Abstract
High oxidative stress can occur during ischemic reperfusion and chronic inflammation. It has been hypothesized that such oxidative challenges could contribute to clinical risks such as deep tissue pressure ulcers. Skeletal muscles can be challenged by inflammation-induced or reperfusion-induced oxidative stress. Oxidative stress reportedly can lower the compressive damage threshold of skeletal muscles cells, causing actin filament depolymerization, and reduce membrane sealing ability. Skeletal muscles thus become easier to be damaged by mechanical loading under prolonged oxidative exposure. In this study, we investigated the preventive effect of poloxamer 188 (P188) on skeletal muscle cells against extrinsic oxidative challenges (H2O2). It was found that with 1 mM P188 pre-treatment for 1 h, skeletal muscle cells could maintain their compressive damage threshold. The actin polymerization dynamics largely remained stable in term of the expression of cofilin, thymosin beta 4 and profilin. Laser photoporation demonstrated that membrane sealing ability was preserved even as the cells were challenged by H2O2. These findings suggest that P188 pre-treatment can help skeletal muscle cells retain their normal mechanical integrity in oxidative environments, adding a potential clinical use of P188 against the combined challenge of mechanical-oxidative stresses. Such effect may help to prevent deep tissue ulcer development.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Deep tissue pressure ulcer is a serious clinical issue affecting millions of people with physical disability. Preventive measures are still limited due to the lack of attention to the many contributing factors. Mechanical deformation due to pressure and shear is a well-recognized predisposing factor in pressure ulcer development. Ischemic–reperfusion (IR) is believed to be also involved in pressure ulcer development.23,32 It has been shown that IR can generate high oxidative stress in various tissues,1,28,38 including skeletal muscle.3 The effects of oxidative stress in muscle have been widely discussed, such as their contribution to force generation,25 their involvement in inflammatory responses during muscle repair13,31 and their role in diseases such as muscle atrophy.26 Our group has previously described the effects of oxidative stress on skeletal muscle cell mechanics. We demonstrated that prolong oxidative stress would lower muscle cell stiffness, the number of actin filament, pre-tension,14,34 compressive damage threshold,36 and membrane repair ability.7 As muscle tissues become easier to be mechanically damaged under prolong oxidative stress due to IR and/or chronic inflammation, oxidative challenge can increase the risk of deep tissue injury (DTI). DTI is hardly detectable clinically at its beginning and can ultimately expand towards the skin surface to become a full-thickness pressure ulcer. Methods that can reduce the combined challenges of oxidative and mechanical stresses may help to lower the risk of deep tissue pressure ulcer.
Antioxidant supplements have been proposed to prevent muscle from damage. Researchers have applied vitamin C/vitamin E supplements to patients at risk of pressure ulcer. However, the beneficial effects of antioxidants supplements have yet to be confirmed. A detailed review can be found in McGinley et al.17 Effective protection of muscle from mechanical damage in oxidative environment is still in demand.
Poloxamer is a general term for a class of nonionic synthetic polymers composed of a hydrophobic poly-oxypropylene chain chelated with two hydrophilic poly-oxyethylene chains (Supplementary Fig. 1). Its amphiphilic property leads to a wide range of industrial and pharmaceutical applications. In addition to its manufactory usages, poloxamer also showed biological effects, such as in altering enzymatic activities in heart and liver.12 Such effects depend on the size and the exact composition of poloxamer.
Among different poloxamer compounds, poloxamer 188 (P188) showed multiple biological effects. Some studies reported that P188 had deleterious effects such as increasing muscle susceptibility to contraction injury30 and increasing the permeability of exercised muscle27 and cardiac fiber.29 On the other hands, it was also reported that P188 protects neuron cells from toxin,15 prevents skeletal muscle necrosis from irradiation,9 blocks dystrophic heart failure,37 and improves renal dysfunction.8 P188 also exhibited protective effect on IR damage in muscles,21,33 intestines11 and neurons.10 Another well-recognized function of poloxamer is its cells membrane repair ability. It could promote membrane repair in neuroblastoma cells,19 fibroblasts,18 electropermeablized skeletal muscles4 and alveolus.24
Taking into account that P188 could help to prevent IR damage and promote membrane sealing, we hypothesized that P188 could protect skeletal muscle cells against the combined challenge of physical and oxidative stresses.
Materials and Methods
Cell Culture, Chemicals and Treatment Groups
C2C12, murine myoblasts cells line, was purchased from ATCC (#CRL-1772). The cells were cultured with medium composed of Dulbecco’s Modified Eagle’s Medium (DMEM), 10% Fetal Bovine Serum (FBS) and 1% Penicillin–Streptomycin (P–S) in a 5% CO2 and 37 °C incubator. When the culture reached 90% confluence, the culture medium was replaced by DMEM + 2% FBS + 1% P-S (differentiation medium) to trigger myotubes differentiation, Myotubes formed after 3–5 days incubation with differentiation medium.
Myotubes were used for compressive damage threshold and actin filament polymerization analysis. Pre-confluent myoblasts culture was used for laser photoporation experiment for better visualization of the cell boundary.
Hydrogen peroxide (H2O2) served as an extrinsic oxidant to introduce oxidative stress to the cells in this study. P188 was purchased from sigma (P5556). Both P188 and H2O2 were diluted with differentiation medium to the desired concentration in each experiment.
To investigate the effect of poloxamer pre-treatment on muscle cells in response to oxidative insult, four experimental groups were set: (A) Control group without any P188 and H2O2 treatment; (B) P188 treatment group in which the cells were treated with 1 mM of P188 for 1 h, to study the effect of P188 on muscle cells; (C) H2O2 treatment group in which the cells were treated with H2O2 for 20 h; (D) P188 pre-treatment group in which the cells were first treated first with 1 mM of P188 for 1 h, then the poloxamer containing medium was removed and the culture was rinsed with PBS three times before H2O2 medium was applied for another 20 h.
Compressive Threshold Measurement
We investigated the effect of P188 pre-treatment on muscle cells compressive damage stress threshold using the similar method that our group reported previously.36 0.5 mM H2O2 was chosen as this concentration could cause significant threshold changes.36 In brief, after the experimental treatments, 0.5% agarose gel was fabricated on top of the monolayer of treated cells. Mach-1 micromechanical system (Biomomentum Inc.) was used to apply an indentation with a half-spherical indenter of 6.38 mm diameter at a rate of 0.01 mm/s until 50% compressive strain of the gel at the center was reached, to generate a radial compressive stress field at the bottom of the gel layer. The stress profile was estimated using a finite element model. The stress is highest at the center and decreases along with the radial position of the dish. Constant indentation was maintained for 70 min. The whole process was conducted within an incubator with temperature maintained at 37 °C. After the indentation, 10 mg/ml propidium iodide (PI) was applied to the culture for cell damage assay. The compressive damage thresholds, with unit Pascal (Pa), were then estimated by defining the radial position of the edge of damage zone. The methodology is illustrated in Fig. 1.
Real-Time PCR
We studied the effect of P188 on actin filament polymerization dynamics using the same approach reported by Wong et al.34 In this part of investigation, the oxidative strength was set at 1.0 mM, as this concentration of H2O2 could induced a significant shift of the polymerization dynamics as we previously demonstrated.34 After the oxidative treatment procedure was done, the cultures were briefly washed with diethyl pyrocarbonate (DEPC) treated PBS. 1 mL of RNAiso Plus (TaKaRa #9109) was applied for total RNA extraction. 200 μL of chloroform was then added to each sample and mixed vigorously. The extracts were centrifuged at 12,500 rpm and 4 °C for 20 min for phase separation. The upper layer, where the total RNA was, was transferred into a new tube. 500 μL of isopropanol was added to the samples, and the samples stood at room temperature for 10 min for RNA precipitation. The same centrifugation was repeated and the supernatants were discarded. The remaining total RNA was washed with 1 mL of 75% DEPC-EtOH, vortexed, and centrifuged at 7500 rpm, 4 °C for 5 min, to remove the unwanted salts. DEPC-EtOH was then discarded and the tubes were allowed to be air dried. The RNA pellet was re-suspended by 20 μL of DEPC-H2O and warmed at 65 °C for 10 min. The concentration of total RNA was measured using Nanodrop®. 1 μg of total RNA was reverse transcribed by using RevertAid™ First Strand cDNA Synthesis Kit (Fermetas, K1622) to convert the mRNA to cDNA. The cDNAs was ready for Real-time PCR assay. The primers used are shown in Table 1. SYBR green reaction kit from TaKaRa (DRR041A) was used for Real-time PCR. The reaction was performed in an Abi viia7 real-time PCR machine with 2(−ΔΔCt) method while GAPDH was used as the housekeeping gene for internal control.
Femtosecond Laser Photoporation
We elucidated the effect of P188 on the vulnerability of muscle cells to damage by femtosecond laser photoporation, largely similar to the methods reported earlier.7 After P188 and/or H2O2 treatment, the cultured cells were stained with calcein AM (1 μg/ml) for viability, and with plasma membrane dye Molecular Probe® (5 μg/ml, Thermo Fisher Scientific, C10046) to identify cell membrane. Photoporation was delivered to the cells with laser power of 22 mV for 2 s exposure. The initial size of the holes generated by the laser and the number of cells capable of resealing the hole was recorded by a 63× water immersed objective lens for analysis. Initial hole means the hole shown on the image scan immediately after laser hit. Images were processed with a built-in binary algorithm by ImageJ. The size was presented in μm2, using the microscope calibration standard for actual length per image pixel. The resealed cells were defined by the criteria that the initial hole could no longer be identified within 100 s after the laser hit. Total 15 cells from 3 separated experiments were observed.
Statistical Analysis
One-way ANOVA test and post hoc Tukey’s HSD test was performed for statistical difference analysis among experimental groups. Statistical significance was claimed with p < 0.05.
Results
P188 Effect on Compressive Damage Stress Threshold of Myotubes After Oxidative Insult
Myotubes cultures were successfully differentiated and confirmed by its fibered morphology (Fig. 2B). The results of the compressive damage threshold study were shown in Fig. 3. The control group, without any P188 and H2O2 treatment, showed a compressive damage threshold at about 288.7 ± 14.4 Pa. After 0.5 mM H2O2 treatment for 20 h, the compressive damage stress threshold decreased to 174.3 ± 65.7 Pa, implying that myotubes became easier to be damaged after the oxidative insult. Pre-treating the cells with 1 mM P188 for 1 h, the compressive threshold declined slightly to 255.5 ± 18.8 Pa, but no significance when compared to control. These data supported that muscle cells would not be significantly weakened after 1 mM P188 treatment for 1 h. For the last group where muscle cells were pre-treated with 1 mM P188 and then subjected to 0.5 mM H2O2 oxidative insult for 20 h, the compressive damage stress threshold value remained at the similar level as control, 291.8 ± 16.9 Pa. Thus, the results of this study supported that pre-treatment of P188 could reduce the weakening effect by prolong H2O2 exposure. No significant differences could be established in the compressive damage stress thresholds between control and the P188 pre-treatment group.
P188 Effect on Actin Filament Polymerization Regulation After Oxidative Insult
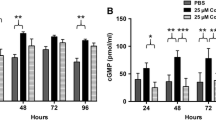
The transcriptional expressions of three actin filament polymerization regulatory proteins, cofilin2, thymosin beta 4 and profilin1 were shown in Fig. 4 and Table 2. For cofilin2, the relative expression level significantly increased by +55.2 ± 14% after 1 mM H2O2 exposure for 20 h. 1 mM P188 treatment for 1 h down-regulated cofilin2 expression by about 6.5 ± 5.5%, but no significant difference was established. Pre-treatment of 1 mM P188 for 1 h and then applying 1 mM oxidative challenge to the culture led to about 12.9 ± 24.5% up-regulation of cofilin2, which was statistically significant when compared to control. For thymosin beta 4, 1 mM H2O2 treatment for 20 h caused about 32.9 ± 14.4% down-regulation, which was statistically significant. 1 mM P188 treatment for 1 h showed 7.5 ± 11.9% increase of thymosin beta 4 expression; and 7.6 ± 9.8% down-regulation of thymosin beta 4 was recorded in the P188 pre-treatment group with the subsequent 20 h of 1 mM H2O2 treatment. These two differences did not show significance compared to control. For Profilin1, 35.3 ± 24.5% up-regulation was shown in 1 mM H2O2 treatment group. 6.2 ± 12.1 and 11.0 ± 8.5% increase in profilin1 expression were recorded respectively for the 1 mM P188 treatment group and the P188 pre-treatment group with subsequent 1 mM H2O2 treatment for 20 h. Only the up-regulation effect in the H2O2 treatment group was found to be significant. No significant differences were found in the CT values of the reference gene among experiments.
Relative expressions of the regulatory proteins for actin filament polymerization. (a) Cofilin2; (b) thymosin beta 4; (c) profilin1. The relative expression level is an average of three individual experiments and each individual experiment consisted of a triplicate assay (*p < 0.05 compared to control).
P188 Effect on Cell Damage and Repair After Femtosecond Laser Photoporation Under Oxidative Stress
The initial hole sizes generated in various experimental groups by 22 mV femtosecond laser power for 2 s exposure were shown in Figs. 5 and 6. The average initial hole size for the control group was 26.5 ± 9.1 μm2. After 0.5 mM H2O2 treatment for 20 h or 1 mM P188 treatment for 1 h, the average initial hole size increased to 40.0 ± 9.2 and 35.8 ± 6.9 μm2 respectively. These increases were found to be statistically significant, indicating that 0.5 mM H2O2 for 20 h alone or 1 mM P188 treatment alone for 1 h would make the cells more vulnerable to laser damage. As for the group with cells pre-treated with 1 mM P188 for 1 h followed by 0.5 mM H2O2 treatment for 20 h, the initial hole size was 25.0 ± 7.1 μm2, which showed no significant difference with the control group. This value was found to be significantly smaller than the two treatment groups mentioned above. The percentages of cells having their laser generated holes resealed were 80, 33, 73 and 100% for the control group, the H2O2 treatment group, the P188 treatment group and the P188 pre-treatment group with subsequent 0.5 mM H2O2 treatment for 20 h, respectively (Table 3).
Discussion
Oxidative stress frequently occurs in skeletal muscle, such as during aerobic activities. We have reported here the preventive effects of P188 against oxidative challenge in myotubes, in terms of their compression damage stress thresholds, actin filament polymerization regulation, and cell membrane damage and repair after femtosecond laser photoporation. Our data revealed that, pre-treatment of 1 mM P188 for 1 h can prevent the H2O2–induced loss of integrity in the cell membrane and cytoskeleton, thus maintaining the resistance of myotubes against biophysical damages.
The compressive damage threshold of myotubes (288.7 ± 14.4 Pa) was slightly lower than our previous finding in myoblasts (330.0 ± 7.8 Pa) as reported by Yao et al.,36 indicating the myotubes might not resist compressive damage as well as myoblasts do. This observation agreed with Bouten’s finding using an agarose 3D muscle construct.2
After H2O2 treatment, the compressive damage threshold was significant lowered, indicating that myotubes become more vulnerable under compressive challenge. One of the possible explanations for such effects was related to the stabilization of actin filament polymerization dynamics. The actin filament network is in a dynamic status. Profilin promotes polymerization by bringing actin monomers into the existing actin filaments, while cofilin takes actin monomer out from the filaments, hence to depolymerize the filament. Thymosin beta 4 competes with cofilin to bind on the actin molecule.6 We have reported that prolonged 1 mM H2O2 treatment can shift actin filament polymerization dynamics to the depolymerization side,34 because of the up-regulation of cofilin and down-regulation of thymosin beta 4, leading to an extra efficiency for actin filament depolymerization. We hypothesize that the up-regulation of profilin is a cellular response to the loss of actin filaments, but such up-regulation could not fully compensate for the actin filaments lost, which was confirmed by phalloidin staining.34 Since actin filaments provide a major structural support to the cells. Actin depolymerization would reduce the mechanical strength of the cells.
With the pre-treatment of P188, the expression of thymosin beta 4 and profilin1 did not show significant difference compared to control, even after 1 mM H2O2 treatment for 20 h. Only cofilin2 showed a significant up-regulation. However, such up-regulation effect was relatively small (the MSD by Tukey’s test was 0.1289, while the critical value was 0.1286) to the point that it did not cause significant change in the compressive damage threshold. This indicates that, with the pre-treatment of P188, the polymerization dynamics was largely maintained in the presence of prolong H2O2 challenge. Such stabilization effect can help to maintain the actin cytoskeleton, allowing the cells to maintain their compressive strength. No additional strengthening effect was observed after P188 treatment.
We studied the vulnerability of cells to photoporation using femtosecond laser. With P188 pre-treatment before the 20 h of oxidative insult, the initial hole created by the same laser power was significantly smaller than the H2O2 treatment group without P188 pre-treatment (25.0 vs. 40.0 μm2). We can claim that P188 helps muscle cell membrane maintain its ability to sustain photoporation after H2O2 challenge. Here again, P188 can only maintain the original resistance of the cells against laser photoporation as before the oxidative insult. No significant differences can be established between control and the group with P188 pre-treatment before the 20 h of 0.5 mM H2O2 treatment.
One intriguing observation was that with P188 treatments alone, the initial hole size was significantly larger than those of control (35.8 vs. 26.5 μm2), though not as large as those in the H2O2 treatment group (40.0 μm2). Yet, 73% of those holes could be resealed by the P188 pre-treated cells, only slightly lower than the 80% resealing rate in the control group. This finding suggests that the P188 treatment could change the physical properties of the cell membrane, making the membrane more vulnerable to laser photoporation. But the P188 pre-treatment did not lower the resealing capacity like H2O2 did. The exact mechanism behind has to be further investigated. This could be the reason of the little difference in the compressive damage stress thresholds between the control and the P188 pre-treatment group, as the damaged cell membrane could be readily resealed and PI could not get in.
Interestingly, with P188 pre-treatment before the oxidative insult, membrane resealing after laser photoporation was 100%, higher than all other groups (Table 3). In most of the reported studies related to membrane sealing in P188 treated cells, P188 was applied after the damage,20 thus affirming the therapeutic effects of P188 rather than its preventive effects. In this study, the enhancement in membrane repair could still be recorded even P188 was not apparently present in the medium when the insult was introduced.
Maskarinec et al. demonstrated how P188 might interact with the lipid bilayer of cell membrane and proposed that this molecule could bind onto the damaged sites on the membrane to facilitate membrane sealing.16 They claimed that P188 would be removed from the membrane after the damage was completely repaired. Another study on the interaction between P188 and cell membrane demonstrated that P188 interacted with structurally disrupted lipid layer and was removed when the membrane became reestablished.35 Our observations here apparently showed for the first time possible interaction between P188 and normal cell membrane, which enough to bring forth the preventive effects of P188.
The interaction between P188 and normal cell membrane has to be further investigated. Dastgheyb et al.5 reported a modification protocol of chelating a fluorescent probe on P188. This approach may help to reveal how P188 interacts with normal cell membrane.
A possible mechanism for P188’s binding on normal cell membrane is related to surface tension. In the above-mentioned study, Maskarinec et al. reported that P188 was inserted into a lipid monolayer with drastically higher rates when the surface tension decreased.16 Assuming surface tension was a key factor permitting P188 to bind to the cell membrane, we hypothesize that P188 may possibly interact with non-damaged cell membrane as a living cell is dynamically modulating cellular homeostasis to accommodate cellular events such as migration and exocytosis. This may lead to inhomogeneous surface tension on the cell membrane, potentially lowering the surface tension at some sites to a point low enough for P188 to interact with cell membrane even without deliberate experimental insults. Such interaction may lead to changes in membrane properties that help the cell to sustain mechanical and oxidative challenge. More studies have to be conducted to fully understand the interaction mechanism between P188 and intact cell membrane to decipher the protective effects of P188 on muscle cells mechanics.
P188 is currently in phase III clinical trial. There are increasing applications of P188 to protect different cell types and tissue systems against pathological challenges.20 The protective mechanism of P188 for muscle cells still leave much to be understood. While P188 treatment could show positive effects like preserving force generation in muscle after contraction injury,22 negative effects like increasing susceptibility to contraction injury have also been reported.30 Such discrepancy may be due to the differences in dose concentration, number of administration or treatment duration of P188 in different systems. The standard treatment protocol of P188 has yet to be confirmed.
Here we submitted with report the effects of P188 in muscle damage mechanics. Pre-treatment of P188 could maintain compressive damage threshold, actin polymerization regulation, and membrane sealing capability of skeletal muscle cells under oxidative stress. Our findings added a potential application of this compound in counteracting the combined damaging effects of prolonged oxidative and mechanical stresses.
References
Aragno, M., J. C. Cutrin, R. Mastrocola, M. G. Perrelli, F. Restivo, G. Poli, O. Danni, and G. Boccuzzi. Oxidative stress and kidney dysfunction due to ischemia/reperfusion in rat: attenuation by dehydroepiandrosterone. Kidney Int. 64(3):836–843, 2003.
Bouten, C. V., M. M. Knight, D. A. Lee, and D. L. Bade. Compressive deformation and damage of muscle cell subpopulations in a model system. Ann. Biomed. Eng. 29(2):153–163, 2001.
Carmo-Araujo, E. M., M. Dal-Pai-Silva, V. Dal-Pai, R. Cecchini, and A. L. A. Ferreira. Ischemia and reperfusion effects on skeletal muscle tissue: morphological and histochemical studies. Int. J. Exp. Pathol. 88(3):147–154, 2007.
Collins, J. M., F. Despa, and R. C. Lee. Structural and functional recovery of electropermeabilized skeletal muscle in vivo after treatment with surfactant poloxamer 188. Biochim. Biophys. Acta 1768(5):1238–1246, 2007.
Dastgheyb R. M., M. C. Cochran, and K. A. Barbee. Interactions of fluorescein isothiocyanate-labeled poloxamer P188 with cultured cells. Bioengineering Conference (NEBEC), 2012. doi:10.1109/NEBC.2012.62070989.
Dedova, I. V., O. P. Nikolaeva, D. Safer, E. M. De La Cruz, and C. G. dos Remedios. Thymosin beta 4 induces a conformational change in actin monomers. Biophys. J. 90(2):985–992, 2006.
Duan, X., K. T. Chan, K. K. H. Lee, and A. F. T. Mak. Oxidative stress and plasma membrane repair in single myoblasts after femtosecond laser photoporation. Ann. Biomed. Eng. 43(11):2735–2744, 2015.
Emanuele, M., and B. Balasubramaniam. differential effects of commercial-grade and purified poloxamer 188 on renal function. Drugs R & D 14:73–83, 2014.
Greenebaum, B., K. Blossfield, J. Hannig, C. S. Carrillo, M. A. Beckett, R. R. Weichselbaum, and R. C. Lee. Poloxamer 188 prevents acute necrosis of adult skeletal muscle cells following high-dose irradiation. Burns 30(6):539–547, 2004.
Gu, J., J. Ge, M. Li, H. Xu, F. Wu, and Z. Qin. Poloxamer 188 protects neurons against ischemia/reperfusion injury through preserving integrity of cell membranes and blood brain barrier. PLoS One 8(4):e61641, 2013.
Hunter, R. L., A. Z. Luo, R. Zhang, R. A. Kozar, and F. A. Moore. Poloxamer 188 inhibition of ischemia/reperfusion injury: evidence for a novel anti-adhesive mechanism. Ann. Clin. Lab. Sci. Spring 40(2):115–125, 2010.
Korolenko, T. A., T. P. Johnston, N. I. Dubrovina, Y. A. Kisarova, S. Y. Zhanaeva, M. S. Cherkanova, E. E. Filijushina, T. V. Alexeenko, E. Machova, and N. A. Zhukova. Effect of poloxamer 407 administration on the serum lipids profile, anxiety level and protease activity in the heart and liver of mice. Interdiscip. Toxicol. 6(1):18–25, 2013.
Kozakowska, M., K. P. Gremplewicz, A. Jozkowicz, and J. Dulak. The role of oxidative stress in skeletal muscle injury and regeneration: focus on antioxidant enzymes. J. Muscle Res. Cell Motil. 26:377–393, 2015.
Ma, Z., Y. S. Wu, and A. F. T. Mak. Rheological behavior of actin stress fibers in myoblasts after nanodissection: effect of oxidative stress. Biorheology 52(3):225–234, 2015.
Marks, J. D., C. Pan, T. Bushell, W. Cromie, and R. C. Lee. Amphiphilic, tri-block copolymers provide potent, membrane-targeted neuroprotection. FASEB J. 15(6):1107–1109, 2001.
Maskarinec, S. A., J. Hannig, R. C. Lee, and K. Y. C. Lee. Direct observation of poloxamer 188 insertion into lipid monolayers. Biophys. J . 82(3):1453–1459, 2002.
McGinley, C., A. Shafat, and A. E. Donnelly. Does antioxidant vitamin supplementation protect against muscle damage? Sports Med. 39(12):1011–1032, 2009.
Merchant, F. A., W. H. Holmes, M. Capelli-Schellpfeffer, R. C. Lee, and M. Toner. Poloxamer 188 enhances functional recovery of lethally heat-shocked fibroblasts. J. Surg. Res. 74(2):131–140, 1998.
Mina, E. W., C. Lasagna-Reeves, C. G. Glabe, and R. Kayed. Poloxamer 188 copolymer membrane sealant rescues toxicity of amyloid oilgomers in vitro. J. Mol. Biol. 390:577–585, 2009.
Moloughney, J. G., and N. Weisleder. Poloxamer 188 (P188) as a membrane resealing reagent in biomedical applications. Recent Pat. Biotechnol. 6(3):200–211, 2012.
Murphy, A. D., M. C. McCormack, D. A. Bichara, J. T. Nguyen, M. A. Randolph, M. T. Watkins, R. C. Lee, and W. G. Austen. poloxamer 188 protects against ischemia–reperfusion injury in a murine hind-limb model. Plast. Reconstr. Surg. 125(6):1651–1660, 2010.
Ng, R., J. M. Metzger, D. R. Claflin, and J. A. Faulkner. Poloxamer 188 reduces the contraction-induced force decline in lumbrical muscles from mdx mice. Am. J. Physiol. Cell Physiol. 295(1):C146–C150, 2008.
Peirce, S. M., T. C. Skalak, and G. T. Rodeheaver. Ischemia–reperfusion injury in chronic pressure ulcer formation: a skin model in rat. Wound Repair Regen. 8(1):68–76, 2000.
Plataki, M., Y. D. Lee, D. L. Rasmussen, and R. D. Hubmayr. Poloxamer 188 facilitates the repair of alveolus resident cells in ventilator-injured lungs. Am. J. Respir. Crit. Med. 184(8):939–947, 2011.
Powers, S. K., and M. J. Jackson. Exercise-induced oxidative stress: cellular mechanisms and impact on muscle force production. Physiol. Rev. 88(4):1243–1276, 2008.
Powers, S. K., A. J. Smuder, and A. R. Judge. Oxidative stress and disuse muscle atrophy: cause or consequence? Curr. Opin. Clin. Nutr. Metab. Care 15(3):240–245, 2012.
Quinlan, J. G., B. L. Wong, R. T. Niemeier, A. S. McCullough, L. Levin, and M. Manuele. Poloxamer 188 failed to prevent exercise-induced membrane breakdown in mdx skeletal muscle fibers. Neuromuscul. Disord. 16(12):855–864, 2006.
Sasaki, M., and T. Joh. Oxidative stress and ischemia–reperfusion injury in gastrointestinal tract and antioxidant, protective agents. J. Clin. Biochem. Nutr. 40(1):1–12, 2007.
Spurney, C. F., A. D. Guerron, Q. Yu, A. Sali, J. H. van der Meulen, E. P. Hoffman, and K. Nagaraju. Membrane sealant poloxamer P188 protects against isoproterenol induced cardiomyopathy in dystrophin deficient mice. BMC Cardiovasc. Disord. 16:11–20, 2011.
Terry, R. L., H. M. Kaneb, and D. J. Wells. Poloxamer 188 has a deleterious effect on dystrophic skeletal muscle function. PLoS One 10(3):e0119252, 2014.
Tidball, J. G. Inflammatory process in muscle injury and repair. Am. J. Physiol. Regul. Integr. Comp. Physiol. 288(2):R345–R353, 2005.
Tsuji, S., S. Ichioka, N. Sekiya, and T. Nakatsuka. Analysis of ischemia–reperfusion injury in a microcirculatory model of pressure ulcer. Wound Repair Regen. 13(2):209–215, 2005.
Walters, T. J., V. J. Mase, J. L. Roe, M. A. Dubick, and R. J. Christy. Poloxamer-188 reduces muscular edema after tourniquet-induced ischemia–reperfusion injury in rats. J. Trauma 70(5):1192–1197, 2011.
Wong, S. W., S. Sun, M. Cho, K. K. H. Lee, and A. F. T. Mak. H2O2 exposure affects myotube stiffness and actin filament polymerization. Ann. Biomed. Eng. 43(5):1178–1188, 2015.
Wu, G., J. Majewski, C. Ege, K. Kjaer, M. J. Weygand, and K. Y. C. Lee. Interaction between lipid monolayers and poloxamer 188: an X-ray reflectivity and diffraction study. Biophys. J. 89(5):3159–3173, 2005.
Yao, Y., Z. Xiao, S. W. Wong, Y. Hsu, T. Cheng, C. Chang, L. Bian, and A. F. T. Mak. The effect of oxidative stress on the compressive damage thresholds of C2C12 mouse myoblasts—implications for deep tissue injury. Ann. Biomed. Eng. 43(2):287–296, 2015.
Yasuda, S., D. Townsend, D. E. Michele, E. G. Favre, S. M. Day, and J. M. Metzger. Dystrophic heart failure blocked by membrane sealant poloxamer. Nature 436(7053):1025–1029, 2005.
Zweier, J. L., and M. A. Talukder. The role of oxidant and free radicals in reperfusion injury. Cardiovasc. Res. 70(2):181–190, 2006.
Acknowledgment
This study was supported by General Research Fund from the Hong Kong Research Grants Council (RGC Ref. No.: CUHK415413).
Author information
Authors and Affiliations
Corresponding author
Additional information
Associate Editor Sean S. Kohles oversaw the review of this article.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Wong, S.W., Yao, Y., Hong, Y. et al. Preventive Effects of Poloxamer 188 on Muscle Cell Damage Mechanics Under Oxidative Stress. Ann Biomed Eng 45, 1083–1092 (2017). https://doi.org/10.1007/s10439-016-1733-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10439-016-1733-0