Abstract
The engineering of technologies for heart valve replacement (i.e., heart valve engineering) is an exciting and evolving field. Since the first valve replacement, technology has progressed by leaps and bounds. Innovations emerge frequently and supply patients and physicians with new, increasingly efficacious and less invasive treatment options. As much as any other field in medicine the treatment of heart valve disease has experienced a renaissance in the last 10 years. Here we review the currently available technologies and future options in the surgical and transcatheter treatment of aortic valve disease. Different valves from major manufacturers are described in details with their applications.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Severe heart valve disease and its sequelae lead to significant morbidity and mortality. Ross and Braunwald in a seminal paper from 1968 demonstrated the natural history of aortic stenosis, which is manifested by a long presymptomatic period followed by complications and short survival times after the onset of symptoms.71 The prevalence and incidence of heart valve disease have continued to rise as life expectancy increases and the population ages.15 Treating severe valve disease and the associated symptoms drives innovation with the ultimate goal of improving patients’ life expectancy and quality of life. While challenging, this ever-changing field has made significant improvements since the first replacement valves were developed in the 1950s.55 The current surgical and transcatheter treatments, while still not ideal, have given patients hope that they can live for an extended period with a disease that previously had very poor outcomes. For instance, a patient who as recently as 10 years ago may have had a prohibitive risk of surgery can now have a transcatheter aortic valve replacement (TAVR) and enjoy the benefits of treatment they otherwise would have been denied. This has resulted in more than 80,000 valve replacements utilizing bioprosthetic valves or mechanical valves per year in the United States alone, and more than 300,000 worldwide.68 , 74 In addition, since 2002, there have also been over 50,000 TAVR procedures performed worldwide.68
Many of the mechanisms involved in the pathophysiology and progression of valve disease are not completely understood, making development of medical therapies difficult. Surgical procedures are the most effective treatment for diseased valves. In fact, surgical intervention is associated with a significant survival benefit and a relatively low perioperative mortality and morbidity, even for elderly patients above 80 years of age.76 Several different types of replacement valves have been developed and continue to evolve in order to be more durable and less invasive. These include mechanical, bioprosthetic, and transcatheter replacement valves currently manufactured by Edwards Lifesciences, Medtronic, St. Jude Medical, Sorin Group, Boston Scientific, and others. Transcatheter valves are currently only recommended for non-operative or high risk patients in the U.S., but require a less invasive procedure as they can be delivered through a minimally-invasive procedure that many can undergo in the absence of general anesthesia. In this portion of a four part review series we discuss with great breadth, the currently available options in the surgical and transcatheter treatment of aortic valve disease. Different valves from major manufacturers are described in detail with the applications for each. Part I of the series reviewed the future directions for heart valve replacement including, but not limited to, tissue engineered and polymeric heart valves. Part III of the series focused on the repair and replacement options for the mitral valve. Finally, part IV is a focused review of advanced computation modeling of and experimental testing of heart valves.
Mechanical Heart Valves
Mechanical heart valves were first designed in the 1950s as a ball-and-cage valve based on the bottle stoppers from the 1800s. The first ever artificial valve approved by the FDA was the Starr-Edwards valve designed by Miles Lowell Edwards, a hydraulics engineer, and Albert Starr, a cardiovascular surgeon.55 This valve was successfully implanted in a human in 1960, and while revolutionary, due to its design, it has high transvalvular gradients in smaller sizes that disrupt hemodynamics and the patient requires lifetime anticoagulation. Although the ball-and-cage valve is not used today because of its shortcomings,62 mechanical valve technology has improved, by leaps and bounds, and still provides the patient with a durable valve that rarely has mechanical failure. In fact, according to the Society of Thoracic Surgeons adult cardiac surgery database, mechanical valves were implanted into 34% of all patients 30 years of age or younger undergoing aortic valve surgery.13 While the use of mechanical valves has been declining in recent years due to the increasing popularity of bioprosthetic surgical and transcatheter valves,60 due to their durability, mechanical valves are and will continue to be commonly implanted, for the foreseeable future.
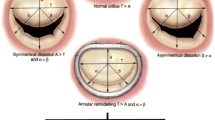
Mechanical valves come in a variety of shapes, sizes, and materials.19 Currently, mechanical aortic valves typically have a bileaflet design consisting of a sewing ring surrounding two semicircular disks (Fig. 1). Bileaflet design has largely replaced monoleaflet valves which are composed a single disk with lateral or central securing struts that allow the disk to open and result in two distinct orifices of different sizes. Pyrolytic carbon, a material similar to graphite, is used for the disks due to its resistance to thrombosis. Here, we summarize the characteristics, studies and future directions of the currently available mechanical aortic valves organized by the manufacturer.
The aortic line of Medtronic mechanical valves consists of the Open Pivot valves, which include the Open Pivot standard aortic valve and Open Pivot AP both of which are also available for implantation in the mitral position. Medtronic also offers the Open Pivot AP360 which is solely for use in the aortic position. AP360 provides a supra-annular flanged cuff for added flexibility and conformability in addition to the features of the other open pivot valves. In general, the purpose of the open pivot as opposed to a cavity pivot is to attempt reducing the nidus for thrombus formation created by a cavity pivot.27 There is a continuous passive washing through an unimpeded flow of blood, which minimizes hemolysis and is considered a secondary mechanism to minimize thrombus formation.45 Excellent hemodynamics, durability, and ease of implantation are felt to be strengths of the Medtronic mechanical valves.28 , 80 Medtronic mechanical aortic valves come in annular sizes that range from 16 to 26 mm.
Most mechanical valves have been implanted in a large volume of patients with significant follow up data, and the Medtronic valves are no exception. A recent publication from a single center in Belgium followed all patients with an Open Pivot valve implanted over a 20 year period.81 In total, 1520 Open Pivot valves were implanted in 1382 consecutive patients with a 99% rate of follow-up. When implanted in the aortic position there were only five documented cases of valve thrombosis and nearly 90% of patients were free of thromboembolism at 240 months. There were no documented cases of structural valve deterioration. Another study from Australia used the Open Pivot valve as part of a conduit for aortic root replacement, and included 246 patients.58 The Open Pivot was found to be a safe and durable option for root replacement and the patients had a 10 year survival of 79%.
Finally, the in vitro studies of the Open Pivot have been compared to valves with a single tilting disk and those with a recessed hinge mechanism to determine if not only does the valve improve hemodynamics, but also prevent thrombus formation. When compared to a single tilting disk, investigators found improved pressure drop characteristics with the Open Pivot valves, and thus a small, but significant improvement in overall fluid dynamic performance.58 Open Pivot compared to a recessed hinge was shown in computational studies to provide more exposure of the hinges to the mainstream laminar flow for a positive washing effect.83 This is of course a computational result and cannot directly infer a lower rate of thrombus, but is encouraging.
St. Jude Medical’s mechanical aortic valve product line consists of the Masters HP Series which can also be used in the mitral position. In addition, St. Jude Medical produces the Regent aortic valve; a supra-annular valve that delivers baseline gradients in the single digits, even in valve sizes as small as 19 mm.6 First implanted in 1977, the Masters Series is still used today, and offers excellent durability with a reasonable flow profile.50 Incremental improvements aimed at ease of implantation,77 hemodynamic performance, effective orifice area, and pressure gradients have been made over the years.94 With the Regent, St. Jude touts improved hemodynamics over the older valve designs and provides more laminar flow.9 Annular sizes covered by the Regent are 19–27 mm, with either a standard sewing cuff or a FlexCuff model.
Given the longevity of the St. Jude valves availability, there has been a great number of clinical and hemodynamic studies conducted on these valves. The most recent work has been centered on the use of the Regent valve in those with small aortic annuli. Most studies are single center but have shown promising results. For instance, a study published this year in patients with severe AS, using a 17 mm Regent valve showed that not only did patients have a significant reduction in New York Heart Association (NYHA) Functional Class, but significant reductions in LV mass index despite the small valve size.65 The investigators drew the conclusion that this valve was an excellent option for those with a small aortic annulus. Hemodynamic studies of the valve have been both in vivo, in vitro and computational. In one study, in vivo hemodynamics was assessed in patients several years after surgery by imaging at rest and under dobutamine stress.61 Under considerable increases in hemodynamic stress, there was an expected increase in transvalvular gradient, but no decreased in effective orifice area. Clinical follow-up was also provided and no cases of structural failure were reported. Simulated studies on flow through the Regent valve and its effect on platelet activation showed that the Regent valve had a favorable flow field that did not activate platelets in the simulation.87
Sorin Group (Sorin Biomedica Cardio S.p.A., Saluggia, Italy) offers several mechanical aortic valves under its Carbomedics line. The Carbomedics aortic valves include the Carbomedics Standard aortic valve, a standard pediatric aortic valve, the Carbomedics Top Hat, the Carbomedics Reduced Series and the Carbomedics Orbis. In addition, there is a Bicarbon line, which is encompassed by the Bicarbon Fitline, Bicarbon Overline and Bicarbon Slimline. Carbomedics aortic valves generally have a low rate of thromboembolism, when compared with other mechanical valves, as is found with their sister Carbomedics mitral valves.16
When directly compared to the ATS (now Medtronic) AP, the On-X and St. Jude Regent, through in vitro testing, Bottio et al. 12 found that the Bicarbon Slimline and the St. Jude Regent had significantly lower baseline gradients when placed in a small aortic annulus (i.e., 21 mm). Additionally, the Bicarbon line has been shown to have a larger effective orifice area compared to the other valves.32 The Fitline is intra-annular and comes in sizes from 19 to 31 mm, the Overline is supra-annular and is sized from 16 to 24 mm, and finally the Slimline is supra-annular and available from 17 to 27 mm.
There is also a large volume of clinical follow-up with Sorin valves. A group in Italy recently published 17 year follow-up from a cohort of 507 patients with Sorin mechanical valves.17 This study found that only five patients required re-operation, which accounted to 0.08% patient-years, and there were a total of 15 valve related deaths in the subset of patients who had an aortic valve replacement.17 Another study from Spain demonstrated that that patients with Sorin Bicarbon used for their aortic valve had over a 93% event free survival at 24 months.67 Overall, Sorin mechanical valves have been consistently shown to have excellent in vitro functionality and favorable clinical outcomes.
On-X Life Technologies (Austin, TX, USA) produces a line of aortic valves that differ based on their sewing ring. The aortic valves come with three available sewing rings as opposed to two as with their mitral valves. There is a standard ring, a conform-x ring, and an anatomic ring. Durability and low rates of thromboembolism are claimed advantages of the On-X aortic valves. Annular sizes available range from 19 to 29 mm. Also available is an Ascending Aortic Prosthesis in the same size range. The valves offer several features that On-X touts which include pure carbon coatings to limit platelet activation, longer axial valves to improve hemodynamics, a flared inlet orifice to reduce turbulent flow, full 90° leaflet opening, and “soft landing” two point closure. Finally, On-X uses an actuated pivot design that they promote as being stasis free and non-hemolytic. This is accomplished by introducing flow paths between the leaflet and pivot wall. Efforts to model the ideal hinge, may sound less critical, but are in fact paramount to the development of durable mechanical valves with a low rate of hemolysis and thrombus formation.
While in many occasions valve manufacturers promote novel features of their valves without concrete evidence, the novel features of the On-X valves to reduce thrombus formation were studied in the Prospective Randomized On-X Anticoagulation Clinical Trial (PROCAT).66 In PROCAT, a prospective randomized control trial, 375 patients underwent AVR with an On-X valve and were assigned to control (INR 2-3 and ASA 81 mg daily) and test (INR 1.5–2 after 3 months and ASA 81 mg daily) groups. The test group patients had a significantly lower rate of major and minor bleeding while having no significant increase in death, stroke or TIA.66 Clinical data from a 12 year follow-up of 691 patients after On-X mechanical valve replacement in England showed a thrombosis rate of 0% in the aortic subset with a reoperation rate of 0.2% and a mortality of only 2.2%.18
Regardless of the type of mechanical valve implanted, lifelong anti-coagulation therapy with a vitamin K antagonist (VKA, i.e., warfarin) is still nearly universally prescribed for patients who can tolerate this therapy, which in turn, increases the risk of major bleeding complications such as hemorrhagic stroke.36 This increased risk of bleeding limits a patient’s ability to participate in activities that have an increased risk of traumatic injury. The 2014 AHA/ACC guidelines for the management of patients with valvular heart disease contain the anticoagulation protocols for those with mechanical valves.59 Class I recommendations in AVR are for anticoagulation with a VKA to achieve an international normalized ratio (INR) of 2.5, regardless of the mechanical valve manufacturer, if no risk factors for thromboembolism exist. If risk factors for thromboembolism exist, then the goal INR is 3 for those with a mechanical AVR. The addition of ASA 75–100 mg daily is also recommended in addition to a VKA. Of note, the results of the previously discussed PROCAT study have not yet been incorporated into the guidelines.
Mechanical valves are indicated in younger patients in whom a durable valve that can last decades is desirable. This decision must also be accompanied by the assessment of the patient’s ability to tolerate anticoagulation. As discussed previously, lifelong treatment with VKA can lead to significant bleeding complications. Ultimately, the durability of mechanical valves is the primary advantage over bioprosthetic valves where leaflet deterioration is a much greater issue. Bioprosthetic valves provide a flow profile that is more physiologic and do not require long term anticoagulation.
Optimizing the design of mechanical valves to improve flow profiles and minimize valve related complications, is achieved through both computational and experimental techniques. As previously discussed, the hinge points promote a complex and unsteady flow which in turn results in stagnation and thrombus formation.43 Reducing the potential for thrombus formation through the redesign of hinges is an active area of research. For instance, computational fluid dynamics (CFD) is used to study flow through physiologic 3D geometries before and after virtual valve implantation.2 , 23 , 92 Additional uses of CFD are the estimation of the thrombogenicity of devices based on their geometry. This is achieved in combination with experimental approaches by examining the effect of distinct flow phases on platelet activation.88 Particle image velocimetry is another in vitro technique that can be used to study systolic and diastolic flow of regurgitant jets,29 , 34 valve orifices,30 and at the leaflet insertion hinges.43 More information on computational and experimental valve studies are provided in Part IV of this review series.
Pre-clinical valve optimization is difficult due to the complex flow across the valve that includes areas of high velocity and viscous shearing, which may in turn cause platelet activation and hemolysis. This is contrasted with areas of the valve that promote thrombus formation due to low flow velocities and resultant increased residence times. An additional manner through which to reduce thrombus formation is the development of surface coatings that resist platelet activation. One relatively new technique utilizes a polymerization process that uses horseradish peroxidase (HRP) as a catalyst to make hydrophilic polymers needed for a non-adhesive outer coating.8 Biocompatible flow chambers used to simulate the ex vivo performance and response of mechanical and bioprosthetic valves may also prove to be a significant development; however, they have yet to be fully optimized.91
A newer mechanical heart valve design utilizes three pyrolytic carbon leaflets and may more closely mimic the hemodynamic properties of native tissue as it has a greater effective orifice area in comparison to a similar bileaflet valve (Fig. 2). This three-leaflet configuration minimizes flow separation and provides a soft closure mechanism, similar to the natural aortic valve, with minimal regurgitation. The trileaflet design has been shown in some studies to reduce outflow tract obstruction, myocardial hypertrophy, and increase blood compatibility.35 , 73 CFD results showed that only 0.7% of the blood volume moving through a trileaflet valve was exposed to shear rates high enough to cause platelet activation.44 Despite these potential advantages, this valve has never been used clinically even though it was developed over a decade ago. Further optimization of mechanical valves to limit thrombosis may provide younger patients with a durable prosthetic valve that has a significantly reduced need for anti-thrombotic medication.
A trileaflet mechanical heart valve provides flow characteristics that more closely mimic native aortic valves. The valve contains a pivot mechanism that allows airfoil-like leaflets to close before flow reverses, a phenomenon that also occurs in the body. (a) Valve from above in fully open position. (b) Elevated isometric view of the valve in a fully open position. (c) Disassembled valve with three pyrolytic carbon leaflets and ring. Images are courtesy of Ulrich Steinseifer, Helmholtz Institute, Aachen, Germany
With the continued evolution of the mechanical heart valve field to optimize hinge design, improve hemodynamics, and develop new surface coatings, it is likely that the valves will incrementally improve as they have over the last decade. Tools such as CFD, particle image velocimetry,29 and echocardiography48 will aid in this process and perhaps improve the pre-clinical evaluation of valves. Additionally, advances in surface coatings to reduce platelet activation, thrombus formation, and protein aggregation will be important. However, with concurrent advances in bioprosthetic valves, mechanical valves will likely continue to primarily be used in younger patients, and not see significant expansion in their use.
Bioprosthetic Heart Valves
Bioprosthetic heart valves are designed to mimic the anatomy of the native aortic valve through the use of a trileaflet valve.63 Composed of either three porcine valve leaflets cross linked with glutaraldehyde or bovine pericardium. By utilizing a more flexible and biocompatible surface results in improved blood flow dynamics to reduce platelet activation, minimize red blood cell damage, reduce thrombus formation and thus mitigate the need for anticoagulation. The main concern for patients when a bioprosthetic heart valve is chosen is degeneration that results in clinical symptoms or the need for reoperation. Bioprosthetic valves require replacement within 10 years in 30% of patients and within 15 years in 50% of patients, and this process is accelerated in those who are young and in pregnant patients.89 Bioprosthetic valves are becoming more durable as the techniques in stent design and fixative methods improve. A bioprosthetic valve with the durability of a mechanical valve is unlikely to exist anytime in the near future; however, progress is being made and the rapid progress in transcatheter valve technology, which use pericardial leaflets, will likely drive innovation. Here, we provide an overview of the currently available bioprosthetic aortic valves.
Edwards Lifesciences has the largest product line of bioprosthetic aortic valves. Sharing the same product line name as their mitral valves, the bovine pericardial Carpentier-Edwards PERIMOUNT™ Aortic valves offer excellent hemodynamics and durability.54 This line consists of the PERIMOUNT™ Magna Ease Aortic Valve, Magna Aortic Valve, Standard Aortic Valve and Theon Aortic Valve. Additional aortic valves offered by Edwards are the Carpentier-Edwards Aortic Porcine, S.A.V. Aortic Porcine and the Edwards Prima Plus Stentless Bioprosthesis. Bovine pericardial valves from Edwards are treated with their ThermaFix process, which is a dual-action treatment aimed at reducing the potential calcium binding sites to improve long term valve performance.74 Porcine aortic valves produced by Edwards are treated with the patented XenoLogiX treatment which has shown to result in low rates of calcification.22 The bovine pericardial Carpentier-Edwards PERIMOUNT™, which is the second generation line of valves, show excellent durability compared to the first generation pericardial valves (Fig. 3).54 Structural valve deterioration in elderly patients, occurs at low enough rate to result in an extremely low rate of reoperation.54 The Prima Plus Stentless Porcine Bioprosthesis is a biograft, a bioprosthesis plus homograft that has exhibited excellent long-term outcomes and maintains optimal hemodynamics.22 , 42
Due to the popularity of Edwards’ aortic valves, and the fact that the entire aortic pericardial portfolio is built on the PERIMOUNT design, there is a large volume of clinical follow-up on patients in whom Edwards’ valves have been implanted. One large study from France followed 1133 patients who over 18 years had a valve from the PERIMOUNT family in their aortic position.4 Patients were followed for an average of 5.5 years and only 19 structural valve failures were reported along with the reported data that in patients over 60 years of age 85% remained free from valve failure.4 A Canadian group directly compared the hemodynamics of the PERIMOUNT Magna valve to the Hancock II valve from Medtronic 1 week postoperatively in matched controls.11 The Magna valves had significantly lower peak and mean transvavlular gradients in addition to a much lower rate of patient-prosthesis mismatch (30 vs. 52%, p = 0.02).11
Medtronic produces the Hancock II and Mosaic line of stented porcine bioprosthetic valves that are implantable in the aortic and mitral positions. The Hancock II demonstrates very low rates of structural deterioration and overall low amount of valve related complications (Fig. 3).10 , 79 Similar to the other bioprosthetic valves, the hemodynamics are vastly improved over those of mechanical valves.10 In addition to the Hancock II there is a Hancock II Ultra with a reduced sewing cuff that is specifically designed for implantation in a small aortic root. Mosaic and Mosaic Ultra are the second line of bioprosthesis available from Medtronic. Using porcine valve tissue combined with a flexible stent to reduce tissues stress, they have shown excellent durability with excellent hemodynamics.69 , 70 Through the use of the proprietary Cinch Implant System, the Mosaic line is especially suited for minimally invasive procedures.
Medtronic also offers the 3f Aortic Bioprosthesis, which they acquired from ATS, and the Freestyle Aortic Root Bioprosthesis. Uniquely designed, the 3f is a tubular structure that aims to mimic the function of a native aortic valve. Through the use of a tubular design, the valve preserves the aortic sinuses, restores the native stress distribution to the entire aortic root, and provides excellent hemodynamics by restoring physiologic and non-turbulent transvalvular flow while maintaining coronary perfusion.21 , 64 , 85 Finally, the Freestyle is a stentless bioprosthesis that aims to replicate human physiology while offering excellent durability.7 As a full root replacement, the Freestyle offers a great deal of surgical versatility. Reported clinical outcomes have been excellent with the Freestyle and studies have shown that use of this device for total root replacement is superior to isolated AVR when the outcome was freedom from reoperation.57
For the aortic position St. Jude Medical offers Bicor and Epic Stented Valves in sizes from 21 to 29 mm for the standard models and a size of 19 to 27 mm for the supra-annular models. Additionally St. Jude Medical offers the Trifecta valve, and the Toronto Porcine Valve. The Trifecta valve is composed of a fatigue resistant titanium stent with pericardial leaflets attached outside of the stent and a supra-annular sewing ring. Trifecta provides excellent hemodynamics and large orifice areas. Overall the durability data for Trifecta has been promising up to this point.25 In order to test the resting and exercise hemodynamics of the Trifecta valve, a group in France conducted a multicenter hemodynamic study of patients after implantation with a Trifecta valve in the aortic position.53 Mean gradients at rest, with low level and peak exercise were measured in addition to transvalvular velocities. The Trifecta valve showed no significant increase in mean gradient or velocity beyond what was expected from altered physiology. Of note, there was also a very low rate of patient-prosthesis mismatch. St. Jude Medical also offers its Toronto stentless porcine valve (SPV) and Toronto SPV II. These valves have excellent hemodynamics with initial durability; however, there have been some concerns over their long-term durability.5 , 26
Sorin Group offers several lines of aortic valves; the Mitroflow Aortic Pericardial Heart Valve (Fig. 3) and the Soprano Armonia Aortic Valve are the stented line of aortic valves. The Mitroflow and Soprano valves have demonstrated excellent hemodynamics, comparable with stentless porcine valves and superior to some stented bioprostheses, particularly in small sizes.90 Durability has also been shown to be excellent despite the low profile and small sewing ring which aid in ease of implantation.90 The valves are available in sizes from 21 to 31 mm. Additionally Sorin Group offers the stentless Freedom Solo and Pericarbon Freedom. Both valves are pericardial valves with no synthetic material aimed at reducing foreign body reactions and infection. The hemodynamics of both valves has been touted as being superior to many of their competitors. In fact, a hemodynamic study directly comparing the stented Carpentier-Edwards PERIMOUNT valve with the stentless Freedom valve showed that the mean AV gradients of the patients who received a Freedom valve were lower immediately post-operatively, at 6 and 12 months.56 Left ventricular mass index also significantly decreased in both groups, but was more significant in the group that received the Freedom stentless valve. Of note, the Pericarbon Freedom is available in a wide range of sizes from 15 to 29 mm.
Since the 1970s, chemically preserved stent-mounted tissue bioprosthetic valves have been used. With advances in the technology behind bioprosthetic valves that has resulted in greater durability, the use has steadily increased, particularly in the past decade.74 Despite advances, structural deterioration continues to be the major cause of valve failure, and the principal underlying pathologic process is cuspal calcification.33 , 74 Many strategies have been used to counteract this process which includes systemic and localized drug delivery along with substrate modification.74 While drug administration has fallen by the wayside, substrate modification through the use of inhibitors for calcium phosphate formation, removal of calcifiable material, improvement of glutaraldehyde fixation and the use of fixatives other than glutaraldehyde.74 Alternative fixative such as epoxy compounds, carbodimides and acyl azide are not widely in clinical use at this time.74 With improvements in anti-calcification treatments, and improved leaflet durability, there may come a time when mechanical valves are only used in very select cases and bioprosthetic valves become even more prevalent.
Transcatheter Aortic Valves
Transcatheter aortic valve replacement (TAVR) is a novel technology that has progressed a great deal in the past several years. The premise of the procedure is that a stent-caged bioprosthetic aortic valve is implanted through a catheter-based delivery system. These valves can be implanted through the femoral artery, the apex of the left ventricle, the subclavian artery, or directly through the aorta. Used as a therapy for severe aortic stenosis, the initial results have been promising. Patients who were high surgical risk, or those who were inoperable, were the first group of patients who underwent TAVR in large-scale studies, but the latest work is including patients of intermediate risk.39 A number of valves and delivery systems have been developed by several companies. Some have been more widely used and others are investigational. As the technology progresses, the goals are to overcome the shortcomings of the early devices and improve the implantation process with an option for transcatheter valve retrieval if the initial implant goes wrong. Several of the devices are discussed here with technical and clinical data.
First Generation Devices
Edwards Lifesciences Sapien Valve
The Edwards Lifesciences (Irvine, CA, USA) Sapien Valve was the first transcatheter aortic valve approved by the Food and Drug Administration (FDA) for implantation in the United States in November of 2011. In addition to the initial Sapien platform, Edwards Lifesciences has developed multiple generations of the Sapien Valve, which include the Sapient XT and the Sapien III (Fig. 4). All Sapien valves are balloon expandable stented valves with bovine pericardial leaflets.39 They all have no capability to be repositioned or retrieved.84 Several differences exist between the Sapien iterations including the use of different stent materials. The initial Sapien platform utilized a stainless steel stent, while the Sapien XT and Sapien III have a cobalt chromium alloy frame. Each valve comes in multiple sizes, with the Sapien being available in 23 and 26 mm sizes, and the Sapien XT and Sapien III being available in 23, 26 and 29 mm sizes (Fig. 4).
Edwards Lifesciences have developed three transcatheter heart valves illustrated here. The first generation Sapien valve has been followed by new iterations in the form of the Sapien XT and Sapien 3 both of which are illustrated here. Medtronics first successful valve is the Medtronic CoreValve pictured here
All Sapien iterations have a polymer skirt that is aimed at reducing paravalvular leak. The delivery system is where the greatest progress has been made between the iterations of the Sapien valve. The first Sapien valve has a delivery system—Retroflex™—with an inner diameter (ID) of 22Fr for the 23 mm valve and a 24Fr ID for the 26 mm valve. Sapien XT has a new delivery system named the NovaFlex+™ with ID of 16Fr, 18Fr and 20Fr for the 23, 26 and 29 mm valves, respectively. Finally, the Sapien III uses the Commander™ delivery system with a 14Fr ID sheath for the 23 and 26 mm valves, and a16Fr ID sheath for the 29 mm valve (Fig. 4). All these valves should be implanted once the stent is expanded; they neither allow for repositioning nor transcatheter retrieval if the valve is misplaced.
To date, the most significant trial of a transcatheter aortic valve was conducted using the Sapien valve. This trial is referred to as the PARTNER trial and was conducted as two parallel independently powered trials that included a total of 1057 patients.52 , 78 All patients had symptomatic severe aortic stenosis, and were determined to be either high risk for traditional open aortic valve replacement or inoperable. The high risk cohort included 699 patients who were randomized 1:1 to either TAVR or traditional open AVR for a primary endpoint of all-cause mortality with the goal being non-inferiority of TAVR.78 Inoperable patients were randomized 1:1 to TAVR or standard medical therapy with the primary endpoint being all-cause mortality with the goal being a superiority of TAVR when compared to medical therapy.52 In the high risk cohort, 3 year outcome data has been published and revealed all cause mortalities of 44.2 and 44.8% in the TAVR and open AVR groups respectively.78 In the TAVR vs. medical therapy group a clear superiority was shown.51 , 52 This trial was the basis for the FDA approval of the Sapien valve in the United States. In June of 2014, Sapien XT received FDA approval for both high-risk and inoperable aortic stenosis patients.
Medtronic CoreValve™
CoreValve is currently manufactured by Medtronic Inc (Minneapolis, MN, USA) and was the second transcatheter aortic valve approved for use in the United States (Fig. 4). There are two iterations of the CoreValve, the original and the CoreValve Evolut. Both versions are made of a self-expanding Nitinol stent with porcine pericardial leaflets and a sealing skirt.84 The Evolut is available in a 23 mm size, while the original CoreValve is available in 26, 29 and 31 mm sizes. All valves are currently delivered through an 18Fr ID delivery system.84 The CoreValve is not primarily designed to be repositioned or retrieved and the manufacturer does not promote it.82 According to a 270 retrospective patients study in UK,47 one-third of the patients undergoing a CoreValve implantation procedure require a permanent pacemaker within the 30 days of the procedure. The approval of the CoreValve was based on the results of the U.S. PIVOTAL Trial.14 In this trial, the CoreValve showed excellent results for all-cause mortality and major stroke in the extreme risk or non-operable group.
Second Generation and Investigational Devices
Medtronic Engager
A second platform from Medtronic, the Engager™ has a self-expanding Nitinol frame, a polyester skirt and bovine pericardial leaflets (Fig. 5). The novelty of this valve lies in its control arms, which both guide the operator with tactile feedback and secure the valve during deployment. Two sizes are available, 23–26 mm, which cover effective aortic annulus diameters of 21–26.5 mm. Currently the valve has only been used from a transapical (TA) approach and short term results have been published.40
St. Jude Medical Portico Valve
St. Jude Medical (St Paul, MN, USA) developed the Portico™ valve that has not yet gained FDA approval and is under investigation. The valve comes only in the 23 mm size currently and is delivered through an 18Fr catheter (Fig. 5).86 Portico™ consists of a self-expanding Nitinol stent and uses bovine pericardial leaflets. A unique component of the delivery system is that it tapers down to 13Fr diameter at the proximal end.86 The possibility to reposition, recapture, redeploy, or remove a partially or fully deployed valve may be desirable if the initial implant is placed incorrectly.86
Boston Scientific Lotus Valve
The Lotus Valve System (Boston Scientific, Natick, MA, USA) is another novel transcatheter valve that is fully repositionable and retrievable.37 Two sizes are available, the 23 mm prosthesis, which is deliverable via an 18Fr sheath and a 27 mm prosthesis whose delivery is made through a 20Fr sheath.37 A braided Nitinol frame is used with a central radiopaque positioning marker and the leaflets are composed of bovine pericardium (Fig. 5). Currently the valve is under study in human subjects, but does not yet have FDA approval.
Direct Flow Medical Valve
Direct Flow Medical (Lake Forest, CA, USA) developed the Direct Flow Medical Transcatheter Aortic Valve System, which is a unique valve in that it contains no metal in the valve frame and is truly fully repositionable. Given the unique design the valve is also able to be fully deployed and undergo full hemodynamic assessment before final implantation. The valve is a bovine pericardial valve with an expandable Dacron polyester double ring design (Fig. 5).75 The upper (aortic) and lower (ventricular) noncompliant ring balloons are interconnected by a tubular bridging system.75 Initially the rings are filled with contrast media and saline. Once the optimal position is obtained, a polymer is infused into the bioprosthesis replacing the contrast and saline. Then the polymer solidifies and the device is no longer retrievable.75 Sizes of 25, 27 and 29 mm are produced at this time, and an 18F sheath is used for all valve sizes.75 The DISCOVER Trial was conducted in Europe using the Direct Flow Valve, and results were promising.
JenaValve
JenaValve (JenaValve Technology, Munich, Germany) is a Nitinol self-expanding valve with porcine pericardial leaflets and a porcine pericardial patch, which functions as the skirt.41 The valve is available in three sizes (23, 25 and 27 mm) that are designed to cover annular sizes from 21 to 27 mm. A unique feature of the JenaValve is the anchoring mechanism which has “feelers” that sit in the sinuses of the native valve (Fig. 5).72 Native valve leaflets are then clipped in between the “feelers” and the valve body. This mechanism of placement ensures that the valve is firmly implanted using active fixation which is independent of the level of calcification on the native aortic valve.72 Using this mechanism of implantation allows JenaValve to be efficacious in the treatment of severe aortic regurgitation in addition to aortic stenosis. A major drawback of the JenaValve is the fact that the delivery system is very large (32Fr in diameter).
Symetis Acurate
Symetis (Ecublens, Switzerland) has developed the Acurate™ system of transcatheter valves that come in separate TA, transfemoral (TF) and transaortic (TAo) systems. All of the valves are composed of a self-expanding Nitinol stent with porcine pericardial leaflets and a polyethylene terephthalate (PET) skirt. The family of valves comes in three sizes, S, M and L, which are designed to cover annular sizes from 21 to 27 mm (Fig. 5). Acurate™ has a novel upper crown that allows for accurate annular placement with tactile feedback, and a lower crown that only minimally protrudes into the left ventricular outflow tract, minimizing conduction system damage. Delivery systems are designed for each system, the TF delivery system is 18Fr. CE mark studies have recently concluded and approval in Europe is expected in 2014.46
Colibri Heart Valve
The Colibri heart valve (Colibri Heart Valve LLC, Broomfield, CO, USA) is a balloon expandable stented valve with limited human clinical testing that is novel in its use of a low-profile (14Fr), pre-mounted, pre-packaged TAVR system (Fig. 5).31 Leaflets are porcine pericardium and the stent material is stainless steel. As with the JenaValve a tissue skirt is utilized to minimize paravalvular leak.31
Foldavalve
An investigational device created by FOLDA, LLC (Rancho Santa Margarita, CA, USA), Foldavalve is a low profile (14Fr) transcatheter valve with a novel leaflet configuration that spares the leaflets from being crimped during delivery, and therefore, preserves the quality of the leaflets comparable to surgical valves (Fig. 5).38 The valve is composed of a self-expanding Nitinol stent surrounding porcine or bovine pericardial leaflets. During delivery, the leaflets are kept outside of the stent and then fold back into the stent forming a trileaflet valve when the stent is expanded. During implantation the valve is repositionable and once placed it can be fully retrieved. Currently the device is in pre-clinical testing.
Limitations and Challenges
TAVR has progressed a great deal and with a host of new devices on the horizon and new iterations of the first generation devices now in market, there is reason to expect further expansion and indications of the technology. Limitations still exist that include, but are not limited to, vascular complications from large delivery systems, paravalvular leak (which has been shown to have clinical adverse effects) and malpositioning (which can result in coronary obstruction or conduction system disruption). Furthermore, there are few recent quantitative data that evaluates leaflets injury due to crimping.1 , 3 , 20 , 24 , 49 , 93 It has been shown that mechanical stresses affecting pericardial leaflets can cause disruption of collagen fiber orientation,1 that may lead to calcification and possible early valve failure.49 , 74 , 93 What effects this damage may have on the durability of transcatheter valves compared to surgical bioprosthetic valves is not yet known.1 , 84 The success of transcatheter technology would suggest that TAVR will see expanded indications in lower risk patients. As a result, leaflet durability will be of increased concern. A recent study by Alavi et al. showed that the aggressively crimped leaflets are severely damaged, suggesting either the leaflets should be placed outside the stent during crimping or they should not be aggressively compacted.1 This study also recommends that the ambition for lower profile devices should be tempered to avoid leaflets damage.1
Conclusion
Aortic valve disease is a significant cause of morbidity and mortality worldwide. With an improvement in global medical care and a resultant increased life expectancy, aortic valve disease will only see an increasing prevalence, which will necessitate more and less invasive therapeutic options. Additionally there will always be a group of patients with congenital valve disease who require valve replacement early in life. Therefore multiple valve replacement options will always be necessary whether they can be performed surgically or percutaneously. Here we have reviewed the currently available mechanical, bioprosthetic and transcatheter valves along with emerging therapies for aortic valve replacement.
References
Alavi, S. H., E. M. Groves, and A. Kheradvar. The effects of transcatheter valve crimping on pericardial leaflets. Ann. Thorac. Surg. 97:1260–1266, 2014.
Alemu, Y., G. Girdhar, M. Xenos, J. Sheriff, J. Jesty, S. Einav, and D. Bluestein. Design optimization of a mechanical heart valve for reducing valve thrombogenicity-a case study with ats valve. ASAIO J. 56:389–396, 2010.
Amahzoune, B., P. Bruneval, B. Allam, A. Lafont, J.-N. Fabiani, and R. Zegdi. Traumatic leaflet injury during the use of percutaneous valves: a comparative study of balloon- and self-expandable valved stents. Eur. J. Cardio Thorac. Surg. 43:488–493, 2013.
Aupart, M. R., A. Mirza, Y. A. Meurisse, A. L. Sirinelli, P. H. Neville, and M. A. Marchand. Perimount pericardial bioprosthesis for aortic calcified stenosis: 18-year experience with 1133 patients. J. Heart Valve Dis. 15:768–775, 2006; (discussion 775-766).
Bach, D. S., T. David, M. Yacoub, J. Pepper, B. Goldman, J. Wood, E. Verrier, M. Petracek, V. Aldrete, and M. Rosenbloom. Hemodynamics and left ventricular mass regression following implantation of the toronto SPV stentless porcine valve. Am. J. Cardiol. 82:1214–1219, 1998.
Bach, D. S., M. P. Sakwa, M. Goldbach, M. R. Petracek, R. W. Emery, and F. W. Mohr. Hemodynamics and early clinical performance of the st. Jude medical regent mechanical aortic valve. Ann. Thorac. Surg. 74:2003–2009, 2002.
Bach, D. S., N. D. Kon, J. G. Dumesnil, C. F. Sintek, and D. B. Doty. Ten-year outcome after aortic valve replacement with the freestyle stentless bioprosthesis. Ann. Thorac. Surg. 80:480–487, 2005.
Benson, A. M., K. Omrane, E. M. Graves, A. L. Haas, E. Bryant, M. Mandalaywala, and A. Mueller. Synthesis of a low thrombogenic heart valve coating with horseradish peroxidase. Polym. Adv. Technol. 16:117–122, 2005.
Blais, C., J. G. Dumesnil, R. Baillot, S. Simard, D. Doyle, and P. Pibarot. Impact of valve prosthesis-patient mismatch on short-term mortality after aortic valve replacement. Circulation 108:983–988, 2003.
Borger, M. A., J. Ivanov, S. Armstrong, D. Christie-Hrybinsky, C. M. Feindel, and T. E. David. Twenty-year results of the hancock ii bioprosthesis. J. Heart Valve Dis. 15:49–56, 2006.
Borger, M. A., A. F. Nette, M. Maganti, and C. M. Feindel. Carpentier-edwards perimount magna valve versus medtronic hancock ii: a matched hemodynamic comparison. Ann. Thorac. Surg. 83:2054–2058, 2007.
Bottio, T., L. Caprili, D. Casarotto, and G. Gerosa. Small aortic annulus: the hydrodynamic performances of 5 commercially available bileaflet mechanical valves. J. Thorac. Cardiovasc. Surg. 128:457–462, 2004.
Bradley, S. M. Aortic valve insufficiency in the teenager and young adult: the role of prosthetic valve replacement. World J. Pediatr. Congenit. Heart Surg. 4:397–402, 2013.
Bruschi, G., De Marco, F., Martinelli, L., Klugmann, S. Corevalve® transcatheter self-expandable aortic bioprosthesis. 2013.
Carabello, B. A., and W. J. Paulus. Aortic stenosis. Lancet 373:956–966, 2009.
Carrier, M., M. Pellerin, A. Basmadjian, D. Bouchard, L. P. Perrault, R. Cartier, P. Page, P. Demers, and Y. Hébert. Fifteen years of clinical and echocardiographic follow up with the carbomedics heart valve. J. Heart Valve Dis. 15:67, 2006.
Celiento, M., L. Filaferro, A. D. Milano, G. Anastasio, G. Ferrari, U. Bortolotti. Single center experience with the sorin bicarbon prosthesis: A 17-year clinical follow-up. J. Thorac. Cardiovas. Surg. 2013.
Chambers, J. B., J. L. Pomar, C. A. Mestres, and G. M. Palatianos. Clinical event rates with the on-x bileaflet mechanical heart valve: a multicenter experience with follow-up to 12 years. J. Thorac. Cardiovasc. Surg. 145:420–424, 2013.
Cheema, F. H., N. Hussain, A. P. Kossar, and G. Polvani. Patents and heart valve surgery—i: mechanical valves. Recent Pat. Cardiovasc. Drug Discov. 8:17–34, 2013.
Convelbo, C., P. Guetat, M. Cambillau, B. Allam, P. Bruneval, A. Lafont, and R. Zegdi. Crimping and deployment of balloon-expandable valved stents are responsible for the increase in the hydraulic conductance of leaflets. Eur. J. Cardio Thorac. Surg. 44:1045–1050, 2013.
Cox, J. L., N. Ad, K. Myers, M. Gharib, and R. Quijano. Tubular heart valves: a new tissue prosthesis design—preclinical evaluation of the 3f aortic bioprosthesis. J. Thorac. Cardiovasc. Surg. 130:520–527, 2005.
Cunanan, C. M., C. M. Cabiling, T. T. Dinh, S. Shen, P. Tran-Hata, J. H. Rutledge, III, and M. C. Fishbein. Tissue characterization and calcification potential of commercial bioprosthetic heart valves. Ann. Thorac. Surg. 71:S417–S421, 2001.
Dasi, L. P., H. A. Simon, P. Sucosky, and A. P. Yoganathan. Fluid mechanics of artificial heart valves. Clin. Exp. Pharmacol. Physiol. 36:225–237, 2009.
de Buhr, W., S. Pfeifer, J. Slotta-Huspenina, E. Wintermantel, G. Lutter, and W. A. Goetz. Impairment of pericardial leaflet structure from balloon-expanded valved stents. J. Thorac. Cardiovasc. Surg. 143:1417–1421, 2012.
Dell’Aquila, A. M., D. Schlarb, S. R. Schneider, J. R. Sindermann, A. Hoffmeier, G. Kaleschke, S. Martens, and A. Rukosujew. Clinical and echocardiographic outcomes after implantation of the trifecta aortic bioprosthesis: an initial single-centre experience. Interact. Cardiovasc. Thorac. Surg. 16:112–115, 2013.
Desai, N. D., O. Merin, G. N. Cohen, J. Herman, S. Mobilos, J. Y. Sever, S. E. Fremes, B. S. Goldman, and G. T. Christakis. Long-term results of aortic valve replacement with the st. Jude toronto stentless porcine valve. Ann. Thorac. Surg. 78:2076–2083, 2004.
Emery, R. W., G. J. Van Nooten, and P. J. Tesar. The initial experience with the ATS medical mechanical cardiac valve prosthesis. Ann. Thorac. Surg. 75:444–452, 2003.
Emery, R. W., C. C. Krogh, D. J. Jones, D. M. Nicoloff, D. P. Blake, and K. V. Arom. A five-year follow up of the ATS mechanical heart valve. J. Heart Valve Dis. 13:231–238, 2004.
Falahapisheh, A., and A. Kheradvar. High-speed particle image velocimetry to assess cardiac fluid dynamics in vitro: from performance to validation. Eur. J. Mech. B/Fluids 35:2–8, 2012.
Fallon, A. M., L. P. Dasi, U. M. Marzec, S. R. Hanson, and A. P. Yoganathan. Procoagulant properties of flow fields in stenotic and expansive orifices. Ann. Biomed. Eng. 36:1–13, 2008.
Fish R. D., D. Paniagua, Ureña P, Chevalier B. The colibri heart valve: Theory and practice in the achievement of a low-profile, pre-mounted, pre-packaged TAVI valve. EuroIntervention: Journal of EuroPCR in Collaboration with the Working Group on Interventional Cardiology of the European Society of Cardiology. 9:S111, 2013.
Fisher, J. Comparative study of the hydrodynamic function of six size 19 mm bileaflet heart valves. Eur. J. Cardio Thorac. Surg. 9:692–696, 1995.
Flameng, W., F. Rega, M. Vercalsteren, P. Herijgers, and B. Meuris. Antimineralization treatment and patient-prosthesis mismatch are major determinants of the onset and incidence of structural valve degeneration in bioprosthetic heart valves. J. Thorac. Cardiovasc. Surg. 147:1219–1224, 2014.
Forleo, M., and L. P. Dasi. Effect of hypertension on the closing dynamics and lagrangian blood damage index measure of the b-datum regurgitant jet in a bileaflet mechanical heart valve. Ann. Biomed. Eng. 42:110–122, 2014.
Gallegos, R. P., A. L. Rivard, P. T. Suwan, S. Black, S. Bertog, U. Steinseifer, A. Armien, M. Lahti, and R. W. Bianco. In-vivo experience with the triflo trileaflet mechanical heart valve. J Heart Valve Dis. 15:791–799, 2006.
Goldhaber, S. Z. “Bridging” and mechanical heart valves: perils, promises, and predictions. Circulation 113:470–472, 2006.
Gooley, R., P. Antonis, and I. T. Meredith. The next era of transcatheter aortic valve replacement: a case illustrating the benefit of a fully re-positionable, re-sheathable, and retrievable prosthesis. Catheter. Cardiovasc. Interv. 83:831–835, 2014.
Groves, E. M., A. Falahatpisheh, J. L. Su, and A. Kheradvar. The effects of positioning of transcatheter aortic valve on the fluid dynamics of the aortic root. ASAIO J. 60(5):545–552, 2014.
Grube, E., J.-M. Sinning, and A. Vahanian. The year in cardiology 2013: valvular heart disease (focus on catheter-based interventions). Eur. Heart J. 35:490–495, 2014.
Haussig, S., G. Schuler, and A. Linke. Worldwide tavi registries: What have we learned? Clin. Res. Cardiol. 2:1–10, 2014.
Holzhey, D., A. Linke, H. Treede, S. Baldus, S. Bleiziffer, A. Wagner, J. Börgermann, W. Scholtz, J.-L. Vanoverschelde, and V. Falk. Intermediate follow-up results from the multicenter engager european pivotal trial. Ann. Thorac. Surg. 96:2095–2100, 2013.
Ielasi, A., A. Latib, and M. Tespili. Current and new-generation transcatheter aortic valve devices: an update on emerging technologies. Expert Rev. Cardiovasc. Ther. 11:1393–1405, 2013.
Jin, X. Y., C. Ratnatunga, and R. Pillai. Performance of edwards prima stentless aortic valve over eight years. Sem. Thorac. Cardiovasc. Surg. 13:163–167, 2001.
Jun, B. H., N. Saikrishnan, and A. P. Yoganathan. Micro particle image velocimetry measurements of steady diastolic leakage flow in the hinge of a st. Jude medical((r)) regent mechanical heart valve. Ann. Biomed. Eng. 42:526–540, 2014.
Kaufmann, T. A., T. Linde, E. Cuenca-Navalon, C. Schmitz, M. Hormes, T. Schmitz-Rode, and U. Steinseifer. Transient, three-dimensional flow field simulation through a mechanical, trileaflet heart valve prosthesis. ASAIO J. 57:278–282, 2011.
Kelly, S., P. Verdonck, J. Vierendeels, K. Riemslagh, E. Dick, and G. Van Nooten. A three-dimensional analysis of flow in the pivot regions of an ATS bileaflet valve. Int. J. Artif. Org. 22:754–763, 1999.
Kempfert, J., H. Treede, A. J. Rastan, M. Schönburg, M. Thielmann, S. Sorg, F.-W. Mohr, and T. Walther. Transapical aortic valve implantation using a new self-expandable bioprosthesis (acurate ta™): 6-month outcomes. Eur. J. Cardio Thorac. Surg. 43:52–57, 2013.
Khawaja, M. Z., R. Rajani, A. Cook, A. Khavandi, A. Moynagh, S. Chowdhary, M. S. Spence, S. Brown, S. Q. Khan, N. Walker, U. Trivedi, N. Hutchinson, A. J. De Belder, N. Moat, D. J. Blackman, R. D. Levy, G. Manoharan, D. Roberts, S. S. Khogali, P. Crean, S. J. Brecker, A. Baumbach, M. Mullen, J.-C. Laborde, and D. Hildick-Smith. Permanent pacemaker insertion after corevalve transcatheter aortic valve implantation: incidence and contributing factors (the uk corevalve collaborative). Circulation 123:951–960, 2011.
Kheradvar, A., H. Houle, G. Pedrizzetti, G. Tonti, T. Belcik, and M. Ashraf. Lindner, J.R., Gharib, M., Sahn, D. Echocardiographic particle image velocimetry: a novel technique for quantification of left ventricular blood vorticity pattern. J. Am. Soc. Echocardiogr. 23:3102–3111, 2010.
Kiefer, P., F. Gruenwald, J. Kempfert, H. Aupperle, J. Seeburger, F. W. Mohr, and T. Walther. Crimping may affect the durability of transcatheter valves: an experimental analysis. Ann. Thorac. Surg. 92:155–160, 2011.
King, M., T. David, and J. Fisher. An initial parametric study on fluid flow through bileaflet mechanical heart valves using computational fluid dynamics. Proc. Inst. Mech. Eng. Part H 208:63–72, 1994.
Kodali, S. K., M. R. Williams, C. R. Smith, L. G. Svensson, J. G. Webb, R. R. Makkar, G. P. Fontana, T. M. Dewey, V. H. Thourani, and A. D. Pichard. Two-year outcomes after transcatheter or surgical aortic-valve replacement. New Engl. J. Med. 366:1686–1695, 2012.
Leon, M. B., C. R. Smith, M. Mack, D. C. Miller, J. W. Moses, L. G. Svensson, E. M. Tuzcu, J. G. Webb, G. P. Fontana, and R. R. Makkar. Transcatheter aortic-valve implantation for aortic stenosis in patients who cannot undergo surgery. New Engl. J. Med. 363:1597–1607, 2010.
Levy, F., E. Donal, L. Bière, C. Szymanski, J. P. Remadi, E. Flécher, O. Fouquet, A. Leguerrier, and C. Tribouilloy. Hemodynamic performance during exercise of the new st. Jude trifecta aortic bioprosthesis: results from a french multicenter study. J. Am. Soc. Echocardiogr. 27:590–597, 2014.
Marchand, M. A., M. R. Aupart, R. Norton, I. R. Goldsmith, L. C. Pelletier, M. Pellerin, T. Dubiel, W. J. Daenen, P. Herijgers, and F. P. Casselman. Fifteen-year experience with the mitral carpentier-edwards perimount pericardial bioprosthesis. Ann. Thorac. Surg. 71:S236–S239, 2001.
Matthews, A. M. The development of the starr-edwards heart valve. Texas Heart Inst. J. 25:282–293, 1998.
Miraldi, F., L. Spagnesi, D. Tallarico, G. Di Matteo, and G. Brancaccio. Sorin stentless pericardial valve versus carpentier–edwards perimount pericardial bioprosthesis: is it worthwhile to struggle? Int. J. Cardiol. 118:253–255, 2007.
Mohammadi, S., D. Kalavrouziotis, P. Voisine, E. Dumont, D. Doyle, J. Perron, and F. Dagenais. Bioprosthetic valve durability after stentless aortic valve replacement: the effect of implantation technique. Ann. Thorac. Surg. 97:2011–2018, 2014.
Naidoo, R., B. Pearse, P. Tesar, S. Yap, A. Barnett, and T. Fayers. Long-term outcomes following medtronic open pivot valved conduit. J Heart Valve Dis. 23:105–111, 2014.
Nishimura, R. A., C. M. Otto, R. O. Bonow, B. A. Carabello, J. P. Erwin, R. A. Guyton, P. T. O’Gara, C. E. Ruiz, N. J. Skubas, and P. Sorajja. AHA/ACC guideline for the management of patients with valvular heart disease: a report of the american college of cardiology/american heart association task force on practice guidelines. J. Am. Coll. Cardiol. 63:e57–e185, 2014.
Northrup, 3rd, W. F., R. W. Emery, D. M. Nicoloff, T. J. Lillehei, A. R. Holter, and D. P. Blake. Opposite trends in coronary artery and valve surgery in a large multisurgeon practice, 1979–1999. Ann. Thorac. Surg. 77:488–495, 2004.
Offstad, J., K. Andersen, P. Paulsson, J. Andreasson, U. Kjellman, O. Lundblad, K. G. Engstrøm, R. Haaverstad, and J. L. Svennevig. The scandinavian multicenter hemodynamic evaluation of the SJM regent aortic valve. J. Cardiothorac. Surg. 6:163, 2011.
Piazza, N., and J. Gregoire. Images in clinical medicines. Starr-edwards heart valves. New Engl. J. Med. 358:e24, 2008.
Pibarot, P., and J. G. Dumesnil. Prosthetic heart valves selection of the optimal prosthesis and long-term management. Circulation 119:1034–1048, 2009.
Pillai, R., C. Ratnatunga, J. L. Soon, H. Kattach, A. Khalil, and X. Y. Jin. 3f prosthesis aortic cusp replacement: implantation technique and early results. Asian Cardiovasc. Thorac. Ann. 18:13–16, 2010.
Prifti, E., M. Bonacchi, A. Baboci, K. Krakulli, and G. Giunti. Early and mid-term functional and hemodynamic evaluation of the st. Jude medical regent 17 mm aortic valve mechanical prosthesis. J. Heart Valve Dis. 23:112–121, 2014.
Puskas, J., M. Gerdisch, D. Nichols, R. Quinn, C. Anderson, B. Rhenman, L. Fermin, M. McGrath, B. Kong, and C. Hughes. Reduced anticoagulation after mechanical aortic valve replacement: interim results from the prospective randomized on-x valve anticoagulation clinical trial randomized food and drug administration investigational device exemption trial. J. Thorac. Cardiovasc. Surg. 147(1202–1211):e1202, 2014.
Rahimtoola, S. H. Choice of prosthetic heart valve in adults an update. J. Am. Coll. Cardiol. 55:2413–2426, 2010.
Reyes, G., S. Badia, P. Alvarez, C. Kallmeyer, S. Rodriguez, A. Sarraj, and J. Bustamante. Results of aortic valve replacement with the supra-annular sorin bicarbon overline prosthesis. J. Heart Valve Dis. 21:358–363, 2012.
Riess, F.-C., R. Bader, E. Cramer, L. Hansen, B. Kleijnen, G. Wahl, J. Wallrath, S. Winkel, and N. Bleese. Hemodynamic performance of the medtronic mosaic porcine bioprosthesis up to ten years. Ann. Thorac. Surg. 83:1310–1318, 2007.
Riess, F.-C., E. Cramer, L. Hansen, S. Schiffelers, G. Wahl, J. Wallrath, S. Winkel, and P. Kremer. Clinical results of the medtronic mosaic porcine bioprosthesis up to 13 years. Eur. J. Cardio Thorac. Surg. 37:145–153, 2010.
Ross, Jr., J., and E. Braunwald. Aortic stenosis. Circulation 38:61–67, 1968.
Rudolph, T. K., and S. Baldus, Jenavalve-transfemoral technology. EuroIntervention: Journal of EuroPCR in collaboration with the Working Group on Interventional Cardiology of the European Society of Cardiology. 9:S101, 2013.
Sato, M., H. Harasaki, K. E. Wika, M. V. Soloviev, and A. S. Lee. Blood compatibility of a newly developed trileaflet mechanical heart valve. ASAIO J. 49:117–122, 2003.
Schoen, F. J., and R. J. Levy. Calcification of tissue heart valve substitutes: progress toward understanding and prevention. Ann. Thorac. Surg. 79:1072–1080, 2005.
Schofer, J., A. Colombo, S. Klugmann, J. Fajadet, F. DeMarco, D. Tchétché, F. Maisano, G. Bruschi, A. Latib, and K. Bijuklic. Prospective multicenter evaluation of the direct flow medical® transcatheter aortic valve. J. Am. Coll. Cardiol. 63:763–768, 2014.
Schwarz, F., P. Baumann, J. Manthey, M. Hoffmann, G. Schuler, H. C. Mehmel, W. Schmitz, and W. Kubler. The effect of aortic valve replacement on survival. Circulation 66:1105–1110, 1982.
Shipkowitz, T., J. Ambrus, J. Kurk, and K. Wickramasinghe. Evaluation technique for bileaflet mechanical valves. J. Heart Valve Dis. 11:275–282, 2002.
Smith, C. R., M. B. Leon, M. J. Mack, D. C. Miller, J. W. Moses, L. G. Svensson, E. M. Tuzcu, J. G. Webb, G. P. Fontana, and R. R. Makkar. Transcatheter versus surgical aortic-valve replacement in high-risk patients. New Engl. J. Med. 364:2187–2198, 2011.
Valfrè, C., P. Ius, G. Minniti, L. Salvador, T. Bottio, F. Cesari, G. Rizzoli, and G. Gerosa. The fate of hancock ii porcine valve recipients 25 years after implant. Eur. J. Cardio Thorac. Surg. 38:141–146, 2010.
Van Nooten, G. J., F. Caes, K. Francois, Y. Van Belleghem, T. Bové, G. Vandenplas, M. De Pauw, and Y. Taeymans. Fifteen years’ single-center experience with the ATS bileaflet valve. J. Heart Valve Dis. 18:445–452, 2009.
Van Nooten, G. J., T. Bové, Y. Van Belleghem, K. François, F. Caes, G. Vandenplas, M. De Pauw, and Y. Taeymans. Twenty-year single-center experience with the medtronic open pivot mechanical heart valve. Ann. Thorac. Surg. 97:1306–1313, 2014.
Vavuranakis, M., D. Vrachatis, and C. Stefanadis. Corevalve aortic bioprosthesisrepositioning techniques. JACC Cardiovasc. Interv. 3:565–565, 2010.
Wang, J., H. Yao, C. Lim, Y. Zhao, T. Yeo, and N. Hwang. Computational fluid dynamics study of a protruded-hinge bileaflet mechanical heart valve. J. Heart Valve Dis. 10:254–262, 2001; (discussion 263).
Webb, J., and A. Cribier. Percutaneous transarterial aortic valve implantation: what do we know? Eur. Heart J. 32:140–147, 2011.
Wendt, D., M. Thielmann, T. Buck, R.-A. Jánosi, T. Bossert, N. Pizanis, M. Kamler, and H. Jakob. First clinical experience and 1-year follow-up with the sutureless 3f-enable aortic valve prosthesis. Eur. J. Cardio Thorac. Surg. 33:542–547, 2008.
Willson, A. B., J. Rodès-Cabau, D. A. Wood, J. Leipsic, A. Cheung, S. Toggweiler, R. K. Binder, M. Freeman, R. DeLarochellière, and R. Moss. Transcatheter aortic valve replacement with the st. Jude medical portico valvefirst-in-human experience. J. Am. Coll. Cardiol. 60:581–586, 2012.
Wu, J., B. M. Yun, A. M. Fallon, S. R. Hanson, C. K. Aidun, and A. P. Yoganathan. Numerical investigation of the effects of channel geometry on platelet activation and blood damage. Ann. Biomed. Eng. 39:897–910, 2011.
Xenos, M., G. Girdhar, Y. Alemu, J. Jesty, M. Slepian, S. Einav, and D. Bluestein. Device thrombogenicity emulator (DTE)—design optimization methodology for cardiovascular devices: a study in two bileaflet mhv designs. J. Biomech. 43:2400–2409, 2010.
Yankah, C. A., M. Pasic, M. Musci, J. Stein, C. Detschades, H. Siniawski, and R. Hetzer. Aortic valve replacement with the mitroflow pericardial bioprosthesis: durability results up to 21 years. J. Thorac. Cardiovasc. Surg. 136:688–696, 2008.
Yin, W., E. C. Ngwe, and D. A. Rubenstein. A biocompatible flow chamber to study the hemodynamic performance of prosthetic heart valves. ASAIO J. 58:470–480, 2012.
Yun, B. M., J. Wu, H. A. Simon, S. Arjunon, F. Sotiropoulos, C. K. Aidun, and A. P. Yoganathan. A numerical investigation of blood damage in the hinge area of aortic bileaflet mechanical heart valves during the leakage phase. Ann. Biomed. Eng. 40:1468–1485, 2012.
Zegdi, R., P. Bruneval, D. Blanchard, and J.-N. Fabiani. Evidence of leaflet injury during percutaneous aortic valve deployment. Eur. J. Cardio Thorac. Surg. 40:257–260, 2011.
Zingg, U., B. Aeschbacher, C. Seiler, U. Althaus, and T. Carrel. Early experience with the new masters series of st. Jude medical heart valve: in vivo hemodynamic and clinical results in patients with narrowed aortic annulus. J. Heart Valve Dis. 6:535–541, 1997.
Acknowledgments
This review article was prepared after the Mathematics Guiding Bioartificial Heart Valve Design meeting held at the Ohio State University, October 28 to 31, 2013. The authors would like to acknowledge the Mathematical Biosciences Institute and its grant from National Science Foundation (DMS 0931642) that facilitated the meeting.
Conflict of interest
Arash Kheradvar is a co-founder of FOLDA LLC, the manufacturer of FOLDAVALVE. Otherwise the remaining authors have nothing to disclose.
Author information
Authors and Affiliations
Corresponding author
Additional information
Associate Editor Estefanía Peña oversaw the review of this article.
Rights and permissions
About this article
Cite this article
Kheradvar, A., Groves, E.M., Goergen, C.J. et al. Emerging Trends in Heart Valve Engineering: Part II. Novel and Standard Technologies for Aortic Valve Replacement. Ann Biomed Eng 43, 844–857 (2015). https://doi.org/10.1007/s10439-014-1191-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10439-014-1191-5