HIV infection is life-long once acquired. Therefore, HIV prevalence in a cross-sectional survey reflects risk behavior over the previous years or even decades. It is probable that most of the HIV infections diagnosed in the study were acquired months or years in the past and that the survey questions about condom use in the previous month did not accurately assess cumulative past risk behavior.
History of sex with an adult before the age of 18 years was associated with HIV infection. Previous studies have shown that childhood sexual abuse was associated with condomless anal sex, alcohol dependence, and sexual violence among male sex workers in HCMC [13] and with HIV infection and drug use among MSM in the USA [14]. Although it is possible that HIV transmission occurred as a result of childhood sexual experiences with adults, in this sample it is unlikely for the majority of participants. The mean age of those with HIV infection was 25 years; it is unlikely that HIV infections would remain asymptomatic and undiagnosed for 7 years or more in most individuals. The mechanism by which early sex with adults affects later HIV risk remains to be elucidated and should be investigated in future studies.
It is notable that 71 % of participants reported sex with an adult before they were 18 years old, but that only 22 % of them perceived this to be sexual abuse. Similar findings have been reported in Brazil, where childhood sexual experiences with adult partners were more commonly experienced by transgender women than by MSM, but were less likely to be perceived as sexual abuse [15]. It may be that early sexual experiences mediate HIV infection risk through the sequelae of mental health issues and substance abuse, which were both highly prevalent in the study population.
Almost half (45 %) of participants screened positive for depression and 69 % had symptoms of PTSD. Substance use was also very common: 51 % had risky alcohol use and 21 % used stimulants in the previous month. Both of these were significantly associated with HIV infection, indicating the need for substance use interventions for HIV prevention as well as for addressing addiction and other harms of drug and alcohol use.
It is notable that all but one HIV infection was previously undiagnosed, despite the fact that 59 % of participants reported previous HIV testing and 45 % were tested in the previous year. It may be that participants over-reported previous HIV testing, or declined to reveal previously known HIV infections, as both of these factors relied on self-report. However, it is also possible that this is a true finding as HIV prevalence among MSM and transgender women appears to be rising rapidly in Vietnam [5, 6, 12]. In any case, the high prevalence of undiagnosed HIV found in this survey indicates that increased access to HIV testing and treatment services is needed for Vietnamese transgender women.
Syphilis infection was also high at 17.6 %. In the multivariable analyses HIV infection was a significant factor associated with syphilis. A number of studies have documented an increased risk for syphilis among people with HIV infection, especially among MSM [16, 17], but it is unclear if this is due to biologic susceptibility, increased sexually activity, higher rates of condomless sex, or a combination of factors [18].
The study has some important limitations. Participants self-reported risk behaviors and the results of previous HIV testing, which might have been under-reported due to social desirability bias. The use of a convenience sample might not be representative, and therefore the results of the study might not be generalizable to the entire transgender population in Ho Chi Minh City or in Vietnam.
The survey questionnaire not differentiate between insertive and receptive anal sex. Although condomless receptive anal intercourse has the highest risk for sexual transmission of HIV and is the presumed route of HIV transmission for most transgender women, there remains a dearth of evidence on the contribution of neovaginal sex or insertive anal intercourse to HIV acquisition in Vietnam and elsewhere [1].
In summary, we found very high prevalences of HIV and syphilis infection in transgender women in Ho Chi Minh City, Vietnam. No interventions or larger programmatic initiatives that specifically target transgender women exist in Vietnam. Existing programs that target MSM may not be reaching this stigmatized and marginalized population with the information and services that they need.
Although no randomized trial data exist on interventions specifically for transgender women [1], there are published guidelines and best practices that can guide the development of HIV prevention programming for this population [19, 20]. HIV counseling and testing, and the promotion of condom and lubricant use for anal sex, remain the cornerstone of HIV prevention for all risk groups. Pre-exposure prophylaxis (PrEP) is highly effective for transgender women when taken regularly [21]. A gender-affirming clinic that integrated basic sexual health services with hormone therapy could attract transgender women for HIV prevention interventions and would serve as an environment for best practices to arise.
References
Baral S, Poteat T, Stromdahl S, Wirtz AL, Guadamuz T, Beyrer C. Worldwide burden of HIV in transgender women: a systematic review and meta-analysis. Lancet Infect Dis. 2013;13:214–22.
National AIDS Committee. Thailand ending AIDS: Thailand AIDS response progress report 2015. Bangkok: ministry of public health. 2015. www.unaids.org/sites/default/files/country/documents/THA_narrative_report_2015.pdf.
Prabawanti C, Bollen L, Palupy R, et al. HIV, sexually transmitted infections, and sexual risk behavior among transgenders in Indonesia. AIDS Behav. 2011;15:663–73.
Sahastrabuddhe S, Gupta A, Stuart E, Godbole S, Ghate M, Sahay S, et al. Sexually transmitted infections and risk behaviors among transgender persons (Hijras) of Pune, India. J Acquir Immune Defic Syndr. 2012;59(1):72–8.
Nguyen TA, Nguyen HT, Le GT, Detels R. Prevalence and risk factors associated with HIV infection among men having sex with men in Ho Chi Minh City Vietnam. AIDS Behav. 2008;12(3):476–82.
Pham QD, Nguyen TV, Hoang CQ, Cao V, Khuu NV, Phan HT, et al. Prevalence of HIV/STIs and associated factors among men who have sex with men in An Giang Vietnam. Sex Transm Dis. 2012;39(10):799–806.
Ministry of Health. Results from the HIV/STI Integrated Biological and Behavioral Surveillance (IBBS) in Vietnam–Round II, 2009. Hanoi: Vietnam Ministry of Health; 2011.
Gual A, Segura L, Contel M, Heather N, Colom J. AUDIT-3 and AUDIT-4: effectiveness of two short forms of the alcohol use disorders identification test. Alcohol Alcohol. 2002;37:591–6.
Prins A, Ouimette P, Kimerling R, Cameron RP, Hugelshofer DS, Shaw-Hegwer J, et al. The Primary care PTSD screen (PC-PTSD): development and operating characteristics. Prim Care Psychiatry. 2003;9:9–14.
Rosenberg M. Society and the adolescent self-image. Middletown: Wesleyan University Press; 1989.
Zhang W, O’Brien N, Forrest JI, Salters KA, Patterson TL, Montaner JSG, et al. Validating a shortened depression scale (10 Item CES-D) among HIV-positive people in British Columbia, Canada. PloS One. 2012;7(7):e40793.
National committee for AIDS drugs, and prostitution prevention. Viet Nam AIDS response progress report 2014. Hanoi: Government of Vietnam, 2014.
Biello KB, Colby D, Closson E, Mimiaga MJ. The syndemic condition of psychosocial problems and HIV risk among male sex workers in Ho Chi Minh City Vietnam. AIDS Behav. 2014;18(7):1264–71.
Brennan DJ, Hellerstedt WL, Ross MW, Welles SL. History of childhood sexual abuse and HIV risk behaviors in homosexual and bisexual men. Am J Public Health. 2007;97(6):1107–12.
Carballo-Dieguez A, Balan I, Dolezal C, Mello MB. Recalled sexual experiences in childhood with older partners: a study of Brazilian men who have sex with men and male-to-female transgender persons. Arch Sex Behav. 2012;41(2):363–76.
Solomon MM, Mayer KH. Evolution of the syphilis epidemic among men who have sex with men. Sex Health. 2014;17(12):96–102.
Hu QH, Xu JJ, Zou HC, Liu J, Zhang J, Ding HB, et al. Risk factors associated with prevalent and incident syphilis among an HIV-infected cohort in Northeast China. BMC Infect Dis. 2014;14(1):658.
Stoltey JE, Cohen SE. Syphilis transmission: a review of the current evidence. Sex Health. 2015;23(12):103–9.
United Nations Development Programme. Implementing comprehensive HIV and STI programmes with transgender people: practical guidance for collaborative interventions. New York: United Nations Development Programme; 2016.
Health Policy Project. Asia pacific transgender network, United Nations development programme. Blueprint for the provision of comprehensive care for Trans people and trans communities. Washington, DC: Futures Group, Health Policy Project; 2015.
Deutsch MB, Glidden DV, Sevelius J, Keatley J, McMahan V, Guanira J, et al. HIV pre-exposure prophylaxis in transgender women: a subgroup analysis of the iPrEx trial. Lancet HIV. 2015;2(12):e512–9.
Funding
This project was funded through a Grant from amFAR and contributions from the University of Pittsburg and the Center for Applied Research on Men and Health, Ho Chi Minh City, Vietnam. Test kits for HIV and syphilis were donated by Alere Inc.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and national research committees and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Colby, D., Nguyen, N.A., Le, B. et al. HIV and Syphilis Prevalence Among Transgender Women in Ho Chi Minh City, Vietnam. AIDS Behav 20 (Suppl 3), 379–385 (2016). https://doi.org/10.1007/s10461-016-1485-8
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10461-016-1485-8