Abstract
Additive manufacturing, also known as 3D printing, has emerged over the past 3 decades as a disruptive technology for rapid prototyping and manufacturing. Vat polymerization, powder bed fusion, material extrusion, and binder jetting are distinct technologies of additive manufacturing, which have been used in a wide variety of fields, including biomedical research and tissue engineering. The ability to print biocompatible, patient-specific geometries with controlled macro- and micro-pores, and to incorporate cells, drugs and proteins has made 3D-printing ideal for orthopaedic applications, such as bone grafting. Herein, we performed a systematic review examining the fabrication of calcium phosphate (CaP) ceramics by 3D printing, their biocompatibility in vitro, and their bone regenerative potential in vivo, as well as their use in localized delivery of bioactive molecules or cells. Understanding the advantages and limitations of the different 3D printing approaches, CaP materials, and bioactive additives through critical evaluation of in vitro and in vivo evidence of efficacy is essential for developing new classes of bone graft substitutes that can perform as well as autografts and allografts or even surpass the performance of these clinical standards.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Three-dimensional (3D) printing, also known as additive manufacturing, is a digital fabrication process in which geometrical data are used to produce 3D solids by incremental addition of material layers. Charles Hull pioneered the modern idea of 3D printing when he first described a vat polymerization method, known as stereolithography (SL), in a 1984 patent.41 The advent of this new photopolymer-based fabrication technique ushered in the era of rapid and economical production of physical prototypes directly from computer-aided designs, with near limitless geometrical complexity. Originally focused on rapid prototyping of preliminary concept models, advances in materials and technologies are enabling the creation of functional products; and thus, are transitioning these fabrication techniques from prototyping to mainstream manufacturing applications. Beyond vat polymerization, other additive technologies including powder bed fusion, material extrusion, and binder jetting,3 have since been developed, and are discussed in more detail in the following sections.
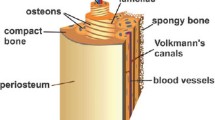
3D printing is being adopted in nearly every industry, including the medical field, with extensive research pursuits focused on novel materials and combinations of techniques that could enhance product functionality and reduce costs. For example, 3D printing an object can enable formation of composites with controlled spatial heterogeneity for superior structure–function relationships that are unachievable with traditional strategies such as machining. This vast potential has made 3D printing extremely popular in the fields of biomedical research and tissue engineering, due to the ability to replicate the intricate architecture as well as the cellular and constituent heterogeneity of tissues and organs.67 Bone, for example, is a complex composite of minerals (mostly calcium phosphates (CaP)) and organic matrix (mostly type I collagen) with exquisite structural organization. This organization spans multiple size scales, such as cortical vs. trabecular bone at the macro-scale and lamellar osteons at the micro-scale. The organization of bone can in theory be imitated using 3D printing. Additionally, 3D printing is amenable to producing patient-specific geometries that are derived from medical images, such as CT scans. This paper systematically reviews progress in 3D printing strategies over the past decade, which have been utilized for bone repair and tissue engineering, with a specific focus on 3D printed pure or composite CaP ceramic scaffolds. The review contrasts the advantages and disadvantages of low-temperature printing vs. high-temperature post-processing for bone tissue engineering applications. It also reviews the state-of-the-art in 3D printed scaffolds for cell and drug delivery in vitro and in vivo in applications involving bone repair and regeneration as well as management of infection.
Three-Dimensional Printing Processes
Vat Polymerization
In the vat polymerization process (e.g., stereolithography), a photo-curable liquid polymer is selectively polymerized at the surface of a vat by a low-power ultraviolet (UV) light source. As the z-axis is translated down, a new thin layer of liquid is spread over the solid surface and this process is repeated until the build is complete (Fig. 1a). Continuous liquid interface production (CLIP) 3D printing has recently been described as an innovative vat polymerization technique that uses UV laser for photocuring and oxygen to create a non-polymerized dead zone to enable the projection of continuous solid objects without the lamination typically seen in standard layer by layer SLA polymerization.84 Some polymers that have been used with vat polymerization for bone tissue engineering applications include poly(propylene fumarate) (PPF)57 and poly(ε-caprolactone fumarate) (PCLF)90 as well as PPF/PCLF blends87 (Table 1). Supplementing these polymers with hydroxyapatite (HA) nanoparticles has been shown to increase the elastic modulus and potentially enhance the osteoconductivity55,58,88 Alternatively, vat polymerization has also been employed to produce complex sacrificial molds for HA scaffolds, which are pyrolyzed before or during sintering of the ceramic.18 The primary advantages of vat polymerization are: (1) the fine resolution that enables interconnected pore diameters and wall thicknesses as small as 100 μm, (2) the tunability of the scaffold stiffness due to the variety of polymers that can be printed and the degree to which crosslinking can be controlled, and (3) the potential for incorporation of bioactive molecules within the polymer.51,56 For bone tissue engineering, vat polymerization is constrained to photo-curable polymers and can be limited in terms of the amounts of ceramic additives.
Powder Bed Fusion
Powder bed fusion (e.g., laser sintering) employs a fine resolution laser or electron beam to achieve selective thermal binding of materials in a layer-by-layer fashion, but unlike liquid photopolymers used in vat polymerization, solid particles from a variety of materials can be bound together by partial or full melting (Fig. 1b). New thin layers of powder are then rolled out over the previous layer and the process is repeated until the build is complete. Materials that have been utilized with these fabrication methods for bone applications include plastics such as poly(ε-caprolactone) (PCL),93 biphasic calcium phosphates,76 polymer/calcium phosphate composites,24,60,95 and titanium alloys85 (Table 1). Although these materials are generally viewed as osteoconductive, they are unable to facilitate complete bone healing without the addition of cells or growth factors. In one study, bone regeneration was enhanced in a rat segmental femoral defect by augmentation of porous titanium scaffolds with growth factor-laden gelatin hydrogels after printing.86 The primary advantage of powder bed fusion is the production of highly detailed, high strength porous scaffolds, which could be used in partial or full load-bearing applications, as in the case of titanium. However, sintering of plastics, ceramics and metals produces localized ultra high temperatures, which preclude the potential for simultaneous incorporation of cells, proteins, or heat-labile bioactive molecules.
Material Extrusion
Material extrusion encompasses any process in which materials are deposited as continuous strands through a nozzle or a dispensing orifice in an incremental layer-by-layer fashion that will yield a 3D product upon solidification of the extruded material (Fig. 1c). A wide variety of material extrusion techniques have been devised and are referred to by an expanding terminology including, but not limited to, 3D (bio)plotting, dispense plotting, or bioprinting which can be used to print bioadditive- and cell-laden hydrogels, to be cross-linked once extruded. In addition extrusion can be achieved by dispensing nearly molten plastic filament through a nozzle (e.g., thermal material extrusion). The material then cools and solidifies into the final 3D form. Material extrusion techniques are the most widely employed 3D printing strategies for tissue engineering, which have led to remarkable progress in the field. This technology has been recently advanced to enable multi-material printing that include cell-laden hydrogels, supporting polymer fibers and sacrificial materials, and has demonstrated the ability to fabricate human-scale tissues of any form including mandible, calvarial bone, cartilage and skeletal muscle.48
With specific focus on bone applications, extrusion-based systems have employed the widest variety of materials using multiple deposition techniques. These materials include synthetic polymers such as polyesters,54,74,75,77 natural polymers such as alginate,69,70 and polymer/ceramic (including bioactive glass) composites30,47,50,54,59,62,73,94,97 (Table 1). While ceramics that are printed by material extrusion often require a secondary heat treatment or sintering, some polymer-based or hybrid scaffolds can be fabricated under mild conditions that are amenable to simultaneous incorporation of growth factors or live cells.69,70,75 The resolution of these techniques depends on the diameter of the dispensing nozzles and the stability of the material after extrusion. Extruded strands commonly have a diameter of 100–200 microns. In some cases, which may depend on the material or geometry, an additional sacrificial support material might be necessary for the scaffolds to maintain form until they can be post-processed.
Binder Jetting
Similar to powder bed fusion, binder jetting selectively binds particulate materials in a layer-by-layer fashion. Instead of fusing the particles with lasers or an electron beam, binder jetting selectively sprays one or more binding solutions from inkjets to unify the particles (Fig. 1d). In bone tissue engineering, the powder phase is most often a CaP, such as tricalcium phosphate (TCP) or hydroxyapatite (HA) (Table 1). The binding solution is usually a sacrificial polymer, which is pyrolyzed during sintering after printing, or an aqueous solution. CaP powders typically require aqueous binding solutions, such as dilute phosphoric acid (in a concentration range of 5–30 wt.%). The acidic binder initiates a dissolution-precipitation reaction within the powder to fuse the particles.35 Typically, a commercial 3D inkjet printer is minimally adapted for printing CaP bone graft substitutes. These printers utilize thermal or piezoelectric inkjet cartridges that are identical to those found in common desktop printers. These ink cartridges can be opened, cleaned, and refilled with the binder solution or bioactive ‘inks’.
The solubility of CaP in the aqueous binder is an important parameter of printability and it depends on its mineral phase as summarized in Table 1. It should be noted that the solubility properties of a given CaP phase can vary depending on synthesis techniques and environmental conditions.25,33 The approximate solubility product constants (K sp) provided in Table 2 indicate equilibrium solubility conditions in a specific chemical system, which is independent of pH and does not represent the absolute dissolution. Solubility isotherms as a function of pH can be better indicators of dissolution and such calculations have been performed for all of the CaP phases listed in Table 1.9,46 Furthermore, mixing CaP with more reactive minerals such as calcium sulfates (CS) has also been shown to improve solubility and binding using aqueous binders, independent of pH.82,99
A comprehensive review of CaP for bone regeneration using fabrication techniques other than 3D printing is beyond the scope of this review, but the interested reader is referred to previous reviews of the topic.6,8,10,16,17 The CaP phase most commonly used in binder jetting is α-TCP, which is more thermodynamically unstable (and thus more soluble) than β-TCP.11 When TCP is combined with phosphoric acid, the dissolution-precipitation reaction yields brushite (CaHPO4·2H2O). Butscher and colleagues demonstrated the superior binder jetting quality and geometrical accuracy of α-TCP vs. β-TCP when using 10% phosphoric acid as the binder solution.12 This study also examined the effects of particle size on printability and observed that when the particle size is too small, flowability is compromised due to agglomeration of the particles, resulting in surface mottling of the powder bed. If the particle size is too large, the powder flows easily but does not pack sufficiently, causing interlayer instability that compromises binding and geometrical accuracy. Powder particles in the size range of 10–50 microns are generally considered optimal.12,43,52,99
Systematic Review of the Literature: Search Algorithm and Inclusion/Exclusion Criteria
The PubMed database was searched on January 5th, 2016 using the string ‘(3D printing OR 3D printed OR rapid prototyping OR additive manufacturing OR inkjet OR granular material binding) AND (bone OR scaffold OR graft) AND (bioceramic OR ceramic OR calcium phosphate)’ to identify articles that investigated the use of 3D-printing to fabricate CaP scaffolds for bone graft substitutes. The search was limited to publications within the last 10 years. Articles in languages other than English were excluded and all reviews were omitted. This search returned 103 results. Studies that utilized 3D-printing, but did not directly involve calcium phosphate in the printing process or bone applications were excluded, as were papers that focused only on optimization or characterization of chemical or mechanical properties of 3D-printed CaP scaffolds with no biological or in vivo assessments. Additional studies that were not returned in the PubMed search, but were identified to be relevant to the topic of this review were included. With this search algorithm and inclusion/exclusion criteria, a total of 45 articles involving in vitro and vivo approaches for bone tissue engineering or drug delivery were fully reviewed and discussed herein, as summarized in Tables 3, 4, 5, 6, and 7. The reviewed papers were broadly categorized into bone regeneration and drug delivery studies in the context of bone repair and infection, which were then further classified into low- and high-temperature 3D printing approaches.
3D Printing for Bone Regeneration
Low Temperature 3D Printing of CaP Scaffolds for Bone Regeneration
Of the papers reviewed in Table 3, the majority used binder jetting approaches, and two studies investigated material extrusion approaches. As described earlier, acidic binder solutions applied to CaP powders in binder jetting enable low temperature binding of the particles in a dissolution-precipitation reaction. In material extrusion, CaP slurries or cements are typically extruded through a non-heated print-head or nozzle under mild conditions, and the extruded materials are then solidified in a variety of ways based on their chemical composition. For example, extruded CaP (composed primarily of α-TCP) paste in a carrier liquid composed of short-chain triglyceride are solidified by placement in water to initiate the cement-setting reaction in just a few minutes, and can be further hardened by incubation at 37 °C for several hours.61 Photocurable hydrogels (poly(ethylene glycol)dimethacrylate (PEGDMA)) with suspended MSCs, bioactive glass (BG), and hydroxyapatite (HA) particles are photo polymerized by UV light.32 Poly(lactic acid) (PLA) (with 5% PEG) polymer blend with BG are cross-linked with NaOH (8% w/v) in 70% ethanol deposited during the 3D printing process and then set by evaporation of the solvent chloroform.2
Regardless of the fabrication method or material, for regenerative applications it is necessary to determine the biocompatibility of the 3D printed scaffold. This is commonly accomplished by seeding cells onto the scaffold and assessing cell viability and proliferation, among a variety of other biological responses.15,32,43,61 Indeed, seeded cells have been shown to attach to a variety of 3D printed scaffolds and achieve a normal cell morphology.43,61,79 In binder jetting, additives to either the binder solution or CaP powder have been shown to affect cell behavior.15,43 For example, Inzana et al. (2014) added solubilized collagen to a phosphoric acid binder solution and observed a significant improvement in relative cell viability (normalized to tissue culture plastic) of C3H/10T1/2 cells seeded onto CaP scaffolds.43 Additionally, Castilho et al. (2015) demonstrated that mixing CaP powder with alginate, enhanced both cell viability and cell proliferation, while vacuum infiltration of alginate into the printed scaffold reduced both cell viability and cell proliferation of the osteoblastic cell line MG63.15 For material extrusion, Lode et al. (2014) showed that human mesenchymal stem cells (hMSCs) attached to a CaP cement scaffold, and the attachment was improved by inducing osteogenic differentiation of hMSCs prior to seeding.61
Low temperature extrusion 3D printing of CaP scaffolds enables direct printing of living cells suspended in ‘bioinks’.32 Investigating the composition of a variety of bioinks consisting of poly(ethylene glycol) dimethacrylate (PEGDMA), BG, HA, and hMSCs Gao et al. (2014) found that cell viability of directly printed hMSCs was highest in pure PEGDMA and PEGDMA-HA bioinks, while PEGDMA-BG had a significantly lower cell viability. The presence of HA in the bioink also led to differentiation towards the osteoblastic lineage. The high resolution (ink drops <0.03 mm diameter) achieved by this material extrusion approach enables precise patterning of cells within the CaP scaffold, which overcomes limitations of post-printing seeding of cells, including reduced cell attachment and inhomogeneous cellular distribution within the porous scaffolds. Mehrban et al. (2013) showed that preconditioning 3D printed CaP scaffolds in acellular and cellular in vitro conditions can help obtain desired physical characteristics for in vivo implementation.65 Morphological changes of 3D printed CaP scaffolds occurred when immersed in culture media over a 28-day period. These changes included an increase in porosity and fluctuations in surface roughness suggesting degradation of the exterior layer of the CaP scaffold. However, the seeding of cells (tenocytes) and the production of ECM on the CaP scaffolds inhibited dissolution and morphological changes.65 Thus, it is important to recognize that not only does the scaffold affect cell function, but the seeded cells can also play an important role in stabilizing the scaffold and controlling its degradation.
When implanted in vivo, scaffolds can elicit a host inflammatory response, but it is not fully understood how this might affect regeneration since inflammation is an important stage in bone repair.38,66,96 Almeida et al. (2014) demonstrated that the immune response of macrophages to 3D printed CaP scaffolds in vitro is sensitive not only to surface properties (i.e., surface chemistry) but also to scaffold geometry (porosity and pore size).2 More research is needed to determine the ideal response and cytokine environment for favorable scaffold-initiated bone regeneration.
3D printed CaP bone graft substitutes fabricated at low temperatures have been shown to be osteoconductive in vivo in a variety of orthotopic implantation models.39,42,43,53 Inzana et al. (2014) showed that binder jetting (inkjet) 3D printed CaP scaffolds with and without incorporated collagen stimulated bone ingrowth and served as osteoconductive spacers in a critically sized murine femoral defect.43 However, CaP-collagen composites did not improve in vivo bone regeneration and complete bridging of the defect. The osteoconductivity of the binder jetting 3D printed TCP scaffolds has been shown to be better than that of HA scaffolds.42 Interestingly, while the size of macropores in 3D printed CaP scaffolds has been shown to affect osteoconductivity and bone regeneration in vivo,42 Habibiovic et al. (2008) reported that pore morphology (open vs. closed macropores of comparable size of 1.3 mm) had no effect on new bone formation in a goat decorticated lumbar implant.39
High Temperature 3D Printing of CaP Scaffolds for Bone Regeneration
The production of CaP scaffolds at high temperatures is necessary for certain 3D printing techniques (i.e., powder bed fusion or thermal material extrusion). Moreover, high temperature post-processing techniques (i.e., heat sintering) applied to 3D printed CaP scaffolds have the primary benefit of enhancing mechanical strength. However, these high temperature limit the ability to incorporate heat-labile biofactors or cells during the fabrication process. This section examines 3D printed CaP scaffolds fabricated or post-processed at high temperatures without incorporated drugs or growth factors. The studies reviewed in Tables 4 and 5 mostly used material extrusion or binder jetting to fabricate pure or composite CaP scaffolds, and assessed their osteogenic potential in vitro or in vivo, and far fewer studies used powder bed fusion or vat polymerization.
CaP scaffolds printed at high temperatures were characterized in vitro to assess biocompatability (Table 4). A wide variety of cells have been used for such characterization, including osteoblasts,7,14,20,24,71,91 preosteoblastic cells,19,49 stromal cells,22,71,98 osteoclasts,21 mesenchymal stem cells (MSCs),68,72 epithelial cells,4 and Schwan cells.80 Cell viability,14,21,22,24,71,80,98 proliferation,14,19,21,22,24,32,40,68,71,72,80,91 and cytotoxicity19,91 assays all show a general consensus of favorable biocompatibility regardless of the 3D printing method using different biomaterials. Furthermore differentiation of MSCs seeded on 3D printed CaP scaffolds into the osteoblastic lineage was only evident when culturing with osteogenic media21,68,71 or an osteoinductive element (e.g., mesoporous glass98). Yet one study demonstrated the ability of HA/TCP scaffolds fabricated by vat polymerization to induce seeded MSCs to differentiate into osteoblast-like cells without osteogenic media as determined by expression of osteogenic markers in vitro and improved calvaria defect repair in vivo.72 Cells not directly involved in the production or resorption of bone have also been seeded and characterized on 3D printed CaP scaffolds to indirectly enhance bone regeneration by supporting innervation and angiogenesis. Sweet et al. (2015) demonstrated that extruding patterned β-TCP composite scaffolds can support the growth of viable Schwann (SC) cells and develop normal nerve-related cell phenotypes and morphologies.80
Castilho et al. (2014) investigated how the composition of CaP (Ca/P ratio) affects biocompatibility, and concluded that biphasic TCP and HA scaffolds produced by binder jetting14 enhanced seeded osteoblasts’ cellular response (viability and proliferation), compared to pure TCP scaffolds. However, Seol et al. (2014) reported that 3D printed HA scaffolds produced from a slurry mixture of ceramic powder with photocurable resin (FA1260T; a urethane acrylate monomer) by vat polymerization, and suggested that these scaffolds promote proliferation of osteoblasts and MSCs, while HA-TCP scaffolds fabricated similarly promote osteoblastic differentiation in vitro.
Almost half of the studies utilizing high temperature 3D printing of CaP scaffolds investigated bone regeneration in vivo (Table 5). The enhanced mechanical properties of CaP scaffolds produced at high temperatures enable them to be structurally sound when orthotopically implanted, especially in load bearing models. Results of these studies showed varying degrees of osteoconductivity for 3D printed CaP scaffolds and collectively conclude that 3D printed CaP scaffolds alone generally do not stimulate bone healing and regeneration compared to autologous bone grafts.81
Osteoinductive dopants or surface modifications were often incorporated pre- or post-fabrication to better enhance the bone regenerative potential of 3D printed CaP scaffolds. Doping 3D printed CaP scaffolds with metal oxides or incorporating additional bioactive materials have been shown to enhance osteoinductivity.29,98 For example, doping raw CaP powder with both SiO2 and ZnO, prior to 3D printing (binder jetting) of CaP scaffolds and post-fabrication sintering at 1250 °C, have been reported to enhance both osteogenic differentiation, as well as neovascularization in a load-bearing rat femoral defect reconstructed with the printed scaffolds.29 CaP scaffolds prepared by material extrusion of β-TCP-PVA slurry and subsequently surface coated with a nanolayer of mesoporous BG and annealed at 650 °C enhanced bone regeneration and angiogenesis in a rabbit calvaria defect model compared to non-coated β-TCP-PVA scaffolds.98 Wang et al. (2014) performed unique post-fabrication modifications to extruded CaP scaffolds, by creating a “virus activated matrix or VAM” wherein RGD-phage nanofibers act as a mimetic ECM for enhanced attachment of endothelial and osteoprogenitor cells, and demonstrated that this approach leads to enhanced vascularization and bone regeneration in a load bearing rat radius defect.89
Cell seeding on 3D printed scaffolds has also been investigated as a strategy for enhancing bone regenerative potential in vivo. For example, Barboni et al. (2013) demonstrated the osteogenic potential of ovine amniotic epithelial cells (oAEC) seeded on a CaP scaffold fabricated by material extrusion of a paste-like aqueous ceramic slurry of HA/β-TCP.4 When implanted in sheep to augment maxillary sinus defects, oAEC-seeding of the 3D printed CaP scaffolds significantly increased bone ingrowth into the defect and accelerated angiogenesis when compared to scaffolds without cells.
3D Printing for Drug Delivery
Low Temperature 3D Printing of CaP Scaffolds for Drug and Growth Factor Delivery
CaP scaffolds produced by binder jetting at low temperature (<37 °C) are theoretically amenable to incorporation of heat-labile bioactive molecules for localized and controlled delivery. These molecules include growth factors to promote angiogenesis and bone regeneration or antibiotics to combat bone infections (Table 6). While it is possible to adsorb growth factors and drugs onto the 3D printed CaP scaffolds after post-processing,5,36,37 the amount of drug adsorption and kinetics of release vary depending on the CaP phase used and the method of drug loading. Regardless, this approach results in burst release of the surface-adsorbed drug within hours and almost consistently fails to sustain release beyond 24 h in vitro. The potential to enable homogeneous volumetric drug loading and to create spatial gradients or site-specific drug localization within a scaffold using 3D printing may offer significant functional advantages over surface adsorption and could dramatically enhance the therapeutic potential of these 3D printed scaffolds. Yet, few studies investigated this approach using low temperature 3D printing and pure CaP scaffolds. In a study by Inzana et al. (2015), volumetric incorporation of antibiotics within 3D printed CaP scaffolds was evaluated as a treatment strategy for implant associated bone infection (osteomyelitis). Cylindrical CaP scaffolds produced by binder jetting incorporated antibiotics either by mixing vancomycin and rifampin directly with phase-pure α-TCP or direct jetting as “bioink” from the color inkjets along with the phosphoric acid binder from the black inkjet cartridge.44 Strategies to control the release kinetics by post-printing coating of the CaP scaffolds with poly (D,L-lactide- co-glycolide) (PLGA) achieved first-order release kinetics, sustained the release over 14 days in vitro and in vivo, and improved flexural biomechanics to values reaching those of dense cancellous bone.44 Interestingly, these CaP scaffolds with incorporated antibiotics significantly reduced the bacterial burden in a mouse model of established femoral osteomyelitis.44
Material extrusion can be more versatile than binder jetting, and when performed under low temperature and mild post-processing conditions it can be amenable to generating drug- or growth factor-loaded composite CaP scaffolds. Mineralized slurry or paste compositions, which can be extruded at physiologic temperature are especially suited for this approach. Martínez-Vázquez et al. (2015) demonstrated the feasibility of 3D printing of porous silicon-doped hydroxyapatite and gelatin (HASi/G) composite scaffolds for delivery of vancomycin.64 These scaffolds behaved as hydrogels, but displayed compressive strength-mineral density relationships that were closer to cancellous than cortical bone, and in general showed a favorable biocompatibility profile in vitro. When loaded with vancomycin, the HASi/G scaffolds achieved first-order diffusive release kinetics, but did not sustain release beyond 10 h in vitro. Furthermore, the incorporation of the antibiotic under the mild scaffold fabrication conditions maintained the drug’s antimicrobial activity in standard in vitro assays.64 Akkineni et al. (2015) described a similar approach of extruding α-TCP-based CaP cement (CPC) premixed with chitosan/dextran sulphate microparticles encapsulating vascular endothelial growth factor (VEGF) or bovine serum albumin (BSA) in a liquid carrier consisting of a biocompatible oil.1 The extruded CPC scaffolds had compressive strength and moduli in the range of the compressive properties of trabecular bone. The bioocompatibility of the scaffolds was demonstrated by the viability and alkaline phosphatase activity of mesenchymal stem cells cultivated on the scaffolds for up 21 days.
While extrusion of CaP composite pastes and hydrogels has the advantage of permitting premixing with drugs and growth factors, this usually means lower printing resolution due to viscosity of these flowable mineralized slurries, which requires large nozzle diameters (>500 microns). The liquid carriers can be organic hydrogels or inorganic carriers, and both require post-processing to allow them to set and harden. Few studies have investigated the performance of 3D printed CaP composites in vivo. Poldervaart et al. (2013) used material extrusion to fabricate composite macroporous alginate scaffolds, which were laden with gelatin microparticles (GMPs) and mesenchymal stem cells.70 The resulting scaffolds had a uniformly distributed array of pores on the order of 500 microns with alginate struts as wide as 2 mm. Due to the viscosity of the composite alginate suspension, concentrations greater than 3% w/v alginate could not be extruded, and this seemed to affect the stability of the printed scaffolds. While this study demonstrates the feasibility of bioprinting CaP composites, and provides one of few examples of in vivo proof of concept, it also highlights the limitations of extrusion based bioprinting; namely the low resolution and the effects of the flowable polymer viscosity on printability.
High Temperature 3D Printing of CaP Scaffolds for Drug and Growth Factor Delivery
High temperature fabrication methods or high temperature post-processing techniques have the primary benefit of enabling CaP ceramics to achieve enhanced mechanical properties. Yet, this methodology hinders the ability to uniformly print cells and/or bioactive molecules. To circumvent this limitation, additional post-processing techniques can be utilized to incorporate biofactors and cells onto the printed construct including surface adsorption or surface modifications, irrespective of the 3D printing technology (Table 7). The most commons additive is BMP-2, which is typically incorporated during the post-processing steps to add an osteoinductive element. For example, Duan et al. (2010) utilized a modified commercial laser sintering (powder bed fusion) system to fabricate composite scaffolds from CaP/poly(hydroxybutyrate-co-hydroxyvalerate) (PHBV) microspheres.23 Rectangular scaffolds with designed macropores of 2 mm evenly patterned throughout the scaffold were fabricated with layer thickness (resolution) of 0.1 mm. This study demonstrated the favorable in vitro biocompatibility of the laser-sintered CaP scaffolds with heparin surface modifications and BMP-2 adsorption, but lacked characterization of drug release release kinetics.
El-Ghannam et al. (2013) adsorbed rhBMP-2 onto sintered silicon doped CaP (SCaP) scaffolds produced by binder jetting and then implanted these scaffolds into a 10 mm rabbit ulna defect.27 Silicon doped CaP has been shown to enhance both the bioactivity and mechanical properties of CaP scaffolds and in combination with rhBMP-2 these CaP scaffolds enabled bone ingrowth, osseointegration, and vascularization.27,28 Strobel et al. (2014) fabricated CaP scaffolds composed of HA, β-TCP, and of an acid-hydrolytic modified potato starch (dextrin) powder using a commercial inkjet 3D-printer with water-glycerol as a binder solution.78 When coated with fibrin premixed with BMP-2 or seeded with osteoblasts, and implanted in subcutaneous pockets in rats, significant ectopic bone formation was observed. One study demonstrated that osteoinductive elements, other than BMP-2 or cells, can be incorporated into 3D-printed CaP scaffolds for enhancing bone formation. Ishack et al. (2015) extruded biphasic CaP (15% HA and 85% β-TCP) in in a colloidal gel ink, and then loaded these scaffolds with either BMP-2 or dipyridamole, a drug that upregulates extracellular adenosine.45 When implanted into a mouse calvarial defect, both BMP-2 and dipyridamole loaded scaffolds promoted bone regeneration 8 weeks post-operatively.
Conclusions
In summary, CaP scaffolds produced using approaches involving low- or high-temperature 3D printing processes or post-processing steps have been shown to be osteoconductive in a variety of animal models; however, complete bone regeneration is typically not achieved without the addition of osteoinductive elements such as cells or biofactors. Future work must focus on refining the right combination of cell populations, growth factors, or other osteoinductive elements needed for complete bone regeneration in orthotopic models of bone regeneration. It is also not known precisely what porosity and pore size distribution are ideal for supporting and enabling bone growth, but this information is vital for optimizing sintering temperatures and duration that affect both mechanical strength and pore morphologies. The advantages of low temperature fabrication approaches are nullified by the poor biomechanical properties of these scaffolds, which makes their use in load-bearing orthotopic models of bone repair challenging. New binders or printing technologies that could improve the mechanical properties of printed CaP scaffolds at biologically-relevant temperatures are an area of research that requires attention. The current 3D printing platforms have limitations intrinsic to the technology used, as described, and future research and development should focus on overcoming these limitations with the goals of enhancing biomechanical properties, resolution, biocompatibility, and sustained drug release that could approach first- or zero-order kinetics. However, an argument can be made that the 3D printing technology has matured to the point where further testing in large animals is required to demonstrate level I preclinical evidence of efficacy.
References
Akkineni, A. R., Y. Luo, M. Schumacher, B. Nies, A. Lode, and M. Gelinsky. 3D plotting of growth factor loaded calcium phosphate cement scaffolds. Acta Biomater. 27:264–274, 2015.
Almeida, C. R., T. Serra, M. I. Oliveira, J. A. Planell, M. A. Barbosa, and M. Navarro. Impact of 3-D printed PLA- and chitosan-based scaffolds on human monocyte/macrophage responses: unraveling the effect of 3-D structures on inflammation. Acta Biomater. 10:613–622, 2014.
ASTM F2792-12a, Standard Terminology for Additive Manufacturing Technologies West Conshohocken, PA, 2012. doi: 10.1520/F2792-12A, http://www.astm.org/.
Barboni, B., C. Mangano, L. Valbonetti, G. Marruchella, P. Berardinelli, A. Martelli, A. Muttini, A. Mauro, R. Bedini, M. Turriani, R. Pecci, D. Nardinocchi, V. L. Zizzari, S. Tete, A. Piattelli, and M. Mattioli. Synthetic bone substitute engineered with amniotic epithelial cells enhances bone regeneration after maxillary sinus augmentation. PLoS One 8:e63256, 2013. doi:10.1371/journal.pone.0063256.
Barralet, J., U. Gbureck, P. Habibovic, E. Vorndran, C. Gerard, and C. J. Doillon. Angiogenesis in calcium phosphate scaffolds by inorganic copper ion release. Tissue Eng. A 15:1601–1609, 2009. doi:10.1089/ten.tea.2007.0370.
Barrere, F., C. A. van Blitterswijk, and K. de Groot. Bone regeneration: molecular and cellular interactions with calcium phosphate ceramics. Int. J. Nanomed. 1:317–332, 2006.
Bergemann, C., M. Cornelsen, A. Quade, T. Laube, M. Schnabelrauch, H. Rebl, V. Weissmann, H. Seitz, and B. Nebe. Continuous cellularization of calcium phosphate hybrid scaffolds induced by plasma polymer activation. Mater. Sci. Eng. C Mater. Biol. Appl. 59:514–523, 2016. doi:10.1016/j.msec.2015.1010.1048.
Black, J., and G. Hastings. Handbook of Biomaterial Properties. New York: Springer, 1998.
Bohner, M. New hydraulic cements based on alpha-tricalcium phosphate-calcium sulfate dihydrate mixtures. Biomaterials 25:741–749, 2004.
Bose, S., and S. Tarafder. Calcium phosphate ceramic systems in growth factor and drug delivery for bone tissue engineering: a review. Acta Biomater. 8(4):1401–1421, 2011.
Brunner, T. J., R. N. Grass, M. Bohner, and W. J. Stark. Effect of particle size, crystal phase and crystallinity on the reactivity of tricalcium phosphate cements for bone reconstruction. J. Mater. Chem. 17:4072, 2007.
Butscher, A., M. Bohner, C. Roth, A. Ernstberger, R. Heuberger, N. Doebelin, P. R. von Rohr, and R. Muller. Printability of calcium phosphate powders for three-dimensional printing of tissue engineering scaffolds. Acta Biomater. 8:373–385, 2012.
Castilho, M., M. Dias, E. Vorndran, U. Gbureck, P. Fernandes, I. Pires, B. Gouveia, H. Armes, E. Pires, and J. Rodrigues. Application of a 3D printed customized implant for canine cruciate ligament treatment by tibial tuberosity advancement. Biofabrication 6:025005, 2014. doi:10.1088/1758-5082/6/2/025005.
Castilho, M., C. Moseke, A. Ewald, U. Gbureck, J. Groll, I. Pires, J. Tessmar, and E. Vorndran. Direct 3D powder printing of biphasic calcium phosphate scaffolds for substitution of complex bone defects. Biofabrication 6:015006, 2014. doi:10.1088/1758-5082/6/1/015006.
Castilho, M., J. Rodrigues, I. Pires, B. Gouveia, M. Pereira, C. Moseke, J. Groll, A. Ewald, and E. Vorndran. Fabrication of individual alginate-TCP scaffolds for bone tissue engineering by means of powder printing. Biofabrication 7:015004, 2015. doi:10.1088/1758-5090/7/1/015004.
Chai, Y. C., A. Carlier, J. Bolander, S. J. Roberts, L. Geris, J. Schrooten, H. Van Oosterwyck, and F. P. Luyten. Current views on calcium phosphate osteogenicity and the translation into effective bone regeneration strategies. Acta Biomater. 8:3876–3887, 2012.
Chow, L. C. Next generation calcium phosphate-based biomaterials. Dent. Mater. J. 28:1–10, 2009.
Chu, T. M., J. W. Halloran, S. J. Hollister, and S. E. Feinberg. Hydroxyapatite implants with designed internal architecture. J. Mater. Sci. Mater. Med. 12:471–478, 2001.
Comesana, R., F. Lusquinos, J. Del Val, F. Quintero, A. Riveiro, M. Boutinguiza, J. R. Jones, R. G. Hill, and J. Pou. Toward smart implant synthesis: bonding bioceramics of different resorbability to match bone growth rates. Sci. Rep. 5:10677, 2015. doi:10.1038/srep10677.
Costa, P. F., C. Vaquette, Q. Zhang, R. L. Reis, S. Ivanovski, and D. W. Hutmacher. Advanced tissue engineering scaffold design for regeneration of the complex hierarchical periodontal structure. J. Clin. Periodontol. 41:283–294, 2014. doi:10.1111/jcpe.12214.
Detsch, R., S. Schaefer, U. Deisinger, G. Ziegler, H. Seitz, and B. Leukers. In vitro: osteoclastic activity studies on surfaces of 3D printed calcium phosphate scaffolds. J. Biomater. Appl. 26:359–380, 2011. doi:10.1177/0885328210373285.
Detsch, R., F. Uhl, U. Deisinger, and G. Ziegler. 3D-Cultivation of bone marrow stromal cells on hydroxyapatite scaffolds fabricated by dispense-plotting and negative mould technique. J. Mater. Sci. Mater. Med. 19:1491–1496, 2008.
Duan, B., and M. Wang. Customized Ca-P/PHBV nanocomposite scaffolds for bone tissue engineering: design, fabrication, surface modification and sustained release of growth factor. J. R. Soc. Interface 7(Suppl 5):S615–S629, 2010.
Duan, B., M. Wang, W. Y. Zhou, W. L. Cheung, Z. Y. Li, and W. W. Lu. Three-dimensional nanocomposite scaffolds fabricated via selective laser sintering for bone tissue engineering. Acta Biomater. 6:4495–4505, 2010. doi:10.1016/j.actbio.2010.4406.4024.
Durucan, C., and P. W. Brown. Reactivity of alpha-tricalcium phosphate. J. Mater. Sci. 37:963–969, 2002.
El-Ghannam, A., L. Cunningham, Jr, D. Pienkowski, and A. Hart. Bone engineering of the rabbit ulna. J. Oral Maxillofac. Surg. 65:1495–1502, 2007.
El-Ghannam, A., A. Hart, D. White, and L. Cunningham. Mechanical properties and cytotoxicity of a resorbable bioactive implant prepared by rapid prototyping technique. J. Biomed. Mater. Res. A 101:2851–2861, 2013.
El-Ghannam, A., C. Q. Ning, and J. Mehta. Cyclosilicate nanocomposite: a novel resorbable bioactive tissue engineering scaffold for BMP and bone-marrow cell delivery. J. Biomed. Mater. Res. A 71:377–390, 2004.
Fielding, G., and S. Bose. SiO2 and ZnO dopants in three-dimensionally printed tricalcium phosphate bone tissue engineering scaffolds enhance osteogenesis and angiogenesis in vivo. Acta Biomater. 9:9137–9148, 2013. doi:10.1016/j.actbio.2013.9107.9009.
Fu, Q., E. Saiz, and A. P. Tomsia. Direct ink writing of highly porous and strong glass scaffolds for load-bearing bone defects repair and regeneration. Acta Biomater. 7:3547–3554, 2011.
Gao, Y., W. L. Cao, X. Y. Wang, Y. D. Gong, J. M. Tian, N. M. Zhao, and X. F. Zhang. Characterization and osteoblast-like cell compatibility of porous scaffolds: bovine hydroxyapatite and novel hydroxyapatite artificial bone. J. Mater. Sci. Mater. Med. 17:815–823, 2006.
Gao, G., A. F. Schilling, T. Yonezawa, J. Wang, G. Dai, and X. Cui. Bioactive nanoparticles stimulate bone tissue formation in bioprinted three-dimensional scaffold and human mesenchymal stem cells. Biotechnol. J. 9:1304–1311, 2014.
Gbureck, U. Mechanical activation and cement formation of β-tricalcium phosphate. Biomaterials 24:4123–4131, 2003.
Gbureck, U., T. Hölzel, C. J. Doillon, F. A. Müller, and J. E. Barralet. Direct printing of bioceramic implants with spatially localized angiogenic factors. Adv. Mater. 19:795–800, 2007.
Gbureck, U., T. Hölzel, U. Klammert, K. Würzler, F. A. Müller, and J. E. Barralet. Resorbable dicalcium phosphate bone substitutes prepared by 3D powder printing. Adv. Funct. Mater. 17:3940–3945, 2007.
Gbureck, U., E. Vorndran, and J. E. Barralet. Modeling vancomycin release kinetics from microporous calcium phosphate ceramics comparing static and dynamic immersion conditions. Acta Biomater. 4:1480–1486, 2008.
Gbureck, U., E. Vorndran, F. A. Muller, and J. E. Barralet. Low temperature direct 3D printed bioceramics and biocomposites as drug release matrices. J. Control Release 122:173–180, 2007.
Gerstenfeld, L. C., T. J. Cho, T. Kon, T. Aizawa, A. Tsay, J. Fitch, G. L. Barnes, D. T. Graves, and T. A. Einhorn. Impaired fracture healing in the absence of TNF-alpha signaling: the role of TNF-alpha in endochondral cartilage resorption. J. Bone Miner. Res. 18:1584–1592, 2003.
Habibovic, P., U. Gbureck, C. J. Doillon, D. C. Bassett, C. A. van Blitterswijk, and J. E. Barralet. Osteoconduction and osteoinduction of low-temperature 3D printed bioceramic implants. Biomaterials 29:944–953, 2008.
He, H. Y., J. Y. Zhang, X. Mi, Y. Hu, and X. Y. Gu. Rapid prototyping for tissue-engineered bone scaffold by 3D printing and biocompatibility study. Int. J. Clin. Exp. Med. 8:11777–11785, 2015.
Hull C. W. Apparatus for production of three-dimensional objects by stereolithography. Google Patents, 1986.
Igawa, K., M. Mochizuki, O. Sugimori, K. Shimizu, K. Yamazawa, H. Kawaguchi, K. Nakamura, T. Takato, R. Nishimura, S. Suzuki, M. Anzai, U. I. Chung, and N. Sasaki. Tailor-made tricalcium phosphate bone implant directly fabricated by a three-dimensional ink-jet printer. J. Artif. Organs 9:234–240, 2006.
Inzana, J. A., D. Olvera, S. M. Fuller, J. P. Kelly, O. A. Graeve, E. M. Schwarz, S. L. Kates, and H. A. Awad. 3D printing of composite calcium phosphate and collagen scaffolds for bone regeneration. Biomaterials 35:4026–4034, 2014. doi:10.1016/j.biomaterials.2014.4001.4064.
Inzana, J. A., R. P. Trombetta, E. M. Schwarz, S. L. Kates, and H. A. Awad. 3D printed bioceramics for dual antibiotic delivery to treat implant-associated bone infection. Eur. Cell Mater. 30:232–247, 2015.
Ishack, S., A. Mediero, T. Wilder, J. L. Ricci, and B. N. Cronstein. Bone regeneration in critical bone defects using three-dimensionally printed beta-tricalcium phosphate/hydroxyapatite scaffolds is enhanced by coating scaffolds with either dipyridamole or BMP-2. J. Biomed. Mater. Res. B Appl. Biomater. 2015. doi:10.1002/jbm.b.33561.
Johnsson, M. S., and G. H. Nancollas. The role of brushite and octacalcium phosphate in apatite formation. Crit. Rev. Oral Biol. Med. 3:61–82, 1992.
Kalita, S. J., S. Bose, H. L. Hosick, and A. Bandyopadhyay. Development of controlled porosity polymer-ceramic composite scaffolds via fused deposition modeling. Mater. Sci. Eng. C 23:611–620, 2003.
Kang, H. W., S. J. Lee, I. K. Ko, C. Kengla, J. J. Yoo, and A. Atala. A 3D bioprinting system to produce human-scale tissue constructs with structural integrity. Nat. Biotechnol. 34(3):312–319, 2016.
Khalyfa, A., S. Vogt, J. Weisser, G. Grimm, A. Rechtenbach, W. Meyer, and M. Schnabelrauch. Development of a new calcium phosphate powder-binder system for the 3D printing of patient specific implants. J. Mater. Sci. Mater. Med. 18:909–916, 2007.
Kim, J., S. McBride, B. Tellis, P. Alvarez-Urena, Y. H. Song, D. D. Dean, V. L. Sylvia, H. Elgendy, J. Ong, and J. O. Hollinger. Rapid-prototyped PLGA/beta-TCP/hydroxyapatite nanocomposite scaffolds in a rabbit femoral defect model. Biofabrication 4:025003, 2012.
Kim, K., A. Yeatts, D. Dean, and J. P. Fisher. Stereolithographic bone scaffold design parameters: osteogenic differentiation and signal expression. Tissue Eng. B Rev. 16:523–539, 2010.
Klammert, U., E. Vorndran, T. Reuther, F. A. Muller, K. Zorn, and U. Gbureck. Low temperature fabrication of magnesium phosphate cement scaffolds by 3D powder printing. J. Mater. Sci. Mater. Med. 21:2947–2953, 2010.
Komlev, V. S., V. K. Popov, A. V. Mironov, A. Y. Fedotov, A. Y. Teterina, I. V. Smirnov, I. Y. Bozo, V. A. Rybko, and R. V. Deev. 3D printing of octacalcium phosphate bone substitutes. Front Bioeng. Biotechnol. 3:81, 2015. doi:10.3389/fbioe.2015.00081.
Lam, C. X., D. W. Hutmacher, J. T. Schantz, M. A. Woodruff, and S. H. Teoh. Evaluation of polycaprolactone scaffold degradation for 6 months in vitro and in vivo. J. Biomed. Mater. Res. A 90:906–919, 2009.
Lee, J. W., G. Ahn, D. S. Kim, and D.-W. Cho. Development of nano- and microscale composite 3D scaffolds using PPF/DEF-HA and micro-stereolithography. Microelectron. Eng. 86:1465–1467, 2009.
Lee, J. W., K. S. Kang, S. H. Lee, J. Y. Kim, B. K. Lee, and D. W. Cho. Bone regeneration using a microstereolithography-produced customized poly(propylene fumarate)/diethyl fumarate photopolymer 3D scaffold incorporating BMP-2 loaded PLGA microspheres. Biomaterials 32:744–752, 2011.
Lee, K. W., S. Wang, B. C. Fox, E. L. Ritman, M. J. Yaszemski, and L. Lu. Poly(propylene fumarate) bone tissue engineering scaffold fabrication using stereolithography: effects of resin formulations and laser parameters. Biomacromolecules 8:1077–1084, 2007.
Lee, K. W., S. Wang, M. J. Yaszemski, and L. Lu. Physical properties and cellular responses to crosslinkable poly(propylene fumarate)/hydroxyapatite nanocomposites. Biomaterials 29:2839–2848, 2008.
Liao, H. T., Y. Y. Chen, Y. T. Lai, M. F. Hsieh, and C. P. Jiang. The osteogenesis of bone marrow stem cells on mPEG-PCL-mPEG/hydroxyapatite composite scaffold via solid freeform fabrication. Biomed. Res. Int. 2014:321549, 2014.
Liao, H. T., M. Y. Lee, W. W. Tsai, H. C. Wang, and W. C. Lu. Osteogenesis of adipose-derived stem cells on polycaprolactone-beta-tricalcium phosphate scaffold fabricated via selective laser sintering and surface coating with collagen type I. J. Tissue Eng. Regen. Med. 2013. doi:10.1002/term.1811.
Lode, A., K. Meissner, Y. Luo, F. Sonntag, S. Glorius, B. Nies, C. Vater, F. Despang, T. Hanke, and M. Gelinsky. Fabrication of porous scaffolds by three-dimensional plotting of a pasty calcium phosphate bone cement under mild conditions. J. Tissue Eng. Regen. Med. 8:682–693, 2014. doi:10.1002/term.1563.
Luo, Y., C. Wu, A. Lode, and M. Gelinsky. Hierarchical mesoporous bioactive glass/alginate composite scaffolds fabricated by three-dimensional plotting for bone tissue engineering. Biofabrication 5:015005, 2013.
Mangano, C., B. Barboni, L. Valbonetti, P. Berardinelli, A. Martelli, A. Muttini, R. Bedini, S. Tete, A. Piattelli, and M. Mattioli. In vivo behavior of a custom-made 3D synthetic bone substitute in sinus augmentation procedures in sheep. J. Oral Implantol. 41:240–250, 2015. doi:10.1563/AAID-JOI-D-1513-00053.
Martinez-Vazquez, F. J., M. V. Cabanas, J. L. Paris, D. Lozano, and M. Vallet-Regi. Fabrication of novel Si-doped hydroxyapatite/gelatine scaffolds by rapid prototyping for drug delivery and bone regeneration. Acta Biomater. 15:200–209, 2015. doi:10.1016/j.actbio.2014.1012.1021.
Mehrban, N., J. Bowen, E. Vorndran, U. Gbureck, and L. M. Grover. Structural changes to resorbable calcium phosphate bioceramic aged in vitro. Colloids Surf. B Biointerfaces 111:469–478, 2013. doi:10.1016/j.colsurfb.2013.1006.1020.
Mountziaris, P. M., P. P. Spicer, F. K. Kasper, and A. G. Mikos. Harnessing and modulating inflammation in strategies for bone regeneration. Tissue Eng. B Rev. 17:393–402, 2011.
Murphy, S. V., and A. Atala. 3D bioprinting of tissues and organs. Nat. Biotechnol. 32:773–785, 2014.
Nandakumar, A., C. Cruz, A. Mentink, Z. Tahmasebi Birgani, L. Moroni, C. van Blitterswijk, and P. Habibovic. Monolithic and assembled polymer-ceramic composites for bone regeneration. Acta Biomater. 9:5708–5717, 2013. doi:10.1016/j.actbio.2012.5710.5044.
Poldervaart, M. T., H. Gremmels, K. van Deventer, J. O. Fledderus, F. C. Oner, M. C. Verhaar, W. J. Dhert, and J. Alblas. Prolonged presence of VEGF promotes vascularization in 3D bioprinted scaffolds with defined architecture. J. Controlled Release 184:58–66, 2014.
Poldervaart, M. T., H. Wang, J. van der Stok, H. Weinans, S. C. Leeuwenburgh, F. C. Oner, W. J. Dhert, and J. Alblas. Sustained release of BMP-2 in bioprinted alginate for osteogenicity in mice and rats. PLoS One 8:e72610, 2013. doi:10.1371/journal.pone.0072610.
Rath, S. N., L. A. Strobel, A. Arkudas, J. P. Beier, A. K. Maier, P. Greil, R. E. Horch, and U. Kneser. Osteoinduction and survival of osteoblasts and bone-marrow stromal cells in 3D biphasic calcium phosphate scaffolds under static and dynamic culture conditions. J. Cell Mol. Med. 16:2350–2361, 2012.
Seol, Y. J., J. Y. Park, J. W. Jung, J. Jang, R. Girdhari, S. W. Kim, and D. W. Cho. Improvement of bone regeneration capability of ceramic scaffolds by accelerated release of their calcium ions. Tissue Eng. A 20:2840–2849, 2014. doi:10.1089/ten.TEA.2012.0726.
Serra, T., J. A. Planell, and M. Navarro. High-resolution PLA-based composite scaffolds via 3-D printing technology. Acta Biomater. 9:5521–5530, 2013.
Seyednejad, H., D. Gawlitta, R. V. Kuiper, A. de Bruin, C. F. van Nostrum, T. Vermonden, W. J. Dhert, and W. E. Hennink. In vivo biocompatibility and biodegradation of 3D-printed porous scaffolds based on a hydroxyl-functionalized poly(epsilon-caprolactone). Biomaterials 33:4309–4318, 2012.
Shim, J. H., S. E. Kim, J. Y. Park, J. Kundu, S. W. Kim, S. S. Kang, and D. W. Cho. Three-dimensional printing of rhBMP-2-loaded scaffolds with long-term delivery for enhanced bone regeneration in a rabbit diaphyseal defect. Tissue Eng. A 20:1980–1992, 2014.
Shuai, C., P. Li, J. Liu, and S. Peng. Optimization of TCP/HAP ratio for better properties of calcium phosphate scaffold via selective laser sintering. Mater. Charact. 77:23–31, 2013.
Sobral, J. M., S. G. Caridade, R. A. Sousa, J. F. Mano, and R. L. Reis. Three-dimensional plotted scaffolds with controlled pore size gradients: effect of scaffold geometry on mechanical performance and cell seeding efficiency. Acta Biomater. 7:1009–1018, 2011.
Strobel, L. A., S. N. Rath, A. K. Maier, J. P. Beier, A. Arkudas, P. Greil, R. E. Horch, and U. Kneser. Induction of bone formation in biphasic calcium phosphate scaffolds by bone morphogenetic protein-2 and primary osteoblasts. J. Tissue Eng. Regen. Med. 8:176–185, 2014. doi:10.1002/term.1511.
Suwanprateeb, J., W. Suvannapruk, and K. Wasoontararat. Low temperature preparation of calcium phosphate structure via phosphorization of 3D-printed calcium sulfate hemihydrate based material. J. Mater. Sci. Mater. Med. 21:419–429, 2010. doi:10.1007/s10856-10009-13883-10851.
Sweet, L., Y. Kang, C. Czisch, L. Witek, Y. Shi, J. Smay, G. W. Plant, and Y. Yang. Geometrical versus random beta-TCP scaffolds: exploring the effects on Schwann Cell growth and behavior. PLoS One 10:e0139820, 2015. doi:10.1371/journal.pone.0139820.
Tamimi, F., J. Torres, K. Al-Abedalla, E. Lopez-Cabarcos, M. H. Alkhraisat, D. C. Bassett, U. Gbureck, and J. E. Barralet. Osseointegration of dental implants in 3D-printed synthetic onlay grafts customized according to bone metabolic activity in recipient site. Biomaterials 35:5436–5445, 2014. doi:10.1016/j.biomaterials.2014.5403.5050.
Thomas, M. V., and D. A. Puleo. Calcium sulfate: properties and clinical applications. J. Biomed. Mater. Res. B Appl. Biomater. 88:597–610, 2009.
Torres, J., F. Tamimi, M. H. Alkhraisat, J. C. Prados-Frutos, E. Rastikerdar, U. Gbureck, J. E. Barralet, and E. Lopez-Cabarcos. Vertical bone augmentation with 3D-synthetic monetite blocks in the rabbit calvaria. J. Clin. Periodontol. 38:1147–1153, 2011. doi:10.1111/j.1600-1051X.2011.01787.x.
Tumbleston, J. R., D. Shirvanyants, N. Ermoshkin, R. Janusziewicz, A. R. Johnson, D. Kelly, K. Chen, R. Pinschmidt, J. P. Rolland, A. Ermoshkin, E. T. Samulski, and J. M. DeSimone. Additive manufacturing. Continuous liquid interface production of 3D objects. Science 347:1349–1352, 2015.
Van der Stok, J., O. P. Van der Jagt, S. Amin Yavari, M. F. De Haas, J. H. Waarsing, H. Jahr, E. M. Van Lieshout, P. Patka, J. A. Verhaar, A. A. Zadpoor, and H. Weinans. Selective laser melting-produced porous titanium scaffolds regenerate bone in critical size cortical bone defects. J. Orthop. Res. 31:792–799, 2013.
van der Stok, J., H. Wang, S. Amin Yavari, M. Siebelt, M. Sandker, J. H. Waarsing, J. A. Verhaar, H. Jahr, A. A. Zadpoor, S. C. Leeuwenburgh, and H. Weinans. Enhanced bone regeneration of cortical segmental bone defects using porous titanium scaffolds incorporated with colloidal gelatin gels for time- and dose-controlled delivery of dual growth factors. Tissue Eng. A 19:2605–2614, 2013.
Wang, S., D. H. Kempen, N. K. Simha, J. L. Lewis, A. J. Windebank, M. J. Yaszemski, and L. Lu. Photo-cross-linked hybrid polymer networks consisting of poly(propylene fumarate) and poly(caprolactone fumarate): controlled physical properties and regulated bone and nerve cell responses. Biomacromolecules 9:1229–1241, 2008.
Wang, S., D. H. Kempen, M. J. Yaszemski, and L. Lu. The roles of matrix polymer crystallinity and hydroxyapatite nanoparticles in modulating material properties of photo-crosslinked composites and bone marrow stromal cell responses. Biomaterials 30:3359–3370, 2009.
Wang, J., M. Yang, Y. Zhu, L. Wang, A. P. Tomsia, and C. Mao. Phage nanofibers induce vascularized osteogenesis in 3D printed bone scaffolds. Adv. Mater. 26:4961–4966, 2014. doi:10.1002/adma.201400154.
Wang, S., M. J. Yaszemski, J. A. Gruetzmacher, and L. Lu. Photo-crosslinked poly(epsilon-caprolactone fumarate) networks: roles of crystallinity and crosslinking density in determining mechanical properties. Polymer (Guildf) 49:5692–5699, 2008.
Warnke, P. H., H. Seitz, F. Warnke, S. T. Becker, S. Sivananthan, E. Sherry, Q. Liu, J. Wiltfang, and T. Douglas. Ceramic scaffolds produced by computer-assisted 3D printing and sintering: characterization and biocompatibility investigations. J. Biomed. Mater. Res. B Appl. Biomater. 93:212–217, 2010. doi:10.1002/jbm.b.31577.
Will, J., R. Melcher, C. Treul, N. Travitzky, U. Kneser, E. Polykandriotis, R. Horch, and P. Greil. Porous ceramic bone scaffolds for vascularized bone tissue regeneration. J. Mater. Sci. Mater. Med. 19:2781–2790, 2008. doi:10.1007/s10856-10007-13346-10855.
Williams, J. M., A. Adewunmi, R. M. Schek, C. L. Flanagan, P. H. Krebsbach, S. E. Feinberg, S. J. Hollister, and S. Das. Bone tissue engineering using polycaprolactone scaffolds fabricated via selective laser sintering. Biomaterials 26:4817–4827, 2005.
Wu, C., Y. Luo, G. Cuniberti, Y. Xiao, and M. Gelinsky. Three-dimensional printing of hierarchical and tough mesoporous bioactive glass scaffolds with a controllable pore architecture, excellent mechanical strength and mineralization ability. Acta Biomater. 7:2644–2650, 2011.
Xia, Y., P. Zhou, X. Cheng, Y. Xie, C. Liang, C. Li, and S. Xu. Selective laser sintering fabrication of nano-hydroxyapatite/poly-epsilon-caprolactone scaffolds for bone tissue engineering applications. Int. J. Nanomed. 8:4197–4213, 2013.
Yang, X., B. F. Ricciardi, A. Hernandez-Soria, Y. Shi, N. Pleshko Camacho, and M. P. Bostrom. Callus mineralization and maturation are delayed during fracture healing in interleukin-6 knockout mice. Bone 41:928–936, 2007.
Yang, S., J. Wang, L. Tang, H. Ao, H. Tan, T. Tang, and C. Liu. Mesoporous bioactive glass doped-poly (3-hydroxybutyrate-co-3-hydroxyhexanoate) composite scaffolds with 3-dimensionally hierarchical pore networks for bone regeneration. Colloids Surf. B Biointerfaces 116:72–80, 2014.
Zhang, Y., L. Xia, D. Zhai, M. Shi, Y. Luo, C. Feng, B. Fang, J. Yin, J. Chang, and C. Wu. Mesoporous bioactive glass nanolayer-functionalized 3D-printed scaffolds for accelerating osteogenesis and angiogenesis. Nanoscale 7:19207–19221, 2015. doi:10.11039/c19205nr05421d.
Zhou, Z., F. Buchanan, C. Mitchell, and N. Dunne. Printability of calcium phosphate: calcium sulfate powders for the application of tissue engineered bone scaffolds using the 3D printing technique. Mater. Sci. Eng. C Mater. Biol. Appl. 38:1–10, 2014.
Acknowledgments
This research was supported by grants from the AO Trauma Research Institute - Clinical Priority Program on Bone Infection and the National Institutes of Health (NIH P30 AR061307 and R34 DE025573). Jason Inzana was supported in part by a Whitaker International Program post-doctoral scholarship and a National Science Foundation graduate research fellowship (NSF Award DGE-1419118). The content is solely the responsibility of the authors and does not necessarily represent the official views of AO Trauma, NIH, NSF, or the Whitaker International Program.
Author information
Authors and Affiliations
Corresponding author
Additional information
Associate Editor Amir Abbas Zadpoor oversaw the review of this article.
Rights and permissions
About this article
Cite this article
Trombetta, R., Inzana, J.A., Schwarz, E.M. et al. 3D Printing of Calcium Phosphate Ceramics for Bone Tissue Engineering and Drug Delivery. Ann Biomed Eng 45, 23–44 (2017). https://doi.org/10.1007/s10439-016-1678-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10439-016-1678-3