Abstract
Identifying the associations between head impact biomechanics and clinical recovery may inform better head impact monitoring procedures and identify athletes who may benefit from early treatments aimed to enhance recovery. The purpose of this study was to test whether head injury biomechanics are associated with clinical recovery of symptom severity, balance, and mental status, as well as symptom resolution time (SRT) and return-to-participation (RTP) time. We studied 45 college American football players (n = 51 concussions) who sustained an incident concussion while participating in a multi-site study. Player race/ethnicity, prior concussion, medical history, position, body mass index, event type, and impact location were covariates in our multivariable analyses. Multivariable negative binomial regression models analyzed associations between our study outcomes and (1) injury-causing linear and rotational head impact severity, (2) season repetitive head impact exposure (RHIE), and (3) injury day RHIE. Median SRT was 6.1 days (IQR 5.8 days, n = 45) and median RTP time was 12.3 days (IQR 7.8 days, n = 36) across our study sample. RTP time was 86% (Ratio 1.86, 95% CI [1.05, 3.28]) longer in athletes with a concussion history. Offensive players had SRTs 49% shorter than defensive players (Ratio 0.51, 95% CI [0.29, 0.92]). Per-unit increases in season RHIE were associated with 22% longer SRT (Ratio 1.22, 95% CI [1.09, 1.36]) but 28% shorter RTP time (Ratio 0.72, 95% CI [0.56, 0.93]). No other head injury biomechanics predicted injury recovery.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Sport-related concussions remain a challenging injury for clinicians and scientists. Despite the Berlin21 guidelines amending the first stage in the return-to-sport strategy from complete rest to “symptom-limited activity,” evidence-based clinical treatment options have not been fully explored. Scientifically, traditional time-of-injury clinical factors (e.g., loss of consciousness, post-traumatic amnesia) have not equivocally predicted an injury’s physiological severity or its clinical recovery.17
The scientific community has responded to these uncertainties by exploring how to reduce head injury risk in American football. Several incursions have resulted in our broader understanding of these concepts. These range from policy/rule changes,33,35 player behavior (e.g., anticipation14,31 and style), and play type23 among others; and all have been soundly informed by studying both individual head impact biomechanics as well as repetitive head impact exposure (RHIE). Despite these advances, much remains unknown about the clinical implications associated with subinjurious RHIE and injurious head impacts sustained by athletes.
Surprisingly, few biomechanical studies have explored clinical injury outcomes following incident sport-related concussions.12,30 No correlations between impact magnitude (linear or rotational acceleration) or impact location and changes in symptoms, balance, and neurocognitive performance were previously reported.12 Injury biomechanics were not correlated with individual symptom severity in American college football players,30 or symptom resolution time in American high school football players.3 A number of additional studies have explored risk curves based on on-field biomechanical data;9,29 however, the clinical utility of employing injury thresholds has been questioned in the literature.11,22 Additionally, no studies have investigated whether injury biomechanics are predictive of clinical trajectories and recovery time in a single study of American college football players. Thus, the purpose of this study was to determine whether head injury biomechanics predicted clinical injury recovery as measured by symptom resolution time (SRT), return-to-play (RTP) time, symptom severity, balance, and mental status in a multi-site American college football study. We studied injury-causing biomechanics as well as season and injury day RHIE.
Materials and Methods
Study Design and Participants
We studied 941 Division I collegiate American football players from four civilian universities and two military service academies. These participants comprised a subset of 2232 athletes participating in the Advanced Research Core arm of the NCAA-DOD Concussion Assessment, Research, and Education (CARE) Consortium. All the local sites’ institutional IRBs authorized a reliance agreement with the Medical College of Wisconsin’s Human Research Protection Program and the Department of Defense’s Human Research Protections Office (HRPO). All participants provided informed consent prior to participating in the study. A total of 51 concussive injuries sustained by 45 different athletes were examined in this study. This sample represented every concussion observation for which we had head impact data. In addition to the clinical measures we describe below, we also collected data related to athlete characteristics (Table 1) and injury-causing impact characteristics (Table 2).
Instrumentation
Head Impact Telemetry (HIT) System
The HIT System (Riddell, Elyria, OH) was used to collect head impact biomechanics. The HIT System comprises two primary components: (1) six spring-loaded single-axis accelerometers inserted into Riddell branded helmets, and (2) the Sideline Response System. The in-helmet accelerometers measured linear accelerations, computed component and resultant peak linear and rotational accelerations, and identified impact location. The HIT System was triggered when at least one accelerometer detected a linear acceleration exceeding 9.6 g. The accelerometers collected data at 1 kHz for 40 ms when triggered (pre-trigger 8 ms; post-trigger 32 ms). These data were then date- and time-stamped, encoded, and transmitted by radiofrequency telemetry link to the Sideline Response System. In special circumstances when the real-time data transmission was absent (e.g., signal interruptions, sideline system not set up, etc.), head impacts were locally stored in non-volatile memory built into the monitoring system. The data were processed through a novel algorithm to determine impact magnitude and location.6 Resultant linear accelerations greater than or equal to 10 g were retained for subsequent analyses. The accelerometers were verified regularly for functionality, battery replacements, and head impact data were exported and transmitted to a central data repository for periodic auditing and data consolidation purposes across the study sites. The HIT System was validated in a laboratory setting using hybrid dummies equipped with American football helmets.18
Symptom Inventory
We evaluated 22 symptoms based on the Sport Concussion Assessment Tool 3 (SCAT3) symptom inventory to determine symptom severity. The SCAT3 symptom score demonstrated high sensitivity (72.2%) and specificity (91.7%) in a sample of Canadian university athletes.7 Participants ranked each symptom using a seven-point Likert scale from 0 to 6: none (0), mild (1), through severe (6). We recorded symptom severity score as our primary measure, which is the sum of all the individual symptom severities reported (possible range: 0 to 132). Higher symptom severity scores are interpreted to mean an overall increase in symptom severity.
Balance Error Scoring System (BESS)
The BESS13,25 is an objective assessment tool to evaluate balance we employed in this study. The BESS has demonstrated strong intratester reliability (intraclass correlation coefficients ranging from 0.74 to 0.98) for scoring BESS errors.8,26 The BESS measures balance in six 20-second trials consisting of three stances (double-leg, single-leg, and tandem) on two surfaces (firm and medium density foam).10,15 Participants were asked to stand as still as possible with hands on iliac crests and eyes closed with feet together (double-leg), balancing on their non-dominant limb (single-leg), or heel-to-toe with non-dominant limb in back (tandem). Leg dominance was defined as whichever leg the patient would use to kick a ball for maximum distance. The BESS was scored based on the number of errors committed by the participant during the 20-second trials. Errors included (1) lifting hands off iliac crests, (2) opening eyes, (3) stepping, stumbling or falling, (4) moving the hip into greater than thirty degrees of flexion or abduction, (5) forefoot or heel losing contact with the ground, or (6) remaining out of the testing position for more than 5 s.24 We recorded the BESS total error score (the sum across all six trials) as our outcome measure (possible range: 0 to 60). Higher BESS total error scores are interpreted as worse performance.
Standardized Assessment of Concussion (SAC)
We employed the SAC to evaluate mental status. Extensive research1,20 has demonstrated that the SAC is a sensitive and specific means to detect concussion, and is a sensitive and specific measure of post-concussion recovery. Several alternate forms were administered sequentially across the injury time points (described below) to minimize the SAC learning effects. Lower SAC total scores (possible range: 0 to 30) indicate decreased mental status.
Procedures
All study participants participated in American football throughout the study period. This included practices and both home and away competitions. Home practices/competitions were defined as those taking place at athletic facilities maintained by the athletes’ academic institution. Every participant was asked to complete preseason clinical testing, which included completing the 22-item symptom inventory, BESS, and SAC among other measures. Readers interested in learning more about the CARE Consortium and all the measures collected but not included in this particular analysis can find them described in more detail elsewhere.5
Concussions for this study were operationally defined as “a change in brain function following a force to the head, which may be accompanied by temporary loss of consciousness, but is identified in awake individuals with measures of neurologic and cognitive dysfunction.”5 Each site’s research and medical staff (team physicians and athletic trainers) identified, assessed, and diagnosed concussions in our study participants. If the athlete was immediately removed from play, we identified the most plausible impacts sustained within the last few minutes of participation according to the HIT System output. If the concussion occurred earlier and was not reported until the session end (or even later), we identified the plausible impacts around the time the athlete believed the concussion occurred through follow-up interviews with the study participants by site personnel. These time-stamped data were then compared to video footage when available to identify the injurious impacts. In all cases, these represented the highest magnitude impacts within the time windows reviewed by our study and site clinical teams. Pre- and post-injury testing, which repeated the symptom inventory, BESS, and SAC described above, occurred at the following five time points: (1) pre-injury baseline, (2) time of injury (< 6 h), (3) 24–48 h post-injury, (4) cleared for RTP progression (asymptomatic), and (5) unrestricted RTP. When data were sufficiently available for accurate computations, we employed these time points to derive two primary study outcomes in addition to symptom severity, balance, and mental status outcomes: complete symptom resolution time (SRT) and return-to-play (RTP) time. Additionally, we adapted Rowson et al.28 and Stemper et al.34 methods to derive our RHIE outcomes. Season RHIE included all impacts sustained by the injured athlete up to and including the session they sustained their injury. Injury day RHIE included all impacts (including any that may have occurred after the incident concussion) sustained by the injured player. We rescaled the injury day RHIE by a factor of 10 to facilitate results interpretation.
Data Analyses
Data collected from 51 concussive injuries were examined in this analysis. Athlete characteristics (race/ethnicity, prior concussions, academic year at time of injury, previously diagnosed medical conditions, primary position, weight, height, body mass index [BMI]), injury-causing impact characteristics (event type/injury situation, impact location, injury linear acceleration, injury rotational acceleration, season RHIE, and injury day RHIE), clinical measures of interest (symptom severity score, BESS total error score, SAC total score) as well as injury outcomes (SRT, RTP time) were examined using frequencies (and percentages) for categorical variables and means (and SDs) as well as medians (and IQRs) for continuous variables. Clinical measures collected at the aforementioned five time points were used for our analyses.
We employed negative binomial regression models to analyze our data. We chose the negative binomial distribution for SRT and RTP time in the interest of expressing time-related outcomes as they are naturally observed by clinicians and practitioners (i.e., days until SRT, or days lost following injury). Negative binomial regression models were used to examine the clinical measures due to the inherently discrete nature of the respective clinical scores. Univariate negative binomial regression models were used to examine associations between each explanatory variable of interest (race/ethnicity, prior concussions, previously diagnosed medical conditions, BMI, injury event type, head impact location, injury linear acceleration, injury rotational acceleration, season RHIE, injury day RHIE), and the following injury outcomes: SRT and RTP time. Multivariable negative binomial regression models were then used to identify associations between linear and rotational accelerations of the injury-causing impact and injury outcomes, after adjusting for all non-biomechanical explanatory effects. These multivariable analyses were repeated two more times, one each for season RHIE and injury day RHIE.
Unadjusted mixed effects (random intercepts) negative binomial regression models were used to identify associations between the explanatory variables and clinical measure trajectories for symptom severity, balance, and mental status. Multivariable mixed effects (random intercepts) negative binomial regression models were used to identify associations between linear and rotational acceleration of the injury-causing impact and trajectories of the aforementioned clinical measures over the time points of interest. This procedure was also repeated for season RHIE and injury day RHIE. Mixed effects models were used to make inferences with regard to differential clinical recovery trajectories for ‘similar athletes’ (i.e., athletes with the same level of the random effect). Quadratic patterns in response trajectories were represented using two time-dependent terms (i.e., time and time2) in these models. We employed this approach to ensure that the overall behavior of response variables over the non-constant effect of time on the response variables (which were apparent upon visual inspection of the response trajectories), were appropriately accommodated in the analyses. In suspect cases of compromised model stability (particularly models of mental status recovery trajectories), models were fit using a repeated structure with compound symmetry covariance in lieu of traditional estimation using a random intercept to improve model stability. Effect estimates (expressed as ratios) with 95% confidence intervals (CI) excluding 1.00 were considered significant. Empirical Wald tests based on the robust sandwich covariance estimator were used to confirm statistical significance. Statistical significance was evaluated at the 0.05 level, and all analyses were conducted in SAS 9.4 (SAS Institute, Cary NC).
Results
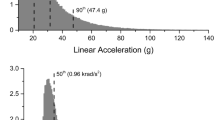
Fifty-one concussions sustained by 45 athletes were examined in this analysis (mass = 108.3 ± 23.2 kg; height = 188.0 ± 7.9 cm; BMI = 30.6 ± 6.3 kg/m2). Injured athlete characteristics (race/ethnicity, academic year, concussion history, medical history, and primary position group) are provided in Table 1. Most concussions occurred during practice sessions (n = 36, 70.6%) and at home sites (n = 42, 76.5%). Over half of all injury-causing impacts were to the front of the head (n = 26, 51.0%). Median injurious linear and rotational accelerations were 66.7 g (IQR 42.8 g) and 2963.0 rad/s2 (IQR 2759.2 rad/s2), respectively. Median season and rescaled injury day RHIE were 0.30 (IQR 1.54) and 0.24 (IQR 0.86), respectively. These and other injury characteristics (event type, injury site, and impact location) are described in Table 2.
Median SRT was 6.1 days (IQR 5.8 days, n = 45) and median RTP time was 12.3 days (IQR 7.8 days, n = 36) for those injuries with data available to accurately compute these outcomes. In our unadjusted analyses, per-unit increases in season RHIE were associated with 22% longer SRT (Ratio 1.22, 95% CI [1.09, 1.36]) and 28% shorter RTP time (Ratio 0.72, 95% CI [0.56, 0.93]). Side impacts were associated with 54% shorter RTP time (Ratio 0.46, 95% CI [0.23, 0.93]) than injurious impacts to front of head. Offensive players had SRTs 49% shorter than defensive players (Ratio 0.51, 95% CI [0.29, 0.92]). The RTP time was 86% longer in athletes with a concussion history compared to those without a concussion history (Ratio 1.86, 95% CI [1.06, 3.28]). All univariate results related to SRT and RTP time can be found in Table 3.
We examined clinical recovery trajectories for symptom severity, balance, and mental status outcomes captured at 5 time points: (1) pre-injury baseline, (2) time of injury (< 6 h), (3) 24–48 h post-injury, (4) cleared for RTP progression (asymptomatic), and (5) unrestricted RTP. In unadjusted analyses, balance outcomes varied by race/ethnicity and for rotational acceleration for similar athletes but did not vary across any other explanatory variable (Table 4). Additionally, trajectories for symptom severity and mental status did not vary across the levels of the explanatory variables of interest for athletes assumed to be at comparable levels of the random effect. No differences in symptom severity, balance, and mental status clinical recovery trajectories were observed in our unadjusted analyses for injury-causing linear acceleration, rotational acceleration (except balance), season RHIE, and injury day RHIE.
In multivariable models, greater season RHIE significantly predicted longer SRT (Ratio 1.25, 95% CI [1.05, 1.48]) and shorter RTP time (Ratio 0.80, 95% CI [0.66, 0.97]) while controlling for our explanatory variables of interest. Linear acceleration, rotational acceleration, and injury day RHIE did not significantly predict SRT or RTP time while controlling for our explanatory variables of interest. Greater rotational acceleration significantly predicted worse balance (Ratio 0.90, 95% CI [0.85, 0.95]) recovery but did not affect symptom severity (Ratio 0.92, 95% CI [0.61, 1.40]) or mental status (Ratio 1.00, 95% CI [0.96, 1.04]) recovery trajectories. Neither linear acceleration, season RHIE, or injury day RHIE predicted symptom severity, balance, or mental status recovery trajectories. All multivariable findings conducted on injury-causing linear acceleration, rotational acceleration, season RHIE, and injury day RHIE after controlling for explanatory variables in SRT, RTP time, and trajectories for symptom severity, balance, and mental status are presented in Table 5.
Discussion
Head injury biomechanics (linear acceleration, rotational acceleration, season RHIE or injury day RHIE) did not predict clinical recovery trajectories for symptom severity, balance, or mental status. Among these biomechanical values, only season RHIE predicted longer SRT and shorter RTP time. These outcomes were measured in 45 concussed American college football athletes representing 51 concussions across six study sites. This overall finding generally agrees with previous preliminary head injury biomechanics studies attempting to address this important clinical research question. Those previous studies demonstrated no correlations between linear and rotational accelerations and post-injury changes in symptoms,12,30 balance,12 and neurocognitive performance.12 Our data additionally support work that has previously addressed American football injury thresholds.11,22 Our findings and those available in the extant literature suggest various additional factors may contribute to individual recovery characteristics including individual tolerability,30 pre-injury head impact exposure,4 and both pre-injury and sub-acute symptom presentations.17
We limited our study of injury-causing head impact biomechanics to those impacts known to cause incident concussion, and to the season RHIE and injury day RHIE sustained by those athletes. Adding RHIE to our study was an important consideration because we must acknowledge that for every injury-causing impact an athlete sustains, they may be exposed to hundreds or even thousands more across a single season or playing career. We cannot discount the role that subinjurious head impact exposure may play in defining individual athlete tolerability to concussion. Rowson et al.30 describe individual-specific tolerance as similar biomechanical inputs producing different clinical manifestations between athletes. Injured American college football players, on average, experienced approximately 94 more head impacts, 10 more high-magnitude impacts (i.e., impacts exceeding the peak acceleration leading to their incident concussion) and a two-fold increase in overall risk-weighted exposure than physically matched controls.27 Our study did not support these Rowson et al.27,30 studies suggesting that pre-injury head impact exposure may play a role in accounting for different recovery trajectories (i.e., symptom severity, balance, and mental status) observed between individuals in large prospective studies such as ours.
Our overall sample median difference between RTP time (12.3 days) and SRT (6.1 days) suggests that most individuals progress through a 6-day RTP strategy consistent with international guidelines.21 However, increases in season RHIE were predictive of longer SRT and shorter RTP time. There may have been mitigating factors beyond the control of our study that led some asymptomatic athletes to progress through their RTP strategy at a quicker rate to return to competition status sooner. It is likely those with higher season RHIE were generated from those athletes who participated more frequently than others (starters vs. reserves). Additionally, the time of season when injuries occurred may have also adjusted site-specific RTP strategies, converting from more conservative approaches early in the season (e.g., fall camp) compared to later in the season. Unfortunately, our study did not capture these details and we can only present reasonable and plausible explanations for the phenomena we observed. Future studies should explore the contrast between an athlete’s symptom duration and resolution time with his or her RTP duration.
The mechanics causing an incident concussion may be plausibly lowered by understanding an athlete’s pre-existing head impact exposure in the context of its temporal distribution. Broglio et al.4 introduced head impact density as a temporally-dependent head impact exposure metric in a cohort of American high school football athletes. Head impact density was higher for injured high school athletes compared to controls despite not observing any differences in head impact magnitudes. Stemper et al.34 additionally studied the effect head impact exposure may have between those who did and did not sustain an incident concussion. Our data support that season RHIE are predictive of longer SRT and shorter RTP time, but do not predict differential recovery trajectories for symptom severity, balance, and mental status. In light of these season RHIE findings, future studies should explore the role impact frequency, chronic exposures (i.e., season and/or career), and timing of these exposures have in contributing to injury risk and subsequent clinical recovery. Future study is warranted to better understand the neurobiopsychosocial underpinnings associated with head impact biomechanics.
Head impact biomechanics alone cannot fully describe the variability we and others have observed in studies addressing clinical outcomes and injury recovery. We studied a number of pre-injury explanatory variables including race/ethnicity, concussion history, medical history, playing position, BMI, event type, and head impact location. Our univariate analyses suggested that non-white/non-black athletes demonstrate longer SRT and longer balance recovery trajectory. Unfortunately, there are no published studies on racial disparities in concussion symptom resolution. However, recent studies have identified that Non-Hispanic Whites perform better on baseline neurocognitive testing,36 demonstrate greater odds of better concussion symptom knowledge and more positive care-seeking attitudes,16 and are more likely to recall and report a possible concussive injury37 than their Black and African American peers. Given racial disparities are pervasive across the medical care continuum, this would be an interesting area for further research. While concussion history did not predict differential clinical recovery trajectories or SRT, we observed an 86% longer RTP time for athletes with a concussion history. These results suggest the clinicians at our study sites likely managed these cases more conservatively than athletes with no injury history. Unfortunately, we do not have data on why clinicians may or may not have elected to follow typical Berlin RTP strategies. A number of unstudied factors may explain this including, but not limited to, symptom exacerbation during one or more steps in the RTP strategy, comorbid conditions (e.g., visual issues not identified until athlete was exposed to more functional activities), or even psychological and mental health considerations. Our study suggests that head injury biomechanics alone are insufficient predictors for clinical recovery. We submit a deeper understanding of neurobiopsychosocial underpinnings can only result from a pan-discipline approach. For example, future studies should intersect head impact biomechanics with advanced neuroimaging and/or biomarkers to better inform clinical recovery characteristics. Incorporating psychosocial outcomes (e.g., Brief Symptom Inventory, anxiety, depression) would complement existing objective outcomes to encompass a holistic neurobiopsychosocial approach to studying sport-related concussion.
Limitations
Despite being one of the largest multi-site studies of its kind, our study was limited to a small sample size that did not permit us to fully explore the scope of potential multivariable analyses described in the discussion. Coupled with our outcomes’ distributional properties, this resulted in analytical instabilities requiring us to tune model parameters (such as the covariance pattern) to find the most appropriately fitting model on an outcome basis. We did not perform a formal power analysis to justify our study’s sample size. Rather, we included all cases for which we had relevant data available. Despite this limitation, we observed several statistically significant differences suggesting our study was adequately powered to support the analyses we conducted. Additionally, participant retention across study time points introduced a pragmatic challenge to our multi-site study. Underreporting concussion symptoms is a known phenomenon among athletes.19 Despite each site’s best efforts, it is possible that our participants chose not to fully disclose their injury symptoms. Additionally, 52% of our injuries were not immediately reported to the site’s clinical staff. Despite this, we describe in our methods the procedures employed for assigning incident impacts to diagnosed injuries and are confident in these assignments. We acknowledge limited video footage available for practice injuries. Our study sample was limited to elite Division I college American football players. We are unable to generalize to other American football levels (professional, high school, youth, etc.) nor are we able to generalize to other helmeted and unhelmeted sports. We also excluded computerized neurocognitive testing for several reasons: (1) computerized neurocognitive testing is not used at all colleges, (2) different platforms were employed by the institutions involved in our study introducing pan-platform compatibility and sample size issues, and (3) data missingness would have compromised our analytical assumptions. Accurately measuring head impact biomechanics presents a continued technical challenge to the scientific community. We acknowledge openly the HIT System is an imperfect system associated with some measurement error2,32 but has been used most frequently in helmeted sports (particularly American football) since 2003.
Conclusions
Sport-related concussions remain a difficult clinical condition to manage. Individualized variability across the injury spectrum (varying injury thresholds, ranging effects of premorbid conditions, etc.) contribute to these challenges. Addressing these and other important clinical research questions also encounter profound technical challenges. We report that head impact biomechanics of incident concussions do not predict recovery in standard clinical outcomes and, with the exception of season RHIE, do not predict SRT or RTP time. We propose a need to follow this study with pan-discipline approaches tying in multiple advanced research metrics to better describe the neurobiopsychosocial underpinnings associated with sport-related concussion and its recovery.
References
Barr, W., and M. McCrea. Sensitivity and specificity of standardized neurocognitive testing immediately following sports concussion. J. Int. Neuropsychol. Soc. 7:693–702, 2001.
Beckwith, J. G., R. M. Greenwald, and J. J. Chu. Measuring head kinematics in football: correlation between the head impact telemetry system and Hybrid III headform. Ann. Biomed. Eng. 40:237–248, 2012.
Broglio, S. P., J. T. Eckner, T. Surma, and J. S. Kutcher. Post-concussion cognitive declines and symptomatology are not related to concussion biomechanics in high school football players. J. Neurotrauma 28:2061–2068, 2011.
Broglio, S. P., A. Lapointe, K. L. O’Connor, and M. McCrea. Head impact density: a model to explain the elusive concussion threshold. J. Neurotrauma 34:2675–2683, 2017.
Broglio, S. P., M. McCrea, T. McAllister, J. Harezlak, B. Katz, D. Hack, B. Hainline, and C. C. Investigators. A National Study on the Effects of Concussion in Collegiate Athletes and US Military Service Academy Members: The NCAA-DoD Concussion Assessment, Research and Education (CARE) Consortium Structure and Methods. Sports Med. 47:1437–1451, 2017.
Crisco, J. J., J. J. Chu, and R. M. Greenwald. An algorithm for estimating acceleration magnitude and impact location using multiple nonorthogonal single-axis accelerometers. J. Biomech. Eng. 126:849–854, 2004.
Downey, R. I., M. G. Hutchison, and P. Comper. Determining sensitivity and specificity of the Sport Concussion Assessment Tool 3 (SCAT3) components in university athletes. Brain Inj. 32:1345–1352, 2018.
Finnoff, J. T., V. J. Peterson, J. H. Hollman, and J. Smith. Intrarater and interrater reliability of the Balance Error Scoring System (BESS). PMR 1:50–54, 2009.
Funk, J. R., S. Rowson, R. W. Daniel, and S. M. Duma. Validation of concussion risk curves for collegiate football players derived from HITS data. Ann. Biomed. Eng. 40:79–89, 2012.
Guskiewicz, K. M. Assessment of postural stability following sport-related concussion. Curr. Sports Med. Rep. 2:24–30, 2003.
Guskiewicz, K., and J. Mihalik. Biomechanics of sport concussion: quest for the elusive injury threshold. Exerc. Sport Sci. Rev. 39:4–11, 2011.
Guskiewicz, K. M., J. P. Mihalik, V. Shankar, S. W. Marshall, D. H. Crowell, S. M. Oliaro, M. F. Ciocca, and D. N. Hooker. Measurement of head impacts in collegiate football players: relationship between head impact biomechanics and acute clinical outcome after concussion. Neurosurgery 61:1244–1252, 2007.
Guskiewicz, K. M., S. E. Ross, and S. W. Marshall. Postural stability and neuropsychological deficits after concussion in collegiate athletes. J. Athl. Train 36:263–273, 2001.
Harpham, J. A., J. P. Mihalik, A. C. Littleton, B. S. Frank, and K. M. Guskiewicz. The effect of visual and sensory performance on head impact biomechanics in college football players. Ann. Biomed. Eng. 42:1–10, 2013.
Hunt, T. N., M. S. Ferrara, R. A. Bornstein, and T. A. Baumgartner. The reliability of the modified Balance Error Scoring System. Clin. J. Sport Med. 19:471–475, 2009.
Kerr, Z. Y., A. K. Nedimyer, M. C. Kay, A. Chandran, P. Gildner, K. H. Byrd, J. K. Haarbauer-Krupa, and J. K. Register-Mihalik. Factors associated with concussion-symptom knowledge and attitudes toward concussion care seeking in a national survey of parents of middle-school children in the U.S. J. Sport Health Sci. 2020. https://doi.org/10.1016/j.jshs.2020.09.001.
Kontos, A. P., R. J. Elbin, A. Sufrinko, G. Marchetti, C. L. Holland, and M. W. Collins. Recovery following sport-related concussion: integrating pre- and postinjury factors into multidisciplinary care. J. Head Trauma Rehabil. 34:394–401, 2019.
Manoogian, S., D. McNeely, S. Duma, G. Brolinson, and R. Greenwald. Head acceleration is less than 10 percent of helmet acceleration in football impacts. Biomed. Sci. Instrum. 42:383–388, 2006.
McCrea, M., T. Hammeke, G. Olsen, P. Leo, and K. Guskiewicz. Unreported concussion in high school football players: implications for prevention. Clin. J. Sport Med. 14:13–17, 2004.
McCrea, M., J. P. Kelly, C. Randolph, J. Kluge, E. Bartolic, G. Finn, and B. Baxter. Standardized assessment of concussion (SAC): on-site mental status evaluation of the athlete. J. Health Trauma Rehabil. 13:27–35, 1998.
McCrory, P., W. Meeuwisse, J. Dvorak, M. Aubry, J. Bailes, S. Broglio, R. C. Cantu, D. Cassidy, R. J. Echemendia, R. J. Castellani, G. A. Davis, R. Ellenbogen, C. Emery, L. Engebretsen, N. Feddermann-Demont, C. C. Giza, K. M. Guskiewicz, S. Herring, G. L. Iverson, K. M. Johnston, J. Kissick, J. Kutcher, J. J. Leddy, D. Maddocks, M. Makdissi, G. T. Manley, M. McCrea, W. P. Meehan, S. Nagahiro, J. Patricios, M. Putukian, K. J. Schneider, A. Sills, C. H. Tator, M. Turner, and P. E. Vos. Consensus statement on concussion in sport-the 5th international conference on concussion in sport held in Berlin, October 2016. Br. J. Sports Med. 51:838, 2017.
Mihalik, J. P., R. C. Lynall, E. B. Wasserman, K. M. Guskiewicz, and S. W. Marshall. Evaluating the “Threshold Theory”: can head impact indicators help? Med. Sci. Sports Exerc. 49:247–253, 2017.
Ocwieja, K. E., J. P. Mihalik, S. W. Marshall, J. D. Schmidt, S. C. Trulock, and K. M. Guskiewicz. The effect of play type and collision closing distance on head impact biomechanics. Ann. Biomed. Eng. 40:90–96, 2012.
Riemann, B. L., and K. M. Guskiewicz. Effects of mild head injury on postural stability as measured through clinical balance testing. J. Athl. Train 35:19–25, 2000.
Riemann, B. L., K. M. Guskiewicz, and E. Shields. Relationship between clinical and forceplate measures of postural stability. J. Sport Rehabil. 8:71–82, 1999.
Riemann, B. L., K. M. Guskiewicz, and E. W. Shields. Relationship between clinical and forceplate measures of postural stability. Journal of Sport Rehabilitation 8:71–82, 1999.
Rowson, S., E. T. Campolettano, S. M. Duma, B. Stemper, A. Shah, J. Harezlak, L. Riggen, J. P. Mihalik, K. M. Guskiewicz, C. Giza, A. Brooks, K. Cameron, T. McAllister, S. P. Broglio, and M. McCrea. Accounting for variance in concussion tolerance between individuals: comparing head accelerations between concussed and physically matched control subjects. Ann. Biomed. Eng. 47:2048–2056, 2019.
Rowson, S., and S. M. Duma. Brain injury prediction: assessing the combined probability of concussion using linear and rotational head acceleration. Ann. Biomed. Eng. 41:873–882, 2013.
Rowson, S., S. M. Duma, J. G. Beckwith, J. J. Chu, R. M. Greenwald, J. J. Crisco, P. G. Brolinson, A. C. Duhaime, T. W. McAllister, and A. C. Maerlender. Rotational head kinematics in football impacts: an injury risk function for concussion. Ann. Biomed. Eng. 40:1–13, 2012.
Rowson, S., S. M. Duma, B. D. Stemper, A. Shah, J. P. Mihalik, J. Harezlak, L. D. Riggen, C. C. Giza, J. P. DiFiori, A. Brooks, K. Guskiewicz, D. Campbell, G. McGinty, S. J. Svoboda, K. L. Cameron, S. P. Broglio, T. W. McAllister, and M. McCrea. Correlation of concussion symptom profile with head impact biomechanics: a case for individual-specific injury tolerance. J. Neurotrauma 35:681–690, 2018.
Schmidt, J. D., K. M. Guskiewicz, J. P. Mihalik, J. T. Blackburn, G. P. Siegmund, and S. W. Marshall. Head impact magnitude in american high school football. Pediatrics 2016. https://doi.org/10.1542/peds.2015-4231.
Siegmund, G. P., K. M. Guskiewicz, S. W. Marshall, A. L. DeMarco, and S. J. Bonin. Laboratory validation of two wearable sensor systems for measuring head impact severity in football players. Ann. Biomed. Eng. 44:1257–1274, 2016.
Stemper, B. D., A. S. Shah, J. Harezlak, S. Rowson, S. Duma, J. P. Mihalik, L. D. Riggen, A. Brooks, K. L. Cameron, C. C. Giza, M. N. Houston, J. Jackson, M. A. Posner, G. McGinty, J. DiFiori, S. P. Broglio, T. W. McAllister, and M. McCrea. Repetitive head impact exposure in college football following an NCAA rule change to eliminate two-a-day preseason practices: a study from the NCAA-DoD CARE Consortium. Ann. Biomed. Eng. 47:2073–2085, 2019.
Stemper, B. D., A. S. Shah, J. Harezlak, S. Rowson, J. P. Mihalik, S. M. Duma, L. D. Riggen, A. Brooks, K. L. Cameron, D. Campbell, J. P. DiFiori, C. C. Giza, K. M. Guskiewicz, J. Jackson, G. T. McGinty, S. J. Svoboda, T. W. McAllister, S. P. Broglio, M. McCrea, and C. C. Investigators. Comparison of head impact exposure between concussed football athletes and matched controls: evidence for a possible second mechanism of sport-related concussion. Ann. Biomed. Eng. 47:2057–2072, 2019.
Stemper, B. D., A. S. Shah, J. P. Mihalik, J. Harezlak, S. Rowson, S. Duma, L. D. Riggen, A. Brooks, K. L. Cameron, C. C. Giza, J. Goldman, M. N. Houston, J. Jackson, G. McGinty, S. P. Broglio, T. W. McAllister, and M. McCrea. Head impact exposure in college football after a reduction in preseason practices. Med. Sci. Sports Exerc. 52:1629–1638, 2020.
Wallace, J., R. Moran, E. Beidler, J. McAllisterDeitrick, J. Shina, and T. Covassin. Disparities on baseline performance using neurocognitive and oculomotor clinical measures of concussion. Am. J. Sports Med. 48:2774–2782, 2020.
Wallace, J., R. Moran, A. Bretzin, B. Hileman, and G. S. Huang. Examination of racial disparities in adolescents seen in the emergency department for head, neck, or brain injury. J. Emerg. Med. 2020. https://doi.org/10.1016/j.jemermed.2020.07.002.
Acknowledgments
This investigation was made possible, in part, with support from the Grand Alliance Concussion Assessment, Research, and Education (CARE) Consortium, funded, by the National Collegiate Athletic Association (NCAA) and the Department of Defense (DoD). The U.S. Army Medical Research Acquisition Activity, 820 Chandler Street, Fort Detrick MD 21702-5014 is the awarding and administering acquisition office. This work was supported by the Office of the Assistant Secretary of Defense for Health Affairs through the Psychological Health and Traumatic Brain Injury Program under Award No. W81XWH-14-2-0151. Opinions, interpretations, conclusions and recommendations are those of the authors and are not necessarily endorsed by the Department of Defense (DHP funds).
The authors would also like to thank Jody Harland, Janetta Matesan (Indiana University); Ashley Rettmann and Nicole L’Heureux (University of Michigan); Melissa Koschnitzke (Medical College of Wisconsin); Michael Jarrett, Vibeke Brinck and Bianca Byrne (Quesgen); Thomas Dompier, Christy Collins, Melissa Niceley Baker, and Sara Dalton (Datalys Center for Sports Injury Research and Prevention); and the research and medical staff at each of the participating sites.
CARE Consortium Investigators: The authors would like to thank the individual site PIs and the study personnel they represent who ensured appropriate participant recruitment, data collection, and providing clinical care to those who were injured. Those site PIs are Alison Brooks (University of Wisconsin), Jonathan Jackson (Air Force Academy), Kenneth Cameron and Megan Houston (West Point Academy), and others from University of California at Los Angeles and Air Force Academy.
Author information
Authors and Affiliations
Consortia
Corresponding author
Additional information
Associate Editor Joel D Stitzel oversaw the review of this article.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Collaborators of the CARE Consortium Investigators are listed in “Acknowledgments”.
Rights and permissions
About this article
Cite this article
Mihalik, J.P., Chandran, A., Powell, J.R. et al. Do Head Injury Biomechanics Predict Concussion Clinical Recovery in College American Football Players?. Ann Biomed Eng 48, 2555–2565 (2020). https://doi.org/10.1007/s10439-020-02658-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10439-020-02658-y