This paper investigates the association between social support, disclosure of HIV/AIDS, and odds of initiating combination antiretroviral drug therapy in its first years on the market. Data are drawn from the first three rounds of the Community Health Advisory and Information Network (CHAIN) survey, collected between 1994 and 1997. CHAIN documents service needs and rates of service utilization among a representative sample of persons with HIV/AIDS in New York City. A two-step logistic regression estimated associations between (1) perceived social support and use of combination antiretroviral therapy, and (2) the interaction between concealing HIV/AIDS and perceived social support. Results offered evidence that the positive association between social support and use of highly active antiretroviral treatment (HAART) and other combination antiretroviral therapies is contingent upon disclosure of HIV status within the household or among friend and acquaintance networks. A positive association between social support and odds of using combination therapy was only observed among those who disclosed their HIV status.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
INTRODUCTION
Since highly active antiretroviral treatment (HAART) became available in 1996, lengths of hospital stays, frequency of opportunitistic infections, and death rates have significantly decreased in developed countries (Herlitz and Steel, 2001). However, efforts to conceal one's diagnosis can pose a serious barrier to use of available medications. Fear of disclosing positive HIV status or HIV-related risk behaviors is directly associated with delays in HIV testing and entry into care after a positive diagnosis (Chesney and Smith, 1999; Fortenberry et al., 2002; Valdiserri, 2002). This paper examines the complex association between perceived social support, disclosing one's HIV status, and the odds of initiating combination antiretroviral drug therapy in its first years on the market. We specifically assess the moderating effect of concealing one's positive HIV status from household members, friends, or relatives on the association between social support and odds of treatment.
It is well known that social support can improve health through a variety of mechanisms. These include enhanced access to resources, enhanced immune response, and improved health-related behaviors. Integration into supportive networks has been shown to improve mental and physical health by reducing levels of stress or by buffering individuals from stressors that diminish health and well-being (Turner and Turner, 1999). Connection to social supports has been shown to reduce risk behaviors and increase emotional bonding through provision of information and advice, and positive peer influence (Ennett et al., 1999; Litwak and Messeri, 1989; Resnick et al., 1997). Moreover, access to information and peer support from friends and acquaintances is likely to improve odds of initiating treatment.
Disclosure of one's HIV status to potential helpers is required to garner maximum social support to improve access to HIV treatment or to cope with the potentially debilitating side related to antiretroviral therapy. Individuals who conceal their HIV status from friends and acquaintances within and outside the household may limit their access to information about available services, reduce potential peer support for engaging in treatment, or postpone treatment altogether if the regimen would disclose his/her HIV/AIDS to household or other network members. For example, if one discloses HIV to a supportive network, he or she could take advantage of the instrumental, informational, emotional, and financial resources contained in that network to improve access to medications. If the same individual attempts to maintain supportive networks while concealing HIV, his or her efforts to conceal the disease may override efforts to access care.
In the current study, our analysis is guided by theoretical and empirical research on social support and stigma (Klitzman and Bayer, 2003) and classic theories of scila stigma. Goffman (1963) describes social stigma as a powerful phenomenon experienced by individuals who share an attribute that “makes [them] different from others in the category of persons available for [them]…an attribute that is deeply discrediting [and observable through] a language of relationships” (p. 3). For many persons living with HIV/AIDS, being HIV positive represents a stigmatizing social identity that may modify the normal operation of social support.
We operationalize perceived stigma with measures of concealing HIV from household members, relatives, and friend/acquaintance networks. Concealing one's HIV/AIDS status is conceived here as a stigma management strategy that moderates the expected positive influence of social support on use of medication. We tested two hypotheses; (1) we expected that perceptions of strong social support from networks comprised of household members, friends/acquaintances, and relatives would be associated with increased odds of using combination antiretroviral therapy, controlling for health status and socio-demographic characteristics, and (2) we predicted that concealing HIV status from network members would moderate the hypothesized positive association between social support and use of combination therapy.
METHODS
Study data were obtained from the first three rounds of interviews from the Community Health Advisory and Information Network (CHAIN) survey. CHAIN was initiated in 1994 in New York City. As part of the evaluation activities, this ongoing survey provides systematic data from the perspective of a representative sample of persons living with HIV/AIDS in New York City. Participants provide detailed information about their needs for health and human services, their encounters with the full continuum of HIV services, and their physical, mental, and social well-being. The survey includes measures of perceived social support from friend and family networks.
Study Sample
CHAIN participants were sampled from over 300 New York City health and social service agencies with HIV caseloads of at least 20 adults over age 20. The sample was drawn in a manner that created a cohort that would be generally representative of the population of people with HIV in all five boroughs of New York City who were aware of their infected status and enrolled in health or social services (excluding private doctors) during 1994. A two-stage sample design was implemented. The first stage sampled 50 recruitment sites from a list of 300 service agencies known to have HIV caseloads of 20 or more. Of the 50 agencies sampled, 43 agreed to assist in recruiting clients for the CHAIN cohort. Thirty agencies prepared a list of their HIV clients, including their gender and date of enrollment in the agency, substituting random IDs for client names before sending the list to CHAIN. CHAIN staff selected IDs at random and sent these back to the agencies for initial contact. When clients agreed, the agency turned over their names and contact information to Columbia staff members, who then obtained informed consent and scheduled the interview. Participants at the remaining agencies were recruited through a sequential enrollment process on site. Agency staff obtained written permissions from perspective clients before CHAIN staff approached them with an invitation to enroll in the study.
The original cohort members were re-inter-viewed up to seven times and received $25 in transportation or food vouchers as compensation for each interview. Follow-up interviews were scheduled for 6-month intervals for the second through fourth rounds of interviews. In order to yield a high rate of return with a difficult to reach population, the actual interval between interviews was often longer than 6 months, and most occurred between 6 and 9 months. Because this study assesses initiation of combination therapy in its early years, we made use of the first three rounds of interview data, Round 1 in 1994–1995, Round 2 in 1995–1996, and Round 3 in 1996–1997. The third round roughly coincides with the period in which the first combination therapy was available for general medical practice. After 1997, HAART was more widely available.
At the time of recruitment in 1994–1995, the demographic composition of the study sample was quite similar to surviving AIDS cases in New York City. The only substantial deviation between the New York City AIDS cases and the study sample population is associated with gender; women were intentionally over-sampled to yield approximately one female for every two males sampled. Table I displays the demographic composition of participants included in the present study compared to New York City's adult HIV population in 1994.
Of the 700 participants interviewed at Round 1, 480 were re-interviewed at Round 3. Of those who were not re-interviewed at Round 3, 106 were deceased at the time of follow-up; 27 moved out of New York City and were no longer eligible to participate in the study; 5 were not mentally competent to complete the interview; 12 were institutionalized and unable to complete the interview; 21 refused; and 49 were lost to follow-up. An additional 21 cases were excluded from this study due to incomplete data on medications used or missing information on social support networks. Compared to those who were not re-interviewed, participants who were re-interviewed at Round 3 (n = 480) were significantly more likely to be female and to report problem drug use (PDU). Members of the study sample were less likely than the original cohort to be Latino. There was no significant difference in baseline age between the study sample and the full cohort.
As displayed in Table I, the majority of the study sample was between the age of 30 and 49. With regard to primary HIV risk factors, 39% of males reported having sex with other men, while 52% reported current or former problem drug use. Among women, 59% reported current or former problem drug use. The majority of the study sample (96%) indicated that they were connected to health or social services at Round 1. Most participants were housed at Round 1, 4% were in institutional settings, with 50% of the sample reporting additional household members. At the baseline, 24% of participants were asymptomatic, 16% were symptomatic without an AIDS diagnosis, and 60% had been diagnosed with AIDS. At Round 3, only 12% remained asymptomatic, 11% were symptomatic without an AIDS diagnosis, and 77% had been diagnosed with AIDS.
Survey Instrument
Data for the CHAIN interviews were collected through personal face-to-face interviews conducted by trained interviewers. The interview drew wherever possible on batteries of questions previously validated in HIV-positive populations. The interview schedule was carefully reviewed by members of the Planning and Evaluation Committee as well as an advisory committee of PLWHs. The complete interview schedule includes 15 sections containing 500 items covering topics in six domains: initial encounter with the health-care delivery system, need for services, access, utilization, and satisfaction with health and social services, socio-demographic characteristics of participants, informal care-giving from friends, family and volunteers, and quality of life with respect to health status, psychological functioning, and social functioning. The interviews took between 2 and 3 hr to complete, depending upon issues relevant to each client's unique service needs. Interviews were conducted in English or Spanish, depending on participant preference.
Measures
This study analyzes responses to CHAIN questions measuring socio-demographic characteristics, health status, perceived social support, HIV disclosure, and use of combination ART. Health status was assessed using survey questions that have well-established psychometric properties, such as the Medical Outcomes Survey (MOS) that have been widely administered to HIV-positive populations (Steward et al., 1991).
Prior research confirmed that use of HAART by the CHAIN cohort members was associated with reduced mortality risk (Messeri et al., 2003). Due to its demonstrated efficacy in extending the lives of HIV-positive individuals during our study period (1994–1997), use of combination therapy in its earliest years is an important measure of access to appropriate medical care. Treatment guidelines for New York State recommend that all persons with an AIDS diagnosis, or a CD4 count less than 200 should start treatment with antiretroviral therapy. Initiation of combination therapy was measured as a dichotomous variable indicating self-reported use of two or more antiretroviral medications at Round 3 (1996–1997) of the CHAIN study. The dependent variable captures initiation of both HAART and earlier combination therapy regimens that were considered to be “appropriate care” by the New York State Department of Health during the four years when combination therapies were first approved for general clinical practice. This allowed us to include participants who initiated therapy prior to the wide availability of HAART.
Concealing HIV status is measured at Rounds 1 and 3, with separate indicators for household members, friends, or acquaintances outside the household, and relatives outside of the household. Conceals HIV from Friends is a dichotomous variable indicating that none of the following “are aware of your HIV status”: close friends, neighbors, coworkers, or acquaintances from church, clubs, school, or other organizations, including support groups. Conceals HIV from Relatives is a dichotomous variable indicating that no relatives outside of the household “are aware of your HIV status.” Because even one network member can provide strong support for use of medication or pose a barrier to treatment, we chose to use dichotomous measures indicating the sharp distinction between reporting no disclosure and even partial disclosure within the support group. While very few participants indicated no disclosure within their support networks, failing to share one's HIV status with even one close associate suggests that the participant was actively concealing the HIV/AIDS diagnosis. Conceals within Household is also a dichotomous variable, but it indicates that the participants concealed from at least one household member. We argue that concealing from just one household member could restrict one's willingness or ability to safely take medications at home.
The CHAIN survey questions permit clear differentiation between the types of support available through specific informal network ties, and also allow for the specification of sequential relationships between perceived support and health seeking behavior. We assessed the overall supportiveness of informal social networks by constructing a global measure of social support that comprises indicators of perceived availability of help from household members, friends/acquaintances outside the household, and relatives outside of the household. During their baseline and follow-up interviews, participants identified and listed up to 21 network members. Measured ties included one spouse/partner, up to five household members, up to five friends, up to five relatives who live outside the home, and up to five acquaintances. From this list, participants then identified specific network members whom they could “count on” for seven specific types of support across four domains: instrumental (i.e., transportation or running errands; home care when confined to bed), informational (i.e., recommending a dentist who treats HIV patients; locating housing), emotional (i.e., discussing troubles with family relationships; hanging out just for fun), and financial (i.e., lending several hundred dollars in an emergency) support.
For each of the four support domains, initial scales were constructed for acquaintance friend, household, and relative support, resulting in a total of 16 scales. The maximum score for each scale is the product of the number of questionnaire items in the support domain, either one or two, and the maximum number of persons listed in the relationship, six for household and five for the other three relationships. For example, if a participant indicated that three friends were potential providers of emotional support for both “troubles with family relationships” and “hanging out just for fun,” and a fourth friend was available only for “hanging out,” that participant would receive a score of 7 out of a possible 10 on the Friend Emotional Support scale. If another participant reported that only two friends were available for “hanging out,” and had no friends that were potential providers of help with “family relationships,” he would receive a score of 2 out of a possible 10 on the same scale. Since there was variation in the number of items included in each support domain, as well as the number of ties in each type of relationship, the summary scores were standardized as proportions. A score of 1.0 indicates that the participant listed the maximum amount of perceived support in each domain.
To assess the validity of including 16 separate social support scales in the analysis, we performed a principle components analysis to verify that the measured dimensions of social support were in fact distinct within the study population. Results indicated that a single underlying factor explained 37% of the variance across the 16 scales at Round 1 and 36% at Round 3 (eigenvalues = 5.995 and 5.778, respectively). Factor loadings ranged from .439 to.774. at Round 1 and from .401 to .770 at Round 3. Since the scales consistently loaded on a single factor at both Round 1 and Round 3, we combined the 16 scales into a single Social Support Scale (alpha = .89 at Round 1; alpha = .87 at Round 3). For ease of the interpretation in the logistic regression models, we then dichotomized the Social Support Scale. A score at or below the 50th percentile is considered low, and a score above the 50th percentile (3.0 out of a possible 16.0) is considered high.
Education and income level were excluded from the multivariate models due to insufficient variance in the CHAIN sample and lack of correlation with the dependent variable (results of Chi-square analyses are available from the authors upon request). Within our study sample, 25% of participants completed high school. The majority of participants reported income levels at or near the poverty line, and most received some sort of public assistance at the time of the interview.
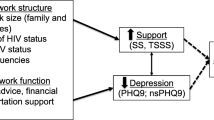
Statistical Analysis
This project employed statistical analyses of panel data from Rounds 1, 2, and 3 of the CHAIN study. As described above, we examined the association between social support on use of combination therapy and the moderating effect of concealing HIV/AIDS on the expected positive relationship between social support and use of combination ART. We implemented two logistic regression models. Interaction terms indicating high social support with and without disclosure to friends/acquaintances, household members, and relatives outside of the home were added to Model 2. Both models included Round 1 measures of baseline data including gender, age, race/ethnicity, use of antiretroviral therapy, social support, and disclosure; Round 2 measures of health status and quality of medical care; and Round 3 measures of social support and disclosure. Model 2 includes Round 1 and Round 3 interaction terms indicating social support with and without disclosure of HIV status. In addition, Wald tests were performed to assess the significance of the Model 2 interactions.
RESULTS
The models below estimate the association between perceived social support and use of any combination of two or more antiretroviral drug therapies between 1995 and 1997, including, but not limited to HAART. Approximately 37% of the study sample reported use of any antiretroviral therapy at Round 1 of the CHAIN study. Of those, 46 participants (9.6% of the sample) indicated that they had used a combination of two or more antiretrovirals. These participants likely obtained combination therapy through participation in clinical trials before these treatments were widely available. By Round 3, 42% of the study sample indicated that they used two or more antiretrovirals, including 64 participants who had initiated HAART.
As indicated in Table II, participants reported fairly low levels of social support at both Rounds 1 and 3 of the CHAIN study. Participants were most likely to report emotional and information support from friends, while financial support and instrumental support were more likely to come from household members. Across domains, the mean Social Support Scale score was only 3.3 out of a possible 16 at Round 1, and 3.14 at Round 2. At Round 1, 47% of the sample scored at or above 3.0, indicating relatively high social support, and 48% scored at or above 3.0 at Round 3.
The frequency of disclosure varied somewhat by relationship to the study participant. At the study baseline, 14% of participants concealed their HIV status from all friends and acquaintances outside of the household. At Round 1, 18% of the study sample concealed their HIV status within the household, and 14% concealed within their household at Round 3. Twenty-two percent concealed from all relatives outside the household at Round 1, and 17% concealed at Round 3. Finally, 14% of participants said that they concealed their HIV status from all friends, neighbors, acquaintances, and coworkers outside the household at Round 1, while 13% concealed from all friends and acquaintances at Round 3.
The logistic regression models presented in Table II suggest that the positive association of social support on participants’ use of combination therapy is contingent on disclosing one's HIV status to network members. As shown in Table II, Model 1, which does not specify interaction terms, does not show a statistically significant association between High Social Support at Round 1 or Round 3 and combination therapy at Round 3. Addition of the interaction terms to Model 1 significantly improves its predictive value, step X 2 (df = 6) = 14.21, p < .05. The odds ratios associated high support at Round 1 and Round 3 are similar in Model 1, 1.12 and 1.36, respectively, but the interaction model indicates a significant cross-sectional association between high support and use of the medications at Round 3, but only when HIV status is disclosed within the household or the friend/acquaintance network. To interpret the interaction effect, it is necessary to multiply the odds ratios associated with social support and the appropriate interaction term. For those who disclosed within the household, social support is associated with a 200% increase in the odds of using combination therapy. For those who conceal their status from at least one household member, high social support is actually associated with a 48% decline in the odds of treatment. Concealing one's HIV status from one's entire network of friends and acquaintances similarly moderates the positive association between support and treatment that is present among those who disclose their HIV. For those who conceal, from friend networks, high social support is associated with an 80% decline in odds of initiating combination therapy. Wald tests showed that the coefficients associated with the social support*household conceal and social support*friend/acquaintance conceal interactions were significant, X 2 (df = 2) = 7.79 and X 2 (df = 2) = 10.47, respectively.
Figures 1 and 2 illustrate the change in the association between social support and treatment when HIV is concealed from friends/acquaintances or within the household. In these figures, the regression equations are used to estimate the predicted probability of use of antiretrovirals for concealers and disclosers. Predicted probabilities were derived by setting the other covariates in the model to their mean value. Among those who disclose their HIV status within their friend/acquaintance networks, our logistic regression model predicts that the average odds of using combination therapy are .38 for those with low social support (n = 194) and .46 for those who perceive high social support (n = 204). Among the much smaller group of participants who concealed their HIV from all friends and acquaintances, odds of using combination therapy were higher when social support was low. For those with low support (n = 43), the average odds of treatment were .44, compared to .13 among those who maintained high social support while concealing their HIV (n = 16).
As shown in Fig. 2, this pattern was repeated when we compared the patterns of social support and odds of treatment between those who concealed from a household member and those who did not.
For those who did not conceal their HIV from any household members, the mean odds of treatment were .37 among those with low support (n = 195), compared to .46 among those with high support (n = 198). The pattern was reversed among those who concealed their HIV at home. In this case, the model predicts that the average odds of treatment are .52 for those with low support (n = 42), compared to only .21 for those who continue to rely on household support while concealing HIV (n = 22).
Although social support at Round 3 (contingent on disclosure to friends or household members) was among the strongest predictors of combination therapy in the model, the largest effect size was use of any antiretrovirals at Round 1 (OR = 3.6), followed by age. Participants aged 50 and older were 2.5 times as likely to report combination therapy as those aged 30–39. Self-reported problem drug use (OR = .50) and black race/ethnicity (OR = .49) were negatively associated with the treatment. As expected, participants with lower T-cell counts at Round 2 were more likely than others to use combination therapy at Round 3, controlling for other factors.
DISCUSSION
Our findings offer evidence that, within the context of a stigmatized disease, the generally expected positive influence of social support is not necessarily associated with improved treatment outcomes. In fact, social support was negatively associated with use of combination therapy when HIV status was concealed within the household or from networks of friends and acquaintances. We posit that initiating an unfamiliar treatment that has potentially visible side effects and requires storage of medication in the home would increase risk of HIV/AIDS disclosure. If one is actively concealing their HIV/AIDS status while maintaining network ties, such a risk becomes a barrier to treatment.
The longitudinal design of the CHAIN study improves our ability to model the net associations between perceived support and concealing HIV on initiation of treatment over time. We observed that the joint influence of perceived social support and disclosing HIV status to network members was cross-sectional, with Round 3 support associated with Round 3 treatment, but the nature of participants’ social connections and perceived availability of support are assumed to precede treatment. We do not expect that perceived social support and decisions to conceal HIV are determined by starting a regimen of combination therapy. Exogenous influences on social support and disclosure are controlled by including baseline measures of perceived support and disclosure to friends, household members, and relatives at Round 1, as well as health status at Round 2.
These results may not be generalizable beyond New York City, where there is a relatively high prevalence of HIV/AIDS, good access to services, and a large, open and supportive community of PLWHs. In New York City, we found that the observed moderating effects of concealing HIV were similar across race, gender, and sexual orientation. However, it is the case that MSMs are less likely to conceal their HIV status than women or other men. It is likely that rates of concealing HIV/AIDS are lower in New York City than other regions, but the general principles of our findings and their statistical significance should maintain in other regions. Note that Fife and Wright (2000) found a similar negative association between social support health outcomes within stigmatized populations living with HIV/AIDS or cancer in the Midwest. Concealing one's HIV status may have an even more prominent effect on treatment in an environment where HIV/AIDS is less prevalent.
The social network variables available for this study have two general limitations, but these do not substantially impact the reliability or validity of the analysis. First, the CHAIN social network questions are “ego-centered,” meaning that potential supporters were not followed up to verify their relationships to the participants. In marginalized populations such as this study's target group, bounded groups can be nearly impossible to identify and recruit into a study. For these reasons, egocentric data are actually preferable to complete network data in such populations, because sample size is increased (Cunningham et al., 1998; Ennett et al., 1999). Second, the participants were limited in the number of names they could supply. This data collection strategy, known as “fixed choice,” introduces measurement error into the analysis, as it restricts the nomination process—and imposes a ceiling on network size (Wasserman and Faust, 1994). However, we would only consider this to be a flaw in the study design if a substantial proportion of participants had listed the maximum number of network members at Rounds 1 and 3. Of the 459 participants included in the study, only 10% listed more than 15 network members, and only 1 participant listed 21 network members.
Wright and Fife (1999) proposed three theoretical possibilities for the influence of social support and stigma on “adjustment to serious illness” (i.e., social support and stigma have independent effects, social support buffers the negative effects of stigma, and stigma influences the social support available). Consistent with Fife and Wright (2000), our findings suggest that the effects of stigma and social support interact. Our findings suggest that while social support is associated with higher rates of treatment, the effect of concealing status on use of medication is not independently meaningful. Rather, concealing HIV moderates the influence of social support on the odds of using appropriate medication. Continuing efforts to reduce the stigma surrounding a diagnosis of HIV/AIDS are critical, as concealing status is among the most common strategies used to manage HIV stigma and can present a serious barrier to adequate medical treatment.
Our findings reinforce the need for our research to carefully consider contextual effects when we study the impact of social support of health outcomes. Within marginalized populations living with HIV, the best sources of support are likely contained in weaker tie relationships that lie beyond the network core. Among gay men in particular, even emotionally supportive roles traditionally occupied by family members are taken on by friend networks (Bartelli, 2000). Identification of social mechanisms through which social support networks reduce morbidity is critical to the design and implementation of social interventions targeted to disconnected populations. We need to understand how social supports can be effectively integrated into systems of care for HIV/AIDS populations, as their social networks are uniquely affected by declining health status, poor access to health resources, and high rates of risky health behavior.
Future research should investigate specific populations within which concealing HIV status from support network members significantly impedes treatment. Personal acceptance of one's identity and talking to family members about AIDS is positively correlated with support (Johnston et al., 1995). The prevalence of stigmatizing social processes of rejection, discrimination, and isolation in particular cultural contexts should also be the focus of future research. When providing case management services to individuals with HIV/AIDS, medical and social service providers must take the extra step to review the client's social environment to determine the potential positive or negative influence of one's social networks on use of available treatment.
REFERENCES
Bartelli, D. (2000). The company they keep. Dr. PH. dissertation, Department of Sociomedical Sciences, Mailman School of Public Health, Columbia University, New York, NY.
Chesney, M. A., and Smith, A. W. (1999). Critical delays in HIV testing and care. American Behavioral Scientist, 42 1158–1170.
Cunningham, W. E., Hays, R. D., Ettl, M. K., Dixon, W. J., Liu, R. C., Beck, C. K., and Shapiro, M. F. (1998). The prospective effect of access to medical care on health-related quality-of-life outcomes in patients with symptomatic HIV disease. Medical Care, 36 295–306.
Ennett, S. T., Bailey, S. L., and Federman, E. B. (1999). Social network characteristics associated with risky behaviors among runaway and homeless youth. Journal of Health and Social Behavior, 40 63–78.
Fife, B. L., and Wright, E. R. (2000). The dimensionality of stigma: A comparison of its impact on the self of persons with HIV/AIDS and cancer. Journal of Health and Social Behavior, 41 50–67.
Fortenberry, J. D., McFarlane, M., Bleakley, A., and Bull, S. (2002). Relationships of stigma and shame to gonorrhea and HIV screening. American Journal of Public Health, 92 378–381.
Goffman, E. (1963). Stigma: Notes on the Management of Spoiled Identity. Englewood Cliffs, NJ: Prentice-Hall.
Hammer, M. (1983). “Core” and “extended” social networks in relation to health and illness. Social Science and Medicine, 17 405–411.
Herlitz, C. A., and Steel, J. L. (2001). Highly active antiretroviral therapy (HAART): Awareness and beliefs about infectivity and the influence on sexual behaviour in the general population of Sweden. European Journal of Public Health, 11 251–256.
Johnston, D., Stall, R., and Smith, K. (1995). Reliance by gay men and intravenous drug users on friends and family for AIDS-related care. AIDS Care, 7 307–319.
Klitzman, R., and Bayer, R. (2003). Mortal Secrets: Truth and Lies in the Age of AIDS. Baltimore, MD: The Johns Hopkins University Press.
Link, B. G., and Phelan, J. C. (2001). Conceptualizing stigma. Annual Review of Sociology, 27 363–385.
Litwak, E., and Messeri, P. A. (1989). Organizational theory, social supports, and mortality rates: A theoretical convergence. American Sociological Review, 54 49–66.
Messeri, P. A., Lee, G., Abramson, D. M., Aidala, A. A., Chiasson, M. A., and Jessop, D. J. (2003). Antiretroviral therapy and declining AIDS mortality. Medical Care, 41 512–521.
Resnick, M. D., Bearman, P. S., Blum, R. W., Bauman, K. E., Harris, K. M., Jones, J., Tabor, J., Beuhring, T., Sieving, R. E., Shrew, M., Ireland, M., Bearinger, L. H., and Udry, J. R. (1997). Protecting adolescents from harm: Findings from the National Longitudinal Study of Adolescent Health. Journal of the American Medical Association, 278 823– 832.
Steward, A. L., Hayes, R. D., and Ware, J. E. (1991). The MOS short-form general health survey: Reliability and validity in a patient population. Medical Care, 26 724–730.
Turner, R. J., and Turner, J. B. (1999). Social integration and support. In C. S. Aneshensel, and J. C. Phelan (Eds.), Handbook of the Sociology of Mental Health. New York: Kluwer Academic/Plenum Publishers.
Valdiserri, R. O. (2002). HIV/AIDS stigma: An impediment to public health. American Journal of Public Health, 92 341–342.
Wasserman, S., and Faust, K. (1994). Social Network Analysis Methods and Applications. Cambridge, NY: Cambridge University Press.
Wright, E. R., and Fife, B. L. (1999). Social support and the stigma of HIV/AIDS and cancer. Presented at the Annual Meeting of the American Sociological Association Annual Meetings, August 6–10, 1999, Chicago, IL.
ACKNOWLEDGMENTS
This research was supported by grant number H89 HA 0015-12 from the U.S. Health Resources and Services Administration (HRSA) HIV/AIDS Bureau with the support of the HIV Health and Human Services Planning Council, through the New York City Department of Health and Mental Hygiene and the Medical and Health Research Association of New York City, Inc. (MHRA). While working on this project, the first author was supported as a postdoctoral fellow in the Behavioral Sciences Training in Drug Abuse Research Program sponsored by Medical and Health Association of New York City, Inc. and the National Development and Research Institutes (NDRI) with funding from the National Institute on Drug Abuse (5T32 DA07233). Points of view, opinions, and conclusions in this paper do not necessarily represent the official position of the U.S. Government, Medical and Health Association of New York City, National Development and Research Institutes, or the New York City Department of Health and Mental Hygiene.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Waddell, E.N., Messeri, P.A. Social Support, Disclosure, and Use of Antiretroviral Therapy. AIDS Behav 10, 263–272 (2006). https://doi.org/10.1007/s10461-005-9042-x
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10461-005-9042-x