Abstract
Background
The prevalence of tobacco use among various cancer types in Iran remains a significant concern, necessitating a comprehensive analysis to understand the extent and patterns of consumption. This study aimed to systematically review and analyze existing literature to delineate the prevalence of tobacco use across different cancer types in Iran, thereby providing a robust basis for future interventions and policy formulations.
Methods
Adhering to the PRISMA guidelines, we conducted a systematic review and meta-analysis of literature available in PubMed and Scopus databases. The initial search identified 351 records, out of which 44 studies were selected based on their relevance and design. These studies spanned various time frames, starting from the 2001s up until 2022, and encompassed diverse geographical locations and cancer types in Iran. To avoid bias and potential data overlap, we opted to incorporate a single comprehensive study from the Golestan Cohort, encompassing all data, while excluding 10 other studies. Our final analysis incorporated data from 34 studies, which accounted for 15,425 patients and 5,890 reported smokers. Statistical analyses were performed to calculate the overall proportion of tobacco consumption and to conduct subgroup analyses based on different variables such as cancer types, gender, geographical locations, and types of tobacco used.
Results
The analysis revealed a substantial prevalence of tobacco use among cancer patients in Iran, with an overall consumption rate of 43%. This rate varied significantly, ranging from 10 to 88% across individual studies. Subgroup analyses further highlighted disparities in tobacco consumption rates across different demographics, geographic areas, and cancer types. Notably, the ‘ever’ smokers category exhibited the highest prevalence of tobacco use. The study also identified a worrying trend of high cigarette smoking rates, along with variable consumption patterns of other forms of tobacco, including waterpipe, ‘Naas’, and ‘Pipe’.
Conclusions
This systematic review and meta-analysis underscores a significant association between tobacco consumption and various cancer types in Iran, with a prevalence rate among cancer patients being three times higher than the average Iranian population. The findings indicate substantial heterogeneity in tobacco use patterns, emphasizing the need for targeted interventions to address this pressing health issue. The study serves as a critical resource for shaping future policies and strategies aimed at curbing tobacco use and mitigating its adverse effects on cancer prevalence in Iran.
Similar content being viewed by others
Introduction
Cancer is the second group of chronic non-communicable disease and ranks as the third most prevalent source of mortality in Iran [1]. Five prevalent types of cancer that affect Iranian men include stomach, prostate, bladder, colorectal, and esophagus. On the other hand, for Iranian women, the most common types of cancer are breast, colorectal, stomach, esophagus, and thyroid [2]. It is noteworthy that there is a discernible upward trajectory in the frequency and fatality rate of the majority of cancers in Iran [3].
Smoking in individuals results in a significant elevation of cancer risk, and it has been confirmed that tobacco smoke contains over 60 well-established carcinogens [4]. Tobacco smoking is a causative agent for multiple types of cancers that affect various parts of the human anatomy, including but not limited to the oral cavity, lung, pharynx, esophagus, kidney, colon, stomach, pancreas, bladder, rectum, liver, larynx, cervix, ureter, and bone marrow [5]. Despite being diagnosed with cancer, the continuation of tobacco use has been found to significantly elevate the likelihood of experiencing treatment-related toxicities, recurrence of cancer, morbidity, and mortality [6].
Smoking is known to elevate the concentration of carbon monoxide in the blood, leading to a reduction in the pulmonary air capacity. Consequently, smokers experience premature exhaustion in contrast to their non-smoking counterparts [7]. According to estimates, smoking is responsible for the untimely deaths of over fifty percent of individuals who engage in it over a prolonged period of time [8]. The mortality rate among individuals who smoke cigarettes across all age cohorts is observed to be 2–3 times greater compared to those who do not partake in smoking [9].
Diagnosing and treating cancer can lead to rapid cessation of smoking so that those with smoking-related cancers are more likely to quit [10]. The evidence pertaining to smoking and its correlation with cancer holds significant ramifications for public health with regards to the prevention of cancer, a condition that could potentially be rectified through the modification of individual behavioral patterns [11, 12]. The alteration in individuals' manner of living and environment can potentially impact the epidemiological trends pertaining to distinct forms of cancer [13]. According to the fact that smoking constitutes the most significant avoidable factor leading to cancer in multiple nations, the considerable shifts in smoking incidence in Iran necessitate a reevaluation of the present condition of malignancies related to tobacco [14]. Therefore, we conducted a comprehensive examination of the existing literature through a systematic review and meta-analysis of the prevalence of tobacco exposure in population who suffer from cancer in Iran.
Methods
We have meticulously adhered to the Guidelines for Accurate and Transparent Health Estimates Reporting, as well as to the rigorous standards outlined in the Preferred Reporting Items for Systematic Reviews and Meta-Analyses [15, 16].
Search strategy
We performed a comprehensive search to find studies published electronically between 21/03/2001 and 28/01/2023, based on articles available in Pubmed and Scopus databases. keywords and the Medical Subject Heading (MeSH) terms included Cigarette OR “Tobacco” OR “Pipe” OR “Cigar” OR “Hookah” AND Iran OR “Iranian” AND Cancer OR “Tumor” OR “Neoplasm” OR “Neoplasia” OR “Malignancy” OR “Malignancies” OR “Malignant” OR “Benign” Moreover, various types of observational studies, including cohort, cross-sectional, and case–control studies were considered.
Criteria for selection and evaluation of quality of the papers
The search process was executed by two authors, so that they could issue a definitive verdict after careful discussion. The relevant title and abstract of the papers have been carefully examined for having acceptable quality of papers using the STROBE checklist (Strengthening the Reporting of Observational Studies in Epidemiology). Data were extracted on description of cancer type, sample size, study province, study period and data collection method. The aim of this study was to determine the correlation between smoking and the development of cancer. Consequently, the inclusion criteria involved providing an accurate estimation of the frequency of tobacco use among Iranian cancer patients.
Data extraction
A form comprising of several sections was devised, and fundamental information necessary for the research was gathered. The required information involved the subject, title, journal’s name, and author, methodology and study design, prevalence of cigarette smoking among cancer patients, cancer type, study province, number of smokers by sex, and type of tobacco use.
Study risk of bias assessment
In order to evaluate the trustworthiness and applicability of the studies included in our review, we undertook a comprehensive assessment of the risk of bias. This process was independently carried out by two reviewers using the Newcastle–Ottawa Scale (NOS). This tool is specifically designed to scrutinize the quality of non-randomized studies, especially observational ones. It takes into consideration three broad aspects: the method of selection for study groups, the degree of comparability between these groups, and the determination of either the exposure or outcome of interest. The NOS allowed us to score each study based on these criteria, leading to classifications of low, high, or unclear risk of bias. In case of any disagreements between the two reviewers, the issue was discussed thoroughly until a mutual agreement was reached.
Data synthesis
Eligibility for each synthesis was determined based on how well the studies aligned with our pre-established inclusion criteria. We categorized studies according to their intervention characteristics, then compared these with the groups we had planned for each synthesis. All included studies in our analysis provided data on both smokers and non-smokers. Subgroup analyses were restricted to studies that specifically reported data for the relevant subgroups and those with missing data were not included. Forest plots, funnel plots, and risk of bias plots were utilized for the graphical representation and tabulation of individual studies and their syntheses.
Due to the high degree of heterogeneity among studies, we used a random effects model for meta-analysis with a random intercept logistic regression method [17]. Furthermore, mixed effect logistic regression models were used to analyze the effect of cigarette and cancer type alone and combined. We used the I2 statistic and the Chi2 test with a p-value less than 0.1 to identify statistical heterogeneity. To explore possible causes of heterogeneity, we carried out subgroup analyses based on factors such as cancer type, gender, geographical location and tobacco consumption habits. Furthermore, we performed sensitivity analyses to assess the stability of our synthesized results, whereby we sequentially removed each study and observed the resulting impact on the overall effect size.
Assessment of reporting bias
In order to gauge the potential bias arising from absent results, we employed Egger’s regression test and conducted a visual inspection of funnel plots for any signs of asymmetry. In theory, studies with significant effects should symmetrically surround the aggregated effect size. If there is any departure from this expected symmetry, it indicates a possible presence of publication bias.
Results
Study selection
We initiated our systematic review and meta-analysis procedure with the identification of 351 records from two databases: PubMed and Scopus. After this initial identification, we removed 103 duplicate records, leaving us with 248 unique records to be screened. All 248 records were carefully evaluated. However, 150 reports were not retrieved for a detailed evaluation as their titles and abstracts were found to be irrelevant to our research question. The remaining 98 reports were thoroughly assessed for their eligibility. After meticulous review and exclusion of reports that didn’t meet our criteria, we were left with 44 studies. Among these, 10 studies [18,19,20,21,22,23,24,25,26,27] were part of the Golestan Cohort. To avoid bias and potential data overlap, we decided to include only one comprehensive study by Sheikh et al. [28] from the Golestan Cohort that encapsulates the data of all 10 studies. A flow diagram detailing this process is included for further clarity (Fig. 1).
Study characteristics
The studies included in this systematic review and meta-analysis encompass various research designs, cancer types, data collection methods, geographical locations, and periods. These key characteristics are summarized in Table 1. In terms of study design, our review incorporated a mix of case–control studies, cross-sectional studies, and cohort studies. The majority of studies employed a case–control or cross-sectional design, with notable examples being Mahouri (2007), Abdolahinia (2021), Ahmadi (2012), and Akbari (2015) [29,30,31,32]. Cohort studies included in our review were Moghadam (2021), Rafati (2019), Samadi (2007), and Sheikh (2020), among others [28, 33,34,35]. Regarding cancer types, the studies focused on a variety of cancers. Some studies, like Mahouri (2007) and Rafati (2019), focused on breast cancer [29, 34], while others, such as Abdolahinia (2021), Ahmadi (2012), and Akbari (2015), investigated bladder cancer [30,31,32]. Several studies, like Hadji (2021) and Momtahen (2009), explored multiple cancer types [36, 37]. The provinces where the studies were conducted cover a broad geographical range across Iran, including Hormozgan, Kerman, Mazandaran, Shiraz, Golestan, Tehran, Fars, and others. A notable study by Hadji (2021) and Hosseini (2022) was conducted in 10 provinces [36, 38]. The study periods also varied widely, with some studies conducted as far back as the 2006s (Tabei, 2006) and as recent as 2022 (Hosseini, 2022) [38].
Syntheses
We included 34 studies with 15,425 patients and 5,890 smokers. The individual tobacco consumption proportions reported ranged from 10.00% (Momtahen et al., 2009) [37] to 82.00% (Masjedi et al., 2013) [48]. Based on study design, 6 cohort, 14 case–control and 14 cross-sectional studies were involved in our analysis. The analysis also considered various cancer types, including 4 bladder, 2 breast, 4 colorectal, 5 esophageal, 3 gastric, 1 gastrointestinal, 4 head and neck squamous cell (HNSC), 5 lung, 1 pancreatic, 2 upper gastrointestinal cancers were included in our analysis. Additionally, 3 studies considered multiple cancer types. The overall proportion of tobacco consumption across all studies, as per the random effects model, was found to be 43.29% (CI95% 35.42%-51.52%, τ2 = 0.86, I2 = 98.0%) (Fig. 2). The Egger’s test p-value was 0.064, suggesting that there was no strong evidence of publication bias, although the intercept value on the funnel plot was 3.57.
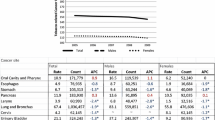
Associations between cancer types and tobacco use
Table 2 presents the outcomes from a comprehensive multiple logistic regression meta-analysis, focusing on the association between cancer type, cigarette smoking, and the prevalence of tobacco use among cancer patients. The analysis highlights a significant heterogeneity (I^2 = 93.792) and reveals distinct associations based on cancer type. The colorectal cancer is significantly associated with lower odds of tobacco use, while laryngeal cancer shows a contrary, positive association. Additionally, the influence of cigarette smoking on its own is significantly affirmed, and its interaction with cancer type elucidates a complex relationship, underscoring the multifaceted dynamics between cancer diagnoses, smoking habits, and their implications for patient health.
Subgroup analysis
The subgroup analysis, which categorizes studies by the type of cancer, showed varying percentages of tobacco consumption for each cancer type. The highest percentage of tobacco use was observed in the laryngeal cancer subgroup at 73.68% (57.63%-85.22%), albeit based on only one study. This was followed by lung cancer at 62.05% (47.00%-75.09%), bladder cancer at 53.74% (41.99%-65.08%) and head and neck cancer at 52.73% (26.80%-77.27%). Tobacco consumption was lower in esophageal cancer at 46.77% (21.35%-73.98%), breast cancer subgroup at 38.96% (12.64%-73.80%), gastric cancer at 36.80% (25.20%-50.16%), and CRC at 24.63% (14.46%-38.72%). The heterogeneity was also found to differ between these cancer type subgroups (τ2 = 0.7654; τ = 0.8749; I2 = 96.8%) (Fig. 3).
On the other hand, the analysis based on gender, encompassing a total of 2362 patients and 1382 smokers, revealed a significant difference in tobacco consumption rates. Overall estimated tobacco consumption was 70.22% (95%CI: 43.21%-87.96%) in men and 17.11% (95%CI: 3.04%-57.59%) (Fig. 4). The study by Saedi et al. (2009) [56] reported the highest rate of tobacco consumption at 90.70% (77.86%-97.41%) in women with esophageal cancer, while the study by Masjedi et al. (2013) [48] reported the highest tobacco consumption at 90.45% (85.15%-94.34%) in men with lung cancer. Conversely, the lowest for both sexes was reported by Aminisani et al. (2016) [40], standing at 21.65% (13.93%-31.17%) and 3.33% (0.41%-11.53%), in men and women with CRC, respectively.
In terms of geographical location, varying tobacco consumption rates were observed across different provinces of Iran. The studies reported a wide range of tobacco consumption proportions, from 10.00% (Momtahen et al., 2009) [37] to 88.30% Saedi et al. (2009) [56]. When the studies were collectively analyzed using a random effects model, the estimated overall rate of tobacco consumption was 41.50% (33.12%-50.41%). A subgroup analysis was conducted based on the province where each study was conducted. It showed a considerable variation in the rate of tobacco consumption across the provinces. For instance, the highest proportion of tobacco consumption was found in Sistan-baluchestan at 81.71%, while the lowest was recorded in North Khorasan at 25.00% (Fig. 5).
When divided based on tobacco consumption habits, the subgroups showed differences. The prevalence of cigarette smoking was notably high, with a proportion of 99.51% (91.16%—99.97%) across 15 studies. For waterpipe smoking, the prevalence was 18.09% (11.14%—28.01%) across seven studies, and other forms of tobacco use had a prevalence of 55.67% (0.65%—99.59%) across four studies. Usage of 'Naas' and 'Pipe' were evaluated in single studies and showed much lower prevalence rates, 2.71% (2.09%—3.51%) and 0.53% (0.03%—0.96%) respectively (Fig. 6).
Results of sensitivity analysis
When potential outliers identified through both dmetar and GOSH methods were removed, the overall proportion did not change considerably, remaining at 0.41. However, the 95% confidence interval narrowed to [0.37–0.45] and [0.35–0.47] respectively, and the heterogeneity decreased notably, with I^2 values of 0.71 and 0.96 respectively. This suggests the overall result was robust but the heterogeneity was driven by a few outlying studies (Table 3).
Discussion
Our comprehensive systematic review and meta-analysis has shed light on the intriguing landscape of tobacco consumption in relation to various cancer types in Iran. The overall tobacco consumption proportions, calculated using a random effects model across all studies, settled at 42%. This means that almost half of the participants in these studies reported consuming tobacco. However, our statistical investigation also brought to light significant heterogeneity within the studies, pointing towards considerable variations in the tobacco consumption patterns.
Looking at the subgroup analysis, it's evident that tobacco consumption varies significantly across different cancer types and demographic groups. For instance, patients with laryngeal cancer showed the highest proportion of tobacco consumption (73%), while colorectal cancer patients showed the lowest (24%). When we examined tobacco use based on gender, we found males to exhibit a higher rate of consumption. Geographical disparities also emerged, with Sistan-baluchestan province reporting the highest rate of tobacco consumption and Tehran the lowest.
In terms of tobacco consumption habits, cigarette smoking emerged as the most prevalent, featuring in 15 studies with a proportion of 99%. Other forms of tobacco use, including waterpipe smoking and the use of ‘Naas’ and ‘Pipe’, showed varying levels of prevalence.
The high prevalence of ever smokers among cancer patients is notable, emphasizing the extensive impact tobacco has had on this population. Recognizing ever smokers—individuals who have smoked at any point in their lifetime—allows for a comprehensive understanding of tobacco exposure and its potential role in cancer progression and outcomes. This understanding is crucial for developing effective public health strategies, designing tailored interventions for tobacco cessation, and informing clinical guidelines aimed at reducing tobacco-related risks among cancer patients.
In 2021, the STEPwise approach to chronic disease risk factor surveillance (STEPS) survey provided comprehensive insights into the prevalence of tobacco use among Iranian adults, revealing distinct variations by gender, age, and usage patterns [64]. Overall, the prevalence of current tobacco smoking among the Iranian adult population was reported at 14.01% (13.56–14.48). When disaggregated by gender, a stark contrast emerges, with 25.88% (25.03–26.75) of men and only 4.44% (4.09–4.82) of women reported as current tobacco users. This gender disparity extends to specific tobacco products, with 19.95% (19.17–20.75) of men and 0.77% (0.62–0.95) of women identified as current cigarette smokers, and 5.56% (5.12–6.03) of men compared to 3.64% (3.33–3.98) of women reported as current hookah smokers.
The survey further delves into the age-related patterns of tobacco use, highlighting that cigarette smoking among men peaks at 26.43% (24.47–28.48) in the 45–54 year age group before declining, while the use of hookah shows its highest prevalence among both men (11.03% [9.66, 12.56]) and women (5.87% [4.98, 6.9]) aged 25–34. This age-specific data suggests a pronounced variation in smoking habits across different life stages. Additionally, the prevalence of second-hand smoking exposure at home was significantly high, with 24.64% (24.05–25.24) overall prevalence, showing higher exposure rates among women (27.38% [26.59–28.18]) compared to men (20.26% [19.39–21.17]). The geographical analysis of tobacco prevalence across the 31 provinces of Iran unveiled significant variations, further emphasizing the need for targeted public health interventions. The survey's findings underscore the persistently high rates of tobacco consumption in Iran, reflecting the pressing need for enhanced tobacco control policies and interventions that are sensitive to gender, age, and regional disparities. Given the elevated rate of tobacco use among patients with cancer at approximately 42% [36,37,38,39,40,41,42, 48, 56, 64,65,66], as identified in our study, these data call for urgent public health actions to address tobacco use as a critical risk factor for cancer and other non-communicable diseases in Iran.
To make sense of the different risks associated with various types of cancer in connection with tobacco use, a previous meta-analysis systematically examined the relative risks. The findings indicated that the highest risks were found in lung, laryngeal, and pharyngeal cancers, with upper digestive tract and oral cancers following closely behind [65]. In our more detailed subgroup analysis, we examined the studies based on cancer type, unveiling differing levels of tobacco consumption for each. We found that tobacco use was most prevalent in patients with laryngeal cancer. This group was closely followed by those with lung, head and neck, and bladder cancers. On the other hand, we noticed lower tobacco use in patients with breast, esophageal, gastric, and colorectal cancers.
Tobacco consumption in Iran presents a complex pattern of regional disparities, with distinct differences observed between the general population and cancer patients. As per the STEPwise report, in 2011, the north-western provinces, including West-Azerbaijan, East-Azerbaijan, Ardabil, Kordestan, Zanjan, Qazvin, and Gilan, recorded the highest rates of current tobacco smoking. However, by 2016, the epicenter of highest prevalence had migrated to Hamadan and Qazvin. Throughout these years, the western provinces, especially the north-west, consistently reported higher tobacco use compared to their eastern counterparts. In 2016, the southern provinces of Bushehr, Fars, and Hormozgan, along with Sistan and Baluchestan in the south-east and Razavi-Khorasan in the north-east, also emerged with high prevalence rates [66].
In examining cancer patients, the pattern of tobacco consumption across different regions reveals nuanced insights. Tehran is notable for its range of tobacco use among cancer patients, reported between 10% and 82.23%. This upper figure aligns with expectations when considering the elevated risk smoking poses for lung cancer, especially given the 26% smoking prevalence among Iranian men. Kerman also exhibits significant tobacco use among cancer patients, with rates from 26.32% to 72%. Mazandaran presents a varied scenario, where tobacco use among cancer patients ranges from 14.65% to 48.15%. Notably, the highest observed prevalence rates among cancer patients are in Sistan-Baluchestan (81.71%) and Tehran (82.23%), underscoring the link between tobacco exposure and cancer incidence in these regions. Therefore, while the general population in north-western provinces and some southern areas shows elevated tobacco consumption, Tehran and Sistan-Baluchestan demonstrate the most pronounced prevalence among cancer patients, reflecting the known risk factors associated with smoking.
We recognize that regional variations in tobacco use among cancer patients may be influenced by the types of cancers predominantly studied within those regions. Given the strong association between smoking and certain types of cancer, such as lung and larynx cancers, the prevalence of smoking is likely higher in regions where these cancers are more frequently studied. This potential confounding factor suggests that our observed regional differences in smoking prevalence might not solely reflect geographical variations in smoking behavior, but also the specific cancer types investigated in each region.
Tobacco consumption in Iran, both in the general populace and among cancer patients, exhibits a distinct pattern when dissected by the type of tobacco product used. In the general population, hookah use is relatively prevalent, with 3.6% of women and 5.6% of men engaging in this practice. Sistan and Baluchistan stand out with the highest usage of smokeless tobacco. The prevalence of men who have ever smoked cigarettes varies widely, from a low of 13.28% in South Khorasan to a high of 39.02% in Qazvin. Similarly, the prevalence of men who have ever used hookah ranges from 3.68% in Kermanshah to 22.38% in Isfahan. Among women, the prevalence of ever smoking cigarettes is generally low, peaking at 1.59% in Tehran, while the current use of hookah ranges from zero in Ardabil and West Azerbaijan to a significant 15.27% in Sistan and Baluchistan. Pipe smoking and smokeless tobacco, however, find little favor among the Iranian population [64].
In contrast, among cancer patients, the landscape of tobacco consumption shifts noticeably. Cigarette smoking emerges as the dominant form, with prevalence rates spanning from 64.15% to a full 100% in various studies. Waterpipe or hookah smoking, while less prevalent than cigarette smoking, still shows a considerable range of 4.17% to 35.85%. Other forms of tobacco use, including smokeless tobacco and pipe smoking, are relatively rare, with prevalence rates of 3.03% to 30.23% and 0.53% respectively. In essence, while cigarette smoking is the most common form of tobacco use across both the general population and cancer patients, hookah use is also a significant concern, particularly in certain provinces. Other forms of tobacco use, such as smokeless tobacco and pipe smoking, are less prevalent.
Strengths and limitations
Our findings, enriched by detailed subgroup analyses across cancer types, gender, geographic regions, and tobacco use modalities, underscore the critical public health implications of tobacco use among cancer patients, revealing a prevalence markedly higher than in the general population. Our study's limitations extend to include a restricted research scope as we relied solely on two databases, and due to a lack of direct studies, we had to use data embedded within these studies. The sustained high heterogeneity detected throughout our analyses suggests that numerous unexplored factors, beyond the boundaries of our study, could have an influential role. These factors might encompass socio-economic conditions in different provinces, distinct cultural practices, the effectiveness of cancer control programs, and the accuracy and accessibility of cancer registries. Additionally, the observed heterogeneity might be attributed to discrepancies in the types of studies we sourced, the specific cancer types analyzed, and their association with smoking. However, it is noteworthy to mention that because our meta-analysis was focused on evaluating prevalence, the high heterogeneity could be deemed acceptable due to these aforementioned reasons. Such a degree of heterogeneity may not present as a critical issue like when we calculate Odds Ratios (OR) or Relative Risks (RR). An important limitation of our study is that the observed regional variations in smoking prevalence among cancer patients could be influenced by the selection of cancer types studied in each region. This aspect might have introduced a bias towards higher smoking prevalence in regions focusing on cancers strongly associated with smoking. Future studies should aim to disentangle the effects of regional cancer type distribution from true variations in smoking behavior.
Conclusion
In conclusion, our systematic review and meta-analysis provide valuable insights into the link between tobacco consumption and various cancer types in Iran, revealing considerable heterogeneity in consumption patterns across different demographics, geographical regions, and cancer types. Notably, the rate of tobacco consumption among cancer patients is threefold higher than in the general Iranian population. The study also unveils a concerning picture of the prevalent use of cigarettes and the variable use of other forms of tobacco, including waterpipe smoking, ‘Naas’, and ‘Pipe’, among cancer patients.
Availability of data and materials
Data will be available upon reasonable request from the corresponding author.
References
Dolatkhah R, Somi MH, Kermani IA, Ghojazadeh M, Jafarabadi MA, Farassati F, et al. Increased colorectal cancer incidence in Iran: a systematic review and meta-analysis. BMC Public Health. 2015;15(1):1–14.
Rafiemanesh H, Rajaei-Behbahani N, Khani Y, Hosseini S, Mohammadian-Hafshejani A, Soltani S, et al. Incidence trend and epidemiology of common cancers in the center of Iran. Global J Health Sci. 2016;8(3):146.
Roshandel G, Ferlay J, Ghanbari-Motlagh A, Partovipour E, Salavati F, Aryan K, et al. Cancer in Iran 2008 to 2025: Recent incidence trends and short-term predictions of the future burden. Int J Cancer. 2021;149(3):594–605.
Hecht SS. Cigarette smoking: cancer risks, carcinogens, and mechanisms. Langenbecks Arch Surg. 2006;391:603–13.
Secretan B, Straif K, Baan R, Grosse Y, El Ghissassi F, Bouvard V, et al. A review of human carcinogens—Part E: tobacco, areca nut, alcohol, coal smoke, and salted fish. Lancet Oncol. 2009;10(11):1033–4.
Sitas F, Weber MF, Egger S, Yap S, Chiew M, O’Connell D. Smoking cessation after cancer. J Clin Oncol. 2014;32(32):3593–5.
Zahra H, Mahshid A, Habib E, Mohammadreza M. Behavior and knowledge of Iranian professional athletes towards smoking. 2012.
Agudo A, Bonet C, Travier N, González CA, Vineis P, Bueno-de-Mesquita HB, et al. Impact of cigarette smoking on cancer risk in the European prospective investigation into cancer and nutrition study. J Clin Oncol. 2012;30(36):4550–7.
Halimi L, Haghdoost AA, Alizadeh SM. Prevalence of cigarette smoking among Iranian women: a systematic review and meta-analysis. Med J Islam Repub Iran. 2013;27(3):132.
Jose T, Schroeder DR, Warner DO. Changes in cigarette smoking behavior in cancer survivors during diagnosis and treatment. Nicotine Tob Res. 2022;24(10):1581–8.
Vioque J, Barber X, Bolumar F, Porta M, Santibáñez M, de la Hera MG, et al. Esophageal cancer risk by type of alcohol drinking and smoking: a case-control study in Spain. BMC Cancer. 2008;8(1):1–10.
Sasco A, Secretan M, Straif K. Tobacco smoking and cancer: a brief review of recent epidemiological evidence. Lung Cancer. 2004;45:S3–9.
Farhood B, Geraily G, Alizadeh A. Incidence and mortality of various cancers in Iran and compare to other countries: a review article. Iran J Public Health. 2018;47(3):309.
Samet JM. Tobacco smoking: the leading cause of preventable disease worldwide. Thorac Cardiovasc Surg. 2013;23(2):103–12.
Stevens GA, Alkema L, Black RE, Boerma JT, Collins GS, Ezzati M, et al. Guidelines for accurate and transparent health estimates reporting: the GATHER statement. Lancet. 2016;388(10062):e19–23.
Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, Ioannidis JP, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. Ann Intern Med. 2009;151(4):W65–94.
Stijnen T, Hamza TH, Ozdemir P. Random effects meta-analysis of event outcome in the framework of the generalized linear mixed model with applications in sparse data. Stat Med. 2010;29(29):3046–67.
Wang Q. Dietary quality using four dietary indices and lung cancer risk: the Golestan Cohort Study (GCS). 2021. p. 493–503.
Etemadi A. Hazards of cigarettes, smokeless tobacco and waterpipe in a Middle Eastern population: A cohort study of 50 000 individuals from Iran. 2017. p. 674–82.
Sheikh M. Household fuel use and the risk of gastrointestinal cancers: The Golestan cohort study. 2020. p. 1–9.
Sheikh M. Individual and combined effects of environmental risk factors for esophageal cancer based on results from the Golestan cohort study. 2019. p. 1416–27.
Rahmati A. Mortality from respiratory diseases associated with opium use: A population-based cohort study. 2017. p. 1028–34.
Moossavi S, Mohamadnejad M, Pourshams A, Poustchi H, Islami F, Sharafkhah M, et al. Opium use and risk of pancreatic cancer: a prospective cohort study. Cancer Epidemiol Biomarkers Prev. 2018;27(3):268–73.
Nasrollahzadeh D. Opium, tobacco, and alcohol use in relation to oesophageal squamous cell carcinoma in a high-risk area of Iran. 2008. p. 1857–63.
Marjani HA. Prevalence of esophageal cancer risk factors among Turkmen and non-Turkmen ethnic groups in a high incidence area in Iran. 2010. p. 111–5.
Aghcheli K. Prognostic factors for esophageal squamous cell Carcinoma-a population-based study in Golestan province, Iran, a high incidence area. 2011.
Abnet CC. Reliability and validity of opiate use self-report in a population at high risk for esophageal cancer in Golestan, Iran. 2004. p. 1068–70.
Sheikh M. Opium use and subsequent incidence of cancer: results from the Golestan cohort study. 2020.
Mahouri KH. Breast cancer risk factors in south of Islamic Republic of Iran: A case-control study. 2007. p. 1265–73.
Abdolahinia Z, Pakmanesh H, Mirzaee M, Bazrafshan A, Bafti MS, Shahesmaeili A. Opium and cigarette smoking are independently associated with bladder cancer: the findings of a matched case - control study. Asian Pac J Cancer Prev. 2021;22(10):3385–91.
Ahmadi M. Epidemiologic and socioeconomic status of bladder cancer in Mazandaran province, northern Iran. 2012. p. 5053–6.
Akbari M. Opium as a risk factor for bladder cancer: A population-based case-control study in Iran. 2015. p. 567–71.
Moghadam TN, Mirzaee M, Bahrampour A, Jahani Y, Abbasi MH. Survival Analysis of gastric cancer patients using illness-death model in Kerman City, Southeast Iran during 2001–2016. Middle East J Dig Dis. 2021;13(3):208–15.
Rafati S, Baneshi MR, Bahrampour A. Factors affecting long-survival of patients with breast cancer by non-mixture and mixture cure models using the Weibull, log-logistic and Dagum distributions: a Bayesian approach. Asian Pac J Cancer Prev. 2020;21(2):485–90.
Samadi F. Survival rate of gastric and esophageal cancers in Ardabil Province, North-West of Iran. 2007. p. 32–7.
Hadji M. The Iranian Study of Opium and Cancer (IROPICAN): Rationale, design, and initial findings. 2021. p. 167–76.
Momtahen S. Assessment of gynecologic malignancies: A multi-center study in Tehran (1995–2005). 2009. p. 226–30.
Hosseini B, Olsson A, Bouaoun L, Hall A, Hadji M, Rashidian H, et al. Lung cancer risk in relation to jobs held in a nationwide case-control study in Iran. Occup Environ Med. 2022;79(12):831–8.
Fayez EA, Moosavi SAJ, Kouranifar S, Delbandi AA, Teimourian S, Khoshmirsafa M, et al. The effect of smoking on latent tuberculosis infection susceptibility in high risk individuals in Iran. J Immunoassay Immunochem. 2020;41(5):885–95.
Aminisani N, Nikbakht HA, Hosseinei SR, Shamshirgaran SM. Adverse health behaviours among colorectal cancer survivors: a case study from Iran. J Gastrointest Oncol. 2016;7(3):373–9.
Andisheh-Tadbir A. Sociodemographic and etiological differences of head and neck squamous cell carcinoma in young and old patients in southern Iran. 2010. p. 126–8.
Azimi S. Socioeconomic determinants as risk factors for squamous cell carcinoma of the head and neck: a case-control study in Iran. 2018. p. 304–9.
Khademi H. Diagnostic accuracy of age and alarm symptoms for upper GI malignancy in patients with dyspepsia in a GI clinic: A 7-year cross-sectional study. 2012.
Khoshbaten M, Naderpour M, Mohammadi G, Alipoor SH, Estakhri R, Fazeli Z. Epidemiology of esophageal lesions in patients with head and neck squamous cell carcinoma. Asian Pac J Cancer Prev. 2010;11(4):863–5.
Mafi N, Kadivar M, Hosseini N, Ahmadi S, Zare-Mirzaie A. Head and neck squamous cell carcinoma in Iranian patients and risk factors in young adults: a fifteen-year study. Asian Pac J Cancer Prev. 2012;13(7):3373–8.
Mahouri K, Zahedani MD, Zare S. Breast cancer risk factors in south of Islamic Republic of Iran: a case-control study. East Mediterr Health J. 2007;13(6):1265–73.
Mashhadi MA. High prevalence of esophageal cancer in South-East of Iran. 2011. p. 18–21.
Masjedi MR. Opium could be considered an independent risk factor for lung cancer: A case-control study. 2013. p. 112–8.
Mohebbi E, Hadji M, Rashidian H, Rezaianzadeh A, Marzban M, Haghdoost AA, et al. Opium use and the risk of head and neck squamous cell carcinoma. Int J Cancer. 2021;148(5):1066–76.
Sanat ZM, Masoudi S, Mansouri M, Shishavan NG, Jameshorani M, Pourshams A. Diabetes mellitus, obesity, and risk of pancreatic ductal adenocarcinoma: a large case-control study from Iran. Middle East J Dig Dis. 2021;13(1):15–20.
Motovali-Bashi M. Role of CYP1A1 MspI polymorphism in CYP1A1 gene with susceptibility to lung cancer in Iranian patients. 2012.
Naghibzadeh-Taham A. Can opium use contribute to a higher risk of colorectal cancers? A matched case-control study in Iran. 2016. p. 1322–31.
Nikbakht H. Trends in the incidence of colorectal cancer and epidemiologic and clinical characteristics of survivors in Babol city in 2007–2012. 2015. p. 7–14.
Pournaghi S. Tobacco consumption, opium use, alcohol drinking and the risk of esophageal cancer in North Khorasan, Iran. 2019. p. 105–9.
Sadjadi A, Derakhshan MH, Yazdanbod A, Boreiri M, Parsaeian M, Babaei M, et al. Neglected role of hookah and opium in gastric carcinogenesis: a cohort study on risk factors and attributable fractions. Int J Cancer. 2014;134(1):181–8.
Saedi B, Razmpa E, Sadeghi M, Mojtahed M, Mojtahed A. The epidemiology of laryngeal cancer in a country on the esophageal cancer belt. Indian J Otolaryngol Head Neck Surg. 2009;61(3):213–7.
Salehi A, Khezri AA, Malekmakan L, Aminsharifi A. Epidemiologic status of bladder cancer in Shiraz, southern Iran. Asian Pac J Cancer Prev. 2011;12(5):1323–7.
Sheikh M, Shakeri R, Poustchi H, Pourshams A, Etemadi A, Islami F, et al. Opium use and subsequent incidence of cancer: results from the Golestan Cohort Study. Lancet Glob Health. 2020;8(5):e649–60.
Shivappa N. Dietary Inflammatory Index and Risk of Esophageal Squamous Cell Cancer in a Case-Control Study from Iran. 2015. p. 1255–61.
Simonian M. Environmental risk factors associated with sporadic colorectal cancer in Isfahan, Iran. 2018. p. 318–22.
Tabei SZ, Heydari ST, Mehrabani D, Shamsina SJ, Ahmadi J, Firouzi SM. Current substance use in patients with gastric cancer in Southern Iran. J Cancer Res Ther. 2006;2(4):182–5.
Tarrahi MJ. Lung cancer occurrence in Southern Iran. 2009. p. 139–40.
Vazirinejad R, Najafipour R, Rezaeian M, Ghazizadeh A, Mohammadi FD. Opium and risk of gastrointestinal cancer: a case-control study. Turk J Med Sci. 2020;50(4):697–705.
Abbasi-Kangevari M, Ghanbari A, Fattahi N, Malekpour M-R, Masinaei M, Ahmadi N, et al. Tobacco consumption patterns among Iranian adults: a national and sub-national update from the STEPS survey 2021. Sci Rep. 2023;13(1):10272.
Gandini S, Botteri E, Iodice S, Boniol M, Lowenfels AB, Maisonneuve P, et al. Tobacco smoking and cancer: a meta-analysis. Int J Cancer. 2008;122(1):155–64.
Sohrabi MR, Abbasi-Kangevari M, Kolahi AA. Current tobacco smoking prevalence among Iranian population: A closer look at the STEPS surveys. Front Public Health. 2020;8:571062.
Acknowledgements
This article is the result of the support of the Research Vice-Chancellor of Mashhad University of Medical Sciences, which is now appreciated.
Funding
This study was supported by Mashhad University of Medical Sciences Research Council, Mashhad, Iran (Ref: 4010809).
Author information
Authors and Affiliations
Contributions
MMV contributed to the conception, design, and methodology of the systematic review and meta-analysis. MMV was also involved in the literature search, study selection, data extraction, data analysis, and contributed to the writing and editing of the manuscript. DD participated in the risk assessment, study selection, data extraction, and interpretation. ZT, AG, and MAK were involved in the risk assessment process, study selection, and data extraction. RM contributed to the data extraction and the interpretation of findings. FS was involved in data analysis and contributed to the writing and editing of the manuscript. RAM and AA contributed to the writing and editing of the manuscript, with AA specifically involved in the draft and revision editing. HKM and NB were involved in data extraction. RK contributed to the conception, design, and methodology of the study. RK was also involved in the literature search, study selection, data extraction, data analysis, and interpretation of findings. PBT participated in data extraction and contributed to the writing and editing of the manuscript. SS contributed to the conception, design, and methodology of the study, and played a supervisory role across all stages of the systematic review and meta-analysis, including literature search, study selection, data extraction, data analysis, and interpretation of findings. All authors contributed to the article and approved the submitted version. CA indicates the corresponding author.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Vakilzadeh, M.M., Khayami, R., Daneshdoust, D. et al. Prevalence of tobacco use among cancer patients in Iran: a systematic review and meta-analysis. BMC Public Health 24, 1081 (2024). https://doi.org/10.1186/s12889-024-18594-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12889-024-18594-8