Abstract
Behavioral surveillance was undertaken among 1,150 male-to-female transgenders (waria) in Java, Indonesia, 2007; samples were collected for HIV and STI testing (n = 748). Almost all waria had ever sold sex (median duration 10 years). Prevalence of HIV was 24.4%, syphilis 26.8% and rectal gonorrhea and/or chlamydia 47.0%. Syphilis and rectal STIs were associated with HIV infection. Consistent condom use during receptive anal sex with clients was reported by 35.9% waria and was higher among those who visited an STI clinic and who knew their HIV status. Efforts should continue to strengthen behavior change and STI care in future HIV prevention programs.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Male-to-female transgender persons are considered to be at high risk for HIV infection [1], mainly because they often engage in unprotected receptive anal sex. Discrimination and stigmatization are common, often resulting in the economic necessity of trading sex for money [1, 2]. Many transgender persons also experience low self esteem and sexual violence, which may lead to psychosocial vulnerability and reduced negotiation of condom use [2].
Male-to-female transgenders in Indonesia (waria) might face discrimination similar to male-to-female transgenders in other countries in South-East Asia, such as hijra’s in India/Nepal and kathoeys in Thailand. Although not prohibited by law, most communities in Indonesia discriminate against waria making it harder for them to finish school, find a job, housing, and access to public health services, which altogether increased their risk for STIs and HIV.
Indonesia has a concentrated HIV epidemic among populations with high-risk behavior, including injecting drug users, female sex workers and their clients, men who have sex with men, and waria in Indonesia. The HIV prevalence among waria in Jakarta increased from 7.9% in 1995 to 22.0% in 2002 [3]. In addition, syphilis prevalence among waria in Jakarta was similarly high in 2002 at 19.3% [3]. Unprotected anal sex among waria was common [3], thereby increasing the risk of HIV and sexually transmitted infection (STI) transmission. These findings prompted the Indonesian Ministry of Health and its implementing partners to strengthen HIV prevention services for the estimated 21,000 waria in Indonesia [4], most of whom live in major cities in Java. These services started in 2002 and included outreach and behavior change interventions to encourage waria to adopt safe sexual behaviors, and to visit clinics for STI screening and treatment and voluntary HIV counseling and testing (VCT).
The 2007 Integrated Biological-Behavioral Surveillance (IBBS) survey gathered data among most-at-risk groups in Indonesia. We report the results from the 2007 IBBS among waria in Indonesia, including the prevalence of HIV, STIs and unprotected commercial sex and factors associated with these outcomes. These data will provide the Ministry of Health with updated information on the epidemic situation among waria with which to assess current program efforts and make changes as appropriate.
Methods
Sampling
Behavioral survey data were collected between August and November 2007 from independent samples of 1,150 waria in five Indonesian cities; Jakarta, Bandung (West Java), Semarang (Central Java), and Surabaya and Malang (East Java). Waria interviewed in Jakarta, Bandung, and Surabaya were asked to provide biological samples and were tested for HIV (n = 748), rectal and urethral gonorrhea and chlamydia (n = 734), syphilis (n = 720), and syphilis titer (n = 462).
Waria are biological males and meet the definition of waria if they cross-dress, adopt the behavior and societal roles of females, identify themselves as waria, and socialize regularly with fellow warias in definable communities.Footnote 1 Local health authorities and local non-governmental organizations providing services to waria obtained city and group-specific sampling frames after mapping commercial sex hotspots. Participants were selected through two-stage, time-location sampling. Primary sampling units (PSU) consisted of ringleaders or mami’sFootnote 2 and streets where waria gathered. PSUs were selected via simple random sampling with probability proportional to estimated waria population size. Mapping identified PSUs and estimated the number of waria at each site. PSUs were selected through simple random sampling until completion of the desired sample size. At the second stage, all waria assembled by their mami or present at sampled street locations at the time of data collection agreed to participate and were included in the survey. Missing PSU identification numbers and missing measures of size for some PSUs precluded the possibility of computing sampling weights.
Survey field teams were drawn from staff of provincial offices of the Central Statistics Bureau and Provincial Health Offices. Following receipt of witnessed verbal consent, interviewers gathered behavioral information using a structured pre-coded questionnaire. In selected cities, following the completion of the behavioral survey, a nurse collected blood through venipuncture and participants provided self-collected rectal swabs and first-void urine. The behavioral survey and biological data were anonymous, linked via a unique identifier for each participant. Per Indonesian Ministry of Health surveillance guidelines, all participants received a coupon for free HIV counseling and testing at a nearby Community Health Center.
Laboratory Analysis
Whole blood was centrifuged and aliquoted. Serum specimens were stored at 4–6°C and tested within 3 days of collection at the nearest local laboratory. HIV testing was done with two parallel rapid tests: SD Bioline HIV 1/2 3.0® (Standard Diagnostic Inc, Suwon City, South Korea) and Determine® HIV-1 (Inverness Medical, Matsudo, Japan). Discrepant results were re-tested at the National Research Laboratory using two ELISA assays: Murex® (Murex Biotech, Dartford, United Kingdom) and Vironostika® (Biomérieux, Marcy l’Etoile, France).
Presence of antibodies against Treponema pallidum was tested using the Rapid Plasma Reagin (RPR) test (Shield Diagnostics, Bridpot, Dorset, UK) as a screening test and the Treponema pallidum Rapid Test (Determine TP Syphilis, Inverness Medical, Bedford, United Kingdom) as a confirmatory test. Specimens with both positive RPR and TPHA results were titered until 1/128 dilution. Those with RPR titer ≥1:8 and TPHA-positive were classified as active syphilis.
Rectal swabs and urine specimens were tested for the presence of Chlamydia trachomatis and Neisseria gonorrhoeae by polymerase chain reaction analysis (Cobas Roche Amplicor Diagnostic System, Basel, Switzerland). Persons were invited to visit an STI clinic to receive their STI test results by showing their unique identity number; treatment was provided free of charge according to the national STI treatment guidelines.
Statistical Analysis
Behavioral data were double-entered using Census and Survey Processing System (CSPro) 2.6.007 (U.S. Census Bureau). Laboratory data were entered using Microsoft Excel. Analysis was performed using Stata 9.0 (Stata Corporation, College Station, TX, USA). Variables of interest were described in terms of frequency, median, and range. Prevalence of HIV, active syphilis (RPR ≥1:8), urethral and rectal gonorrhea and chlamydia were assessed with 95% exact binomial confidence intervals (CIs). Associations between categorical variables were assessed using the Wald test and P-values less than 0.05 were considered as significant.
Factors potentially associated with HIV infection, rectal gonorrhea or chlamydia infection and consistent condom use during receptive anal sex with clients in the last week were analysed in bivariable and multivariable models. Logistic regression was used to calculate odds ratios (OR) with 95% CIs; continuous variables were dichotomized. Multivariable modeling included factors with P < 0.2 level of significance in the bivariable analysis. Following backward elimination; significant risk factors with P < 0.05 were retained in the model. The purpose of this modeling exercise was to explore associations present in the study population with the intention of generating hypotheses, and with no intention of making causal inferences that are generalizable beyond this study population.
Analyses were performed on the multi-site pooled data assuming stratified cluster sampling, with the recruiting mami in Jakarta and street locations in other cities being considered as clusters.
The study protocol was approved by both the Ethics Committee of the Indonesian Center for Biomedical and Pharmaceutical Research and the Family Health International Protection of Human Subjects Committee.
Results
General Characteristics
The median age among waria was 30 years (range 15–83). More than half of waria (58.3%) had only primary education or less, and most reported to have been discriminated against in the last year (64.7%), including physical harassment and/or being insulted at work or in daily life because of being waria (Table 1). Approximately half (46.9%) reported having a steady sexual partner, most of them being male partners. A quarter of waria reported having been forced into sex in the last year.
Behavioral Characteristics
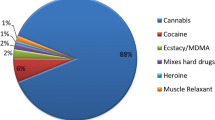
Injecting drug use among waria was rare (0.3%), but 10% reported to have used recreational drugs in the last 3 months. Condom breakage and the use of more than one condom (one on top of the other) were reported by 14.7 and 11.5% waria, respectively. Almost all (97.0%) reported having ever sold sex. The median age waria started selling sex was 19 years, with a median duration of 10 years. The median number of clients for anal sex in the last week was 2.0 with a median fee for last sex of 20,000 Indonesian Rupiah (roughly equivalent to 2 USD). The proportion of waria who reported consistent condom use during receptive anal sex with clients in the last month was 35.9%, although condom use with the last client was reported by 79.5% of waria (85.1% of waria in Jakarta). Twenty percent reported buying anal sex in the last month, and half reported non-paying sex (with casual or steady partners) in the last year.
Three quarters had visited an STI clinic for a routine check-up in the last 3 months. Around a quarter of waria reported STI symptoms in the last year, most of them visited the STI clinic for treatment. More than half of waria had an HIV test in the last year (58% of waria in Jakarta).
HIV-Related Knowledge
Overall levels of HIV-related knowledge among waria were moderate (data not shown). Nearly one-half (45.9%) of waria provided correct answers to Abstinence, Being faithful and Condom use (ABC) knowledge; 65.5% said reducing number of partners reduces HIV risk, 72.7% said that being faithful reduced HIV infection risk, and 83.0% knew HIV could be prevented by condom use. However, misconceptions about HIV acquisition persist; such as getting HIV from mosquito bites (22.2%) or by sharing food utensils with an HIV-infected person (21.2%).
HIV and STI Prevalence
The overall HIV prevalence among waria was 24.4%, and was highest in Jakarta (34.0%) (Table 2). Overall syphilis prevalence was 26.8% and was similar among waria in all three cities; active syphilis (RPR ≥1:8) was assessed among waria in Jakarta (15.0%) and Surabaya (14.9%). The prevalence of rectal gonorrhea was 29.0%, chlamydia 30.4% and gonorrhea and/or chlamydia 47.0%. The highest rectal gonorrhea and/or chlamydia prevalence was found among waria in Bandung (54.6%). The prevalence of urethral gonorrhea and/or chlamydia was much lower at 1.1%, and was similar across cities. Overall, more than half (59.1%) of waria had one or more STI.
Factors Associated with HIV, STIs and Condom Use
Several factors were associated with HIV infection in bivariable analysis. Multivariable analysis showed that not having a steady sex partner, longer duration of sex work (>4 years), syphilis and rectal STIs were independently associated with HIV infection (Table 3).
The proportion of waria with reactive syphilis serology was similar among those who had visited an STI clinic for a check-up at least once in last 3 months compared to those who had not (28.8% vs. 21.7%; P = 0.3). Older age, lower education, more clients and HIV positive test result were independently associated with syphilis (Table 4).
The proportion of waria with rectal gonorrhea/chlamydia was also similar among those who did and who did not visit an STI clinic (47.8% vs. 43.6%; P = 0.3). Most (82.3%) underwent an anal exam during the STI clinic visit; the gonorrhea/chlamydia prevalence was similar among those who did and who did not undergo an anal exam (49.0% vs. 44.0%; P = 0.3). Multivariable analysis of factors associated with rectal gonorrhea/chlamydia showed experience of discrimination in the last year and HIV positive test results to be independently associated with rectal gonorrhea/chlamydia (Table 5).
Waria who received VCT and their test result last year were more likely to use condoms consistently during receptive anal sex with clients in the last month compared to waria who did not know their status. Other factors independently associated with consistent condom use were better HIV knowledge, higher than median fee for selling anal sex and currently carrying a condom; having STI symptoms was associated with less condom use (Table 6).
Discussion
The 2007 IBBS survey among waria revealed high HIV and STI prevalence, along with low consistent condom use. Apparently, HIV and STIs continue to spread among waria and their male clients. The finding that HIV prevalence in Jakarta increased from 22% in 2002 [3] to 34% in the current 2007 survey is alarming. However, the proportion of waria in Jakarta who received an HIV test in the last year increased from less than 3% in 2002 [3] to 58%, likely the result of prevention efforts. Although current HIV prevention services seem insufficient to curb the HIV epidemic, efforts to increase access to VCT have been successful and more waria have become aware of their HIV status. Linkages to HIV care and treatment have been established, but information about HIV test results and receipt of antiretroviral treatment (ART) was not included in this study. Clearly, access to ART will need to be assessed in future surveys and interventions implemented as needed to ensure adequate utilization of care and support services (Table 6).
The overall HIV prevalence among waria was 24.4%, which was higher than the prevalence found among female sex workers (FSW) (7.9%) [5] and men who have sex with men (MSM) (5.2%) [6], in surveys conducted in the same year. This observation is in accordance with a meta-analysis from studies in fourteen countries showing higher HIV prevalence among transgenders compared to FSWs and MSM [7]. Sex work, low education levels, discrimination and coercion into sex were common among waria in our survey contributing to higher vulnerability for STIs and HIV [1]. Among waria in our study, we found that having experienced discrimination in the last year was associated with a higher prevalence of rectal STIs. The explanation for this is not clear as discrimination was not associated with lower condom use; probably because different time frames were used. Perhaps those experiencing discrimination had a lower self esteem placing them somehow at risk for acquiring rectal STIs; for example, they may not be particular in partner selection. Discrimination, stigmatization and marginalization among waria need to be addressed and may include facilitating access to the formal employment sector.
The syphilis seroprevalence was 26.8% for waria in Indonesia. We found an increase in syphilis prevalence among waria in Jakarta from 19.3% in 2002 to 25.2% in 2007 [3]. Syphilis control needs to be emphasized as syphilis fuels the HIV epidemic by increasing susceptibility for HIV and by increasing HIV infectiousness among those already infected with HIV [8]. In addition, untreated syphilis results in short-term (e.g., genital lesions, lymphadenopathy, and alopecia) and long-term (cardiovascular complications such as aortic aneurysm and neurological complications such as meningitis) morbidity [9]. Although three quarters of waria reported to have visited an STI clinic in the last 3 months for routine check-ups, those visiting STI clinics did not have lower syphilis rates. This could result from inadequate syphilis screening and treatment at the clinics or from high re-infection rates.
This study highlights for the first time high prevalence of rectal gonorrhea and chlamydial infection among waria across the three cities. The 2007 IBBS showed similar high rectal STIs among MSM as shown in a separate report [6]. Waria in Surabaya had significantly lower rectal gonorrhea prevalence compared to waria in the other cities, most likely resulting from receipt of PPT one-two month prior to the survey (as part of a Family Health International and World Health Organization project for FSWs in four cities and waria in Surabaya). Surprisingly, the rectal STI prevalence was not lower among waria who had visited STI clinics. This may result from re-infection or from inadequate treatment of these STIs. Many clinics still provide ciprofloxacin for gonorrhea treatment (personal communication, Robert Magnani, country director FHI Indonesia) although resistance has been reported since 2006 [10] and cefixime replaced ciprofloxacin as the treatment of choice in the 2006 STI treatment guidelines. Emphasis is now being placed on providing correct treatment for rectal STIs at the STI clinics. This would also reduce HIV acquisition as a recent cohort study showed men with anal gonorrhea to be seven times more likely to acquire HIV compared to those without anal gonorrhea [11].
Syphilis and rectal STIs were associated with HIV infection in our study. As previous studies have indicated that these infections may result in increased risk of HIV transmission [8], it seems appropriate to focus on controlling STIs among waria in order to decrease HIV transmission. We have shown previously that periodic presumptive treatment for gonorrhea and chlamydia among female sex workers in Indonesia resulted in a rapid decline in prevalence of gonorrhea and Chlamydia [12]. A similar project has been developed by the Indonesian Ministry of Health for waria and the first round of presumptive treatment for gonorrhea and chlamydia has been provided for 250 waria in Surabaya in December 2009.
Consistent condom use in the past month with different partners and during different roles was low across cities, despite HIV prevention program implementation since 2002. The finding that a low proportion of waria reported consistent condom use is in accordance with the high HIV and STI prevalence found among waria in this survey. However, the proportion of waria in Jakarta who used condoms with their last client doubled since 2002 (85% vs. 43% in 2002) [3], although social desirability bias might have prompted waria to report condom use. Waria with good knowledge about prevention of HIV transmission were more likely to use condoms consistently with clients. Having a condom at the time of the interview was associated with more condom use, which could reflect willingness to use a condom or availability of condoms.
Waria who had received HIV test results in the last year were more likely to use condoms with their clients. This association has also been observed by others [13] in a cross-sectional assessment. Persons may adopt safer behavior after knowing their HIV status or safer behavior may be a result from counseling on condom use during VCT. Perhaps, persons who are more likely to use condoms may also be the ones who decide to receive VCT and the observed association between condom use and VCT might not be causally related. The relationship between receipt of VCT and subsequent reported behavior was assessed in a recent population-based cohort study in Zimbabwe [14], which showed a reduction in the number of new partners for women but no increase in condom use. No behavioral risk reduction was observed after VCT among men. A prospective cohort study among waria could clarify the temporal relationship between condom use and VCT in our setting. In addition, we did not collect information about HIV test results and a future study could also assess associations between self-reported HIV status and condom use.
A possible limitation of the time-location sampling design is that waria in highest demand for sex work, representing those with most clients and at highest risk for HIV transmission, may not have been present during the time of sampling for this survey. Alternatively, waria not selling sex are likely not present at commercial hotspots and might be under represented in this survey. Another limitation is a possible selection bias as mami’s invited waria to participate in this survey. Therefore, estimates need to be interpreted with some caution, particularly when comparing them with estimates from an earlier survey in Jakarta. Another limitation of this assessment is that we cannot show a temporal association between behaviors and the outcomes, due to the cross-sectional design as mentioned above. Although associations may differ per city we did not undertake risk analysis for cities separately due to limited sample size.
Our analyses indicate the need for further expansion of HIV program coverage, integrating behavior change communication, STI care, VCT and HIV care in a comprehensive approach to leverage the contributions in each area to maximize the final impact on HIV transmission. In addition, efforts should continue to educate waria on HIV prevention and create an enabling environment for behavioral change by addressing discrimination through community mobilization and other “structural” interventions. Interventions should address motives for unprotected sex and psychological, social and cultural factors that determine sexual risk behavior among waria.
Notes
Most waria have breast implants, use hormones such as oral contraception and some might have undergone surgery.
Waria often live in small groups, coordinated by a ring leader or ‘mami’. A mami usually is a senior waria who provides support for the 5–15 waria in her group, including violence protection and promotion of condom use, VCT and regular routine STI check-ups.
References
De Santis JP. HIV infection risk factors among male-to-female transgender persons: a review of the literature. J Ass Nurses AIDS Care. 2009;20(5):362–72.
Clements-Nolle K, Guzam R, Harris SG. Sex trade in a male-to-female transgender population: psychosocial correlates of inconsistent condom use. Sexual Health. 2008;5:49–54.
Pisani E, Girault P, Gultom M, et al. HIV, syphilis infection, and sexual practices among transgenders, male sex workers, and other men who have sex with men in Jakarta, Indonesia. Sex Transm Infect. 2004;80(6):536–40.
National AIDS Commission. Kegiatan estimasi populasi dewasa rawan terinfeksi HIV, tahun 2006 (in Bahasa Indonesia). Jakarta: National AIDS Commission; 2006.
Magnani R, Riono P, Nurhayati, et al. Sexual risk behaviors, HIV and other sexually transmitted infections among female sex workers in Indonesia. Sex Transm Inf. E-publication.
Morineau G, Nugrahini N, Riono P, et al. Sexual risk taking, STI and HIV prevalence among men who have sex with men in six Indonesian cities. AIDS Behav. doi:10.1007/s10461-009-9590-6.
Operario D, Soma T, Underhill K. Sex work and HIV status among transgender women: systematic review and meta-analysis. J Acquir Immune Defic Syndr. 2008;48(1):97–103.
Dallabetta G, Neilsen G. Efforts to control sexually transmitted infectionis as a means to limit HIV transmission: what is the evidence? Curr Infect Dis Rep. 2005;7:79–84.
Singh AE, Romanowski B. Syphilis: review with emphasis on clinical, epidemiologic, and some biologic features. Clin Microb Review. 1999;12(2):187–209.
Sutrisna A, Soebjakto O, Wignall FS, et al. Increasing resistance to ciprofloxacin and other antibiotics in Neisseria gonorrhoeae from East Java and Papua, Indonesia, in 2004 - implications for treatment. Int J STD AIDS. 2006;17(12):810–2.
Jin F, Prestage GP, Imrie J, et al. Anal sexually transmitted infections and risk of HIV infection in homosexual men. J Acquir Immune Defic Syndr. 2010;53(1):144–9.
Bollen LJM, Anartati AS, Morineau G, et al. Addressing the high prevalence of gonorrhea and chlamydia among female sex workers in Indonesia: results of an enhanced, comprehensive intervention. Sex Transm Infect. 2010;86:61–5.
Kayembe PK, Mapatano MA, Busangu AF, et al. Determinants of consistent condom use among female commercial sex workers in the Democratic Republic of Congo: implications for interventions. Sex Transm Infect. 2008;84(3):202–6.
Cremin I, Nyamukapa C, Sherr L, Hallett TB. Patterns of self-reported behaviour change associated with receiving voluntary counselling and testing in a longitudinal study from Manicaland, Zimbabwe. AIDS Behav. 2010;14(3):708–15.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Prabawanti, C., Bollen, L., Palupy, R. et al. HIV, Sexually Transmitted Infections, and Sexual Risk Behavior Among Transgenders in Indonesia. AIDS Behav 15, 663–673 (2011). https://doi.org/10.1007/s10461-010-9790-0
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10461-010-9790-0