Abstract
Background
Several studies have established the association of various cancers with tobacco consumption. However, hardly any attempt has been made to examine the combined effect of various forms of tobacco consumption. Hence, the present study was undertaken to measure the overall risk of different cancer sites associated with various forms of tobacco used individually or in combination, and to investigate the risk variation within each site by different forms of use.
Methods
Meta-analysis was carried out on the findings of 22 published studies of samples exposed to tobacco use and control groups that were not exposed to tobacco. The pooled odds ratios (ORs) for each cancer for different combinations of forms of tobacco were calculated using a random effects model.
Results
Smoking was found to be associated with a 5-fold higher risk of oropharynx, larynx, and lung, a 3-fold higher risk of hypopharynx, and esophagus, and a 2-fold higher risk of oral cancer. Esophagus (OR = 3.5) and oral cancer were the only sites significantly associated with tobacco chewing. The OR associated with bidi smoking was highest for lung (6-fold) followed by esophagus (3.5-fold) and oral cancer (3-fold). Lung cancer was also significantly associated with cigarette smoking.
Conclusions
The present study reported pooled ORs for different tobacco-related cancers associated with various forms of tobacco use, both individually as well as in various combinations. Collecting data on the consumption of tobacco is a complex exercise. Pooled ORs reported in this study will be useful in working out the quantum of diverse tobacco-related cancers attributable to different forms of tobacco consumption, both individually as well as in combination.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Background
Globally, oral cancer, and cancer of the pharynx account for about 5% of all cancers in men (220,000 new cases every year) and 2% of cancers in women (90,000 new cases every year) (Parkin et al. 1999). Mortality rates due to oral and other types of tobacco-related cancer (hypo pharynx, pharynx, lung, larynx etc.) vary widely across regions, but prevalence and rates of incidence are highest in developing countries such as India, Pakistan, and Bangladesh, where these (oral and other tobacco-related cancers) are the most common forms of cancer (Bhurgri et al. 2000; Parkin et al. 1997). Epidemiological evidence about the association between cigarette smoking and cancer first came into light in 1920, and its causal relationship with lung cancer was established in 1950 (Doll and Hill 1964; IARC 1986; Levin et al. 1950; Sinha et al. 2002). In 1985, an international working group of experts from the International Agency for Research on Cancer (IARC) also recognized the causal relationship between smoking tobacco and cancer of the pharynx, larynx, lung, and urinary bladder, and oral cancer (IARC 1986).
A large number of people consume smokeless tobacco and suffer from severe related health hazards, such as oral cancer, uterine cervical cancer, etc. (Parkin et al. 2002; Warnakulasuriya 2009). The majority of smokeless tobacco users (over 90%) live in Southeast Asian countries. Within this region, India is one of the largest producers and consumers of smokeless tobacco, where its use among 15–49 year-olds has steadily increased from 19% in 1998 to 25% in 2010, despite the adoption of stringent policy actions for controlling tobacco consumption (Awan et al. 2014).
In India, the prevalence of chewing tobacco and smoking varies widely across the states and shows a strong association with regional sociocultural characteristics. According to the third round of the National Family Health Survey, men in the age group 15–49 years are more prone to tobacco use than women; 57% of men, as compared to 11% of women, use some form of tobacco. One third of men smoke cigarettes or bidis, and 37% consume paan (betel quid), gutkha and paan masala substitutes, or other forms of chewing tobaccos (Bhojani et al. 2009). Moreover, the pattern of tobacco consumption in India is probably more diverse than any other country in the world, which is the reason for the regional variations in the consequential burden of tobacco-related diseases and deaths (Sinha et al. 2002). Bidi smoking is one of the earliest forms of tobacco consumption; it is practiced mostly by people belong to the lower strata of Indian society (Rahman and Fukui 2000).
The number of tobacco-attributable deaths worldwide in the late 1980s was estimated to be 630,000 per year (Conrad et al. 1992). Today, conservative estimates of tobacco-attributable deaths are between 800,000 and 900,000 per year. The major challenge for India is that it has the highest rates of oral cancer in the world, accounting for 12% of all cancers in men and 8% in women. This is partly because of the easy availability of tobacco products—smokeless, as well as for smoking. Nearly 4.5 million Indian smokers are afflicted by heart disease or angina every year, and nearly 3.9 million people develop lung diseases. Nearly half of all cancers in men are tobacco-related, while over 60% of those who are less than 40 years of age, and suffering from heart disease, are smokers. In India, there are also an estimated 12 million cases of preventable illnesses that are attributed to tobacco use (Chaudhry et al. 2001). The World Health Organization predicts that deaths related to tobacco use in India may exceed 1.5 million annually by 2020 (Stroup et al. 2000).
Although several studies, epidemiological as well as experimental, have found a significant association between tobacco (smokeless and smoking) and several types of cancers, there has been no attempt at a systematic review of this major health issue. In an endeavor to address this gap, this study undertook a meta-analysis to quantify the overall risk of different cancer sites associated with various forms of tobacco use individually or in combination, and to examine the variation in risk at each site for different forms of tobacco use.
Material and methods
Selection of major tobacco-related cancers
In India, the National Cancer Registry Programme (NCRP) of the Indian Council of Medical Research (ICMR) has listed ten sites (lip, tongue, mouth, esophagus, pharynx, hypopharynx, pharynx unspecified, larynx, lung, and urinary bladder) as being associated with tobacco use. Lung, esophagus, and mouth cancer are the leading sites in 11, eight, and seven registries respectively, with their contribution relative to total cancers varying according to registry (NCRP 2016). These cancers are highly associated with tobacco use in both the developing world and the developed world. There are some studies in India, and many in developed countries, which showed these sites to be significantly associated with forms of tobacco use. Of these studies, all those which were freely accessible and conducted in India on oral, lung, larynx, esophagus, hypopharynx, and oropharynx cancers have been taken into account. They are presented in Figs. 2, 3, 4, 5, 6, and 7, with their separate and combined risk analyzed by a random effect model.
Literature search
A literature search was conducted using Scopus, the Science Direct database and Google Scholar for locating and accessing articles related to the forms of cancer associated with tobacco-chewing, bidi, and cigarette smoking, and which were published before April 2017. The keywords used for the search were bidi, cigarette, smoking, smokeless, chewing, oral, oral cavity, oropharynx, esophagus, larynx, hypopharynx, lung cancer, and India. Only those that were published as full-length articles and in English were considered for this study. The references listed in these articles were also accessed for additional support.
Inclusion and exclusion criteria
Studies were considered for meta-analysis if they pertained to associations between various forms of tobacco use (as exposure variables) and one or more of various kinds of cancer (oral, oropharynx, esophagus, larynx, hypopharynx, and lung) as outcome variables. Only those studies that allowed 2 × 2 tables to estimate ORs at 95% confidence intervals (CIs) were included in the meta-analysis. The following selection criteria were also applied to the studies:
They must have a case–control study design;
They must have reported 2 × 2 contingency tables for recalculating ORs and their corresponding 95% CIs of cancers related to bidi and cigarette smoking, and chewing tobacco consumption, separately.
Studies of mixed (smoking and chewing tobacco) were excluded if the effects of forms of tobacco use could not be shown separately, as well as those in which categories of case and control were not reported, which disallowed adequate classification of intake. Additionally, full-length reports that could not be accessed in English were also excluded. Overall, this study included only those articles that provided detailed information on both outcomes and forms of tobacco consumption.
A flow chart of the study selection process along with numbers selected and excluded at different levels appears in Fig. 1.
Data extraction
The epidemiological guidelines of observational studies for meta-analysis (Jussawalla and Deshpande 1971) were followed. From each study, the following information was extracted: (1) first author’s last name, (2) year of publication, (3) number of exposed with different forms of tobacco consumption in cases and control, and (4) cancer sites (oral, oropharynx, esophagus, larynx, hypopharynx, and lung), for recalculating ORs as risks and corresponding 95% CIs for bidi, cigarette, and smoking and chewing tobacco separately.
Statistical analysis
For each study, 2 × 2 contingency tables were constructed to recalculate OR and the 95% CI by following the standard procedure. Separate contingency tables were developed for chewing tobacco, and bidi/cigarette smoking if data was available in the same article. The overall OR (combined for all existing case–control studies for making 2 × 2 contingency tables) and its 95% CI was calculated by using the random effects model for tobacco-chewing, bidi, and cigarette smoking, because the data used in the meta-analysis were assumed to be a random selection from all possible studies examining the association between exposure and outcomes.
The studies are hospital-based case–control and nested case–control types that were carried out in India. This is significant because of the diverse patterns of tobacco consumption in India. A forest plot was prepared using STATA-12 statistical software to describe individual studies and pooled ORs. Heterogeneity between studies was indicated by the I2 value. I2 statistics of less than 50% were considered as low and indicating a greater degree of similarity between studies. Statistical significance was set at a p value less than 5%.
Results
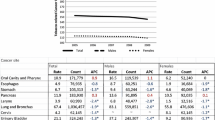
Twenty-two published articles (Balaram et al. 2002; Dar et al. 2012; Das et al. 2014; Dikshit and Kanhere 2000; Gajalakshmi et al. 2003; Ganesh et al. 2011; Ihsan et al. 2014; Jussawalla and Jain 1979; Kapil et al. 2005; Madani et al. 2010; Mahapatra et al. 2015; Nandakumar et al. 1996; Nandakumar et al. 1990; Notani and Sanghvi 1974; Phukan et al. 2001; Phukan et al. 2014; Petti et al. 2013; Sapkota et al. 2007; Sehgal et al. 2012; Talukdar et al. 2013; Wasnik et al. 1998; Znaor et al. 2003) that met the eligibility criteria for this study and dealt with the association of tobacco consumption with one or more of six cancers (oral, oropharynx, esophagus, larynx, hypopharynx, and lung) were included in the study. The number of studies available was highest for esophageal (eight studies) followed by oral (seven studies) and lung cancer (six studies). All these sites were reported to be highly significantly associated with tobacco consumption. ORs pooled for different forms of tobacco consumption were around three,with a highest OR of 3.6 for oropharyngeal and lowest of 2.7 for esophageal cancer. There was a high degree of divergence among the studies dealing with different sites, with the index of heterogeneity being more than 90% (Table 1). Detailed results for individual cancer sites under study are presented in the following sections.
Oral cancer (Fig. 2)
All seven studies dealing with oral cancer reported its association with chewing and all reported a statistically significant association, with OR ranging between 4.4 and 8.5. ORs pooled for all seven studies were 6.6, with a 95% CI of 5.2 to 8.4.
Four studies reported a correlation between oral cancer and bidi smoking, and three of them reported statistically significant ORs ranging between 2.5 and 6.9. The pooled OR was 2.9 which was statistically significant, with a 95% CI of 1.5 to 5.4.
Four studies dealt with an association with cigarette smoking, and none of them reported a significant association with protective effect. Thus, there was no evidence of cigarette smoking being associated with oral cancer.
A linkage with smoking in general (without specifying type) was reported by five of the studies. It was significant in all of them, with OR being 1.5 to 3. The pooled OR was 2, with a 95% CI of 1.5 to 2.5.
Oropharynx cancer (Fig. 3)
All of the three studies dealing with oropharyngeal cancer reported its association with chewing; in two of them it was statistically significant. Pooled OR for all three studies was 2.49, with a 95% CI of 0.96 to 6.48.
As far as smoking is concerned, there was no study in the Indian context dealing with an association between oropharynx cancer and bidi or cigarette smoking separately. However, an association with smoking in general was reported by three studies. It was significant in all three studies, with ORs ranging between 2.12 and 9.28. The pooled OR was 5.26, with a 95% CI of 2.28 to 12.14.
Hypopharynx cancer (Fig. 4)
Both of the studies dealing with hypopharyngeal cancer reported a statistically significant association with chewing. However, the pooled OR of 2.59 was not statistically significant.
There was no study in an Indian context dealing with the association of hypopharyngeal cancer and bidi or cigarette smoking separately. An association with smoking in general was reported as significant by both studies, with an OR ranging between 2.44 and 4.28. The pooled OR was 3.36, with a 95% CI of 1.95 to 5.79.
Esophagus cancer (Fig. 5)
Seven of eight studies analyzed the association either for only males or for both sexes taken together, whereas one study reported the analysis for males and females separately. Thus there were nine investigations into the association of esophageal cancer with different forms of tobacco use. All of the nine analyses investigated the association with tobacco chewing, and eight of them reported a significant association, with ORs ranging between 2.44 and 6.10. The pooled OR for all nine studies was 3.46, with a 95% CI of 2.83 to 4.22.
Bidi smoking was stated by four studies to be significantly associated, with ORs varying from a low of 2.76 to a high of 12.08. The pooled OR was 3.63, with a 95% CI of 2.41 to 5.45.
An association with cigarette smoking was also reported by four studies, and two of them reported a significant association with OR from 2.11 to 3.59. The pooled OR was 1.17, with a 95% CI between 0.65 and 2.08.
All nine studies dealing with tobacco consumption studied the role of smoking in general without specifying the type, and eight of them reported a significant association, with a low variation in ORs. ORs ranged from a low of 2.05 to a high of 4.50. The pooled OR was 2.67, with a 95% CI of 2.06 to 3.47.
Larynx cancer (Fig. 6)
All three studies dealing with laryngeal cancer reported its association with chewing, but only one of them was found to be statistically significant. The OR pooled for these three studies was 1.42, with a 95% CI of 0.69 to 2.90.
There was no study in the Indian context dealing with an association between laryngeal cancer and bidi or cigarette smoking separately. An association with smoking in general was reported by all three studies, with ORs ranging between 4.54 and 7.47. The pooled OR was 5.47, with a 95% CI of 4.01 to 7.46.
Lung cancer (Fig. 7)
Four of the studies investigated the association between lung cancer and tobacco chewing, but only one of them reported a significant association. The pooled OR was not statistically significant.
Bidi smoking was reported by all four studies to be significantly associated, with ORs varying from a low of 2.2 to a high of 11. The pooled OR was 5.9, with a 95% CI of 2.7 to 13.1.
An association with cigarette smoking was also reported by all four studies, and three of them reported a significant association, with ORs from 1.8 to 6.4. The pooled OR was 2.2, with a 95% CI ranging from 1.2 to 3.8.
All six studies dealing with tobacco consumption studied the role of smoking in general, without specifying the type, and all of them reported a significant association; however there was a high variation in ORs, ranging from a low of 1.8 to a high of 15.8. The pooled OR was 5.1, with a 95% CI of 2.4 to 10.7.
Findings
Table 2 summarizes the findings of our study in the form of ORs of different tobacco-related sites of cancer associated with various types of tobacco consumption. The risk of oral cancer is about seven times higher among chewers and three times higher among bidi smokers. Similarly, the risk of esophageal cancer is about four and three times higher among chewers and bidi smokers respectively. These two sites are not significantly associated with cigarette smoking. On the other hand, four other sites under study, namely, oropharynx, hypopharynx, larynx, and lung, were also significantly associated with smoking and not only with chewing. The risk for lung cancer associated with bidi smoking was around six times higher.
Discussion
Chewing and smoking tobacco are among the most well-established causes of various forms of cancer. The magnitude of risks varied from study to study, and was calculated based on extracted information about case and control among both exposed and non-exposed individuals and different forms of tobacco consumption. Information on case and control was obtained from a systematic review of published articles. The objective of the study was to arrive at a reasonably accurate assessment, based on the various methods of sampling and analysis in the articles studied, of the risks of cancers due to tobacco consumption. The study used a random effect model, with the assumption that each study used randomly selected samples for analysis. The high heterogeneity observed in the studies of each cancer type was due to the different periods in which the studies were carried out, and the diversity of locations, cultures and economic status.
Many systematic reviews have been carried out regarding the association between chewing tobacco and oral cancer in the developing and developed worlds (Awan and Patil 2016; Bhawna 2013; Boffetta et al. 2008; Critchley and Unal 2003; Guha et al. 2014; Gupta and Ray 2003; Gross et al. 1995; Khan et al. 2014; Lee and Hamling 2009). Among them, a study by Gupta et al. is regarded as one of the most extensive. It reported a high pooled OR for oral cancer (Lee and Hamling 2009), and found a significant association between chewing tobacco and oral cancer. The finding added strong evidence-based support to the IARC’s inclusion of chewing (smokeless) tobacco in the list of risk factors associated with oral cancer (Awan and Patil 2016; Khan et al. 2014). Awan and Patil found a 7-fold higher risk of oral cancers due to betel-quid chewing (Gupta and Ray 2003). A similar risk level was also observed for other types of chewing tobacco. The risk of oral cancer was higher among females, most likely because of the nature of their mucosa, which is more susceptible to spoil on exposure to tobacco, and/or lack of knowledge and awareness about tobacco use (Balaram et al. 2002; Lee and Hamling 2009). The causal relationship observed between exposure to chewing tobacco and oral cancer is consistent with IARC reports. However, a review of some studies in Europe and North America reported conflicting outcomes (Blot et al. 1988; Lee 2011; Weitkunat et al. 2007). This may be because of the differences in the types of smokeless tobacco available, and different environmental, ethnic and socioeconomic, conditions between South Asian and European/North American populations. Moreover, the duration of chewing habits may also play a part. It has been observed that a longer duration of chewing (exposure) is linked with a higher risk of oral cancer (Rahman et al. 2003).
Our meta-analysis indicates that bidi smokers have a 3-fold higher risk of oral cancer than non-smokers. However, the study did not find a significant relationship between cigarette-smoking and oral cancer. Another study also showed a significantly high association with bidi smoking but an insignificant one with cigarette smoking (Rahman et al. 2003). This is because of the toxicity, as measured by nicotine, tar carbon monoxide, hydrogen cyanide, ammonia, other volatile phenols, and carcinogenic hydrocarbons, benz[a]pyrene, benz[a]anthracine and radioactive uranium, which are higher in bidi smoke than cigarette smoke (Sankaranarayanan et al. 1991). Moreover, bidi wrappers are made from tendu leaves, which are less porous than cigarette paper and are also less combustible. This results in higher intake of tar, nicotine, and carbon monoxide (Narayan et al. 1996).
In India, 21% of urban and 42% of rural adult males choose to expose themselves to bidi smoking (Rahman and Fukui 2000), most of whom are from disadvantaged sections of the society. The pooled OR for cancer of the esophagus (3.6 times) and lung (5.9 times) are higher in bidi smokers than for other forms of tobacco consumed. Some other studies also indicate that bidi smoking has a greater OR than cigarette smoking in developing cancers of the lung, esophagus, and larynx and other chronic conditions (Humans 2012; Jayanta et al. 1983; Notani et al. 1977; Phukan et al. 2001; Petti et al. 2013; Sankaranarayanan et al. 1990; Znaor et al. 2003). Aggressive combating of bidi smoking is therefore necessary to prevent thousands of deaths from cancers associated with it.
The pooled OR of oropharynx, hypopharynx, larynx, and lung cancers had an insignificant association with chewing tobacco, while other forms of tobacco were significantly associated with them. However, Lee et al. reported a significant association between chewing tobacco and larynx cancer, while evidence in the IARC’s report and Western studies was equivocal (Lewin et al. 1998; Stockwell and Lyman 1986; Weitkunat et al. 2007; WHO 2011). Although our meta-analysis found a high OR and significant association between chewing and esophagus cancer, as Lee and Hamling also showed, there is an insignificant association on the basis of Western studies (Weitkunat et al. 2007). Meta-analysis showed that smoking tobacco has a high association with esophagus cancer. Heterogeneity among these studies was also higher than esophagus cancer associated with use of chewing tobacco. This variation might be due to small and insignificant associations with cigarette smoking and/or socioeconomic inequality.
The present study also showed a definite association between smoking tobacco and oral, oropharynx, hypopharynx, esophagus, larynx, and lung cancers. The proportion of bidi users in this group is high. Most bidi smokers belong to the vulnerable lower socioeconomic groups in India and cancer pushes them even further into poverty. These groups are often not able to access appropriate treatment, which exacerbates their situation.
Strict implementation of effective tobacco control measures can prevent globally about 900,000 deaths per year associated with smoking and smokeless (chewing) tobacco. Our meta-analysis also found a high and significant association between smoking and lung cancer (OR = 5.1; CI 2.40–10.71). This supports WHO estimates that smoking is the cause of over 70% of lung cancers (WHO 2011). The findings of this study will help to generate and raise awareness, educate the masses, and inform policy makers when taking the necessary actions to combat rampant tobacco use. Smoking and smokeless tobacco are both dangerous for health.
Conclusions
This study has reported pooled ORs for different tobacco-related cancers associated with different forms of tobacco use, both individually as well as in different combinations. Collecting data on the consumption of tobacco is a complex phenomenon. Pooled ORs reported in this study will be useful in working out the quantum of various tobacco-related cancers attributable to different forms of tobacco consumption, both individually as well as in combination. In addition, it may be concluded from pooled ORs that chewing and bidi smoking were responsible for the large burden of oral and esophagus cancers. For lung cancer, bidis were more significantly linked than cigarettes. The study also confirms the insignificant association of chewing tobacco with larynx and lung cancer.
References
Awan KH, Patil S (2016) Association of smokeless tobacco with oral cancer—evidence from the South Asian studies: a systematic review. J Coll Physicians Surg Pak 26(9):775–780
Awan KH, Khang TW, Yee TK, Zain RB (2014) Assessing oral cancer knowledge and awareness among Malaysian dental and medical students. J Cancer Res Ther 10(4):903
Balaram P, Sridhar H, Rajkumar T, Vaccarella S, Herrero R, Nandakumar A, Ravichandran K, Ramdas K, Sankaranarayanan R, Gajalakshmi V (2002) Oral cancer in southern India: the influence of smoking, drinking, paan-chewing and oral hygiene. Int J Cancer 98(3):440–445
Bhawna G (2013) Burden of smoked and smokeless tobacco consumption in India—results from the Global Adult Tobacco Survey India (GATS-India) — 2009–2010. Asian Pac J Cancer Prev 14(5):3323–3329
Bhojani U, Chander S, Devadasan N (2009) Tobacco use and related factors among pre-university students in a college in Bangalore, India. Accessed 2 Dec 2017
Bhurgri Y, Bhurgri A, Hassan SH, Zaidi S, Rahim A, Sankaranarayanan R, Parkin DM (2000) Cancer incidence in Karachi, Pakistan: first results from Karachi cancer registry. Int J Cancer 85(3):325–329
Blot WJ, McLaughlin JK, Winn DM, Austin DF, Greenberg RS, Preston-Martin S, Bernstein L, Schoenberg JB, Stemhagen A, Fraumeni JF (1988) Smoking and drinking in relation to oral and pharyngeal cancer. Cancer Res 48(11):3282–3287
Boffetta P, Hecht S, Gray N, Gupta P, Straif K (2008) Smokeless tobacco and cancer. Lancet Oncol 9(7):667–675
Chaudhry K, Prabhakar A, Prabhakaran P, Prasad A, Singh K, Singh A (2001) Prevalence of tobacco use in Karnataka and Uttar Pradesh in India. Final report of the study by the Indian Council of Medical Research and the WHO South East Asian Regional Office, New Delhi. Accessed 20 Dec 2017
Conrad KM, Flay BR, Hill D (1992) Why children start smoking cigarettes: predictors of onset. Addiction 87(12):1711–1724
Critchley JA, Unal B (2003) Health effects associated with smokeless tobacco: a systematic review. Thorax 58(5):435–443
Dar N, Bhat G, Shah I, Iqbal B, Kakhdoomi M, Nisar I, Rafiq R, Iqbal S, Bhat A, Nabi S (2012) Hookah smoking, nass chewing, and oesophageal squamous cell carcinoma in Kashmir, India. Br J Cancer 107(9):1618–1623
Das M, Sharma SK, Sekhon GS, Saikia BJ, Mahanta J, Phukan RK (2014) Promoter methylation of MGMT gene in serum of patients with esophageal squamous cell carcinoma in North East India. Asian Pac J Cancer Prev 15(22):9955–9960
Dikshit RP, Kanhere S (2000) Tobacco habits and risk of lung, oropharyngeal and oral cavity cancer: a population-based case-control study in Bhopal, India. Int J Epidemiol 29(4):609–614
Doll R, Hill AB (1964) Mortality in relation to smoking: ten years' observations of British doctors. Br Med J 1(5395):1399
Gajalakshmi V, Hung RJ, Mathew A, Varghese C, Brennan P, Boffetta P (2003) Tobacco smoking and chewing, alcohol drinking and lung cancer risk among men in southern India. Int J Cancer 107(3):441–447
Ganesh B, Sushama S, Monika S, Suvarna P (2011) A case–control study of risk factors for lung cancer in Mumbai, India. Asian Pac J Cancer Prev 12(2):357–362
Gross A, Lackland D, Tu D (1995) Oral cancer and smokeless tobacco: literature review and meta-analysis. Environ Int 21(4):381–394
Guha N, Warnakulasuriya S, Vlaanderen J, Straif K (2014) Betel quid chewing and the risk of oral and oropharyngeal cancers: a meta-analysis with implications for cancer control. Int J Cancer 135(6):1433–1443
Gupta PC, Ray CS (2003) Smokeless tobacco and health in India and South Asia. Respirology 8(4):419–431
IARC Working Group on the Evaluation of Carcinogenic Risks to Humans (2012) Pharmaceuticals. Volume 100 a. a review of human carcinogens. IARC Monogr Eval Carcinog Risks Hum 100(PT A):1
IARC (1986) Tobacco smoking. IARC Monogr Eval Carcinog Risk Chem Hum 38:35–394
Ihsan R, Chauhan PS, Mishra AK, Singh L, Sharma JD, Zomawia E, Verma Y, Kapur S, Saxena S (2014) Copy number polymorphism of glutathione-S-transferase genes (GSTM1 & GSTT1) in susceptibility to lung cancer in a high-risk population from north-east India. Indian J Med Res 139(5):720
Jayanta K, Notani P, Sanghvi L (1983) Health consequences of smoking in two socioeconomic classes in Bombay, India. In: Proceedings of 5th World Conference on Smoking and Health, 1983, pp 149–156
Jussawalla D, Deshpande V (1971) Evaluation of cancer risk in tobacco chewers and smokers: an epidemiologic assessment. Cancer 28(1):244–252
Jussawalla D, Jain D (1979) Lung cancer in Greater Bombay: correlations with religion and smoking habits. Br J Cancer 40(3):437
Kapil U, Singh P, Bahadur S, Dwivedi SN, Singh R, Shukla N (2005) Assessment of risk factors in laryngeal cancer in India: a case-control study. Asian Pac J Cancer Prev 6(2):202–207
Khan Z, Tönnies J, Müller S (2014) Smokeless tobacco and oral cancer in South Asia: a systematic review with meta-analysis. J Cancer Epidemiol 2014:394696
Lee PN (2011) Summary of the epidemiological evidence relating snus to health. Regul Toxicol Pharmacol 59(2):197–214
Lee PN, Hamling J (2009) Systematic review of the relation between smokeless tobacco and cancer in Europe and North America. BMC Med 7(1):36
Levin ML, Goldstein H, Gerhardt PR (1950) Cancer and tobacco smoking: a preliminary report. J Am Med Assoc 143(4):336–338
Lewin F, Norell SE, Johansson H, Gustavsson P, Wennerberg J, Biörklund A, Rutqvist LE (1998) Smoking tobacco, oral snuff, and alcohol in the etiology of squamous cell carcinoma of the head and neck. Cancer 82(7):1367–1375
Madani AH, Jahromi AS, Madhurima D, Debanshu B (2010) Risk assessment of tobacco types and oral cancer. Am J Pharmacol Toxicol 5(1):9–13
Mahapatra S, Kamath R, Shetty BK, Binu V (2015) Risk of oral cancer associated with gutka and other tobacco products: a hospital-based case–control study. J Cancer Res Ther 11(1):199
Nandakumar A, Thimmasetty K, Sreeramareddy NM, Venugopal T (1990) A population-based case-control investigation on cancers of the oral cavity in Bangalore, India. Br J Cancer 62(5):847
Nandakumar A, Anantha N, Pattabhiraman V, Prabhakaran P, Dhar M, Puttaswamy K, Venugopal T, Reddy N (1996) Importance of anatomical subsite in correlating risk factors in cancer of the oesophagus—report of a case–control study. Br J Cancer 73(10):1306
Narayan KV, Chadha S, Hanson R, Tandon R, Shekhawat S, Fernandes R, Gopinath N (1996) Prevalence and patterns of smoking in Delhi: cross sectional study. BMJ 312(7046):1576–1579
National Cancer Registry Programme (NCRP) (2016) Three-year report of the population based cancer registries: 2012–2014, Indian Council of Medical Research, New Delhi, India. Accessed 16 Feb 2017
Notani P, Sanghvi L (1974) A retrospective study of lung cancer in Bombay. Br J Cancer 29(6):477
Notani P, Rao D, Sirsat M, Sanghvi L (1977) A study of lung cancer in relation to bidi smoking in different religious communities in Bombay. Indian J Cancer 14(2):115
Parkin D, Whelan S, Ferlay J, Raymond L, Young J (1997) Cancer incidence in five continents, Vol VII. IARC Scientific Publications, Lyon. Accessed 20 Jan 2017
Parkin DM, Pisani P, Ferlay J (1999) Estimates of the worldwide incidence of 25 major cancers in 1990. Int J Cancer 80(6):827–841
Parkin D, Whelan S, Ferlay J, Teppo L, Thomas D (2002) Cancer incidence in five continents, Vol. VIII. IARC Scientific Publications, Lyon. Accessed 20 Jan 2017
Petti S, Masood M, Scully C (2013) The magnitude of tobacco smoking–betel quid chewing–alcohol drinking interaction effect on oral cancer in South-East Asia. A meta-analysis of observational studies. PLoS One 8(11):e78999
Phukan R, Ali M, Chetia C, Mahanta J (2001) Betel nut and tobacco chewing; potential risk factors of cancer of oesophagus in Assam, India. Br J Cancer 85(5):661
Phukan RK, Borah PK, Saikia BJ, Das M, Sekhon GS, Mahanta J (2014) Interaction of tobacco smoking and chewing with angiotensin converting enzyme (insertion/deletion) gene polymorphisms and risk of lung cancer in a high risk area from Northeast India. Asian Pac J Cancer Prev 15(24):10691–10695
Rahman M, Fukui T (2000) Bidi smoking and health. Public Health 114(2):123–127
Rahman M, Sakamoto J, Fukui T (2003) Bidi smoking and oral cancer: a meta-analysis. Int J Cancer 106(4):600–604
Sankaranarayanan R, Duffy SW, Nair MK, Padmakumary G, Day NE (1990) Tobacco and alcohol as risk factors in cancer of the larynx in Kerala, India. Int J Cancer 45(5):879–882
Sankaranarayanan R, Duffy SW, Padmakumary G, Nair SM, Day NE, Padmanabhan T (1991) Risk factors for cancer of the oesophagus in Kerala, India. Int J Cancer 49(4):485–489
Sapkota A, Gajalakshmi V, Jetly DH, Roychowdhury S, Dikshit RP, Brennan P, Hashibe M, Boffetta P (2007) Smokeless tobacco and increased risk of hypopharyngeal and laryngeal cancers: a multicentric case–control study from India. Int J Cancer 121(8):1793–1798
Sehgal S, Kaul S, Gupta B, Dhar M (2012) Risk factors and survival analysis of the esophageal cancer in the population of Jammu, India. Indian J Cancer 49(2):245
Sinha D, Gupta P, Pednekar M, Jones J, Warren C (2002) Tobacco use among school personnel in Bihar, India. Tob Control 11(1):82–83
Stockwell HG, Lyman GH (1986) Impact of smoking and smokeless tobacco on the risk of cancer of the head and neck. Head Neck 9(2):104–110
Stroup DF, Berlin JA, Morton SC, Olkin I, Williamson GD, Rennie D, Moher D, Becker BJ, Sipe TA, Thacker SB (2000) Meta-analysis of observational studies in epidemiology: a proposal for reporting. JAMA 283(15):2008–2012
Talukdar FR, Ghosh SK, Laskar RS, Mondal R (2013) Epigenetic, genetic and environmental interactions in esophageal squamous cell carcinoma from Northeast India. PLoS One 8(4):e60996
Warnakulasuriya S (2009) Global epidemiology of oral and oropharyngeal cancer. Oral Oncol 45(4):309–316
Wasnik KS, Ughade SN, Zodpey SP, Ingole D (1998) Tobacco consumption practices and risk of oro-pharyngeal cancer: a case–control study in Central India. Southeast Asian J Trop Med Public Health 29(4):827–834. Accessed 26 Jan 2017
Weitkunat R, Sanders E, Lee PN (2007) Meta-analysis of the relation between European and American smokeless tobacco and oral cancer. BMC Public Health 7(1):334
WHO (2011) Global status report on noncommunicable diseases 2010. World Health Organization, Geneva. Accessed 18 Jan 2017
Znaor A, Brennan P, Gajalakshmi V, Mathew A, Shanta V, Varghese C, Boffetta P (2003) Independent and combined effects of tobacco smoking, chewing and alcohol drinking on the risk of oral, pharyngeal and esophageal cancers in Indian men. Int J Cancer 105(5):681–686
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Availability of supporting data
This meta-analysis study was based on secondary data sources (published studies).
Competing interests
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Prasad, J., Dhar, M. Risk of major cancers associated with various forms of tobacco use in India: a systematic review and meta-analysis. J Public Health (Berl.) 27, 803–813 (2019). https://doi.org/10.1007/s10389-018-0992-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10389-018-0992-7