Abstract
HIV status disclosure can help patients obtain support which may influence treatment adherence and subsequent healthcare needs. We examined the extent of disclosure and correlates of non-disclosure among 1180 adults newly initiating antiretroviral treatment (ART). While 91 % of those in a relationship shared their status with their partners, 14 % of the overall sample had not disclosed to anyone. Non-disclosure was positively associated with older age; control over household resources; and concerns about unintended disclosure, life disruptions, and family reactions. Knowing other HIV-positive people and longer time since diagnosis were associated with lower odds of non-disclosure. Most respondents reporting disclosure experienced supportive responses, frequently including decision to get an HIV test by confidants who had not known their own status. Although HIV status disclosure prior to ART initiation was high, some individuals cited concerns about unintended disclosure, gossip, and partner violence, and may benefit from additional disclosure support.
Resumen
La revelación del estado serológico del VIH puede ayudar a los pacientes a obtener apoyo que podría influir en la adherencia al tratamiento y en las necesidades de cuidado para su salud. Examinamos la frecuencia y factores asociados con la no revelación del estado serológico del VIH en 1180 adultos iniciando tratamiento antirretroviral (TARV) por primera vez. Mientras 91 % de los que estaban en una relación compartió su estado serológico con su pareja, 14 % de la muestra total no reveló su estado a nadie. La no revelación del estado serológico estuvo asociada positivamente con mayor edad, control sobre los recursos familiares, y preocupaciones sobre revelaciones no intencionales, interrupciones en la vida cotidiana y las reacciones familiares. Conocer otras personas VIH-positivas y mayor tiempo desde el diagnóstico estuvieron asociados con menor posibilidades de no revelación. La mayoría de los encuestados que revelaron su estado recibieron respuestas de apoyo, incluyendo una aceptación considerable del test de VIH en confidentes que no conocían su estado serológico. Aunque la revelación del VIH antes de iniciar TARV fue alta, ciertos individuos mencionaron preocupaciones sobre revelaciones no intencionales, chismes y violencia por parte de su pareja, y podrían beneficiarse de apoyo adicional para revelar su estado serológico.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Disclosure of one’s HIV positive status facilitates access to care and treatment for patients and their sexual partners, benefits the community by promoting openness about HIV, and is therefore key to curbing the HIV epidemic [1]. However, disclosure is a complex process that involves knowledge, motivations, and choices influenced by socio-cultural norms and assessment of associated risks and benefits. The decision whether to disclose, to whom, and when, depends on patient’s readiness to take a perceived risk [2, 3]. As a result, the level of disclosure of HIV positive status varies geographically and among different patient populations. Indeed, a review of 17 studies on disclosure among women in Africa and Asia found disclosure rates ascertained at varying time points following diagnosis ranging from 17 to 86 % [4].
Research in Ethiopia has documented that disclosure of HIV positive status is common in the general population of patients receiving HIV services (76–95 %) [5–8], with slightly lower levels of disclosure to sex partners (57–93 %) [5–12]. Knowledge of partner’s HIV status, prior communication about HIV testing, pre-test counseling, advanced disease stage, being married, and longer time since diagnosis were found to be important facilitators of disclosure [6–10, 12].
Disclosure prior to initiating antiretroviral therapy (ART) is of particular importance, as it may influence timing of treatment initiation, subsequent adherence to treatment and patient outcomes in several ways [13, 14]. It may improve the patient’s psychological well-being and the support they can count on for keeping drugs at home and taking them daily, following dietary and lifestyle modifications required for specific medications, as well as discussion and management of side effects [15–17]. However, to date, no data on the extent of disclosure specifically as of the time of ART initiation are available in Ethiopia or other regions.
With an estimated 760,000 people living with HIV (PLWH) and adult prevalence of 1.3 % [18, 19], Ethiopia began scaling up comprehensive HIV services, including ART, in 2005, and adopted a family-centered approach to HIV prevention, treatment, care and support in order to curb the primarily heterosexually transmitted disease affecting families. Disclosure of HIV positive status to partners and other family members is a central pillar of this approach [20].
The aim of this study was thus to assess the extent of disclosure of HIV positive status and correlates of non-disclosure at the time of ART initiation. Additionally, we aimed to compare actual disclosure experiences with stigma anticipated by patients in the event of HIV status disclosure. Assessment of disclosure-related patient perceptions and experiences in a setting where disclosure is highly encouraged will help generate evidence for the design of appropriate interventions and improvements to clinic-based counseling.
Methods
Study Setting
The six study sites are HIV clinics in the Oromia regional state of Ethiopia, and part of the Ethiopian National ART Program, overseen by the Oromia Regional Health Bureau. All sites are secondary health facilities in urban areas, with on-site CD4 testing capability and ART pharmacies. All offer onsite voluntary counseling and testing, perform provider initiated counseling and testing, and have an antenatal clinic, labor and delivery wards providing Prevention of Mother to Child Transmission (PMTCT) services. All of the clinics are open Monday to Friday for HIV care services, and four of the six are open seven days per week. All clinics offer adherence support for ART and pre-ART patients through adherence supporters and case managers.
Enrollment and Data Collection
Data collection consisted of structured patient interviews and abstraction of routine clinical information collected at patient visits.
Patient Interviews
All outpatients aged 18 years and older initiating ART at the six study clinics during June 2012–April 2013 were eligible for inclusion in the study. Eligible patients were referred by providers, given more information about the study and invited by study staff to participate on the day of ART initiation. Interested patients were screened for eligibility and requested to sign an informed consent form. Upon receipt of informed consent, study staff, who fluently spoke the two local languages, administered the 45–60 min structured questionnaire in Amharic or Oromiffa language as per participant preference. The questionnaire covered topics such as socio-demographics, HIV knowledge, HIV testing and care experience, HIV status disclosure, HIV beliefs, stigma, emotional health, and sexual history. Patients unable to complete the interview right away had up to 2 weeks to do so. Upon completion, participants were given a snack and money for transportation home from the clinic (20 birr ~1 USD).
Routine Clinical Information
Patient information routinely collected at enrollment in HIV care and during subsequent clinic visits (e.g. CD4 counts, disease stages, weight) was documented by clinicians on structured national forms. Trained data clerks entered the baseline and follow-up clinic visit information into electronic databases. Data quality assessments were done every 3 months to assess completeness, accuracy and paper-electronic data concordance.
Data Management
Interview data were double entered in a Microsoft Access database developed for the study and were linked with the de-identified clinic medical record data abstracted from patient-level electronic database for the period of HIV care enrollment through 12 months after ART initiation. The study was approved by the Institutional Review Boards of the Oromia Regional State Health Bureau, Columbia University Medical Center, and the City University of New York.
Outcome Definition
Disclosure was defined as sharing one’s HIV positive status with an individual other than clinic staff member (i.e. a health care provider, adherence counselor or case manager) at any point following diagnosis but prior to the date of ART initiation. Information on disclosure and its extent was obtained through two questions: (1) how many people, other than health care workers, participants had told their HIV status to; and (2) whether they had disclosed to specific persons such as their partner, parent, sibling, child, another relative, or friend.
Correlate Definitions
Patient Interviews
To identify possible associations between non-disclosure and fears about the consequences of sharing one’s HIV status, we examined the intensity of concern about unintended disclosure, as well as the number of concerns across categories of anticipated stigma, with items (alpha = 0.764) created in accordance with the concept described by Earnshaw and Chaudoir [21]. These items were later divided into four areas, based on principal component analysis: concerns about major life disruptions (loss of job or housing), partner’s reaction (violence, abandonment), impact on children (abuse, upset), and social implications and family reactions (different treatment by family, loss of friends, gossip, anxiety, negative impact on social relations). Impact on children was not used in this analysis, not to exclude participants who did not have children. We examined patients’ social environment, possibly reflecting the opportunity and/or support for disclosure, as knowing other PLWH, number of close friends, participation in a community group (dichotomized into traditionally close-knit groups, such as village committees and burial societies, and all others, for example credit or trade groups), control over household assets, as well as relationship status and having ever had children.
To explore possible associations with motivation for HIV testing and/or counseling differences between different types of testing sites, we also included unit/clinic of diagnosis: provider-initiated testing and counseling (PITC) and voluntary counseling and testing (VCT).
Reactions to disclosure were recorded separately for first person disclosed to and for partner (if not the first person), through a list of 13 yes/no items.
The earliest available diagnosis date (from self-report during interview and patient’s medical record) was used to compute the time between diagnosis and ART initiation.
Routine Clinical Information
Severity of illness at enrollment was based on the earliest CD4 and World Health Organization (WHO) stage measurements during the first three months in HIV care. For analysis, the variable was dichotomized into advanced disease (WHO stage III, IV, or CD4 < 150) and less advanced disease (WHO stage I or II).
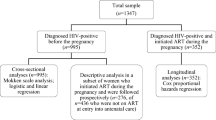
Statistical Methods
We conducted gender-stratified descriptive analyses, comparing the distribution of key characteristics between male and female participants using χ 2 and Mann–Whitney tests of statistical significance (p < 0.05). We further examined bivariate associations with non-disclosure through logistic regression, also using p < 0.05 as the level of statistical significance. To identify potential correlates of non-disclosure to anyone and to partner specifically, we developed two logistic regression models to estimate adjusted odds ratios (aOR). Multivariable regression models initially included age, gender and other variables that had p values < 0.20 in bivariate analyses. Covariates with the highest p values were eliminated through backward stepwise regression until all remaining variables had p values < 0.05. To rule out the possibility of negative confounding (i.e. associations observed only in the presence of other variables), excluded variables were added individually back into the model and retained if their p value was <0.05. Analyses were conducted in SAS 9.3 (Cary, NC) using generalized linear models (PROC GENMOD) with a logit link and generalized estimating equations to account for clustering of observations within clinical sites.
Results
Participant Characteristics
We interviewed 1182 patients initiating ART at the six study sites. After excluding 2 for being underage, the final dataset for this analysis comprised 1180 respondents. The mean age of participants was 34 years, interquartile range (IQR) 28–40. There were more female (61.2 %) than male (38.8 %) respondents, over two thirds (69.9 %) were Ethiopian Orthodox followers, 60.4 % had attended primary or secondary school, 57.0 % were in a relationship, and 78.0 % were urban residents. The median length of time since diagnosis was 8.3 months (IQR 1.1 months–3.4 years). (Table 1)
Levels of HIV Status Disclosure by Type of Confidant
Overall, 85.9 % of study participants disclosed their HIV status to at least one person prior to ART initiation. Although disclosure was high among both gender groups, female participants were more likely to disclose to anyone as compared to males (males 81.2 %, females 88.8 %, p < 0.001). Among 686 participants currently or previously in a relationship, 91.1 % disclosed their HIV status to their partners. Despite a lower overall disclosure rate, male participants were more likely than women to disclose their HIV status to their partner (males 94.1 %, females 88.9 %, p = 0.018). Over half (53.5 %) of respondents disclosed their HIV status to a family member other than their partner (males 46.5 %, females 57.9 %, p < 0.001). Over 50 % of respondents disclosed to two or more people (males 46.3 %, females 52.5 %, p = 0.001), whereas 14.1 % told no one (Table 2)
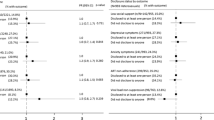
Factors Associated with Non-disclosure to Anyone
In the multivariable regression model, non-disclosure of HIV positive status to anyone prior to ART initiation was associated with not being in a relationship (aOR 2.84, 95 % CI 1.83–4.39), control over household assets (aOR 3.10, 95 % CI 2.15–4.48), and a strong concern about unintended disclosure (aOR 2.80, 95 % CI 1.72–4.57). An association was also observed between major disruption concerns and non-disclosure (1 concern vs. 0 aOR 1.54, 95 % CI 1.08–2.19; 2 vs. 0 aOR 2.08, 95 % CI 1.23–3.53). Factors associated with lower odds of non-disclosure were female gender (aOR 0.41, 95 % CI 0.33–0.52), having ever had children (aOR 0.55, 95 % CI 0.30–0.99), knowing other PLWH (aOR 0.36, 95 % CI 0.31–0.43), having three or more close friends (aOR 0.36, 95 % CI 0.18–0.73) and a longer period between HIV diagnosis and ART initiation (31 days–1 year vs. ≤30 days aOR 0.52, 95 % CI 0.36–0.76) ( Table 3).
Factors Associated with Non-disclosure to Partner
Non-disclosure of HIV status to one’s partner prior to ART initiation was strongly associated with female gender (aOR 4.03, 95 % CI 2.22–7.31), older age (40-44 vs. 25–29, aOR 1.92, 95 % CI 1.64–2.26; 45+ vs. 25–29 aOR 2.64, 95 % CI 1.54–4.51), secondary education (vs. none, aOR 1.68, 95 % CI 1.09–2.59), concern about social implications and family reactions (3–5 concerns vs. 0 aOR 3.63, 95 % CI 1.81–7.27), control over household assets (aOR 4.73, 95 % CI 2.76–8.10), and advanced stage HIV disease at enrollment in care (aOR 3.26, 95 % CI 1.76–6.04). Patients who knew other PLWH (aOR 0.21, 95 % CI 0.11–0.38), members of close-knit social groups (aOR 0.36, 95 % CI 0.15–0.91), and those with a longer time period since HIV diagnosis (31 days–1 year vs. ≤30 days aOR 0.62, 95 % CI 0.43–0.89) were less likely to withhold their HIV status from their partners (Table 3).
Reactions Upon Disclosure to First Person and Partner
Upon disclosure to the first confidant, 85.6 % of participants were encouraged to get treatment. About a third (30.9 %) were told not to tell anyone (males 26.1 %, females 33.8 %, p < 0.05), and 10.5 % said the first confidants became angry (males 17.5 %, females 6.4 %, p < 0.001). Upon disclosure to partner, the majority of participants received a supportive response: 82.2 % were encouraged to get treatment. Over three quarters (78.0 %) of participants reported that their partner decided to get tested for HIV if they didn’t already know their status (males 84.7 %, females 70.0 %, p < 0.001). Almost two thirds (62.8 %) of participants reported their partner was sad (males 72.4 %, females 55.2 %, p < 0.001). Additionally, 28.6 % (males 32.6 %, females 25.4 %, p < 0.05) reported their partner blamed them and 13.0 % (males 20.8 %, females 6.9 %, p < 0.001) stated that their partner was angry at them (Table 4).
Anticipated Stigma: Concerns of Patients Who Did Not Disclose to Anyone
Among the 167 (14.1 %) participants who had not disclosed their status to anyone, main concerns included unintended disclosure by confidant (73.9 %) and gossip (68.7 %). Participants who did not disclose also feared partner violence (63.3 %), abandonment by partner (54.2 %), upsetting their children (58.9 %), and child abuse or discrimination (52.3 %) in the event of HIV status disclosure (Table 5).
Discussion
This study examined the extent of disclosure of HIV positive status prior to ART initiation overall and by type of confidant, and factors associated with non-disclosure among patients initiating ART at 6 clinical sites in Oromia regional state, Ethiopia. The level of reported HIV status disclosure in our study was high, at 86 % overall and 91 % to partner, among those currently or previously in a relationship. The overall disclosure level we found was slightly lower than that reported by some studies among patients in HIV care in Ethiopia (76–95 %) [5–7]. However, disclosure to partner in our sample was generally higher than that reported elsewhere in the country (57–93 %) [5–7, 9–11]. The proportion disclosing to partner among those reporting a relationship was higher than the overall disclosure level in our sample, which may reflect the emphasis on disclosure to partner as a key component of family-centered ART preparatory counseling at the study clinics [20].
We found that knowing other PLWH and a longer period of time between HIV diagnosis and ART initiation were associated with lower odds of non-disclosure to partner and overall, in agreement with other studies in similar settings [7, 22]. This could be because some patients need to decide to whom and when to disclose, carefully weighing the risks and benefits of their choice. As they live longer with the infection, they might have more opportunities to meet PLWH who can share their experiences and support them on the path to disclosure [23].
Although women in our study were overall less likely than men to withhold their HIV status, they were more likely not to tell their partner, specifically. Although gender-specific disclosure levels to partner vary by context, studies in the region have found that women may fear blame of bringing HIV into the family and abandonment in the event of status disclosure to partner [7, 11, 23]. Some women may therefore need additional, culturally sensitive support to facilitate disclosure to partner, or counseling on the risks versus benefits of non-disclosure.
This study has also identified asset control as a predictor of non-disclosure, which is in agreement with previous reports of anticipation of economic support as a factor motivating disclosure [24–27]. Persons who consider themselves as in charge of household assets or household itself may not perceive a great need for additional support, or may fear losing their position in the household if their HIV-positive status is revealed. The association with asset control may also encompass employment, previously found to decrease the odds of disclosure, perhaps due to fear of workplace repercussions [28].
Odds of non-disclosure to partner were higher among participants who enrolled in HIV care at an advanced stage of HIV, which is contrary to results reported by Deribe [6] and counterintuitive, because noticeable signs of disease may make it harder to keep illness secret. Patients physically weakened by disease, however, may be more vulnerable in the possible event of a negative reaction to disclosure, which may affect their perception of risk and benefit: the fear of losing existing social support may outweigh the desire for additional support which could result from disclosure. Some patients with advanced HIV at enrollment in care may have also delayed HIV testing and/or accessing care, perhaps due to similar stigma-related concerns that appear to underlie non-disclosure. Additionally, debilitating symptoms may be a barrier to open communication with partners, which could be mediated by psychological distress associated with physical illness and the stress of sharing a diagnosis that may affect the partner. Odds of non-disclosure to partner also were consistently higher among participants older than 40, perhaps due to fear of blame for bringing sexually transmitted disease to the family; a finding which merits further in-depth inquiry. Prior research from Sub-Saharan Africa reported inconsistent associations between age and HIV status disclosure (higher likelihood of disclosure among older [29, 30] and younger [4, 31] persons), but our results suggest that older patients could benefit from tailored interventions in support of HIV status disclosure to partners.
However, odds of non-disclosure to partner were lower among those reporting membership in close-knit social groups. Among factors possibly mitigating disclosure-related stress and concerns, community groups relying on mutual trust (such as village or burial committees) may help provide social support beneficial in the process of HIV status disclosure. This is consistent with our finding that non-disclosure overall was less likely among patients who had three or more close friends, underlining the importance of social network in disclosure.
Finally, concerns ranging from reactions of the loved ones to unintended disclosure underscore patients’ need of control over the disclosure process and support across various settings where PLWH may encounter stigma or discrimination. Overall, reported disclosure experiences were largely positive; participants felt they were encouraged to get treatment by 86 % of first persons and by 82 % of partners they confided in. Supportive experience in our study was more common than described in Ethiopia by Gari and Seid [7, 11]. However, some participants faced non-supportive reactions including blame, anger, and being asked not to share their status further. Pervasive fear and reports of non-supportive experiences upon disclosure indicate a need to identify patients who could benefit from personalized support to minimize negative reception and cope with reactions that might otherwise compromise their care and health outcomes. While it is encouraging that only a fraction of those who have disclosed their HIV status faced serious consequences such as physical violence, loss of housing or children (less than 1 % each), persons who still haven’t disclosed their HIV status and report such fears may be those at highest risk of negative reactions.
Importantly, timely disclosure appears to have facilitated partner decision to undergo HIV testing, which has the potential effect of resulting in earlier HIV diagnosis among partners than would have occurred without disclosure. Partners of persons with HIV are more likely to be HIV positive themselves, and therefore, disclosure can have a potential public health effect of earlier diagnosis and more timely treatment initiation, potentially reducing onward spread of HIV. Additionally, partners who test negative can provide an indication for earlier HIV treatment of the index patient, which has been shown to reduce transmission by 96 % in serodiscordant couples [32].
The major strength of this study comes from the time of assessment of HIV status disclosure (ART initiation), a period during the HIV care continuum when disclosure is of great importance, as it may impact patients’ subsequent engagement and success in treatment. The care procedures and environment in which the study was conducted are similar to other HIV care and treatment settings across Ethiopia, allowing the results of this study to inform future interventions and programmatic planning in the region.
However, there may have been a social desirability bias due to the fact that participants were interviewed on the premises of the care and treatment facility where they went through ART preparatory sessions that strongly encourage patients to disclose their HIV status as a critical step to build treatment support and initiate family-centered care. We also did not capture the information on the reason for disclosure, when and how it happened, as well as possible differences in initial and follow-up reactions to disclosure. Since our study was focused on a segment of PLWH (those with clinical HIV care experience in an urban setting) at a specific point in the HIV care cascade (ART initiation), estimates of disclosure rates cannot be generalized to the general HIV infected population.
Conclusions
Our findings revealed high levels of HIV status disclosure, with 86 % of respondents reporting disclosure to anyone and 91 % of those currently/previously in relationships reporting disclosure to their partners. Though women were overall less likely not to tell anyone about their HIV status than men, they had higher odds of not disclosing to partner, and may need targeted support in this respect. Patients 40 years of age and older, those who enrolled with advanced HIV and those initiating treatment soon after diagnosis may benefit from additional help to disclose their status to people in their lives who can offer support. Concerns about life disruptions, social reactions, and potentially about diminished role in household were barriers to disclosure and should be addressed during ART preparatory and follow-up counseling sessions. Though HIV status disclosure experiences in our study were largely positive, some patients also faced a negative reception. Presence of such reactions necessitates continued policy emphasis on fostering greater social support for PLWH and, on the clinic level, a personalized counseling approach to support patients to disclose in a way that minimizes negative reactions and provides coping skills for various life contexts in which negative consequences may occur. Future research should examine the effect of time-updated disclosure status on outcomes following ART initiation, such as care engagement, medication adherence, and retention in HIV care.
References
Joint United Nations Programme on HIV/AIDS. Opening up the HIV/AIDS epidemic. Guidance on encouraging beneficial disclosure, ethical partner counselling and appropriate use of HIV case-reporting. Geneva: World Health Organization. 2000.
Southern African AIDS Trust. Guidelines for Counseling on Disclosure of HIV Status. Southern African AIDS Trust. 2011.
Petrak JA, Doyle A-M, Smith A, Skinner C, Hedge B. Factors associated with self-disclosure of HIV serostatus to significant others. Br J Health Psychol. 2001;6(1):69.
Medley A, Garcia-Moreno C, McGill S, Maman S. Rates, barriers and outcomes of HIV serostatus disclosure among women in developing countries: implications for prevention of mother-to-child transmission programmes. Bull World Health Organ. 2004 Apr;82(4):299–307.
Deribe K, Woldemichael K, Njau BJ, Yakob B, Biadgilign S, Amberbir A. Gender differences regarding barriers and motivators of HIV status disclosure among HIV-positive service users. SAHARA J. 2010;7(1):30–9.
Deribe K, Woldemichael K, Wondafrash M, Haile A, Amberbir A. Disclosure experience and associated factors among HIV positive men and women clinical service users in Southwest Ethiopia. BMC Public Health. 2008;8:81.
Gari T, Habte D, Markos E. HIV positive status disclosure among women attending art clinic at Hawassa University Referral Hospital, South Ethiopia. East Afr J Public Health. 2010 Mar;7(1):87–91.
Genet M, Sebsibie G, Gultie T. Disclosure of HIV seropositive status to sexual partners and its associated factors among patients attending antiretroviral treatment clinic follow up at Mekelle Hospital, Ethiopia: a cross sectional study. BMC Res Notes. 2015;8:109.
Kassaye KD, Lingerh W, Dejene Y. Determinants and outcomes of disclosing HIV-sero positive status to sexual partners among women in Mettu and Gore towns, Illubabor Zone southwest Ethiopia. Ethiop J Health Dev. 2005;19(2):126–31.
Reda AA, Biadgilign S, Deribe K, Deribew A. HIV-positive status disclosure among men and women receiving antiretroviral treatment in eastern Ethiopia. AIDS Care. 2013 Aug;25(8):956–60.
Seid M, Wasie B, Admassu M. Disclosure of HIV positive result to a sexual partner among adult clinical service users in Kemissie district, northeast Ethiopia. Afr J Reprod Health. 2012 Mar;16(1):97–104.
Alemayehu M, Aregay A, Kalayu A, Yebyo H. HIV disclosure to sexual partner and associated factors among women attending ART clinic at Mekelle hospital, Northern Ethiopia. BMC Public Health. 2014;14:746.
Mills EJ, Nachega JB, Buchan I, Orbinski J, Attaran A, Singh S, et al. Adherence to antiretroviral therapy in sub-Saharan Africa and North America: a meta-analysis. JAMA J Am Med Assoc. 2006 Aug 9;296(6):679–90.
Skhosana N, Struthers H, Gray G, McIntyre J. HIV disclosure and other factors that impact on adherence to antiretroviral therapy: the case of Soweto, South Africa. Afr J AIDS Res. 2006;5(1):17–26.
Kalichman SC, Nachimson D. Self-efficacy and disclosure of HIV-positive serostatus to sex partners. Health Psychol. 1999 May;18(3):281–7.
Stirratt MJ, Remien RH, Smith A, Copeland OQ, Dolezal C, Krieger D. The role of HIV serostatus disclosure in antiretroviral medication adherence. AIDS Behav. 2006 Sep;10(5):483–93.
Waddell EN, Messeri PA. Social support, disclosure, and use of antiretroviral therapy. AIDS Behav. 2006 May;10(3):263–72.
Central Statistical Agency [Ethiopia] and ICF International. Ethiopia Demographic and Health Survey. Addis Ababa: Central Statistical Agency and ICF International. 2011.
Joint United Nations Programme on HIV/AIDS (UNAIDS). Global report: UNAIDS report on the global AIDS epidemic 2013. Geneva. 2013. 978-92-9253-032-7.
Federal HIV/AIDS Prevention and Control Office. Federal Ministry of Health. Guidelines for Implementation of the Antiretroviral Therapy Programme in Ethiopia. Federal HIV/AIDS Prevention and Control Office. Federal Ministry of Health. 2007
Earnshaw VA, Chaudoir SR. From conceptualizing to measuring HIV stigma: a review of HIV stigma mechanism measures. AIDS Behav. 2009;13(6):1160–77.
Makin JD, Forsyth BW, Visser MJ, Sikkema KJ, Neufeld S, Jeffery B. Factors affecting disclosure in South African HIV-positive pregnant women. AIDS patient care and STDs. 2008 Nov;22(11):907–16.
Kulkarni S, Hoffman S, Gadisa T, Melaku Z, Fantehun M, Yigzaw M, et al. Identifying perceived barriers along the HIV care continuum: findings from providers, peer educators, and observations of provider-patient interactions in Ethiopia. J Intern Assoc Provid AIDS Care. 2015. doi:10.1177/2325957415593635.
Akani CI, Erhabor O. Rate, pattern and barriers of HIV serostatus disclosure in a resource-limited setting in the Niger delta of Nigeria. Trop Doct. 2006;36(2):87–9.
Antelman G, Smith Fawzi MC, Kaaya S, Mbwambo J, Msamanga GI, Hunter DJ, et al. Predictors of HIV-1 serostatus disclosure: a prospective study among HIV-infected pregnant women in Dar es Salaam, Tanzania. AIDS (London, England). 2001;15(14):1865–74.
Ezegwui HU, Nwogu-Ikojo EE, Enwereji JO, Dim CC. HIV serostatus disclosure pattern among pregnant women in Enugu, Nigeria. J Biosoc Sci. 2009 Nov;41(6):789–98.
Kadowa I, Nuwaha F. Factors influencing disclosure of HIV positive status in Mityana district of Uganda. Afr Health Sci. 2009;9(1):26–33.
Longinetti E, Santacatterina M, El-Khatib Z. Gender perspective of risk factors associated with disclosure of HIV status, a cross-sectional study in Soweto, South Africa. PLoS ONE. 2014;9(4):e95440.
Maman S, Mbwambo JK, Hogan NM, Weiss E, Kilonzo GP, Sweat MD. High rates and positive outcomes of HIV-serostatus disclosure to sexual partners: reasons for cautious optimism from a voluntary counseling and testing clinic in Dar es Salaam, Tanzania. AIDS Behav. 2003 Dec;7(4):373–82.
Ndiaye C, Boileau C, Zunzunegui MV, Koala S, Aboubacrine SA, Niamba P, et al. Gender-related factors influencing HIV serostatus disclosure in patients receiving HAART in West Africa. World Health Popul. 2008;10(3):43–54.
Farquhar C, Ngacha D, Bosire R, Nduati R, Kreiss J, John G, editors. Prevalence and correlates of partner notification regarding HIV-1 in an antenatal setting in Nairobi, Kenya. XIII International AIDS Conference; 2000.
Cohen MS, Chen YQ, McCauley M, Gamble T, Hosseinipour MC, Kumarasamy N, et al. Prevention of HIV-1 infection with early antiretroviral therapy. N Engl J Med. 2012 Aug 11;365(6):493–505.
Acknowledgments
This study was funded by a grant from the National Institutes of Health R01 (5R01MH89831) entitled “Multi-level determinants of late ART initiation in sub-Saharan Africa” (LSTART) and the President’s Emergency Plan for AIDS Relief (PEPFAR).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Gadisa, T., Tymejczyk, O., Kulkarni, S.G. et al. Disclosure History Among Persons Initiating Antiretroviral Treatment at Six HIV Clinics in Oromia, Ethiopia, 2012–2013. AIDS Behav 21, 70–81 (2017). https://doi.org/10.1007/s10461-016-1290-4
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10461-016-1290-4