Abstract
The public health risks associated with dairy farming intensification are an emerging concern. We examine the association between dairy cattle density and cryptosporidiosis risk in children <5 years old in New Zealand from 1997 to 2008, a period of rapid intensification of the dairy industry. Multi-level Poisson regression was used to model reported cryptosporidiosis (N = 3869 cases) incidence in relation to dairy cattle densities across urban and rural areas separately, after controlling for microbiological quality of public drinking water supplies and neighbourhood socio-economic factors using the Census Area Unit of residence. Within urban areas, the risk of cryptosporidiosis in children less than 5 years old was significantly, positively associated with medium and high dairy cattle density IRR 1.3 (95% CI 1.2, 1.5) and 1.5 (95% CI 1.2, 1.9) respectively, when compared to areas with no dairy cattle. Within rural areas, the incidence risk of cryptosporidiosis in children less than 5 years old were significantly, positively associated with medium and high dairy cattle density: IRR 1.7 (95% CI 1.3, 2.3) and 2.0 (95% CI 1.5, 2.8) respectively, when compared to areas with no dairy cattle. These results have public health implications for children living on and in proximity to intensively stocked dairy cattle farms.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Over 60% of known infectious agents pathogenic to humans are zoonotic (Taylor et al. 2001), with over three quarters of recorded emerging infectious disease events originating from animal sources (Jones et al. 2008). There is consistent evidence of a link between domestic food-producing animals and gastrointestinal illness in humans across a range of animal exposures and enteric pathogens (Zambrano et al. 2014).
Cryptosporidium spp. are some of the most frequently isolated enteric parasites of both humans and domestic animals (Hunter and Thompson 2005), with considerable zoonotic transmission. Cryptosporidiosis in children less than 5 years old is particularly high (Kotloff et al. 2012). Like many other gastrointestinal illnesses, cryptosporidiosis is faecal-orally spread, meaning that clean drinking water and adequate hygiene are important to reduce infection (Burnet et al. 2014; Sarkar et al. 2014). In addition, positive associations of human cryptosporidiosis incidence with livestock density in New Zealand (Snel et al. 2009a, b), the US (Jagai et al. 2010) and Scotland (Pollock et al. 2009), and higher disease rates in rural Canada (Odoi et al. 2004) suggest that livestock are an important reservoir for human infection.
New Zealand has recently experienced rapid dairy farming intensification (Bouwman et al. 2011). Increased dairy cattle stocking rates (MacLeod and Moller 2006) are considered one of the keystones to achieving this greater agricultural production (Statistics New Zealand 2012a, b). From 1990 to 2012, the number of dairy herds decreased by 19%, while the average herd size expanded by 147%. Such intensification of dairy cattle production may increase the public health risk from zoonotic pathogens (Crump et al. 2001; Derraik and Slaney 2007). Understanding the implications of such an increase in stocking rates is important to provide an evidence base to guide environmental and public health management to reduce the health impacts.
Despite the obvious disease burden in children and the importance of livestock as a reservoir for human infection (Pollock et al. 2009), as far as we are aware, there are no studies that have examined the association between increased stocking rates of dairy cattle and cryptosporidiosis risk in children under 5 years. Building on a previous study in New Zealand that used data on reported cryptosporidiosis from 1997 to 2006 to identify correlations with animal density (Snel et al. 2009a, b), we examine the association between increasing dairy cattle densities and the risk of reported cryptosporidiosis in children under 5 years old, after controlling for the well-established association of cryptosporidiosis with public drinking water quality, urban–rural residence and neighbourhood socio-economic status.
Methods
Notification Data
All notified cases of cryptosporidiosis reported in children less than 5 years old between 1 January 1997 to 31 December 2008 in New Zealand were extracted from the National Notifiable Disease Surveillance system. No major changes were made to the surveillance of these notifiable diseases from 1997 to 2008 (except for the addition of direct laboratory notification in 2008). This was also a period of rapid change in livestock farming across New Zealand, with an increase in cattle numbers, decrease in number of farms and increase in stock density (Figure S1 Supplementary Material). A Census Area Unit (CAU) is a geographical unit defined by Statistics New Zealand, each of which has a population of 3000–5000 people. The CAU was chosen as the unit for analysis (n = 1769). CAUs are composed of smaller meshblocks (n = 41,385) and can be aggregated to form larger Territorial Authorities (TA) (n = 72, see Fig. 1). Laboratory-confirmed cases of cryptosporidiosis (n = 3869) were extracted along with the following case information: report date, age of notified case and CAU code of residence.
Population at Risk
The estimated resident population of children less than 5 years old from the 2006 National Census for each CAU were used to calculate the annual average number of notifications per 100,000 population (referred to as Incidence Risk, IR) (Statistics New Zealand A 2010).
Urban/Rural Status
CAUs are classified by Statistics New Zealand into one of the following categories: main urban areas, satellite urban areas, independent urban areas, rural areas with high urban influence, rural areas with moderate urban influence, rural areas with low urban influence, highly rural/remote areas, areas outside urban/rural profile (Statistics New Zealand 2012a, b). Only the urban/rural classification was required since the main hypothesis for this analysis concerned differing risk factors in main urban areas and rural areas. Therefore, the categories ‘Main urban areas’, ‘Satellite urban areas’ and ‘Independent urban areas’ were classified as urban, whereas the categories ‘Rural areas with high urban influence’, ‘Rural areas with moderate urban influence’, ‘Rural areas with low urban influence’ and ‘Highly rural/remote areas’ were classified as rural.
New Zealand Deprivation Index
The New Zealand Deprivation Score (2006) is an area-based measure which combines nine social and economic measures from census data to categorize the CAU based on deprivation (Salmond et al. 2006). These dimensions include income, home ownership, parental support if under 65 years, employment, qualifications, living space, access to telecommunications and transport. In the current study, the Deprivation scores for each CAU were categorized into tertiles. The least deprived areas were the reference category.
Drinking Water Quality
Drinking water quality for the year 2006 was supplied by the Institute of Environmental Science and Research (ESR) Water Programme. ESR used both the distribution zone code and protozoa compliance to construct a scoring system for drinking water quality. Modifying the methods used by Brock (2011), in this study, Level 0 denoted good drinking water quality (complied with microbiological standards) (reference category); Level 1 denoted intermediate and poor drinking water quality (inadequately monitored and/or non-compliant with microbiological standards) and Level 2 indicated that the quality was unknown. The method of assigning drinking water quality to CAUs is detailed in the Supplementary Material methods Sect. 1.
Dairy Cattle Density
Numbers of dairy cattle for meshblocks were obtained from the Agribase™ database for 2006. Dairy cattle including milking cows, replacement heifers, breeding bulls and calves for each farm were geocoded to a Meshblock based on the location of the main farm gate or homestead. The average density of dairy cattle per square kilometre for each CAU was calculated by summing the counts by meshblock divided by CAU area and categorized as follows: no dairy cattle; 1-100 cattle/km2 and greater than 100 cattle/km2. The areas with no dairy cattle were chosen as the reference category.
Data Analysis
To account for the hierarchical nature of our data (Fig. 1), we performed a two-level Poisson regression analysis adjusted for population size (Duncan et al. 1996). The analysis was conducted separately for urban and rural areas as we were interested in how the associations between dairy cattle density and risk of reported disease in preschool children vary across these areas, after controlling for public drinking water quality and neighbourhood socio-economic characteristics. Area-level socio-economic deprivation, quality of drinking water supplies and dairy cattle density were modelled as categorical variables. All analyses were conducted in Stata version 13 (StataCorp 2013).
Results
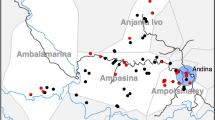
Descriptive data show that 59% of the cases resided in urban areas (incidence risk 77/100,000 population per year) and 41% in rural areas (incidence risk 338/100,000 population per year). Thirty-nine percent of the reported cases resided in CAUs with least deprived neighbourhoods (incidence risk 158.8 illnesses per 100,000 population per year), 37% (incidence risk 135.9 illnesses per 100,000 population per year) and 23% (incidence risk 64.3 illnesses per 100,000 population per year) in intermediate and most deprived neighbourhoods respectively (Table 1). CAUs with microbiologically safe (good) drinking water quality comprised 35% of the sample (incidence risk 89.3 illnesses per 100,000 population per year), with 58% (incidence risk 156 illnesses per 100,000 population per year) and 6% (incidence risk 51.8 illnesses per 100,000 population per year) of reported cases classed as residing in areas with intermediate and poor drinking water quality and unknown quality respectively. The distribution of notified cases across CAUs with and without dairy cattle was fairly even with 46% of cases reported from CAUs with no dairy cattle and 54% of cases reported from areas with dairy cattle (40% from areas with dairy cattle density between >0 and 100 cattle/km2, and 14% from areas with dairy cattle density greater than 100 cattle/km2). However, the incidence risk of reported cryptosporidiosis per 100,000 population per year in these areas varied. In areas with no dairy cattle, the incidence risk was 68.7 illnesses per 100,000 population per year, in areas with dairy cattle density between >0 and 100 cattle/km2, the incidence risk was 217.4 illnesses per 100,000 population per year, and in areas with dairy cattle density greater than 100 cattle/km2, the incidence risk was 395.4 illnesses per 100,000 population per year. Figure 2a shows the spatial distribution of reported cryptosporidiosis incidence in preschool children from 1997 to 2008 at CAU scale. Figure 2b shows the spatial distribution of the 2006 dairy cattle density categories at the CAU scale. Correlations between variables were low (Table 2). Negative correlations were observed between the reported cryptosporidiosis incidence and neighbourhood level deprivation (−0.1) (P < 0.001) and drinking water quality (-0.01) (P > 005), with positive correlations between the cryptosporidiosis incidence and dairy cattle density (0.2) (P < 0.001). Dairy cattle density was positively correlated with drinking water quality (0.1) (P < 0.001). Thus, the final analysis was performed with all the variables to adjust for confounding (Model 2).
Spatial distribution of cryptosporidiosis risk and dairy cattle density. a Incidence risk of cryptosporidiosis per 100,000 population per year in preschool children in New Zealand, 1997–2008. b Census Area Units categorized into 2006 dairy cattle densities; 0 (no cattle), Medium (0.1–100 cattle/km2), and High (>100 cattle/km2).The inset in the maps shows Hamilton city and surrounding Waikato District with respect to average annual cryptosporidiosis incidence risk (Fig. 2a) and dairy cattle density categories (Fig. 2b).
Multi-Level Model Analyses
Results from the two-level Poisson regression analysis (Table 3) show that compared to rural areas with no dairy cattle, the incidence risk of cryptosporidiosis in children less than 5 years old were significantly, positively associated with medium and high dairy cattle density: IRR 1.7 (95% CI 1.3, 2.3) and 2.0 (95% CI 1.5, 2.8) respectively. Compared to rural areas with microbiologically safe drinking water quality, drinking water of unknown quality was inversely associated with cryptosporidiosis risk: IRR 0.5 (95% CI 0.3, 0.8). Areas with poor drinking water quality were not significantly associated with cryptosporidiosis risk: IRR 1.1 (95% CI 0.9, 1.3). The variance explained at the TA level was 0.56.
Compared to urban areas with no dairy cattle, the risk of cryptosporidiosis in children less than 5 years old was significantly, positively associated with medium and high dairy cattle density IRR 1.3 (95% CI 1.2, 1.5) and 1.5 (95% CI 1.2, 1.9), respectively. The variance explained at the TA level was 0.54.
Discussion
In New Zealand, rates of cryptosporidiosis are among the highest reported for any developed country (Snel et al. 2009a, b) and are a substantial economic concern (Moore et al. 2010). We have found that the intensification of livestock production, as measured by increasing dairy cattle stocking densities, are associated with a greater risk of reported cryptosporidiosis in children under 5 years old, after controlling for area-level socio-economic status and public drinking water quality. However, in rural areas, drinking water of unknown quality was inversely associated with disease risk, when compared to areas with microbiologically adequate water supplies.
Our finding of a greater risk of reported illness in children under 5 years with increasing dairy cattle densities in New Zealand is supported by results from cryptosporidiosis outbreak investigations due to farm visits (Stefanogiannis et al. 2001) and direct contact with calves (Grinberg et al. 2011). Molecular analyses implicating cattle as a source of human cryptosporidiosis in spring and as a potential reservoir for human infection, presenting a threat to both animal and human health, have also been documented (Learmonth et al. 2001, 2003; Abeywardena et al. 2012; Mawly Al et al. 2015).
In our study, urban areas included satellite towns and independent urban communities, which, in New Zealand, are commonly surrounded by farmland, providing a biologically plausible explanation for the statistically significant association of disease risk with dairy cattle density in urban areas. Dairy farming in New Zealand is primarily a pastoral activity with outdoor gazing of cows which are moved between pastures and to milking sheds on a daily basis, and thus opportunity to spread contamination through the environment is high. For instance, open grazing allows faecal deposits on pasture potentially being mobilised into surface water via a rainfall event. The number of human illnesses from contact with recreational water is increasing (Yoder et al. 2012), and this may be related to runoff from pastures contaminating waterways. Degraded water quality is a common feature of streams in intensively farmed pastoral catchments in New Zealand (Davies-Colley et al. 2004, 2008). Such an environmental risk is particularly important in New Zealand, where much recreation is based on access to the outdoors and water activities.
Another possible explanation is that intensive farming systems rely on genetic selection of stock and management practices such as high animal densities. Low genetic diversity and high animal numbers create optimal conditions for pathogens to amplify and evolve into more pathogenic strains (Jones et al. 2013) and greater opportunities for contact and zoonotic spread (Murray et al. 2016). However, restricting livestock access to waterways, such as via stream bank fencing, can reduce microbial pollution to streams (Davies-Colley et al. 2004). Vegetated strips when placed near dairy calf areas significantly reduced the concentration of another water-borne parasite, Giardia, in runoff during storm events (Miller et al. 2007). It is reasonable to conclude that changes to farm management, such as maintaining vegetative buffer strips along river banks and reducing stock access to water sources can be considered an intervention point to reduce environmental contamination with benefits to both veterinary and public health.
We found that in rural regions, drinking water of unknown quality was inversely associated with cryptosporidiosis risk, when compared to areas with microbiologically adequate water supplies. This is in contrast to previous findings where the lowest mean rates of notified cryptosporidiosis were observed in communities served by drinking water supplies with completely satisfactory public health gradings and the highest rates in communities served by ungraded drinking water supplies (Duncanson et al. 2000). However, Duncanson et al. were unable to account for other common risk factors in small communities such as animal densities, which may have confounded their results.
The “unknown” category in our study includes smaller public water supplies that are not routinely tested and private water supplies. It is possible that these supplies are of better quality; however, this aspect is not addressed by the grading used in the current study. Also, many rural areas have roof water supplies, which are less likely to be contaminated by dairy effluent compared to groundwater supplies, especially in areas with major irrigation schemes (Close et al. 2008, 2010). It is also possible that the high awareness of drinking water contamination in these areas have led to increased protection of water sources. As contamination of drinking water sources is an important pathway for Cryptosporidium spp., especially C. parvum in rural areas, clarifying the role of these smaller water supplies in transmission may help develop interventions such an enhanced drinking water infrastructure to reduce disease burden in areas dominated by intensive cattle farming.
Our study uses disease surveillance data, known to suffer from significant under-ascertainment (Arshad et al. 2007). This bias is highlighted in the results, where, living in urban, more deprived areas are inversely associated with risk of disease. Such patterns could be due to poorer access to health resources resulting in lower rates of reported cryptosporidiosis in socio-economically deprived populations (Baker et al. 2007). However, by creating independent exposure measures we also reduce the potential for misclassification bias whereby area-level exposures are incorrectly assigned. The patterns reported here could differ by pathogen strain (McCarthy et al. 2012), particularly for cryptosporidiosis, where clear differences in seasonal patterns of cryptosporidiosis across urban and rural areas indicate different dominant strains (Learmonth et al. 2001, 2003). Strain specific information was not available for this study. The main aim of this study was to examine the potential public health implications of increasing stocking densities. Similar to previous studies in New Zealand, a key strength of this study is that by integrating different data sources intended for unrelated purposes, we provide a resource-efficient but data-intensive method to identify a public health problem that may be exacerbated by dairying intensification in New Zealand (Snel et al. 2009a, b; Britton et al. 2010).
It is possible that the association with dairy cattle density is confounded by the presence of other livestock in the same area. However, a previous study which included sheep, poultry, pig, deer and dairy cattle density at the CAU level found that only dairy cattle density was significantly, positively associated with cryptosporidiosis risk in New Zealand (Lal 2014). Our results are consistent with other studies in New Zealand (Snel et al. 2009a, b; Brock 2011; Thorburn 2011) and elsewhere (Pollock et al. 2009; Jagai et al. 2010), conducted across different spatial scales and using varying methodologies. Our finding of a significant relationship between cryptosporidiosis in children under 5 years and increasing stocking densities for dairy cattle is novel and is likely to be causal. A concerted effort between the human health and animal sector in rural and fringe areas, where person-to-person transmission is unlikely to be the major pathway for disease spread is needed.
Our findings have implications for the planning of zoonoses prevention strategies as the most effective interventions may not necessarily emerge from the health sector (Zinsstag et al. 2005). Efforts should be made to strengthen the links between the animal and public health sectors and promote inter-disciplinary surveillance of zoonoses (Wendt et al. 2016). At the same time, carrying out public health awareness campaigns on zoonoses and promoting behaviour change could help reduce the implications of zoonotic infections in human–domestic animal interface areas. Finally, information to increase farmers’ awareness of zoonotic disease risks and farm-level responses to reduce such risk could help uptake of measures to reduce disease.
Conclusion
Even in an industrialized nation like New Zealand, reducing the vulnerability of children to infectious, zoonotic disease remains a challenge. When the underlying neighbourhood socio-economic characteristics are accounted for, we found a significant relationship between cryptosporidiosis risk and increasing densities of dairy cattle. This study adds to the growing concern about the public health impacts of high-density livestock production. These findings highlight the importance of developing strategies across the animal and public health sectors to address specific risk factors for children living on and in proximity to intensively stocked dairy cattle farms.
References
Abeywardena H, Jex AR, et al. (2012) Genetic characterisation of Cryptosporidium and Giardia from dairy calves: Discovery of species/genotypes consistent with those found in humans. Infection, Genetics and Evolution 12(8): 1984–1993
Mawly Al J, Grinberg A, et al. (2015) Cross sectional study of prevalence, genetic diversity and zoonotic potential of Cryptosporidium parvum cycling in New Zealand dairy farms. Parasites and Vectors 8(1): 240
Arshad MM, Wilkins MJ, et al (2007) A registry-based study on the association between human salmonellosis and routinely collected parameters in Michigan, 1995-2001. Foodborne Pathogens and Disease 4(1): 16–25
Baker MG, Sneyd E, et al. (2007) Is the major increase in notified campylobacteriosis in New Zealand real? Epidemiology and Infection 135(01): 163–170
Bouwman L, Goldewijk KK, et al. (2011) Exploring global changes in nitrogen and phosphorus cycles in agriculture induced by livestock production over the 1900–2050 period. Proceedings of the National Academy of Sciences. doi:10.1073/pnas.1012878108
Britton E, Hales S, et al. (2010) The impact of climate variability and change on cryptosporidiosis and giardiasis rates in New Zealand. Journal of Water and Health 8(3): 561–571
Brock A (2011) The effect of climate variation on infectious diseases in humans in New Zealand. Masters in Veterinary Studies, Massey University.
Burnet JB, Penny C, et al. (2014) Spatial and temporal distribution of Cryptosporidium and Giardia in a drinking water resource: Implications for monitoring and risk assessment. Science of the Total Environment 472: 1023–1035
Close M, Dann R, et al. (2008) Microbial groundwater quality and its health implications for a border-strip irrigated dairy farm catchment, South Island, New Zealand. Journal of Water and Health 6(1): 83–98
Close M, Noonan M, et al. (2010) Microbial Transport from Dairying under Two Spray-Irrigation Systems in Canterbury, New Zealand. Journal of Environmental Quality 39(3): 824–833
Crump JA, Murdoch DR, et al. (2001) Emerging infectious diseases in an island ecosystem: the New Zealand perspective. Emerging Infectious Diseases 7(5): 767–772
Davies-Colley R, Lydiard E, et al. (2008) Stormflow-dominated loads of faecal pollution from an intensively dairy-farmed catchment. Water Science and Technology 57(10): 1519–1523
Davies-Colley RJ, Nagels JW, et al. (2004) Water quality impact of a dairy cow herd crossing a stream. New Zealand Journal of Marine and Freshwater Research 38(4): 569–576
Derraik JGB, Slaney D (2007) Anthropogenic environmental change, mosquito-borne diseases and human health in New Zealand. Ecohealth 4(1): 72–81
Duncan C, Jones K, et al. (1996) Health-related behaviour in context: a multilevel modelling approach. Social Science & Medicine 42(6): 817–830
Duncanson M, Russell N, et al. (2000) Rates of notified cryptosporidiosis and quality of drinking water supplies in Aotearoa, New Zealand. Water Research 34(15): 3804–3812
Grinberg A, Pomroy WE, et al. (2011) Retrospective cohort study of an outbreak of cryptosporidiosis caused by a rare Cryptosporidium parvum subgenotype. Epidemiology & Infection 139(Special Issue 10): 1542–1550
Hunter PR, Thompson RCA (2005) The zoonotic transmission of Giardia and Cryptosporidium. International Journal for Parasitology 35(11–12): 1181–1190
Jagai J, Griffiths J, et al. (2010) Patterns of protozoan infections: Spatiotemporal associations with cattle density. EcoHealth 7(1): 33–46
Jones BA, Grace D, et al. (2013) Zoonosis emergence linked to agricultural intensification and environmental change. Proceedings of the National Academy of Sciences 110(21): 8399–8404
Jones KE, Patel NG, et al. (2008) Global trends in emerging infectious diseases. Nature 451(7181): 990–993
Kotloff KL, Blackwelder WC, et al. (2012) The Global Enteric Multicenter Study (GEMS) of diarrheal disease in infants and young children in developing countries: epidemiologic and clinical methods of the case/control study. Clin Infect Dis 55 Suppl 4: S232–245
Lal A (2014) Evaluating the Environmental and Social Determinants of Enteric Disease in New Zealand. Doctor of Philosophy, Univesity of Otago.
Learmonth J, Ionas G, et al. (2001) Seasonal shift in Cryptosporidium parvum transmission cycles in New Zealand. Journal of Eukaryotic Microbiology 48(Suppl): 34S–35S
Learmonth J, Ionas G, et al. (2003) Identification and genetic characterisation of Giardia and Cryptosporidium strains in humans and dairy cattle in the Waikato Region of New Zealand. Water Science and Technology 47(3): 21–26
MacLeod CJ, Moller H (2006) Intensification and diversification of New Zealand agriculture since 1960: An evaluation of current indicators of land use change. Agriculture, Ecosystems & Environment 115(1–4): 201–218
McCarthy ND, Gillespie IA, et al. (2012) Molecular epidemiology of human Campylobacter jejuni shows association between seasonal and international patterns of disease. Epidemiology and Infection 140(12): 2247–2255
Miller WA, Lewis DJ, et al. (2007) Climate and on-farm risk factors associated with giardia duodenalis cysts in storm runoff from california coastal dairiesv. Applied and Environmental Microbiology 73(21): 6972–6979
Moore D, Black M, et al. (2010) Cost benefit analysis of raising the quality of New Zealand networked drinking water., CH2M Beca Limited: 103
Murray KA, Allen T, et al. (2016) Emerging Viral Zoonoses from Wildlife Associated with Animal-Based Food Systems: Risks and Opportunities. In: Food Safety Risks from Wildlife, New York: Springer, pp 31–57
Odoi A, Martin S, et al. (2004) Investigation of clusters of giardiasis using GIS and a spatial scan statistic. International Journal of Health Geographics 3(1): 1–11
Pollock KGJ, Ternent HE, et al. (2009) Spatial and temporal epidemiology of sporadic human cryptosporidiosis in Scotland. Zoonoses and Public Health 57(7–8): 487–492
Salmond C, Crampton P, et al. (2006) NZDep2006 Index of deprivation user’s manual- research report, Wellington School of Medicine and Health Sciences
Sarkar R, Kattula D, et al. (2014) Risk factors for cryptosporidiosis among children in a semi urban slum in Southern India: a nested case-control study. The American Journal of Tropical Medicine and Hygiene 91(6): 1128–1137
Snel SJ, Baker MG, et al. (2009) A tale of two parasites: the comparative epidemiology of cryptosporidiosis and giardiasis. Epidemiology and Infection 137(11): 1641–1650
Snel SJ, MG Baker, et al. (2009) The epidemiology of cryptosporidiosis in New Zealand. New Zealand Medical Journal 122: 1290
StataCorp (2013) Stata Statistical Software: Release 13, College Station, Texas: StataCorp LP
Statistics New Zealand (2012) Agricultural Production Statistics: June 2012 (final)—Media Release. Retrieved 30 July, 2013, from http://www.stats.govt.nz/browse_for_stats/industry_sectors/agriculture-horticulture-forestry/AgriculturalProduction_final_MRJun12final.aspx
Statistics New Zealand (2012) New Zealand: An Urban/Rural Profile Update. Retrieved 30 July, 2013, from http://www.stats.govt.nz/browse_for_stats/people_and_communities/Geographic-areas/urban-rural-profile-update.aspx
Statistics New Zealand, A. (2010) Historical Population Estimates. Wellington, Government of New Zealand
Stefanogiannis N, McLean M, et al. (2001) Outbreak of cryptosporidiosis linked with a farm event. New Zealand Medical Journal 114(1144): 519–521
Taylor LH, Latham SM, et al. (2001) Risk factors for human disease emergence. Philosophical Transactions of the Royal Society B: Biological Sciences 356(1411): 983–989
Thorburn D (2011) Ruminant density, Verocytotoxigenic Escherichia Coli and cryptosporidiosis in New Zealand: Descriptive and ecological analyses, Dunedin: University of Otago
Wendt A, Kreienbrock L, et al. (2016) Joint use of Disparate Data for the Surveillance of Zoonoses: A Feasibility Study for a One Health Approach in Germany. Zoonoses and Public Health
Yoder JS, Wallace RM, et al. (2012) Cryptosporidiosis surveillance—United States, 2009–2010. Morbidity and mortality weekly report. Surveillance summaries (Washington, D.C.: 2002) 61(5): 1–12
Zambrano LD, Levy K, et al. (2014) Human diarrhea infections associated with domestic animal husbandry: a systematic review and meta-analysis. Transactions of the Royal Society of Tropical Medicine and Hygiene 108(6): 313–325
Zinsstag J, Roth F, et al. (2005) A model of animal–human brucellosis transmission in Mongolia. Preventive Veterinary Medicine 69(1): 77–95
Acknowledgment
This study was possible through A Lal’s salaried position at the Australian National University.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Author Simon Hales is a review editor for the journal.
Research Involving Human Rights
The authors assert that all the procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Electronic Supplementary Material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Lal, A., Dobbins, T., Bagheri, N. et al. Cryptosporidiosis Risk in New Zealand Children Under 5 Years Old is Greatest in Areas with High Dairy Cattle Densities. EcoHealth 13, 652–660 (2016). https://doi.org/10.1007/s10393-016-1187-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10393-016-1187-8