Abstract
Purpose
Previous research has suggested that individuals are mostly prone to loneliness in their later years of life because of exposure to several risk factors typical of old age. The current study aims to examine possible demographic, health and social determinants of loneliness among older adults in Europe.
Methods
Data on a nationally representative sample of 5074 Europeans aged ≥ 65 years were drawn from the first wave of the Survey of Health, Aging and Retirement in Europe (SHARE, 2004/2005). Frequency of feelings of loneliness was examined according to adverse health conditions, stressful life events and social isolation indicators.
Results
Female gender, older age, lower socioeconomic status, living unpartnered, being childless and having no activity involvement were significantly associated with frequent feelings of loneliness (p < 0.001). The proportion of the respondents who declared enduring loneliness most of the time compared with none of the time was significantly higher among Southern Europeans relative to their Northern counterparts (p < 0.001). Recent departure of offspring from the parental nest was a significant predictor of loneliness in both the second (ORs = 2.08; 95% CI 1.24–3.48) and the third (ORs = 1.75; 95% CI 1.03–2.96) multiple regression models.
Conclusion
In this sample of older Europeans, several demographic characteristics, specific adverse health conditions, stressful life events and social isolation indicators were associated with feelings of loneliness. Policy initiatives for the alleviation of loneliness in older age should therefore aim at improving psychosocial and health-related difficulties faced by this population.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Loneliness is an unpleasant and distressful emotional state whereby a person undergoes a deprivation of social resources pertaining to interpersonal relations, connectedness, companionship and support (van Baarsen et al. 2001) and thus perceives a discrepancy between the desired amount of social relationships and contacts and the ones they have managed to obtain (Perlman and Peplau 1981). Loneliness is usually appraised subjectively by the extent to which an individual is integrated in social networks or the degree of their social alienation (Wenger et al. 1996). Although a universal definition does not exist, loneliness has mainly been conceptualized as a self-identified painful experience, characterized by a cognitive evaluation of the divergence between real relationships and those anticipated by individuals (Cacioppo and Hawkley 2009). Therefore, loneliness refers to the social deficiency arising from an imbalance between the social interactions a person holds and the ones they would wish for (Peplau and Perlman 1982), which is thus intertwined with self-perceptions of isolation, negligence and abandonment (Singh and Kiran 2013).
Previous psychological and sociological research has portrayed loneliness as a major health, well-being and mortality risk factor (Holt-Lunstad et al. 2015), which can pose a health burden equivalent to common risky health behaviors, such as smoking, alcohol consumption and physical inactivity, particularly in older adults (Valtorta and Hanratty 2012). Potential mechanisms underlying the health implications of loneliness in this population include the inducement of physiological, behavioral and psychological changes, such as increased stress-related responses (Steptoe et al. 2004), elevated blood pressure, cardiovascular activation, sleep disturbance (Cacioppo et al. 2002; Hawkley and Cacioppo 2010) and functional decline (Perissinotto et al. 2012). Loneliness, "as a stressor itself,” accounts for higher negative affect and less emotional regulation (Cacioppo and Hawkley 2003) and thus greater depression (Singh and Misra 2009). There is also empirical evidence to relate the higher incidence of loneliness with the arousal of feelings of rejection, interpersonal mistrust and lack of self-confidence (Masi et al. 2011), whereas chronic loneliness has been linked to unpleasant emotional states, such as anger, anxiety, pessimism and low self-esteem (Cacioppo et al. 2006). In addition, the likelihood of being physically inactive, smoking and indicating multiple health-detrimental behaviors has been shown to be greater among lonely individuals of advanced age (Shankar et al. 2011). Loneliness has thus been associated with increased healthcare services utilization (Gerst-Emerson and Jayawardhana 2015) and frequent nursing home admission, potentially increasing health care costs (Russell et al. 1997).
The onset of loneliness in the later-life context has been attributed to the occurrence of considerable changes in life circumstances that are particularly related to older age. Old age itself constitutes a transition that is accompanied by several adverse social and health conditions with salient implications for loneliness. Life-course trajectories accompanying aging, such as the deterioration of family and social networks due to adult offspring leaving the parental home, death of a spouse, a parent or friend, and age-related health decline and impairment, can particularly subject older people to loneliness (Yang and Victor 2011). Old age has thus been considered as a life period where intimate attachment figures are more likely to be lacking because of loss of contemporaries and shrinkage of prior family and social bonds (van Baarsen et al. 2001).
Evidence to date has suggested that the prevalence of loneliness in older people ranges from around 7% and 9% to 14.5% in Great Britain (Thomas 2015; Victor and Bowling 2012; Victor and Yang 2012) and 10% to 25% in the US (AARP 2010; Kuwert et al. 2014). According to recent findings of the Generations and Gender Survey, loneliness was common among 30% to 55% of older people in Central and Eastern Europe and 10% to 20% in Northwestern Europe (Hansen and Slagsvold 2016). Therefore, loneliness in older age has been regarded a major public health and social issue, which seems to affect a considerable proportion of older adults (Bernard 2013) and to bear important implications for their emotional and psychological well-being (Allen 2008).
Susceptibility to loneliness among older people could be alleviated through active involvement in social activities and engagement with extensive family networks and supportive marital relations (Gierveld Jde et al. 2009). Moreover, studies examining the predictors of loneliness in old age have suggested the protective role of living within a partnered arrangement (Gierveld Jde et al. 2012), being socially engaged and having a confidant, friends, relatives and children (Steed et al. 2007) in loneliness prevention. Relevant research has also indicated an array of health and social conditions as possible predictors of loneliness among older individuals. More specifically, depression and mobility problems have been identified as life events along with bereavement and widowhood, which seem to bear upon feelings of loneliness (Dahlberg et al. 2015). Other health-related outcomes that have been suggested to put older adults at a higher risk of enduring loneliness include functional limitations (Luhmann and Hawkley 2016), pain (Emerson et al. 2017), anxiety and poor subjective health (Fees et al. 1999).
However, evidence on the demographic, health and social patterns of loneliness remains limited. In addition, the determinants of loneliness from a cross-national perspective have not been fully investigated. In this respect, identifying factors related to loneliness is essential for recognizing individuals who are at increased risk of feeling lonely and developing appropriate intervention strategies to tackle and alleviate loneliness. The aim of the current study was thus to examine the prevalence of loneliness in a nationally representative sample of European older adults and consider various health, psychological and social variables possibly associated with the experience of loneliness.
Methods
Subjects and data collection
The current study is based on data of a subsample of 5129 adults, 65 years of age and older, of the total sample of 27,444 individuals who took part in the first wave of the Survey of Health, Aging and Retirement in Europe (SHARE, http://www.share-project.org), which was conducted between 2004 and 2005 in 11 European countries (Austria, Belgium, Denmark, France, Germany, Greece, Italy, The Netherlands, Spain, Sweden and Switzerland).
A centrally programmed, computer-assisted personal interviewing technique (CAPI) was administered for the collection of the main survey data by means of an automatically generated questionnaire that comprised 21 modules on a wide range of research domains. Interviews conducted through CAPIs were further supplemented by a brief, self-completed paper-and-pencil questionnaire with additional queries on social networks, health care, medical examinations and physical and mental health.
Measures
Loneliness
To assess feelings of loneliness, respondents were asked to demonstrate how frequently they had recently been feeling lonely through a general question retrieved from the abbreviated version of the Center for Epidemiological Studies Depression scale (CES-D) and phrased as follows: “How often have you experienced the following feelings over the last week?”: “I felt lonely.” Responses were classified according to a four-point scale (almost all of the time; most of the time; some of the time; almost none of the time). Participants who reported feeling lonely ‘almost all of the time’ and ‘most of the time’ were considered to be severely lonely. This self-reported measure has been commonly applied to determine levels of loneliness among older individuals as it is easily comprehended (Victor et al. 2009) and concurs with the results of other multi-item scales (Pinquart and Sorensen 2001b).
Determinants of loneliness
Possible factors related to loneliness were addressed along three domains, namely adverse health conditions, stressful life events and social isolation. Adverse health conditions, which have also been incorporated in recent research as components of physical and mental health status (Linardakis et al. 2015), were assessed by the presence of one or more chronic diseases (heart attack, high blood pressure, high blood cholesterol, stroke, diabetes or high blood glucose, chronic lung cancer, asthma, arthritis, osteoporosis, cancer, and stomach or duodenal/peptic ulcer), functional limitations in activities and instrumental activities of daily living [(I)ADLs] (dressing, walking across a room, bathing or showering, eating, cutting up food, getting in or out of bed, using the toilet, using a map in a strange place, preparing a hot meal, shopping for groceries, making telephone calls, taking medications, doing work around the house or garden and managing money), disease symptoms (pain in the back, knees hips or other joints, heart trouble, breathlessness, persistent cough, swollen legs, sleeping problems, falls, fear of falling down, dizziness, faints or blackouts, stomach or intestine problems, and incontinence) and four or more clinically depressive symptoms, according to the 12-item European Depression (Euro-D) scale (Guerra et al. 2015). Stressful life events were measured on the occurrence of four unpleasant circumstances, comprising quitting work on account of health problems, undergoing a greatly deteriorated financial situation compared with the previous year, being a widower and enduring an ‘empty nest’ due to adult children having recently left the parental home. Social isolation was defined as: (1) small network size, assessed by living unpartnered, being unmarried and having no children, and (2) social disengagement, assessed by means of infrequent contact with offspring, separate residence to children, infrequent social involvement and rare or no social support exchanges.
Demographic and socioeconomic characteristics
Demographic characteristics included gender (male/female) and years of age (65–74, 75–84 and 85+). The social background variables of educational attainment, measured as years of schooling obtained (0–7, 8–12, 13+), retirement status (retired/not retired) and self-reported household income, defined by country-specific quartiles (low <25%, average between 25 and 75% and high >75%), were incorporated in the analysis. Additionally, the 11 European countries were geographically classified into northern (Denmark, Sweden), central (Austria, Belgium, France, Germany, The Netherlands, Switzerland) and southern (Greece, Italy, Spain).
Statistical analysis
Data analyses were performed using SPSS (IBM SPSS Statistics for Windows, version 23.0. Armonk, NY: IBM Corp). Sampling design weights, adjusted for non-response, were employed according to the complex multi-stage stratification sampling design of the study. First, prevalence of loneliness was assessed, and chi-square tests were used to compare this variable according to demographic characteristics. Odds ratios (ORs, adjusted) were estimated with socio-demographic characteristics as covariates, using multiple logistic regression analysis. Prevalence of loneliness was also examined according to adverse health conditions, stressful life events and social isolation indicators using similar methods as previously described. Second, multiple logistic regression analysis was applied for adults endorsing feelings of loneliness most of the time compared with none of the time. Three models were fitted to compute adjusted ORs to examine the effect of adverse health conditions, stressful life events and social isolation indicators on feeling lonely most of the time compared with none of the time. In the first model, we estimated the effect of adverse health conditions on feeling lonely most of the time, adjusting for age, gender, education, retirement status, household income and country regions. In the second model, stressful life events were added, whereas the effect of social isolation indicators was examined in the final model. Nagelkerke pseudo R estimators were also assessed for the evaluation of goodness of fit in the three models.
Results
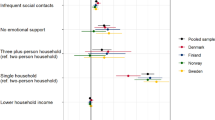
The distribution of loneliness by demographic and socio-structural variables is depicted in Table 1. Enduring severe (‘almost most of the time’ and ‘most of the time’) and frequent (‘some of the time’) feelings of loneliness was mostly reported by females relative to males (59.1 vs. 38%, p < 0.001), and females had higher odds of considering themselves lonely most of the time (OR = 2.08; 95% CI 1.35–3.19). Prevalence of feeling lonely most of the time was higher among the oldest-old participants (85+) (12.4%) compared with participants aged 65–74 (7.7%) and 75–84 years old (11.9%) (p < 0.001). Individuals aged 75–84 years were more likely to feel lonely most of the time compared with their younger and older counterparts (OR = 1.72; 95% CI 1.14–2.59). Higher prevalence of persistent feelings of loneliness was also observed among the respondents with the lowest educational attainment (12.4 vs. 7.3%, p < 0.001), those who were not retired (11.3 vs. 9.2%, p = 0.009) and those with the lowest household income (13.6 vs. 7.3%, p < 0.001). Respondents of lower household income had higher odds of reporting frequent feelings of loneliness compared with those with greater incomes (OR = 2.88; 95% CI 1.49–5.58). A higher proportion of southern older adults (12.6%) declared feeling lonely most of the time compared with central (7.5%) and northern (5.0%) Europeans. Participants of Central and Southern European countries had higher odds of feeling lonely most of the time (OR = 2.63; 95% CI 1.54–5.51 and OR = 4.62; 95% CI 2.63–8.10, respectively) compared with their Northern counterparts. Significant differences were also observed at the country level (Fig. 1), with the greatest prevalence of loneliness found among the Italian (27.8%) and the lowest among the Swiss older population (5.0%). In addition, the percentage of the participants feeling lonely most of the time was significantly higher among those living alone in Italy (20.4%) and Greece (16.6%), and it was almost three times as high compared with older individuals in Switzerland (5.5%) and Denmark (7.6%) (Fig. 2). Overall, 40.9% of the study sample endorsed feelings of loneliness some of the time and 9.6% most of the time (results not shown in the table).
The prevalence of loneliness according to adverse health conditions, stressful life events and social isolation indicators is presented in Table 2. Participants with one or more chronic diseases, (I)ADL limitations, disease symptoms and adverse health events as well as those with four or more depressive symptoms were significantly more likely to report persistent or frequent feelings of loneliness compared with those with none of these conditions or less than four depressive symptoms. As far as stressful life events are concerned, the percentage of widowers who reported feeling lonely most of the time was significantly higher compared with their non-widowed counterparts (12.2 vs. 7.8%, p < 0.001), while being a widow(er) was associated with higher odds of frequent feelings of loneliness (OR = 1.87; 95% CI 1.16–3.02). Additionally, more participants whose offspring had recently moved out of the parental home felt lonely most or some of the time compared with those who still lived with their children (52.4% vs. 44.7%, p = 0.032) and were thus significantly more likely to feel lonely most of the time (OR = 1.75; 95% CI 1.06–2.89). Loneliness was also significantly more frequently reported by socially isolated adults, as indicated by their living status, number of children and activity participation (p < 0.001). Living without a partner or spouse (OR = 3.96; 95% CI 2.52–6.22) and being childless (OR = 2.27; 95% CI 1.35–3.83) equated with a higher likelihood of feeling lonely most of the time. A greater proportion of participants reporting more than four social isolation indicators felt lonely most or some of the time compared with those with less than four indicators (69.7 vs. 46.0%, p < 0.001), and these participants had higher odds of persistent loneliness (OR = 2.65; 95% CI 1.57–4.64).
Finally, the association between adverse health conditions, stressful life events and social isolation and feeling lonely most of the time compared with none of the time was examined by means of multiple regression analysis (Table 3). Adults with four or more depressive symptoms had higher odds of persistent loneliness in both the first (OR = 2.89; 95% CI 1.89–4.44) and the second (OR = 2.84; 95% CI 1.83–4.39) models. Widowhood in the second model (OR = 2.00; 95% CI 1.21–3.31) and having a child recently moved away from the parental home (second and third models, OR = 2.08; 95% CI 1.24–3.48 and OR = 1.75; 95% CI 1.03–2.96, respectively) were significant predictors of persistent feelings of loneliness.
Discussion
This study aimed to examine the prevalence of loneliness among a nationally representative sample of older individuals residing in 11 European countries and participating in the first wave of the SHARE study and determine its possible association with socio-demographic characteristics, adverse health conditions, stressful life events and social isolation. To our knowledge, this is the first study to afford a comprehensive assessment of loneliness by utilizing multiple health, psychological and social variables that are particularly relevant in the context of later life, resting upon cross-country data.
In line with the previous findings regarding the prevalence of loneliness (Savikko et al. 2005; Victor et al. 2015), the proportion of older adults in our sample who declared feeling lonely most or some of the time was 50.5%. This was found to be particularly the case for older women compared with men. These findings are in agreement with relevant investigations, which have reported differences in loneliness among European adults associated with being of female gender and older age (Fokkema et al. 2012; Tobiasz-Adamczyk et al. 2017). Gender- and age-related variations in loneliness have been widely considered, concomitant with health decline, widowhood, bereavement and solitary living to be mostly prominent among females, adults of advanced age and disadvantaged older people (Fokkema et al. 2012; Pinquart and Sorensen 2001a). It is thus well established that women tend to live longer than their spouses and partners, and hence they are more likely to go through widowhood and get older in solitude, conditions that potentially make them more prone to psychological distress and loneliness due to subsequent losses in previous supportive exchanges that are meaningful for later-life health and well-being (Hall and Havens 2001). The above gender-linked differences might also be in part due to men’s unwillingness to admit to feeling lonely, whereas it seems more socially accepted for women to express their emotional states (Borys and Perlman 1985).
Not surprisingly, frequent feelings of loneliness were more prevalent among southern European seniors. Earlier studies have affirmed the existence of a North-South gradient in loneliness, suggesting a higher prevalence among southern Europeans compared with their northern counterparts (Trivedi et al. 2009). According to Dykstra’s (2009) review of empirical literature on loneliness, there seems to be an overall pattern regarding the regional distribution of loneliness, with the older population in the South of Europe, whereby societies are considered more “family-oriented,” contrary to the individualistic Northern European countries, indicating greater levels of loneliness. In the present study, the highest percentage of severe loneliness among the 11 European countries under study was spotted in Greece and Italy. It was also demonstrated that among older adults living alone, the proportion of those who declared feeling lonely most of the time was significantly higher in Italy and Greece compared with the other European countries. These findings might be due to the “cultural expectation” that facilitates a “loneliness-provoking factor” assumed to be mostly prevalent among older individuals living alone in these countries, whereby co-residence or nearness of parents to their offspring is highly appreciated as a core aspect of intergenerational solidarity (Zavaleta et al. 2014).
The prevalence of loneliness differed significantly by educational attainment and household income level, with less educated and less affluent participants being more likely to report frequent feelings of loneliness compared with their counterparts of higher socioeconomic status. This further corroborates the previously ascertained social patterning of loneliness. For instance, Hawkley et al. (2008) used data from the Chicago Health, Aging and Social Relations Study and showed that loneliness among adults 50 to 68 years of age was significantly explained by socioeconomic status, as assessed by education and income. In addition, Theeke (2010) found educational level and household income to be associated with the frequency of feeling lonely among adults 50+ years old from the Health and Retirement Study (HRS).
To date, most studies have examined loneliness as a risk factor for a wide range of health-related physical and mental outcomes (Richard et al. 2017; Singh and Misra 2009). Even though few studies have assessed feelings of loneliness as a potential outcome of unfavorable health-related circumstances drawing mainly on single-country data, higher levels of loneliness have been consistently associated with poor health and well-being in middle-aged and older individuals (Koropeckyj-Cox 1998; Theeke 2009; Victor et al. 2005). In the current study, we also found that the proportion of older adults who reported experiencing frequent loneliness was significantly greater among those suffering from more than one adverse health conditions relative to their healthy counterparts. Accordingly, older individuals with more than one chronic disease, (I)ADL limitations and disease symptoms and more than four depressive symptoms had a significantly higher prevalence of severe feelings of loneliness. In line with the above findings, poor health status has been found to predict feelings of loneliness among older Finnish adults aged 75 years and over (Savikko et al. 2005), whereas functional decline has also been significantly related to loneliness among the oldest-old German individuals (Luhmann and Hawkley 2016). Depression was also associated with loneliness over a 7-year follow-up in a sample of older women and men in Sweden (Dahlberg et al. 2015). It could be possible, as also previously suggested (Paul 2015), that morbidity worsens older individuals’ ability to preserve their social contacts and impedes them from maintaining their social involvements because of their difficulties in communication or unwillingness to share their ill-health conditions, which might trigger feelings of loneliness. It might also be that poor mental health status, such as depression, entails several functional, mood and cognitive limitations that adversely affect older people’s capacities and willingness regarding involvement in social activities (Adams et al. 2004). It could be, therefore, fairly assumed that addressing older people’s health needs could be seen as an important means of promoting their level of social connectedness and alleviating their feelings of loneliness.
In concordance with prior evidence suggesting that the loss of a spouse or partner constitutes a risk factor for loneliness (Dahlberg et al. 2015; Pinquart 2003), the proportion of widowed older adults reporting frequent feelings of loneliness in our sample was significantly higher compared with their non-widowed counterparts. It has been suggested that age-related losses, such as widowhood, affect the quality and quantity of social ties and thus provoke feelings of loneliness (Pinquart 2003). Furthermore, a significantly higher percentage of participants whose offspring had recently moved out from the parental home declared feeling lonely most or some of the time compared with participants who still shared their household with their children. This pattern also held true in both regression models with the odds of feeling lonely most of the time compared with none of the time being significantly higher among adults whose children had recently left the parental household. It could be fairly assumed that loneliness is triggered by the lack of adequate family networks that determine supportive transactions and contribute to maintaining a sense of belonging.
Lastly, being socially isolated, as indicated by living unpartnered, having no children and being socially inactive over the course of the previous month, was significantly associated with the occurrence of frequent loneliness. The likelihood of feeling lonely most of the time was approximately four times as high among adults living without a partner compared with those living in a partnered arrangement Moreover, participants presenting more than four social isolation indicators were more likely to feel lonely most of the time compared with non-isolated seniors. Similarly, spouseless older participants of the English Longitudinal Study of Aging (ELSA) were found to be lacking companionship and displayed low levels of life satisfaction (Demakakos et al. 2006). Higher levels of loneliness have also been confirmed among childless older individuals (Koropeckyj-Cox 1998) and the least socially integrated (Jylhä 2004).
Study limitations and strengths
The above findings should be interpreted with consideration because of the limitations described below. First is the cross-sectional nature of the current analyses, which renders determining the direction of the association between loneliness and the factors under study. It might also well be that feeling lonely leads to several adverse health and social outcomes in old age. The prospective examination of determinants of loneliness could allow for causal inferences to be drawn between loneliness and adverse health conditions, stressful life events and social isolation. Second, the relatively low proportion of participants found to encounter severe feelings of loneliness might be attributed to the measure employed to assess loneliness, which corresponded to current feelings of loneliness, as opposed to other studies examining persistent loneliness. It has also been suggested that a single-item question asking respondents to directly indicate how lonely they feel, even though frequently used in the literature, might lead to the underestimation of the true levels of loneliness, as people seem to be reluctant to admit to experiencing loneliness because of unfavorable perceptions attached to loneliness as a socially undesirable state (Victor et al. 2000). However, one of the main advantages of this global measure lies in the fact that it is able to capture the understanding of the experience of loneliness from the perspective of the respondent and the importance they attach to it (Jylhä and Saarenheimo 2010).
Conclusions
Despite the above limitations, the present findings suggest that loneliness among European older adults is associated with age-related specific adverse health conditions, stressful life events and social isolation indicators. Identifying loneliness should therefore be an integral part of psychological and health assessment by health and social professionals in this population. Health and social policy makers involved in the development of interventions to reduce levels of loneliness with an aim to improve well-being and quality of life in older life should direct particular attention to the implications of those aspects of older adults’ social and health resources that are mostly relevant to loneliness and the challenges they confront to remaining socially engaged.
Abbreviations
- SHARE:
-
Survey of Health, Aging and Retirement in Europe
- Euro-D:
-
European Depression Scale
- (I)ADLs:
-
Activities and Instrumental Activities of Daily Living
References
AARP (2010) Loneliness among older adults: a national survey of adults 45+. https://assets.aarp.org/rgcenter/general/loneliness_2010.pdf. Accessed 23 Oct 2017
Adams KB, Sanders S, Auth EA (2004) Loneliness and depression in independent living retirement communities: risk and resilience factors. Aging Ment Health 8(6):475–485. https://doi.org/10.1080/13607860410001725054
Allen J (2008) Older people and well-being. London Institute for Public Policy Research. https://www.ippr.org/files/images/media/files/publication/2011/05/older_people_and_wellbeing_1651.pdf. Accessed 23 Oct 2017
Bernard S (2013) Loneliness and social isolation among older people in North Yorkshire. https://www.york.ac.uk/inst/spru/research/pdf/lonely.pdf. Accessed 1 Sep 2017
Borys S, Perlman D (1985) Gender differences in loneliness. Personal Soc Psychol Bull 11:63–76. https://doi.org/10.1177/0146167285111006
Cacioppo JT, Hawkley LC (2003) Social isolation and health, with an emphasis on underlying mechanisms. Perspect Biol Med 46(3 Suppl):S39–S52
Cacioppo JT, Hawkley LC (2009) Perceived social isolation and cognition. Trends Cogn Sci 13(10):447–454. https://doi.org/10.1016/j.tics.2009.06.005S1364-6613(09)00147-8
Cacioppo JT, Hawkley LC, Crawford LE, Ernst JM, Burleson MH, Kowalewski RB, Malarkey WB, Van Cauter E, Berntson GG (2002) Loneliness and health: potential mechanisms. Psychosom Med 64(3):407–417
Cacioppo JT, Hawkley LC, Ernst JM, Burleson M, Berntson GG, Nouriani B, Spiegel D (2006) Loneliness within a nomological net: an evolutionary perspective. J Res Pers 40(6):1054–1085. https://doi.org/10.1016/j.jrp.2005.11.007
Dahlberg L, Andersson L, McKee KJ, Lennartsson C (2015) Predictors of loneliness among older women and men in Sweden: a national longitudinal study. Aging Ment Health 19(5):409–417. https://doi.org/10.1080/13607863.2014.944091
Demakakos P, Nunn S, Nazroo J (2006) Loneliness, relative deprivation and life satisfaction. In: Banks J, Breeze E, Lessof C, Nazroo J (eds) Retirement, health and relationships of the older population in England: the 2004 english longitudinal study of aging. Institute of Fiscal Studies, London, pp 297–318
Dykstra PA (2009) Older adult loneliness: myths and realities. Eur J Ageing 6(2):91–100. https://doi.org/10.1007/s10433-009-0110-3
Emerson K, Boggero I, Ostir G, Jayawardhana J (2017) Pain as a risk factor for loneliness among older adults. J Aging Health 0898264317721348. https://doi.org/10.1177/0898264317721348
Fees B, Martin P, Poon L (1999) A model of loneliness in older adults. J Gerontol B Psychol Sci Soc Sci 54(4):P231–P239
Fokkema T, De Jong Gierveld J, Dykstra PA (2012) Cross-national differences in older adult loneliness. Aust J Psychol 146(1–2):201–228. https://doi.org/10.1080/00223980.2011.631612
Gerst-Emerson K, Jayawardhana J (2015) Loneliness as a public health issue: the impact of loneliness on health care utilization among older adults. Am J Public Health 105(5):1013–1019. https://doi.org/10.2105/AJPH.2014.302427
Gierveld Jde J, Dykstra P, Schenk N (2012) Living arrangements, intergenerational support types and older adult loneliness in Eastern and Western Europe. Demogr Res 27(7):167–200. https://doi.org/10.4054/DemRes.2012.27.7
Gierveld Jde J, van Groenou MB, Hoogendoorn AW, Smit JH (2009) Quality of marriages in later life and emotional and social loneliness. J Gerontol B Psychol Sci Soc Sci 64(4):497–506. https://doi.org/10.1093/geronb/gbn043gbn043
Guerra M, Ferri C, Llibre J, Prina AM, Prince M (2015) Psychometric properties of EURO-D, a geriatric depression scale: a cross-cultural validation study. BMC Psychiatry 15:12. https://doi.org/10.1186/s12888-015-0390-4
Hall M, Havens B (2001) The effects of social isolation and loneliness on the health of older women. Research Bulletin. http://www.cwhn.ca/sites/default/files/PDF/CEWH/RB/bulletin-vol2no2EN.pdf. Accessed 23 Oct 2017
Hansen T, Slagsvold B (2016) Late-life loneliness in 11 European countries: results from the generations and gender survey. Soc Indic Res 129:445. https://doi.org/10.1007/s11205-015-1111-6
Hawkley LC, Cacioppo JT (2010) Loneliness matters: a theoretical and empirical review of consequences and mechanisms. Ann Behav Med 40(2):218–227. https://doi.org/10.1007/s12160-010-9210-8
Hawkley LC, Hughes ME, Waite LJ, Masi CM, Thisted RA, Cacioppo JT (2008) From social structural factors to perceptions of relationship quality and loneliness: the Chicago health, aging, and social relations study. J Gerontol B Psychol Sci Soc Sci 63(6):S375–S384
Holt-Lunstad J, Smith T, Baker M, Harris T, Stephenson D (2015) Loneliness and social isolation as risk factors for mortality: a meta-analytic review. Perspect Psychol Sci 10(2):227–237. https://doi.org/10.1177/1745691614568352
Jylhä M (2004) Old age and loneliness: cross-sectional and longitudinal analyses in the Tampere longitudinal study on aging. Can J Aging La Revue Canadienne du Vieillissement 23(2):157–168. https://doi.org/10.1353/cja.2004.0023
Jylhä M, Saarenheimo M (2010) Loneliness and ageing: comparative perspectives. In: Dannefer D, Phillipson C (eds) Handbook of social gerontology. Sage, London, pp 317–328
Koropeckyj-Cox T (1998) Loneliness and depression in middle and old age: are the childless more vulnerable? J Gerontol B Psychol Sci Soc Sci 53(6):S303–S312
Kuwert P, Knaevelsrud C, Pietrzak RH (2014) Loneliness among older veterans in the United States: results from the national health and resilience in veterans study. Am J Geriatr Psychiatry 22(6):564–569. https://doi.org/10.1016/j.jagp.2013.02.013S1064-7481(13)00160-7
Linardakis M, Papadaki A, Smpokos E, Micheli K, Vozikaki M, Philalithis A (2015) Association of behavioral risk factors for chronic diseases with physical and mental health in European adults aged 50 years or older, 2004-2005. Prev Chronic Dis 12:E149. https://doi.org/10.5888/pcd12.150134E149
Luhmann M, Hawkley L (2016) Age differences in loneliness from late adolescence to oldest old age. Dev Psychol 52(6):943–959. https://doi.org/10.1037/dev0000117
Masi CM, Chen HY, Hawkley LC, Cacioppo JT (2011) A meta-analysis of interventions to reduce loneliness. Personal Soc Psychol Rev 15(3):219–266. https://doi.org/10.1177/1088868310377394
Paul C (2015) Loneliness and health in later life. In: Pachana NA, Laidlaw K (eds) Oxford handbook of clinical geropsychology. Oxford University Press, Oxford, pp 381–394
Peplau L, Perlman D (1982) Perspectives on loneliness. In: Peplau LA, Perlman D (eds) Loneliness: a sourcebook of current theory, research and practice. Wiley, New York, pp 1–18
Perissinotto CM, Stijacic Cenzer I, Covinsky KE (2012) Loneliness in older persons: a predictor of functional decline and death. Arch Intern Med 172(14):1078–1083. https://doi.org/10.1001/archinternmed.2012.19931188033
Perlman D, Peplau L (1981) Toward a social psychology of loneliness. In: Gilmour R, Duck S (eds) Personal relationships 3: personal relationships in disorder. Academic, London, pp 31–56
Pinquart M (2003) Loneliness in married, widowed, divorced, and never-married older adults. J Soc Pers Relat 20(1):31–53. https://doi.org/10.1177/02654075030201002
Pinquart M, Sorensen S (2001a) Gender differences in self-concept and psychological well-being in old age: a meta-analysis. J Gerontol B Psychol Sci Soc Sci 56(4):P195–P213
Pinquart M, Sorensen S (2001b) Influences on loneliness in older adults: a meta-analysis. Basic Appl Soc Psychol 23(4):245–266. https://doi.org/10.1207/s15324834basp2304_2
Richard A, Rohrmann S, Vandeleur CL, Schmid M, Barth J, Eichholzer M (2017) Loneliness is adversely associated with physical and mental health and lifestyle factors: results from a Swiss national survey. PLoS One 12(7):e0181442. https://doi.org/10.1371/journal.pone.0181442
Russell DW, Cutrona CE, de la Mora A, Wallace RB (1997) Loneliness and nursing home admission among rural older adults. Psychol Aging 12(4):574–589
Savikko N, Routasalo P, Tilvis RS, Strandberg TE, Pitkala KH (2005) Predictors and subjective causes of loneliness in an aged population. Arch Gerontol Geriatr 41(3):223–233. https://doi.org/10.1016/j.archger.2005.03.002
Shankar A, McMunn A, Banks J, Steptoe A (2011) Loneliness, social isolation, and behavioral and biological health indicators in older adults. Health Psychol 30(4):377–385. https://doi.org/10.1037/a00228262011-08649-001
Singh A, Misra N (2009) Loneliness, depression and sociability in old age. Ind Psychiatry J 18(1):51–55. https://doi.org/10.4103/0972-6748.57861
Singh B, Kiran U (2013) Loneliness among elderly women. Int J Hum Soc Sci Invention 2(2):10–14
Steed L, Boldy D, Grenade L, Iredell H (2007) The demographics of loneliness among older people in Perth, Western Australia. Aust J Aging 26(2):81–86. https://doi.org/10.1111/j.1741-6612.2007.00221.x
Steptoe A, Owen N, Kunz-Ebrecht SR, Brydon L (2004) Loneliness and neuroendocrine, cardiovascular, and inflammatory stress responses in middle-aged men and women. Psychoneuroendocrinology 29(5):593–611. https://doi.org/10.1016/S0306-4530(03)00086-6
Theeke LA (2009) Predictors of loneliness in US adults over age sixty-five. Arch Psychiatr Nurs 23(5):387–396. https://doi.org/10.1016/j.apnu.2008.11.002
Theeke LA (2010) Sociodemographic and health-related risks for loneliness and outcome differences by loneliness status in a sample of US older adults. Res Gerontol Nurs 3(2):113–125. https://doi.org/10.3928/19404921-20091103-99
Thomas J (2015) Insights into loneliness, older people and well-being, 2015. http://webarchive.nationalarchives.gov.uk/20160106033522/http://www.ons.gov.uk/ons/dcp171766_418058.pdf. Accessed 24 Oct 2017
Tobiasz-Adamczyk B, Galas A, Zawisza K, Chatterji S, Haro JM, Ayuso-Mateos JL, Koskinen S, Leonardi M (2017) Gender-related differences in the multi-pathway effect of social determinants on quality of life in older age—the COURAGE in Europe project. Qual Life Res 26(7):1865–1878. https://doi.org/10.1007/s11136-017-1530-8
Trivedi JK, Sareen H, Dhyani M (2009) Psychological aspects of widowhood and divorce. Mens Sana Monogr 7(1):37–49. https://doi.org/10.4103/0973-1229.40648MSM-7-37
Valtorta N, Hanratty B (2012) Loneliness, isolation and the health of older adults: do we need a new research agenda? J R Soc Med 105(12):518–522. https://doi.org/10.1258/jrsm.2012.120128
van Baarsen B, Snijders TAB, Smit JH, van Duijn MAJ (2001) Lonely but not alone: emotional isolation and social isolation as two distinct dimensions of loneliness in older people. Educ Psychol Meas 61(1):119–135. https://doi.org/10.1177/00131640121971103
Victor C, Scambler S, Bond J (2009) The social world of older people: understanding loneliness and social isolation in later life (Growing Older). Maidenhead, UK
Victor C, Scambler S, Bond J, Bowling A (2000) Being alone in later life: loneliness, social isolation and living alone. Rev Clin Gerontol 10(4):407–417
Victor C, Sullivan M, Woodbridge R, Thomas M (2015) Dancing with loneliness in later life: a pilot study mapping seasonal variations. Open Psychol J 8(1):97–104
Victor CR, Bowling A (2012) A longitudinal analysis of loneliness among older people in Great Britain. Aust J Psychol 146(3):313–331. https://doi.org/10.1080/00223980.2011.609572
Victor CR, Scambler SJ, Bowling ANN, Bond J (2005) The prevalence of, and risk factors for, loneliness in later life: a survey of older people in Great Britain. Ageing Soc 25(6):357–375. https://doi.org/10.1017/s0144686x04003332
Victor CR, Yang K (2012) The prevalence of loneliness among adults: a case study of the United Kingdom. J Psychol 146(1–2):85–104. https://doi.org/10.1080/00223980.2011.613875
Wenger GC, Davies R, Shahtahmasebi S, Scott A (1996) Social isolation and loneliness in old age: review and model refinement. Ageing Soc 16(3):333–358. https://doi.org/10.1017/s0144686x00003457
Yang K, Victor C (2011) Age and loneliness in 25 European nations. Ageing Soc 31(8):1368–1388. https://doi.org/10.1017/s0144686x1000139x
Zavaleta D, Samuel K, Mills C (2014) Social isolation: a conceptual and measurement proposal. OPHI Working Paper 67, Oxford University. University of Oxford, Oxford
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Research involving human participants
ᅟ
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the Ethics Committee of the University of Crete and with 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Disclosure of potential conflicts of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Vozikaki, M., Papadaki, A., Linardakis, M. et al. Loneliness among older European adults: results from the survey of health, aging and retirement in Europe. J Public Health (Berl.) 26, 613–624 (2018). https://doi.org/10.1007/s10389-018-0916-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10389-018-0916-6