Abstract
The objective of this study is to determinate the factors that mediate in the self-reported consistent condom use over the 24-months post-intervention period in adolescents who received COMPAS, a sexual health promotion intervention targeted to Spanish adolescents. Twelve high schools located in Spain were randomized to an intervention or a control group with baseline, immediate-post, 12 and 24-month post-intervention assessments. Self-reported consistent condom use by 24 months post-intervention was the primary outcome. Based on the theory of planned behavior, we identified which theory-based variables mediated the intervention’s effect on consistent condom use. Serial multiple mediation analysis indicated that attitudes toward condom use, when there are obstacles to use it, and self-efficacy mediated the COMPAS’s effect in increasing consistent condom use. This is the first study that identifies the theoretical constructs that mediate the efficacy of a school-based intervention to promote sexual health in adolescents from Spain.
Resumen
El objetivo de este estudio es determinar los factores que median el uso consistente del preservativo en los adolescentes tras 24 meses de haber recibido COMPAS, una intervención para promover una sexualidad saludable dirigida a los adolescentes españoles. Fueron seleccionados 12 centros educativos de España, donde se realizó una evaluación en la línea base, post-implementación, a los 12 y 24 meses de seguimiento. El uso consistente del preservativo fue la conducta final evaluada mediante autoinforme a los 24 meses de la implementación. Basado en la teoría de la conducta planeada, se identificaron las variables que median el efecto de la intervención sobre el uso consistente del preservativo. El análisis de mediación múltiple indica que las actitudes hacia el uso del preservativo cuando hay obstáculos para su uso y la autoeficacia mediaron el efecto del programa COMPAS en el incremento del uso consistente del preservativo. Éste es el primer estudio que identifica los constructos teóricos que median la eficacia de una intervención de promoción de hábitos sexuales saludables en adolescentes españoles.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
In Spain, the main route of HIV transmissions are unprotected sexual relations, and young individuals between 15 and 24 years of age represent 11.2 % of recorded cases there [1]. During the last decade, the number of STI diagnoses under epidemiological surveillance has increased [2]. In 2013, the highest infection rate in women between 15 and 24 was for chlamydia trachomatis and herpes simplex virus 1. Neisseria gonorrhoeae rate is highest in men 25–34 years old, followed by the group between 15 and 24 years old [3]. It is estimated that between 80 and 95 % of Spanish adolescents use condoms during their sexual relations; however, they do not use them consistently [4–6]. One recent study indicates that only 37 % of Spanish adolescent use condoms every time they engage in sexual relations [7]. Because of this, and despite advances in sexual education, implementing effective prevention programs whose objective is to promote healthy sexual habits, among them consistent condom use, remains necessary.
The COMPAS program (Spanish name: Competencias para adolescentes con una sexualidad saludable) is a school-based intervention directed at developing skills for preventing the transmission of HIV/AIDS, other STIs, and unplanned pregnancies. It has shown to be effective in promoting healthy sexuality in several controlled studies. In a first controlled study, COMPAS showed to be effective in increasing the level of knowledge about HIV and the intention to use condoms, and it improved the attitude towards HIV and protection methods in 832 adolescents from 15 schools [8]. Another study concluded that the program’s effectiveness was greater when it was applied by experts in sexual health promotion in comparison to trained peer applicators [9]. COMPAS was recently confirmed to be at least as effective 12 months after its application as an evidence-based intervention [10].
The effectiveness of prevention programs is usually evaluated by the impact on mediating variables that predict the final behavior [7, 11]. The theory of planned behavior (TPB) [12], one of the most used to predict health behavior, shows the presence of relationships between intermediate variables and the expected final behavior. In accordance with the TPB, the final behavior is predicted by the intention, whose predictors are perceived norms, the perceived behavior control—equivalent to the concept of self-efficacy proposed by Bandura [13]—and the attitude.
Mediation analyses provide valuable information for learning which variables addressed in the program have greater influence on the expected behavioral change, i.e., which elements are responsible for the success or failure of the interventions; this way, the interventions can adapt and become more effective following their implementation. On the one hand, they provide data on the effects of the intervention on the potential mediators, and the influence of these on the expected final behavior; and on the other, about the indirect effect of the intervention on the behavior by the potential mediators [14, 15]. This perspective permits rigorously assessing the effectiveness of the prevention programs and tests the fit of the data with the theoretical models underlying the intervention [16]. Despite the importance of identifying the mediators of the effectiveness of the interventions, the factors underlying the effectiveness of the COMPAS program in promoting consistent condom use have yet to be learned. The mediation analysis would permit identifying the outcomes that mediate the effect between the intervention and the final result, as well as those that do not play a relevant role in achieving the objectives.
This work’s objective was to examine the effect of variables based on the TPB [12] to increase consistent condom use 24 months after the application of a sexual health promotion intervention in adolescents. In accordance with this model, the attitude, perceived norm, and self-efficacy are precursors of the intention, and in turn, the intention is the best predictor of behavior [17]. Based on the structural model of the TPB, we hypothesize that the intention to use condoms will mediate the effect of other theoretical constructs on self-reported consistent condom use. The results of this study will permit identifying the variables—based on the theory and worked in the intervention—that mediate their effectiveness to increase consistent condom use with respect to a control group.
Methods
Participants
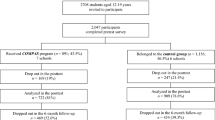
On the baseline, the sample comprised 1121 adolescents aged 14–16 (50.7 % girls; average age = 14.76, SD = 0.75). As reported elsewhere [7], the participants were 9th and 10th grade high school students at the beginning of the study. They participated in the trial over a 25-month period that began in January 2012. Of them, 78.1 % reported that their parents were married. Regarding socioeconomic status, 33.4 % belong to a low SES, 58.4 % to a middle SES, and 8.2 % to a high SES. Just over half, 50.5 % (n = 566) of the adolescents are sexually active when considering sexual practices that include vaginal penetration, anal sex, and/or oral sex. Most identified themselves as heterosexual (95.5 %), and there were no differences for this variable between the control and intervention groups (χ 2 = 3.74; p = 0.61) (Table 1).
Participants were recruited from 12 high schools located in the north, east, and south of Spain. Six of the schools were randomly assigned to the COMPAS group (n = 622) with the remaining to the control without intervention condition (n = 499). On the baseline, the groups were equivalent in the variables analyzed except for age (COMPAS = 14.70; SD = 0.71 vs. control group = 14.84; SD = 0.78) (F = 3.55; p < 0.05) and the percentage reporting to be sexually active (COMPAS = 45 % vs. control group = 57.3 %) (F = 16.75; p < 0.001) (Table 1). These differences on the baseline were controlled in all analyses.
Measures
The participants were evaluated before implementing the intervention, immediately afterwards, and the effects were monitored at 12 and 24 months. The primary outcome was self-reported consistent condom use at the 24-month follow-up. The potential mediators (M1)—precursors of the intention in accordance with the TPB [12]—were evaluated in the post-test, and the intention of using condoms (M2) was evaluated during the 12-month follow-up.
All provided sociodemographic information including age, sex, sexual orientation (heterosexual, homosexual, and bisexual), and reported about their sexual experience—vaginal penetration, anal sex and/or oral sex, family structure, and socioeconomic status. The Family Affluence Scale (FAS) [18] was used, which evaluates a family’s economic wellbeing with four items: the number of cars and computers a family possesses, possession of a bedroom by oneself, and the number of family vacation periods taken during the preceding 12 months. Good criteria validity is observed with respect to actual economic indicators such as gross national product (r = 0.87).
Knowledge about HIV and STIs was assessed using the Scale of Knowledge about HIV and other STIs (ECI, its Spanish acronym for the Escala de Conocimiento sobre HIV y otras ITS) [19]. This consists of 24 items distributed in five factors: general knowledge about HIV, knowledge about condoms, knowledge about the transmission routes of STIs, knowledge about prevention, and knowledge about other STIs. There is also a general scale of knowledge about HIV and other STIs. True, False, and I do not know are the response options for each statement. Item examples include “When a boy/girl has gonorrhea, treating their partner is unnecessary” and “HIV is transmitted by vaginal and seminal secretions, and blood.” In this sample, the questionnaire showed good internal consistency (α = 0.84).
Attitude towards condom use was rated from 1 (Strongly disagree) to 5 (Strongly agree), evaluated with the 3-item Attitude towards condom use subscale from the 12-item HIV Attitudes Scale for Adolescents [20]. One item example is, “If I were to have sexual relations and I realized that neither of us possesses any condoms, I would wait to acquire some before maintaining sexual contact.” The subscale reliability with the sample from this study was adequate (α = 0.76).
Perceived norm was evaluated with the item, “How frequently do you believe that your peers use condoms in their sexual relations,” with a Likert-type response scale of 1 meaning Never and 4 meaning Always.
Self-efficacy was evaluated with the General Self-Efficacy Scale with Spanish adolescents [21]. It is comprised of 10 items with a 10-point Likert response scale ranging from 1 (Totally disagree) to 10 (Totally agree). The instrument explains 51.88 % of the explained variance and possesses high internal consistency with this sample (α = 0.90).
Sexual risk perception was evaluated with a 3-item scale and a 4-point Likert response scale of 1 meaning No risk and 4 meaning Very risky. The participants had to indicate how risky they thought vaginal sex without a condom was for having an unwanted pregnancy, in addition to contracting HIV or other STIs (non-HIV). The internal consistency of this scale in this study was good (α = 0.88).
Intention towards condom use was evaluated with the item, “I will use a condom during the upcoming 12 months if I have sexual relations,” included in the intention to acquire, use, and negotiate condom use with a sexual partner (α = 0.80) factor from the 5-item Scale of intention to engage in safer sexual behavior in the next 12 months. This used a 5-point Likert response scale with 1 = Definitely not and 5 = Certainly. Previous studies attest to the good psychometric properties of this scale [7, 10].
Consistent condom use was calculated from responses to the item, “What percentage of the time do you use a condom in your sexual relations?” with a continuous response scale between 0 (Never) and 100 (Always). Those who indicated using a condom 100 % of the time were categorized in the group that consistently used condoms while the rest were included in the group that did not use condoms consistently. Only those participants who reported to be sexually active responded to this question.
Intervention
COMPAS is a school intervention promoting sexual health and HIV prevention based on the Social Learning Theory [22] and the Information-Motivation-Behavioral Skills model (IMB) [23]. These theoretical models strive to learn the predicting factors of sexual behavior, highlighting social influence, the level of information, attitudes and beliefs, and behavioral intention as precursors. The program’s objectives are to increase the level of knowledge and attitudes related to HIV/AIDS, as well as reduce risky sexual behavior. The main components of COMPAS are transmission of information, social skills training, problem-solving training, and strategies to maintain safer sexual behavior.
The intervention consists of five 50-min sessions during school hours that address the following contents, respectively: (1) AIDS and Health: introduction to HIV/AIDS, transmission routes, sexual risk vulnerability, and training on identifying HIV risk behavior; (2) Knowing AIDS better: works on knowledge about prevention methods and demystification of erroneous beliefs about sexuality established in adolescents; (3) Making decisions: Decision making on condom use and in the affective sexual area through assessment of situations where there are obstacles for acquiring condoms; (4) Improving your communication about sex: includes dynamics for training on assertiveness and communication skills for negotiating condom use and refusing unprotected sex; and (5) Maintaining your decisions: includes training on correct condom use, self-instructions, and covert behavior rehearsal. These contents are presented in mixed groups of approximately 15–20 participants via participatory activities, group games, role-playing, and group discussions, encouraging the involvement of each of the adolescents.
Procedure
Authorization was obtained by the ethics committee of the institution responsible for the study. Participating in it were 12 of the 15 schools invited from five Spanish provinces: Alicante, Oviedo, Castellón, Granada, and Murcia, of which six schools had been randomly assigned the COMPAS condition (n = 622) and the other six to the control/without intervention group (n = 499). The main reason why these 3 schools refused to participate in the study was the incompatibility with other scholar activities. In general, the schools reported high satisfaction and sensitivity with the program because they perceived the need to promote healthy sexual behaviors among adolescents. All of the schools met the criteria of not having applied any sexual health promotion interventions in the year prior, and furthermore, they committed to not hold any during the duration of the project. The participants were assessed before the intervention, immediately after (in 2012), and again after 12 (in 2013) and 24 months (2014).
The application of the intervention, as well as the administration of the questionnaires, was conducted in groups during school hours and this explains the high rate of participation (97 %). There were 5 facilitators (one per province), 2 male and 3 female, (average age = 28.8, range 25–29), qualified university psychologists, with experience and specific training in applying prevention programs in the area of sexuality. Each facilitator received 6 h of training on the COMPAS program to ensure high fidelity in its implementation. A video was shown to them on the application of each of the sessions to a group of adolescents, and online tutorials were scheduled to resolve doubts that arose throughout the fieldwork.
Data Analysis
Statistical analyses were carried out using SPSS Statistics v 20.0. A descriptive analysis of the sociodemographic variables and outcomes was conducted first. ANOVA simple was used to compare the baseline of the quantitative dependent variables, and Chi square (χ2) for the qualitative variables between the control and experimental groups.
Mediation analyses were performed using the PROCESS v 2.12 macro for Windows [24]. The significant criterion was p ≤ 0.05, and 5000 samples were used for bias-corrected bootstrap confidence intervals. We conducted serial multiple mediator models using the procedures described by Hayes [24]. The generic model of serial multiple mediation with two mediators was used (Fig. 1). The predictor was a dummy variable contrasting the sexual health promotion intervention (COMPAS) with the control group. The primary outcome was a binary variable, self-reported consistent condom use at the 24-month follow-up. Analyses were controlled for age, being sexually active or not, and baseline measures.
Based on the TPB, we assigned Mediator 1 (M1) as changes in knowledge about HIV and STIs, attitudes towards condom use, attitudes towards condom use when barriers exist, sexual risk perception, self-efficacy, and perceived norms; Mediator 2 was assigned (M2) as a change in the intention to use condoms. Three indirect effects are estimated in serial multiple mediation models as products of regression weight linking X to Y through M1 (Ind 1), M2 (Ind 3), and M1 and M2 (Ind 2) [24]. According to previous studies evaluating HIV risk-reduction intervention [25], separate mediation analyses were conducted for each potential mediator using a product-of-coefficient approach [26]. Path α demonstrates the effect of the intervention on the potential mediators (M1); path β shows the effect of the potential mediators (M1) on the intention to use condoms mediator (M2); path c evaluates the effect of the intention to use condoms (M2) on the outcome (Y), consistent condom use. The mediation was determined by testing whether the indirect effects are statistically different from zero.
Results
Mediation
Table 2 shows the averages and standard deviations of the outcomes in each evaluation: baseline, post, 12-month follow-up, and 24-month follow-up in the intervention and control groups. As Table 3 shows, the intervention had a significant impact on 4 of the 6 outcomes: knowledge about HIV and other STIs (ACI = 0.23, 1.28; p < 0.005), attitude towards condom use (ACI = 0.19, 1.10; p < 0.05), attitude towards condom use when barriers exist for their use (ACI = 0.09, 0.90; p < 0.05), and self-efficacy (ACI = 1.26, 6.85; p < 0.005). However, the intervention did not have a significant impact on the perceived norm (ACI = −0.28, 0.02; p = 0.11) or the perception of risk (ACI = −0.11, 0.60; p = 0.19).
Path β shows the existing relationship between the outcomes and the intention to use condoms. The results show that four of the six outcomes had a significant statistical impact on the intention to use condoms: attitude towards condom use when barriers exist for their use (ACI = 0.001, 0.07; p < 0.05), perception of risk (ACI = 0.003, 0.08; p < 0.05), self-efficacy (ACI = 0.00, 0.01; p < 0.05), and perceived norm (ACI = −0.23, −0.05; p < 0.005). In all the models analyzed, path c shows that the intention to use condoms at 12 months was related to consistent condom use at 24 months.
The intervention did not have an indirect impact on consistent condom use through the level of knowledge (Ind 1 = −0.002; ACI = −0.07, 0.05), attitude towards condom use (Ind 1 = 0.03; ACI = −0.01, 0.14), attitude towards condom use when barriers exist for their use (Ind 1 = 0.04; ACI = −0.008, 0.15), perception of risk (Ind 1 = −0.01; ACI = −0.08, 0.01), self-efficacy (Ind 1 = −0.004; ACI = −0.08, 0.07), or perceived norm (Ind 1 = −0.001; ACI = −0.05, 0.03).
The intervention positively affected consistent condom use indirectly through the attitude towards condom use when barriers exist (M1) in serial with the intention to use condoms (M2) (Ind 2 = 0.03; ACI = 0.002, 0.12). Additionally, the intervention had a significant impact on consistent condom use indirectly through self-efficacy (M1) in serial with the intention to use condoms (M2) (Ind 2 = 0.03; ACI = 0.002, 0.12).
Indirect effects through the intention to use condoms mediator were significant in four of the six models analyzed: attitude towards condom use (Ind 3 = −0.27; ACI = −0.69, −0.01), attitude towards condom use when barriers exist (Ind 3 = −0.30; ACI = −0.71, −0.04), self-efficacy (Ind 3 = −0.28; ACI = −0.70, −0.008), and perceived norm (Ind 3 = −0.26; ACI = −0.69, −0.01). For the models that included the variables of knowledge about HIV and other STIs (M1) and perception of risk (M1), no indirect effect of the intervention on consistent condom use through the intention of condom use (M2) was observed, (Ind 3 = −0.25; ACI = −0.68, 0.02) and (Ind 3 = −0.26; ACI = −0.68, 0.02), respectively.
It is noteworthy that even though the intervention had no impact on the perceived norm or the perception of risk, path β shows that the adolescents who perceive that their peers use condoms more frequently in their sexual relations and/or those who perceive that unprotected sex involves a greater risk for contracting HIV/STIs or unwanted pregnancies had firmer intentions to use condoms during sex, which was related with the self-reported consistent condom use (ACI = 1.04, 2.33; p < 0.005) (ACI = 1.06, 2.36; p < 0.001), respectively. In contrast, the intervention increased the level of knowledge about HIV and other STIs. However, possession of greater levels of knowledge about HIV and other STIs was not related with the intention of using condoms (path β) (ACI = −0.01, 0.04; p = 0.29) or with consistent condom use (Ind 2 = 0.01; ACI = −0.01, 0.08).
Discussion
The present study confirms the positive changes produced by COMPAS in the short term for increasing the level of knowledge about HIV and other STIs, the attitude towards condom use along with when barriers exist for their use, and self-efficacy. These results are consistent with previous studies evaluating the short-term effectiveness of COMPAS [7, 8] and subsequent to 12 months after its application [10], except in the perception of sexual risk. Espada [4] found that COMPAS increases the perception of risk in its participants with respect to a control group. However, the effect size of this inter-group difference was small (d = 0.11) [27]. Other studies, such as that by Baumler [14], found inconsistencies between the evaluation study and the results from the mediation, and they justify them by the use of a different type of analysis.
In accordance with the TPB [12], the results show that the attitude towards condoms when difficulties exist for their use, the perceived norm of condom use by peers, and self-efficacy were precursors of the intention to use condoms, which stands out by being the variable with the greatest capacity to influence consistent condom use. Other variables, such as the level of knowledge of condom use and the attitude towards condoms, were not related with the intention to use this method of protection.
The perceived norm was the most influential variable on the intention, just as in other studies [28]; however, COMPAS did not have a significant short-term impact on this precursor. This unexpected result can be explained by several reasons. On the one hand, COMPAS was implemented by experts in sexual health promotion, rather than peers who can change the perception of peers’ condom use. On the other hand, participants’ close friends outside the school environment did not receive the intervention, so it would not be expected that participants’ close friends increase condom use after the intervention. Consequently, the participants’ perception of peers’ condom use remained over time [25]. The inclusion in the program of specific activities to modify perceived norms, such as group dynamics that encourage participants’ expressions and opinions about condom use, could contribute to improve the participants’ perception of peers’ condom use [29]. Unlike the TPB—which indicates that self-efficacy/perceived control may have a direct/indirect impact on the behavior—the variables analyzed were not directed related with consistent condom use after 24 months without mediating through the intention.
Mediation analyses show that self-efficacy and the attitude towards condoms when barriers exist mediate the relationship between the COMPAS program, the intention to use condoms, and consistent condom use 24 months after application of the program. A large number of studies that analyze the effect of the theoretical constructs as mediators of the effectiveness of sexual risk reduction interventions highlight self-efficacy as one of the main variables involved in the success of the intervention [25, 30–33]. These results are consistent with the TPB [12], which shows the perception of control—equivalent to the concept of self-efficacy by Bandura [22]—as a precursor of the intention and with a direct effect on the final behavior. In one recent study, the perceived control shows to be the best predictor of the intention to use condoms (effect coefficient = 0.36; p < 0.01) [34]. In this study, the attitude towards condom use when there obstacles to use and self-efficacy were the variables with the greatest indirect effect on consistent condom use through intention. However, the results suggest that the impact of the intervention on the intention would be sufficient to produce a change in behavior.
The suitability of the activities that promote the intention to use condoms, self-efficacy, and the attitude to promote condom use is confirmed, especially when barriers exist for their use (for example, having a sexual partner who refuses to use condoms, the unavailability of condoms at the time of the sexual activity, etc.). However, we recommend reviewing the content of COMPAS in order to strengthen the components of perceived norm and perception of risk due to their contribution to increasing the intention of using condoms. Mackinnon [15] recommends assessing the variables more precisely in order to identify the real changes resulting from the intervention. Studies like that of Jemmott [29] point to the importance of the perceived norm to produce a change in behavior; this is despite the intervention that they test not having a significant effect on this variable, just like our results show. Jemmott proposes including close friends of the participants in the study to achieve a significant change in the perceived norm.
No indirect effect was observed between the level of knowledge about HIV and other STIs on condom use, nor through the intention towards using condoms. This explains the ineffectiveness of programs whose objectives are directed exclusively at increasing the level of information in the sexual field [35]. These results suggest that knowledge is not sufficient for producing a long-term behavioral change [36].
This study has important implications for the promotion of sexual health in adolescents. Its results permit identifying the mechanisms involved in the effectiveness of COMPAS for increasing consistent condom use 24 months subsequent to its application. In Spain, COMPAS is the only school intervention promoting sexual health whose effectiveness has been proven in different controlled studies with samples from different geographical areas [8, 9], and its effects have been evaluated at 12 [10] and 24 months [Espada et al., unpublished]. To our knowledge, this is the first study to identify the indirect effects of a school intervention—directed at Spanish adolescents—to promote consistent condom use from the theoretical approach of the TPB.
The present study has some limitations. The intervention’s effect was basically assessed with a self-report. Using biological measures, such as the serostatus for HIV, syphilis, or gonorrhea might have strengthened confidence in the results. Although the study involved a large sample from a varied geographical origin with the experimental conditions assigned randomly, the participating schools were not recruited by representative sampling, so generalizations must be made with caution. Another limitation is that mediation analyses imply correlation; experimental studies with manipulation of the variables under study would be necessary to be able to conclude causality [15].
It is concluded that the attitude adolescents hold about condom use when barriers exists for using them, self-efficacy, and the intention to use condoms are key elements in the effectiveness of the COMPAS program for increasing the consistency in using condoms in Spanish adolescents. The intention to use condoms is the most relevant variable, since it by itself mediates the effect of the intervention on consistent condom use 24 months after the application of the intervention. Therefore, all efforts should be directed at strengthening activities that promote the intention of using condoms, as a positive impact on this variable is sufficient to demonstrate more long-term consistent condom use in Spanish adolescents.
References
Centro Nacional de Epidemiología. Vigilancia Epidemiológica del VIH/sida en España. Situación 30 Junio de 2014 [Epidemiological surveillance of HIV/AIDS in Spain. Situation 30 June 2014]. 2014. http://www.msssi.gob.es/ciudadanos/enfLesiones/enfTransmisibles/sida/vigilancia/InformeVIHSida_Junio2014.pdf. Accessed 16 Jan 2015.
Centro Nacional de Epidemiología. Vigilancia Epidemiológica de las infecciones de transmisión sexual, 1995-2010 [Epidemiological surveillance of STI´s, 1995-2010]. 2012. http://www.msssi.gob.es/ciudadanos/enfLesiones/enfTransmisibles/sida/vigilancia/VigilanciaITS1995_2010.pdf. Accessed 20 Feb 2015.
Centro Nacional de Epidemiología. Informe annual del Sistema de Información Microbiológica 2013 [Annual report 2013 information system microbiologica]. 2014. http://www.isciii.es/ISCIII/es/contenidos/fd-servicios-cientifico-tecnicos/fd-vigilancias-alertas/fd-sistema-informacion-microbiologica/Informe_anual_SIM_2013.pdf. Accessed 20 Feb 2015.
Espada JP, Escribano S, Orgilés M, Morales A, Guillén-Riquelme A. Sexual risk behaviors increasing among adolescents over time: comparison of two cohorts in Spain. AIDS Care. 2015;27(6):783–8.
Faílde JM, Lameiras M, Bimbela JL. Prácticas sexuales de chicos y chicas españoles de 14-24 años de edad [Sexual behavior in a Spanish simple aged 14 to 24 years old] Gac Sanit. 2008;22(6): 511–519. http://scielo.isciii.es/scielo.php?script=sci_arttext&pid=S0213-91112008000600002&lng=es. Accessed 10 Jan 2015.
Muñoz-Silva A, Sánchez-García M, Martins A, Nunes C. Gender differences in HIV-related sexual behavior among college students from Spain and Portugal. Span J Psychol. 2009;12(2):485–95.
Espada JP, Morales A, Orgilés M, Jemmott JB III, Jemmott LS. Short-term evaluation of a skill-development sexual education program for Spanish adolescents compared with a well-established program. J Adolesc Health. 2015;56(1):30–7.
Espada JP, Orgilés M, Morales A, Ballester R, Huedo-Medina TB. Effectiveness of a school HIV/AIDS prevention program for Spanish adolescents. AIDS Educ Prev. 2012;24(6):500–13.
Morales A, Espada JP, Orgilés M, Secades-Villa R, Remor E. The short-term impact of peers as co-facilitators of an HIV prevention programme for adolescents: a cluster randomised controlled trial. Eur J Contracept Reprod Health Care. 2014;19(5):379–91.
Morales A, Espada JP, Orgilés M. A 1-year follow-up evaluation of a sexual-health education program for Spanish adolescents compared with a well-established program [published online May 9 2015]. Eur J Public Health. 2015;. doi:10.1093/eurpub/ckv074.
Borawski EA, Tufts KA, Trapl ES, Hayman LL, Yoder LD, Lovegreen LD. Effectiveness of health education teachers and school nurses teaching sexually transmitted infections/human immunodeficiency virus prevention knowledge and skills in high school. J Sch Health. 2015;85(3):189–96. doi:10.1111/josh.12234.
Ajzen I. The theory of planned behavior. Organ Behav Hum Decis Process. 1991;50(2):179–211.
Fishbein M. A reasoned action approach to health promotion. Med Decis Making. 2008;28(6):834–44. doi:10.1177/0272989X08326092.
Baumler E, Glassman J, Tortolero S, et al. Examination of the relationship between psychosocial mediators and intervention effects in it’s your game: an effective HIV/STI/pregnancy prevention intervention for middle school students. AIDS Res Treat. 2012;2012:298494. doi:10.1155/2012/298494.
MacKinnon DP. Introduction to statistical mediation analysis. New York: Lawrence Erlbaum Associates; 2008.
Ato M, Vallejo G. The effects of third variables in psychological research. An Psicol. 2011;27(2):550–61. http://hdl.handle.net/10201/26561. Accessed 10 Jan 2015.
Fishbein M, Ajzen I. Predicting and changing behavior: the reasoned action approach. New York: Psicoholgy Press; 2010.
Boyce W, Torsheim T, Currie C, Zambon A. The family affluence scale as a measure of national wealth: validation of an adolescent self-report measure. Soc Indic Res. 2006;78(3):473–87.
Espada JP, Guillén-Riquelme A, Morales A, Orgilés M, Sierra JC. Validación de una escala para evaluar el conocimiento sobre el VIH y otras infecciones de transmisión sexual en población adolescente [Validation of a scale to assess knowledge about HIV and other sexually transmitted infections in adolescent population]. Aten Prim. 2014;46(10):558–64. doi:10.1016/j.aprim.2014.03.007.
Espada JP, Ballester R, Huedo-Medina TB, Secades-Villa R, Orgilés M, Martínez-Lorca M. Development of a new instrument to assess AIDS-related attitudes among Spanish youngsters. An Psicol. 2013;29(1):83–9. doi:10.6018/analesps.29.1.132301.
Espada JP, Gonzálvez MT, Orgilés M, Carballo JL, Piqueras JA. Validación de la Escala General de Autoeficacia con adolescentes españoles [Validation of the general self-efficacy scale with spanish adolescents]. Electronic J Res Educ Psychol. 2012;26:355–370. http://www.redalyc.org/articulo.oa?id=293123551018. Accessed 15 Feb 2015.
Bandura A. Social foundations of thought and action. Englewood Cliffs, NJ: Prentice-Hall; 1986.
Fisher JD, Fisher WA. Changing AIDS-risk behavior. Psychol Bull. 1992;111(3):455–74.
Hayes AF. Introduction to mediation, moderation, and conditional process analysis: a regression-based approach. New York, NY: Guilford Press; 2013.
Jemmott JB III, Jemmott LS, O’Leary A, Icard LD, Rutledge SE. On the efficacy and mediation of a one-on-one HIV risk-reduction intervention for african american men who have sex with men: a randomized controlled trial. AIDS Behav. 2014. doi:10.1007/s10461-014-0961-2.
Preacher KJ, Hayes AF. Asymptotic and resampling strategies for assessing and comparing indirect effects in multiple mediator models. Beh Res Methods. 2008;40(3):879–91.
Cohen J. Statistical power analysis for the behavioral science. Hillsdale: Lawrence Earbaum; 1998.
Couture M, Soto J, Akom E, Joseph G, Zunzunegui MV. Determinants of intention to use condoms among clients of female sex workers in Haiti. AIDS Care. 2010;22(2):253–62.
Jemmott JB III, Stephens A, O’Leary A, et al. Mediation of effects of a theory-based behavioral intervention on self-reported physical activity in South African men. Prev Med. 2015;72:1–7. doi:10.1016/j.ypmed.2014.12.022.
O’ Leary A, Jemmott LS, Jemmott JB III. Mediation analysis of an effective sexual risk-reduction intervention for women: the importance of self-efficacy. Health Psychol. 2008;27(2):180–4. doi:10.1037/0278-6133.27.2.
O’ Leary A, Jemmott JB III, Jemmott LS, et al. Moderation and mediation of an effective HIV risk-reduction intervention for South African adolescents. Ann Behav Med. 2012;44(2):181–91.
Schmiege SJ, Broaddus MR, Levin M, Bryan AD. Randomized trial of group interventions to reduce HIV/STD risk and change theoretical mediators among detained adolescents. J Consult Clin Psychol. 2009;77(1):38–50.
Snead MC, O’Leary AM, Mandel MG, et al. Relationship between social cognitive theory constructs and self-reported condom use: assessment of behaviour in a subgroup of the Safe in the City trial. BMJ Open. 2014;4(12):e006093. doi:10.1136/bmjopen-2014-0093.
Sacolo HN, Chung M-H, Chu H, et al. High risk sexual behaviors for HIV among the in-school youth in swaziland: a structural equation modeling approach. PLoS ONE. 2013;8(7):e67289. doi:10.1371/journal.pone.0067289.
Peters LW, Kok G, Ten Dam GTM, Buijs GJ, Paulussen TG. Effective elements of school health promotion across behavioral domains: a systematic review of reviews. BMC Public Health. 2009;9:182. doi:10.1186/1471-2458-9-182.
Romero LM, Galbraith JS, Wilson-Williams L, Gloppen KM. HIV prevention among African American Youth: how well have evidence-based interventions addressed key theoretical constructs? AIDS Behav. 2011;15(5):976–91.
Acknowledgments
This research was financed by the Fundación para la Investigación y la Prevención del Sida en España (Foundation for Research and Prevention of Aids in Spain) (FIPSE 360971/10) and by the Program VALi + d for Research Staff training of the Conselleria de Cultura, Educació, y Ciència de la Generalitat Valenciana (Council of Culture, Education, and Science of the Valencian Autonomous Government) (ACIF/2012/132). We thank professor Jimena Y. Ramírez-Marín for her statistical assistance and discussion.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Escribano, S., Espada, J.P., Morales, A. et al. Mediation Analysis of an Effective Sexual Health Promotion Intervention for Spanish Adolescents. AIDS Behav 19, 1850–1859 (2015). https://doi.org/10.1007/s10461-015-1163-2
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10461-015-1163-2
Keywords
- Consistent condom use
- Sexual health promotion intervention
- Adolescents
- Mediation analysis
- Theory of planned behavior