Abstract
Embolization has tremendously evolved in recent years and has expanded to treatment of a variety of pathologic processes. There has been emerging evidence that the level of arterial occlusion and the distribution of embolic particles may play an important role in the clinical outcome. This is a comprehensive literature review to identify variables that play important role in determination of level of occlusion of blood vessels and distribution of embolic particles. The literature searches between 1996 to 2020 through PubMed and Ovid-MEDLINE yielded over 1030 articles of which 30 studies providing details on the level of occlusion are reviewed here. We divided the playing factors into characteristics of the particles, solution/injection and vascular bed. Accordingly, particle size, type and aggregation, compressibility/deformability, and biodegradability are categorized as the factors involving particles’ behavioral nature. Infusion rate and concentration/dilution of the medium are related to the carrying solution. Hemodynamics and the arterial resistance are characteristics of the vascular bed that also play an important role in the distribution of embolic particles. Understanding and predicting the level of embolization is a complex multi-factor problem that requires more evidence, warranting further randomized controlled trials, and powered human and animal studies.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Interventional radiology employs image-guided techniques to perform minimally invasive procedures for diagnosis and treatment.5 Embolization has recently brought a leap in modern medicine as a minimally-invasive treatment.51 Vascular embolization is a minimally invasive catheter-based procedure in which an occlusive material is placed into a blood vessel to block the arterial lumen and blood flow.5,42,51 Before embolization, interventional radiologist puts an angiography catheter into the artery and performs selective diagnostic angiography to obtain an anatomic roadmap of the blood vessels, understands the flow dynamics of the artery, size of the arterial lumen, and plans for occluding the desired level of blood vessel depending on the clinical situation.5,51 The goal of the embolization may be used to stop blood flow in active bleeding (such as in patients with trauma or gastrointestinal bleeding), to block the blood flow to a tumor (such as hepatocellular carcinoma or liver metastatic colorectal cancer), or to decrease vascular flow in an area of hypertrophied tissue with abnormal vascularity (such as uterine fibroids, or benign prostatic hyperplasia, or knee osteoarthritis).5,17,42,51 The ideal embolic material should effectively and rapidly occlude blood vessel at certain point of the artery (proximal, or distal to the target tissue), without any non-target embolization of arteries surrounding the target tissue or blood vessel. Embolization can be permanent or temporary. The former is more common and is performed utilizing liquid agents (such as n-butyl-2-cyanoacrylate (NBCA) or ethylene vinyl alcohol copolymer (EVOH)), Sodium tetradecyl sulfate (STS) (in the form of foam when mixed with Co2 or air), mechanicals (coils and plugs), and particles (including spherical and non-spherical particles) that are the focus of this review.
The clinical application of particle embolization has surged in the past couple of decades, including uterine fibroid embolization, prostate artery embolization, embolization for sports medicine complaints, and drug eluting-particles for oncologic purposes among others.42
There are various particles available in the market with different shape, size, surface characteristics, loading capability, opacity, etc. An understanding of the characteristics of the particle and its expected behavior in a blood vessel is of paramount importance in order to ensure the desired clinical outcome. From an engineering standpoint, embolization is a multi-factor problem of particle distribution. A complex interaction of particle-flow dynamics depends on the particle properties, particle to vessel size ratio, particle volume fraction (in the injected solution) in addition to the local Reynolds, Womersley and Stokes numbers. However, at times, the role of physics in the turn of events is neglected both in the procedure implementation and the design of relevant biomedical devices.
Previously, spherical particles and non-spherical particles have been compared to identify the properties that determine the distribution of the particles and level of the target vessel occlusion.15,17,24 Polyvinyl alcohol (PVA) particles’ irregular shape, tendency to aggregate, and their wide granulometric size range has led to a lack of correlation between target vessel size and particle diameter, leading to more proximal large vessel occlusion, non-target embolization, or catheter clogging. These lead to unpredictable results and sometimes complications, such as non-target embolization and early recanalization of the previously occluded blood vessel. Calibrated microspheres offer better target and distal vessel occlusion, with regular surfaces and less aggregation. This allows for a more predictable and reliable behavior and therefore better clinical results. Certain microspheres such as trisacryl gelatin microspheres (TGMS, Embosphere; Biosphere Medical, Roissy, France) and PVA microspheres (PVAMSs, Contour SE, Boston scientific Corp. Fremont, CA, USA) have new properties such as having a hydrophilic and microporous structure. These confer a better compressibility and malleability allowing the particle to flow relatively freely within the vessel lumen, resulting in deeper penetration and more distal occlusion.
Levels of occlusion of particles also depends on a number of other intrinsic and extrinsic factors such as particle type and size, aggregation, compressibility, local flow dynamics, arterial resistance, and the type of the microcatheter tip. In the quest to develop an ideal embolic particle with a predictable distribution and level of embolization, it is necessary to understand how particles behave in the blood vessels and which of the particle properties reliably predict the level of the arterial occlusion. This is a comprehensive review of the available literature to evaluate this complex clinical issue and bring this gap to the attention of the physical and engineering communities. We also provide an organized framework to comprehend the intricate physical properties of particles which affect the distribution of the particles in the blood vessels and the level of the embolization, based on the current clinical practice and literature review.
Materials and Methods
Search Strategy and Data Sources
This systematic review was in-line with Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA).36 A systematic search was performed to collect current evidence on factors affecting arterial distribution of particles and levels of occlusion. Literature searches were performed in PubMed over a period of two decades (Jan 1996 to Dec 2020). The following keywords were used to search for relevant literature: “embolization” and “microspheres” and “polyvinyl alcohol” or “poly vinyl” (using filter “all fields”) and “embolization therapeutic/methods” (MeSH terms).
Eligibility Criteria and Study Selection
This review includes all randomized clinical trials (RCT), animal models, case reports, and in vitro studies discussing different properties of embolic particles. Additionally, review articles on this topic were studied and their results were included. Studies analyzing particle distribution, specificity in vessel occlusion and comparing different physical properties of embolic particles were included in this review. We excluded studies on radioembolization, chemoembolization, preclinical studies on cancer treatment using embolic particles, and studies on loaded particles. Any studies dealing with other type of embolic agents such as liquid agent, coil, plug, vascular occlusion device, and balloons were not considered here. Only articles in English were included in this review.
Data Extraction and Quality Assessment
A total of 1030 articles were screened. 977 non-relevant articles were excluded based on title and/or abstract. These articles did not discuss the properties of embolic particles, particle distribution in vascular bed, or level of occlusion. Articles discussing radioembolization, chemoembolization, preclinical cancer treatments and loadable particles were excluded. In addition, articles pertaining to embolic devices other than embolic particles were excluded. Duplicates were also removed. The details of the algorithm are described in the diagram shown in Fig. 1. From the 53 articles left, all were critically reviewed by 3 authors and similar inclusion/exclusion criteria were applied. Finally, 30 articles were deemed relevant for the review. Abstracts and full texts were then reviewed to extract details on the type of the study (RCT, comparative animal/human study, in vitro, literature review, etc), the number of subjects, the type of embolic particles and the outcome of embolization. In order to quantify the clinical significance of the reviewed studies, we used the levels developed by the Centre for Evidence Based Medicine (CEBM) for treatment. We assigned a level of evidence (LOE) score to all reviewed articles in the scale of 1 to 5, with 1 being the highest level of evidence.10
Results
General Review Information
We initially searched literature reviews, commentaries and comparative studies in order to collect information on the different studies available on particle characteristics affecting arterial distribution and occlusion. Studies by Sheth et al.,42 Golzarian and Weng et al.,20 Senturk et al.,41 and Wenxiao et al.25 helped greatly in this process as they summarized the main embolic particles used and the various intrinsic and extrinsic characteristics affecting their behavior. As addressed in the following, several characteristics were identified in these studies: particle size, particle type/aggregation, compressibility/deformability, infusion rate, concentration/dilution, and hemodynamics/arterial resistance, elastic recovery/viscous relaxation and particle density/constitution.
Study Composition and Description
We selected a total of 30 articles that specifically studied the topic of interest (RCT’s, in vitro, comparative animal or human models) including 4 articles that were found in bibliographies of primary sources. Articles were grouped into 6 categories following the characteristics discussed: particle size, type/aggregation, compressibility/deformability, infusion rate, concentration/dilution, particle biodegradability, flow dynamics/arterial resistance. Seven studies were reported discussing the effect of the size on arterial distribution and occlusion of particles, including 4 animal models; Bilbao et al. (swine kidney, n = 18),8 Pelage et al. (sheep uterine and renal artery, n = 26),40 Stampfl et al. (porcine kidney, n = 9),45 Kishimoto et al. (dog superior mesenteric artery, n = 10)28 and 3 comparative human studies; including Laurent et al., Beaujeux et al. (n = 49 and 105 patients, respectively)6,29 as well as Bendszus et al. (n = 60, meningioma embolization with PVA vs. TGMS).7 All 4 animal models compared different types of microspheres (different in type and/or size), while the human models studied for the most part, trisacryl gelatin microspheres and only one comparative TGMS vs. two different sizes of PVA. All of these studies were given a level of evidence score of 2B.
For the effect of the particle aggregation on distribution and arterial occlusion, we included a total of 9 articles including 1 commentary by Golzarian and Weng et al.,20 1 comparative human model by Chua et al. (n = 17),15 and finally 7 animal models as follows; Choe et al. (rabbit renal artery, n = 14),14 Derdeyn et al. (Swine rete mirabile, n = 7),18 Siskin et al. (miniature pigs renal artery, n = 11),43 Bilbao et al. (swine kidney, n = 18),8 Andrews and Binkert et al. (swine renal artery, n = 20),2 Pelage et al. (sheep uterine and renal artery, n = 26),40 Laurent et al. (sheep uterine artery, n = 10).30 Seven of the 9 studies compared microspheres (TGMS) with non-microspherical particles (PVA) and included 5 animal models, 1 human comparative study and 1 literature review. The two remaining articles were studies on specifically PVA particles and 4 types of microspheres. The level of evidence of all the study models was attributed a score of 2B, except for the literature review which was scored 4.
Seven studies were found discussing the impact of compressibility and deformability on the arterial distribution. Two studies, Lewis et al. comparing 4 types of microspheres,32 Peixoto et al. comparing microspheres with non-microspheres,39 were found and attributed an LOE score of 5. One Double-blinded randomized controlled trial (LOE = 1) on uterine artery embolization (Yu et al., n = 56) compared two types of microspheres (TGMS and PVAMSs).52 The remaining four were animal models; Verret et al. (sheep uterine and renal artery, n = 12) studying two types of microspheres,47 Bilbao et al., Pelage et al. (swine kidney, n = 18 and sheep uterine artery, n = 26, respectively) comparing microspheres with non-spherical particles8,40 and Laurent et al. (sheep uterine artery, n = 6) comparing TGMS and PVMS.31 In terms of the level of evidence, they were given a score of 2B.
One article (Choe et al., rabbit kidney, n = 14) focused on two categories; infusion rate and concentration and dilution of PVA non-spherical particles. It was attributed to a level of evidence of 2B.14 Similarly, only one article by Patel et al. (rabbit renal artery, n = 2) was found discussing the effect of flow dynamics and arterial resistance on the arterial distribution and occlusion of particles.38 An in vitro study by Hidaka et al. was the only available model to investigate the elastic recovery and viscous relaxation of three types of microspheres. It was attributed to a level of evidence of 5.21
Bioresorbable particles were specifically studied in two animal models and one in vitro study. Weng et al. and Keussen et al. compared bioresorbable microspheres with TGMS in a rabbit kidney model (n = 10) and sheep uterine artery embolization (n = 22), respectively.27,49 The effect of the biodegradable material in the microspheres embolization performance was investigated in vitro by Sommer et al.44
Experimental studies on the hemodynamics of the embolization process are also rare. The transport and distribution of embolic particles in vessels is a function of the particle’s size, material, mechanical properties, concentration, the infusion rate and pressure, catheter tip, vessel anatomy, distal pressure and arterial flow distribution. In vitro studies by Bushi et al. and Caine et al. explored the particle distribution under different conditions in in vitro models of an idealized bifurcation and in a hepatic arterial system, respectively.11,12
Discussion
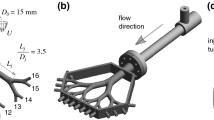
As described earlier, particles remain a primary embolic staple in the field of interventional radiology. Depending on the clinical indication of a procedure, interventional radiologists should be equipped with the knowledge of the distribution properties of the particles and factors that could affect the level of arterial embolization, to choose a correct type and size of particle for an embolization procedure. Need-driven progress has been made in embolic agents in order to address deficiencies of the existing products. While several features of particle embolic require consideration, features that are subject of more clinical interest recently are particle size, type and aggregation, compressibility/deformability, carrying solution, biodegradability, and hemodynamics (Fig. 2). In this review, we evaluated the existing evidence regarding these factors and their effect on arterial distribution of embolic particles and level of embolization.
Particle Size
Choosing a particle size is of utmost clinical significance. Depending on the goal of the embolization, a certain level of the artery (with a certain diameter) needs to be occluded. For example, if the goal of the embolization is necrosis of the tumor or devascularization of hypertrophied tissue (i.e., hepatocellular carcinoma, uterine leiomyoma (uterine fibroids), or prostatic hyperplasia),34,35,37 the particle size needs to be small so that a more distal level of the artery be blocked. On the other hand, if there is concern regarding non-target passage of the embolic beads into venous circulation (like, in arteriovenous malformations or arteriovenous fistulae) or if accidental passage of embolic material into smaller size arteries could have a devastating consequence (for example, accidental passage of embolic particles smaller than 200 micro meters may occlude spinal artery and cause permanent spinal infarction and paralysis, in patients who have bronchial artery embolization9), then larger size particles should be utilized for embolization. In addition, an irregular particle size distribution makes the level of embolization difficult to control; i.e. a significant number of small particles would penetrate further into the vascular bed than desirable and other larger particles would form aggregates that cause a more proximal embolization than desirable.
Several comparative animal model studies have compared the effect of the microspheres size in the arterial distribution7,8,28,29,40,45 all pointing to the same conclusion; microspherical particles size is well correlated with the embolized vessel diameter. Thus, microspheres with smaller sizes occlude more distal vessels. Animal studies were limited because they were mainly healthy non-tumorous models and cannot be transposed to a clinical context. Another limitation is that statistical analysis for too-deep penetration compares different embolic materials, although different particle amounts were injected. It is difficult to quantify the amount of particles for each embolic agent that was injected during the procedure. Laurent et al.’s study offers a pathological context in a retrospective comparative study with 49 patients (suffering from nasopharyngeal angiofibromas and paragangliomas) further supporting the animal model findings.29 Similar results were inferred from Beaujeux et al., where calibrated trisacryl gelatin microspheres of different diameters were used for superselective embolization of 105 patients who had tumors or facial, spinal cord, or cerebral arteriovenous malformations (AVMs), which allowed a larger scale study of this phenomenon.6 Unfortunately, no RCT studies were found concerning the effect of the size in particle distribution. A summary of studies considering the size is given in Table 1. A recent publication on prostate artery embolization (PAE) reported that the clinical outcomes were not significantly affected by the particle size.46 However, there was an increased risk of adverse events with the use of smaller particles.
Particle Type and Aggregation
Aggregation of the particles commonly leads to bigger particle conglomerates which results in more proximal obstruction of arteries (than intended). More proximal obstruction could cause more tissue infarction but less effective ischemia of the target treatment region and eventually less tissue necrosis.33 This feature can be used and the level of embolization can be geared towards the desired clinical outcome that is intended. In order to achieve tumor necrosis, if ischemia to an organ is intended at the cellular level, then distal embolization is favorable and uniformly small particles are needed to achieve tissue necrosis. On the other hand, if no necrosis is intended more proximal level of embolization with larger particles and more heterogeneity in size will be utilized to occlude the blood vessel more proximally.
In terms of particle type and aggregation, six animal model studies have analyzed mainly PVA particles and calibrated microspheres. The study by Bilbao et al. compared 4 different microspheres.8 As mentioned above, the animal models may not necessarily reflect the real-world clinical situation as most embolized organs were healthy. A second limitation was the restricted number of subjects (between 10 and 14) which may diminish power of these studies. A human comparative study performed by Chua et al. with 17 patients who had uterine artery embolization (UAE) before myomectomy, is one of the only available studies performed in a pathological context on humans.15 They concluded that the use of microspheres is advantageous over non-spherical PVA particles since the former penetrate considerably deeper into leiomyomata in comparison with the latter, allowing a better target embolization. The major weakness of this study is the limited number of cases. Golzarian and Weng et al. provided an overview of the embolic agents and concluded that particle may aggregate in the catheter or in the vessels resulting in the proximal embolization of the vessels.20 No larger studies and RCTs have confirmed these conclusions. Additional studies examining the relationship between particle type/ aggregation and the level of embolization are provided in Table 2.
Particle Compressibility/Deformability
Particles which are more compressible tend to deform more easily during embolization and this translates to a more distal embolization.19 This is a physical characteristic which could be favorable in clinical situations when distal embolization is intended such as in prostate artery embolization, uterine artery embolization, or embolization in treatment of hepatocellular carcinoma.
Studies on particle compressibility and deformability are more common and diverse. They include four animal models comparing microspherical with non-microspherical particles31,40,47 and a comparison of 4 different types of microspheres,8 two in vitro studies,32,39 and one double blinded RCT with 56 patients.52 All concluded that higher deformability leads to more distal occlusion. Despite the high level of evidence of a double blinded RCT study, this particular one has certain limitations. There were a relatively small number of patients in each arms, with 27 patients in the trisacryl microsphere group and 29 in the PVA microsphere group. Secondly, using a power Doppler ultrasound for the assessment of residual perfusion for the purpose of comparison of treatment effectiveness between the two embolic agents, is not sufficiently sensitive as would have been using magnetic resonance imaging (which is the standard for such assessments). The in vitro study by Hidaka et al. showed that acrylamido polyvinyl alcohol (APVA) microspheres have a lower rigidity but a comparable viscous relaxation to TGMS.21 They conjectured that APVA microspheres deform less than softer microspheres and hence will locate more proximally than PVA microspheres. In continuum mechanics, stress relaxation or viscous relaxation refers to the stress reduction for a given applied strain. It is a behavior of viscoelastic material that exhibits both viscous and elastic characteristics under deformation. It represents how a viscoelastic material relieves stress under constant strain over time. Embolic beads that have viscoelasticity properties will show such a behavior when deformed in vessels or microcatheters that typically have smaller sizes than the embolic particles.21 A summary of studies considering the particle compressibility and deformability is given in Table 3.
Particle Carrying Solution
Despite being a well-known phenomenon amongst practicing interventional radiologists, very little evidence is available concerning the effect of the infusion rate, concentration/dilution (both from the same study conducted by Choe et al.14) to be able to confidently state the effects of these factors on particle distribution. One animal model comparative study was performed for each category leaving space for many possibilities of larger scale and pertinent studies. In essence, with a lower infusion rate and higher dilution, a more distal dislodgement of embolic particles could be anticipated. A summary of the study examining concentration/dilution/infusion rate is provided in Table 4. It is of utmost clinical importance to be aware that the slower rate of administration of the embolic particle will lead to a more distal arterial level embolization.14,48 This is a physical characteristic which could be favorable in clinical situations when distal embolization is intended such as bariatric arterial embolization, prostate artery embolization, uterine artery embolization, or embolization in treatment of hepatocellular carcinoma.
Particle Biodegradability
In several clinical situations, practitioners prefer to use a bioabsorbable particle to avoid permanent occlusion of the blood vessels.23,50 Concerning the effect of bioresorbable/biodegradable particles, Weng et al. (animal model) and Sommer et al. (in vitro) compared bioresorbable microspheres with TGMS and Embospheres, respectively.44,49 Both concluded that bioresorbable agents occlude more proximally than TGMS and permanent microspheres. From a density point of view, Weng et al. explain that a higher cross-linking density results in a higher rigidity of the microspheres and therefore occlude slightly more proximally.49 Sommer et al. .showed that the biodegradable microspheres in comparison with established permanent microspheres lead to less distal occlusion immediately one week after embolization.44 However, they would cause less post-procedure complications. Keussen et al. investigated the use of biodegradable microspheres in comparison with trisacryl gelatin particles and concluded that the former led to significantly more recanalization after embolization.27 Table 5 concludes the studies evaluating the effect of bioresorbability on particle distribution.
Hemodynamics
Finally, despite the importance of understanding the hemodynamics governing the distribution of embolic particles in target embolization, very few relevant clinical studies are available. In the animal study by Patel et al., it was shown that lower resistance vascular beds preferentially receive more embolic agents, a phenomenon also known as pseudoselection or flow directed selection.38 With progression of embolization, the vascular resistance increases which leads to a change of local flow dynamics. Bushi et al. studied the effect of the particle size, density, and flow pulsatility in distal distribution in an idealized bifurcation model.11 Notably they showed that the particle distribution is proportional to the flow rate division at the bifurcation. This study and certain others have suggested the prevailing opinion that the embolic beads typically follow the blood stream and distribute proportional to the flow split through ramified vascular branches. However, there has been emerging evidence from in vitro and numerical studies showing the limits of this intuitive assumption. In fact, the fate of particles is a function of multiple hemodynamic factors of which many relevant to the scope of this article has been addressed. For example, Kennedy et al., Childress and Leinstreuer et al. and Amili et al. showed how the fate of particles is strongly affected by their initial location across the vessel.1,13,26 Along with the initial location of the particle trajectories, Aramburu et al. and Van den Hoven et al. showed the location and direction of the microcatheter tip in the injection site is crucial in the fate of particle distribution.3,4,22 In addition, Caine et al. studied the distribution of glass and resin microspheres in an in vitro model of the hepatic arterial bed under physiologically realistic flow conditions and concluded that both types of particles follow the distributing injection solution (containing contrast agent) rather than the arterial flow distribution.12 In another relevant study, Chung et al. studied the particle distribution in a realistic replica of an arterial bed and showed that the particle diameter with respect to the vessel size has an important effect on their transport beyond what is suggested by the flow division at bifurcations.16 All these studies highlight the fact that particle behavior is a complex hemodynamic problem depending on a large number of parameters and cannot be simply estimated by assumptions such as the volumetric flow distribution at bifurcating branches. Further studies with verification and validation by clinical trials and animal models are absolutely needed to shed light on this problem.
Challenges and Recommendation (Expanding Horizons in Embolization)
Challenges primarily include non-target embolization, particle reflux, poor predictability in the particle distribution, extent of necrosis and cell death provoked by occlusion of arteries and poor control on the level of occlusion. Effects of hemodynamics, elasticity, infusion rate and concentration/dilution was also equivocal among different studies.
Our perspective on future research can include addressing challenges in the precise and sufficient transportation of embolic beads to the target vascular bed, design of desirable embolic particles and occlusion microcatheters. In our view, further in vitro and in silico studies are required to understand the fundamental underlying physics governing particle interactions with the blood stream which requires it to be fully verified against animal models and clinical trials. With ever increasing resolution of medical imaging techniques and development of more sophisticated numerical methods, we envision development of physics-informed mathematical models for a precise prediction of the particle distribution as a function of the large parameter space.
Conclusion
Our literature review of the levels of evidence concerning factors that affect the level of distribution and arterial occlusion by embolic particles reveals the sophisticated multifactorial nature of this mechanical-physiological interactive phenomenon. So far we know of a multitude of factors that play different roles in particle distribution and possibly affect the clinical outcomes as detailed above. It has also brought to light several deficiencies. Firstly, it shows the necessity of performing further randomized controlled trials, particularly to investigate the interaction of these factors in different pathological models. Secondly, it highlights the lack of adequately powered trials to produce high quality data. Thirdly, most of the models available are not directly transposable to a clinical context. Finally, with more than 80% of studies focusing on size, aggregation and compressibility, very limited evidence is available concerning the effects of hemodynamics, elasticity, infusion rate and concentration/dilution. Each available product comes with its own set of benefits and drawbacks, all of which require careful consideration by the interventionist. Continued innovation is requisite in order to continue to evolve embolization procedures and ultimately, improve patient outcomes.
Abbreviations
- PVA:
-
Polyvinyl alcohol
- TGMS:
-
Trisacryl gelatin microspheres
- PVAMSs:
-
PVA microspheres
- AVMs:
-
Arteriovenous Malformations
- UAE:
-
Uterine Artery Embolization
References
Amili, O., J. Golzarian, and F. Coletti. in vitro study of particle transport in successively bifurcating vessels. Ann. Biomed. Eng. 47(11):2271–2283, 2019.
Andrews, R. T., and C. A. Binkert. Relative rates of blood flow reduction during transcatheter arterial embolization with tris-acryl gelatin microspheres or polyvinyl alcohol: quantitative comparison in a swine model. J. Vasc. Interv. Radiol. 14(10):1311–1316, 2003.
Aramburu, J., R. Antón, A. Rivas, J. C. Ramos, B. Sangro, and J. I. Bilbao. Numerical investigation of liver radioembolization via computational particle–hemodynamics: the role of the microcatheter distal direction and microsphere injection point and velocity. J. Biomech. 49(15):3714–3721, 2016.
Aramburu, J., R. Antón, A. Rivas, J. C. Ramos, B. Sangro, and J. I. Bilbao. Computational assessment of the effects of the catheter type on particle–hemodynamics during liver radioembolization. J. Biomech. 49(15):3705–3713, 2016.
Arnold, M. J., J. J Keung, and B. McCarragher. Interventional Radiology: Indications and Best Practices: American Academy of Family Physicians; 2019 [Available from: https://www.aafp.org/afp/2019/0501/p547.html.
Beaujeux, R., A. Laurent, J. Hodes, M. Wassef, and J. J. Merland. Calibrated sphere embolization of craniofacial tumors and arteriovenous malformations. Neuroradiology. 16:562–564, 1991.
Bendszus, M., R. Klein, R. Burger, M. Warmuth-Metz, E. Hofmann, and L. Solymosi. Efficacy of trisacryl gelatin microspheres versus polyvinyl alcohol particles in the preoperative embolization of meningiomas. AJNR. 21(2):255–261, 2000.
Bilbao, J. I., E. de Luis, J. A. G. de Jalón, A. de Martino, M. D. Lozano, A. M. de la Cuesta, et al. Comparative study of four different spherical embolic particles in an animal model: a morphologic and histologic evaluation. J. Vasc. Intervent. Radiol. 19(11):1625–1638, 2008.
Brown, A. C., and C. E. Ray. Anterior spinal cord infarction following bronchial artery embolization. Semin. Interv. Radiol. 29(3):241–244, 2012.
Burns, P. B., R. J. Rohrich, and K. C. Chung. The levels of evidence and their role in evidence-based medicine. Plastic Reconstr. Surg. 128(1):305–310, 2011.
Bushi, D., Y. Grad, S. Einav, O. Yodfat, B. Nishri, and D. Tanne. Hemodynamic evaluation of embolic trajectory in an arterial bifurcation: an in-vitro experimental model. Stroke. 36(12):2696–2700, 2005.
Caine, M., M. S. McCafferty, S. McGhee, P. Garcia, W. M. Mullett, X. Zhang, et al. Impact of Yttrium-90 microsphere density, flow dynamics, and administration technique on spatial distribution: analysis using an in vitro model. J. Vasc. Interv. Radiol. 28(2):260–8.e2, 2017.
Childress, E. M., and C. Kleinstreuer. Impact of fluid-structure interaction on direct tumor-targeting in a representative hepatic artery system. Ann. Biomed. Eng. 42(3):461–474, 2014.
Choe, D. H., M. H. Han, G. H. Kang, K. M. Yeon, and M. C. Han. An experimental study of embolic effect according to infusion rate and concentration of suspension in transarterial particulate embolization. Invest. Radiol. 32(5):260–267, 1997.
Chua, G. C., M. Wilsher, M. P. Young, I. Manyonda, R. Morgan, and A. M. Belli. Comparison of particle penetration with non-spherical polyvinyl alcohol versus trisacryl gelatin microspheres in women undergoing premyomectomy uterine artery embolization. Clin. Radiol. 60(1):116–122, 2005.
Chung, E. M., J. P. Hague, M. A. Chanrion, K. V. Ramnarine, E. Katsogridakis, and D. H. Evans. Embolus trajectory through a physical replica of the major cerebral arteries. Stroke. 41(4):647–652, 2010.
Das, R., A. Wale, S. A. Renani, L. Ratnam, L. Mailli, J. Y. Chun, et al. Randomised controlled trial of particles used in uterine fibRoid Embolisation (PURE): non-spherical polyvinyl alcohol versus calibrated microspheres. Cardiovasc. Interv. Radiol. 45(2):207–215, 2022.
Derdeyn, C. P., V. B. Graves, M. S. Salamat, and A. Rappe. Collagen-coated acrylic microspheres for embolotherapy: in vivo and in vitro characteristics. AJNR Am. J. Neuroradiol. 18(4):647–653, 1997.
Golzarian, J., E. Lang, D. Hovsepian, T. Kroncke, L. Lampmann, P. Lohle, et al. Higher Rate of partial devascularization and clinical failure after uterine artery embolization for fibroids with spherical polyvinyl alcohol. Cardiovasc. Interv. Radiol. 29(1):1–3, 2006.
Golzarian, J., and L. Weng. Particle embolization: factors affecting arterial distribution. J. Vasc. Interv. Radiol. 25(11):1773–1774, 2014.
Hidaka, K., L. Moine, G. Collin, D. Labarre, J. L. Grossiord, N. Huang, et al. Elasticity and viscoelasticity of embolization microspheres. J. Mech. Behav. Biomed. Mater. 4(8):2161–2167, 2011.
Hu, J., H. Albadawi, B. W. Chong, A. R. Deipolyi, R. A. Sheth, A. Khademhosseini, et al. Advances in biomaterials and technologies for vascular embolization. Adv. Mater. 31(33):1901071, 2019.
Hwang, J. H., S. W. Park, I. S. Chang, S. I. Jung, H. J. Jeon, Y. S. Lho, et al. Comparison of nonspherical polyvinyl alcohol particles and microspheres for prostatic arterial embolization in patients with benign prostatic hyperplasia. BioMed Res. Int. 2017:8732351, 2017.
Jiang, W., Z. Shen, H. Luo, X. Hu, and X. Zhu. Comparison of polyvinyl alcohol and tris-acryl gelatin microsphere materials in embolization for symptomatic leiomyomas: a systematic review. Minim. Invasive Therapy Allied Technol. 25(6):289–300, 2016.
Kennedy, A. S., C. Kleinstreuer, C. A. Basciano, and W. A. Dezarn. Computer modeling of yttrium-90-microsphere transport in the hepatic arterial tree to improve clinical outcomes. Int J. Radiat. Oncol. Biol. Phys. 76(2):631–637, 2010.
Keussen, I., J. Bengtsson, D. Gavier-Widén, and E. Karlstam. Uterine artery embolization in a sheep model: biodegradable versus non-degradable microspheres. Acta radiologica. 59(10):1210–1217, 2018.
Kishimoto, K., K. Osuga, N. Maeda, Y. Higashi, A. Hayashi, Y. Hori, et al. Embolic effects of transcatheter mesenteric arterial embolization with microspheres on the small bowel in a dog model. J. Vasc. Interv. Radiol. 25(11):1767–1773, 2014.
Laurent, A., M. Wassef, R. Chapot, Y. Wang, E. Houdart, L. Feng, et al. Partition of calibrated tris-acryl gelatin microspheres in the arterial vasculature of embolized nasopharyngeal angiofibromas and paragangliomas. Journal of Vascular and Interventional Radiology 16(4):507–513, 2005.
Laurent, A., M. Wassef, J. Namur, J. Martal, D. Labarre, and J. P. Pelage. Recanalization and particle exclusion after embolization of uterine arteries in sheep: a long-term study. Fertil. Steril. 91(3):884–892, 2009.
Laurent, A., M. Wassef, J. P. Saint Maurice, J. Namur, J. P. Pelage, A. Seron, et al. Arterial distribution of calibrated tris-acryl gelatin and polyvinyl alcohol microspheres in a sheep kidney model. Invest. Radiol. 41(1):8–14, 2006.
Lewis, A. L., C. Adams, W. Busby, S. A. Jones, L. C. Wolfenden, S. W. Leppard, et al. Comparative in vitro evaluation of microspherical embolisation agents. J. Mater. Sci. Mater. Med. 17(12):1193–1204, 2006.
Maluccio, M. A., A. M. Covey, L. B. Porat, J. Schubert, L. A. Brody, C. T. Sofocleous, et al. Transcatheter arterial embolization with only particles for the treatment of unresectable hepatocellular carcinoma. J. Vasc Interv. Radiol. 19(6):862–869, 2008.
McLucas, B., L. Adler, and R. Perrella. Uterine fibroid embolization: nonsurgical treatment for symptomatic fibroids11No competing interests declared. J. Am Coll. Surg. 192(1):95–105, 2001.
McWilliams, J. P., T. A. Bilhim, F. C. Carnevale, S. Bhatia, A. J. Isaacson, S. Bagla, et al. Society of Interventional Radiology Multisociety Consensus Position Statement on Prostatic Artery Embolization for Treatment of Lower Urinary Tract Symptoms Attributed to Benign Prostatic Hyperplasia: From the Society of Interventional Radiology, the Cardiovascular and Interventional Radiological Society of Europe, Société Française de Radiologie, and the British Society of Interventional Radiology: Endorsed by the Asia Pacific Society of Cardiovascular and Interventional Radiology, Canadian Association for Interventional Radiology, Chinese College of Interventionalists, Interventional Radiology Society of Australasia, Japanese Society of Interventional Radiology, and Korean Society of Interventional Radiology. J Vasc Interv. Radiol. 30(5):627–37.e1, 2019.
Moher, D., A. Liberati, J. Tetzlaff, and D. G. Altman. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ. 339:2535, 2009.
Morishita, A., J. Tani, T. Nomura, K. Takuma, M. Nakahara, K. Oura, et al. Efficacy of combined therapy with drug-eluting beads-transcatheter arterial chemoembolization followed by conventional transcatheter arterial chemoembolization for unresectable hepatocellular carcinoma: a multi-Center study. Cancer. 13(18):4605, 2021.
Patel, T. Y., D. M. Hovsepian, and J. R. Duncan. Measurement of blood flow before and after embolization with use of fluorescent microspheres in an animal model. J. Vasc. Interv. Radiol. 17(1):103–111, 2006.
Peixoto, L. S., F. M. Silva, M. A. L. Niemeyer, G. Espinosa, P. A. Melo, M. Nele, et al. Synthesis of Poly(Vinyl Alcohol) and/or Poly(Vinyl Acetate) Particles with Spherical Morphology and Core-Shell Structure and its Use in Vascular Embolization. Macromol. Symp. 243(1):190–199, 2006.
Pelage, J. P., A. Laurent, M. Wassef, M. Bonneau, D. Germain, R. Rymer, et al. Uterine artery embolization in sheep: comparison of acute effects with polyvinyl alcohol particles and calibrated microspheres. Radiology. 224(2):436–445, 2002.
Senturk, C., V. Cakir, K. Yorukoglu, O. Yilmaz, and A. Y. Goktay. Looking for the ideal particle: an experimental embolization study. Cardiovasc. Interv. Radiol. 33(2):336–345, 2010.
Sheth, R. A., S. Sabir, S. Krishnamurthy, R. K. Avery, Y. S. Zhang, A. Khademhosseini, et al. Endovascular embolization by transcatheter delivery of particles: past, present, and future. J. Funct. Biomater. 8(2):14, 2017.
Siskin, G. P., K. Dowling, R. Virmani, R. Jones, and D. Todd. Pathologic evaluation of a spherical polyvinyl alcohol embolic agent in a porcine renal model. J. Vasc. Interv. Radiol. 14(1):89–98, 2003.
Sommer, C. M., T. D. Do, C. L. Schlett, P. Flechsig, T. L. Gockner, A. Kuthning, et al. In vivo characterization of a new type of biodegradable starch microsphere for transarterial embolization. J. Biomater. Appl. 32(7):932–944, 2018.
Stampfl, S., N. Bellemann, U. Stampfl, C. M. Sommer, H. Thierjung, R. Lopez-Benitez, et al. Arterial distribution characteristics of Embozene particles and comparison with other spherical embolic agents in the porcine acute embolization model. J. Vasc. Interv. Radiol. 20(12):1597–1607, 2009.
Torres, D., N. V. Costa, J. Pisco, L. C. Pinheiro, A. G. Oliveira, and T. Bilhim. Prostatic artery embolization for benign prostatic hyperplasia: prospective randomized trial of 100–300 μm versus 300–500 μm versus 100- to 300-μm + 300- to 500-μm embospheres. J. Vasc. Interv. Radiol. 30(5):638–644, 2019.
van den Hoven, A. F., M. G. E. H. Lam, S. Jernigan, M. A. A. J. van den Bosch, and G. D. Buckner. Innovation in catheter design for intra-arterial liver cancer treatments results in favorable particle-fluid dynamics. J. Exp. Clin. Cancer Res. 34(1):74, 2015.
Verret, V., S. H. Ghegediban, M. Wassef, J. P. Pelage, J. Golzarian, and A. Laurent. The arterial distribution of Embozene and Embosphere microspheres in sheep kidney and uterus embolization models. J. Vasc. Interv. Radiol. 22(2):220–228, 2011.
Weiss, C. R., Y. Fu, C. Beh, C. Hu, D. Kedziorek, E.-J. Shin, et al. Bariatric arterial embolization with calibrated radiopaque microspheres and an Antireflux catheter suppresses weight gain and appetite-stimulating hormones in swine. J. Vasc. Interv. Radiol. 31(9):1483–1491, 2020.
Weng, L., M. Rusten, R. Talaie, M. Hairani, N. K. Rosener, and J. Golzarian. Calibrated bioresorbable microspheres: a preliminary study on the level of occlusion and arterial distribution in a rabbit kidney model. J. Vasc. Interv. Radiol. 24(10):1567–1575, 2013.
Wong, Y. S., A. V. Salvekar, K. D. Zhuang, H. Liu, W. R. Birch, K. H. Tay, et al. Bioabsorbable radiopaque water-responsive shape memory embolization plug for temporary vascular occlusion. Biomaterials. 102:98–106, 2016.
Young, S., N. Rostambeigi, and J. Golzarian. The common but complicated tool: review of embolic materials for the interventional radiologist. Semin. Intervent. Radiol. 38(5):535–541, 2021.
Yu, S. C., I. Lok, S. S. Ho, M. M. Tong, and J. W. Hui. Comparison of clinical outcomes of tris-acryl microspheres versus polyvinyl alcohol microspheres for uterine artery embolization for leiomyomas: results of a randomized trial. J. Vasc. Interv. Radiol. 22(9):1229–1235, 2011.
Funding
This study was not supported by any funding.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Informed consent
For this type of study consent for publication is not required.
Additional information
Associate Editor Mona Kamal Marei oversaw the review of this article.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Talaie, R., Torkian, P., Amili, O. et al. Particle Distribution in Embolotherapy, How Do They Get There? A Critical Review of the Factors Affecting Arterial Distribution of Embolic Particles. Ann Biomed Eng 50, 885–897 (2022). https://doi.org/10.1007/s10439-022-02965-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10439-022-02965-6