Abstract
This study aimed to evaluate the role of interleukin (IL)-1 inhibitors anakinra (ANA) and canakinumab (CAN) in the treatment of Behçet’s disease (BD)-related uveitis. Multicenter retrospective observational study includes 19 consecutive BD patients (31 affected eyes) received treatment with anti-IL-1 agents. Data were analyzed at baseline and at 3 and 12 months. The primary endpoint is the reduction of ocular inflammatory flares (OIF). The secondary endpoints are improvement of best corrected visual acuity (BCVA); reduction of macular thickness defined by optical coherence tomography (OCT) and of vasculitis identified with fluorescein angiography (FA); evaluation of statistically significant differences between patients treated with IL-1 inhibitors as monotherapy, subjects also administered with disease modifying anti-rheumatic drugs (DMARDs) and/or corticosteroids as well as between patients administered with IL-1 inhibitors as first line biologic treatment and those previously treated with TNF-α inhibitors. At 12 months, OIF significantly decreased from 200 episodes/100 patients/year to 48.87 episodes/100 patients/year (p < 0.0001). The frequency of retinal vasculitis identified by FA significantly decreased between baseline and 3- and 12-month follow-up visits (p < 0.0001 and p = 0.001, respectively). OIF rate was significantly higher in patients co-administered with DMARDs (81.8 episodes/100 patients/year) than in patients undergoing IL-1 inhibitors as monotherapy (0.0 episodes/100 patients/year) (p = 0.03). No differences were identified on the basis of corticosteroid use and between patients administered with IL-1 inhibitors as first line biologic approach or second line. Steroid dosage was significantly decreased at 12-month visit compared to baseline (p = 0.02). Treatment with IL-1 inhibitors is effective in the management of BD-related uveitis and provides a long-term control of ocular inflammation in refractory and long-lasting cases.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Behçet’s disease (BD) is a chronic and relapsing multi systemic inflammatory disorder at the crossroad between autoimmune and autoinflammatory diseases. Recurrent oral aphthosis, genital ulcers, skin lesions, and severe intraocular inflammation leading to sight-threatening sequelae are the main features of BD [1]. In BD patients, uveitis is the most significant cause of morbidity ranging from 50 to 70% of cases; in this context, blindness is reported with a frequency rate of about 25% [2–5]. According to the European League Against Rheumatism (EULAR) recommendations for the management of BD uveitis, the aim of treatment is to rapidly and effectively suppress intraocular inflammation to prevent irreversible damage due to posterior segment involvement, mainly defined by the presence of retinal vasculitis with a significant ischemic element [6]. Therefore, treatment of BD uveitis is often tailored according to the severity of clinical features while control of inflammation with new alternative therapeutic tools should be attempted when conventional immunosuppressive and anti-TNFα agents have proven to be ineffective.
Our improved understanding of the molecular mechanisms involved in BD and the definition of its autoinflammatory pathogenetic nature have recently opened up new interesting sceneries in terms of local and systemic therapeutic options which might be useful in severe cases in order to avoid potentially blinding complications [7, 8]. Interleukin (IL)-1 has shown to be a key proinflammatory cytokine in BD pathogenesis and its inhibition might have a promising future among the novel therapeutic opportunities [9]. In this regard, a pilot study demonstrated a rapid and sustained reduction of intraocular inflammation in patients with BD-resistant uveitis and retinal vasculitis following treatment with gevokizumab, a recombinant humanized allosteric monoclonal antibody that binds to human IL-1β [10]. Data from prospective open label randomized trials confirmed these findings in refractory BD-related uveitis and autoimmune anterior scleritis [11, 12]. However, to date the evidence on the use of IL-1 receptor antagonist anakinra (ANA) and the anti-IL-1β antibody canakinumab (CAN) in BD uveitis mostly relies on small case series or isolated case reports [13–18].
The present study is the first at evaluating the efficacy of ANA and CAN on ocular functional, morphological, and clinical parameters in a large series of patients affected by BD-related refractory or long-standing uveitis.
Materials and methods
Medical information from 19 consecutive BD patients with refractory uveitis (31 eyes) treated with IL-1 inhibitors was retrospectively collected. Diagnosis of BD was based on International Study Group Criteria (ISGC) [19] and/or International Criteria for BD (ICBD) [20].
The primary aim of the study was to evaluate the efficacy of ANA and CAN on BD uveitis during a 12-month follow-up period. The secondary aims were (i) to evaluate the possible effect of concomitant DMARDs and corticosteroid treatment on IL-1 inhibition as monotherapy, (ii) to identify any difference in terms of efficacy between patients treated with IL-1 inhibitors as first line biologic agent and those already administered with other biologic agents, and (iii) to establish any steroid-sparing effect of IL-1 inhibition. A further ancillary aim was represented by the evaluation of efficacy of anti-IL-1 agents on overall extraocular disease activity according to BD Current Activity Form (BDCAF) [21].
Our primary endpoint was represented by the reduction of ocular flares during the 12 month of treatment with IL-1-inhibitors compared to the 12-month preceding therapy with anti-IL-1-agents.
Secondary endpoints were represented by the following: (i) improvement of best corrected visual acuity (BCVA); (ii) macular thickness reduction measured by optical coherence tomography (OCT); (iii) reduction in the occurrence of vasculitis assessed by fluorescein angiography (FA) at 3- and 12-month visits; (iv) the evaluation of statistically significant differences in terms of frequency of ocular flares, BCVA changes, macular thickness reduction, FA evidences of vasculitis between patients treated with anti-IL-1 agents as monotherapy and those undergoing IL-1 inhibitors plus DMARDs or corticosteroids; (v) the evaluation of statistically significant differences in terms of frequency of ocular flares, BCVA changes, macular thickness reduction, FA evidences of vasculitis between patients treated with IL-1 inhibitors as first biologic treatment, and those previously administered with anti-TNFα agents; and (vi) assessment of prednisone dosages (or equivalent) at the start of therapy, at 3-month and 12-month visits.
No patient presented liver virus infections, toxoplasmosis, tuberculosis, or syphilis; other liver, renal, and cardiac disorders had been ruled-out along with substance abuse and malignancies before starting anti-IL-1 treatment. According to customary monitoring of the best standard of care, all patients had been evaluated by both the rheumatologist and the ophthalmologist every 3 months or when needed (relapse or safety concerns).
An ocular flare was regarded as such when ocular inflammatory manifestations occurred after a period of remission.
Descriptive statistics was evaluated for sample size, percentages, mean, and standard deviation. The rate of ocular flares during the 12 months preceding and following the start of IL-1 inhibitors was calculated as events/100 patients/year. For statistical analysis, Graphpad Prism 6.0 software was used. In particular, ANOVA or Kruskall–Wallis test (as required) were used for quantitative variables and chi-square test for qualitative variables for comparisons among baseline and 3- and 12-month follow-up evaluations. For pair wise comparisons, we performed Fisher’s exact test for qualitative variables and Mann–Whitney U test or Student’s t test (as required) for quantitative data. Normality was evaluated by using Anderson–Darling test and significance was defined as p < 0.05.
Results
We identified 19 patients (7 males, 12 females) suffering from BD-related uveitis and treated with IL-1 inhibitors. Table 1 describes demographic and clinical data of patients enrolled.
Thirteen (68.4%) patients had undergone ANA treatment at the dosage of 100 mg/day; CAN had been administered in 3 (15.8%) patients at the dosage of 150 mg every 6 weeks; the other three patients were treated with CAN at the dosage of 150 mg every 4 weeks (n = 1), 150 mg every 8 weeks (n = 1), and 300 mg every 6 weeks (n = 1), respectively.
All patients had started IL-1 inhibitors because of refractory or long-lasting unresponsive intraocular inflammation. Figure 1 specifically describes characteristics of eye involvement. Ocular involvement was monolateral in 7 (36.8%) patients and bilateral in 12 (63.2%) subjects; on the whole, 31 eyes were interested with uveitis.
At baseline, anti-IL-1 agents were administered as monotherapy in 9 (47.4%) cases; the remaining patients were co-administered with cyclosporine A at a dosage of 2.5 mg/Kg/day (n = 4), azathioprine at a dosage of 2.5 mg/Kg/day (n = 3), methotrexate at a dosage of 7.5–10 mg/Kg/day (n = 2), and sulfasalazine at a dose of 2 g/day (n = 1). Azathioprine was introduced in a patient at 3-month evaluation because of mucocutaneous BD-related manifestations. Steroids were employed in 15 (78.9%) patients, while colchicine was never co-administered. Seven (36.8%) patients underwent IL-1 inhibition as first line biologic approach; 12 (63.2%) patients had already been administered with biologics.
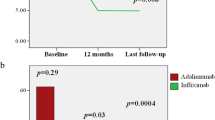
During the 12-month preceding anti-IL-1 administration, the number of ocular flares was 200/100 patients/year; this number decreased to 48.87/100 patients/year during the 12-month study period with a significant decrease during anti-IL-1 treatment compared to the preceding 12 months (p < 0.0001). Similarly, the number of patients presenting ocular flares was significantly lower during the first 12 months of anti-IL-1 treatment compared to the preceding 12 months (19/19 versus 6/19, p < 0.0001). The number of ocular flares during the study period was found significantly higher in patients co-administered with DMARDs (81.8/100 patients/year) than in patients undergoing IL-1 inhibitors as monotherapy (0.0/100 patients/year) (p = 0.03). No differences were identified on the basis of corticosteroid use (53.3 flares/100 patients/year versus 25 flares/100 patients/year, respectively; p = 0.76) and between patients administered with IL-1 inhibitors as first line biologic approach (57.1/100 patients/year) and those previously administered with other biologics (41.7 flares/100 patients/year) (p = 0.99).
Regarding retinal vascular involvement, at baseline 20 out of 31 (64.5%) eyes showed vasculitis at FA evaluation. The percentage of eyes involved with vasculitis significantly decreased to 9.7% (3/31 eyes) and 20.8% (5/24 eyes) at 3- and 12-month follow-up visits (p < 0.0001 and p = 0.001, respectively). No statistical differences were found between 3- and 12-month evaluations (p = 0.44).
Table 2 describes BCVA, central macular thickness (CMT) OCT values, and fluorangiographic evidence of active vasculitis at baseline, 3-month follow-up, and at the end of the study period. No differences were identified between groups regarding OCT changes and FA abnormalities when patients were distinguished according to the concomitant use of corticosteroids, co-administration of DMARDs, and the line of biologic approach. Conversely, BCVA values proved to be significantly higher among patients with no DMARDs co-administration both at baseline (p = 0.007) and at 3-month evaluation (p = 0.001) and at 12-month follow-up visit (p = 0.03). No significant changes were highlighted concerning BCVA values regarding the use of corticosteroids and the different lines of anti-IL-1 administration. Such data are specifically reported in Table 3.
The mean prednisone (or equivalent) dosage used was 6.11 ± 6.12 mg/day at baseline, 7.6 ± 4.2 mg/day at 3-month follow-up visit, and 5.8 ± 2.7 mg at 12-month follow-up evaluation. Steroid dosage was significantly decreased at 12-month visit compared to baseline (p = 0.02), while no statistical differences were highlighted between baseline and 3-month follow-up evaluation (p = 0.38). On the whole, 9/19 (47.36%) of patients had been treated with more than 10 mg/day of prednisone at baseline, while this number decreased to 5/19 (26.3%) at 3-month visit and at 1/15 (6.7%) at 12-month evaluation. This decrease was statistically significant (p = 0.02).
The mean BDCAF value at the start of treatment was 8.42 ± 2.21, at 3-month visit was 5.06 ± 1.62 and at 12-month follow-up was 3.5 ± 3.3. The BDCAF value was significantly reduced both at 3-month and at 12-month visits (p < 0.0001 in both cases).
During the 12-month follow-up period, no adverse events occurred; however, ANA was interrupted in 3/13 (15.4%) patients because of lack of efficacy at 3-month follow-up evaluation and in 1/13 (7.7%) at 6-month visit because of loss of efficacy; CAN was interrupted in 1/6 (16.7%) patient after 6 months because of reactivation of BD at central nervous system level.
Discussion
To the best of our knowledge, this study represents the largest series of patients with ocular BD treated with the anti-IL-1 agents ANA and CAN. These biologics achieved a rapid and sustained clinical efficacy and were able to preserve visual acuity in patients with refractory and/or long-lasting multi-resistant BD-related uveitis. In particular, IL-1 inhibition induced a significant reduction in the relapse rate and in the occurrence of retinal vasculitis.
The highly significant reduction of intraocular flares confirms that anti-IL-1 agents have a therapeutic role in the treatment of BD-related inflammation as with systemic inflammatory attacks of monogenic autoinflammatory diseases [22]. In support of this, BD has been recently classified among multifactorial autoinflammatory disorders on the basis of clinical and laboratory clues including IL-1 overproduction by inflammasome activation [22–25]. On the whole, these evidences support IL-1 involvement in the pathogenesis of BD and suggest that IL-1 may represent a potential therapeutic target for this disease as shown by the increasing number of studies on this issue [13, 14, 17, 26–31]. In this regard, we have recently published a retrospective multicenter study showing favorable results with ANA and CAN and acceptable retention rate in a cohort of 30 BD patients, 53% of them having ocular involvement [32]. Other studies explored the effectiveness of ANA and CAN treatment in BD ocular involvement, with all the limits related to the small sample size and the lack of objective ocular parameters analyzed [13–18]. However, a recent study from Wan and colleagues provided direct evidence that IL-1 signaling plays a pivotal role in the pathogenesis of uveitis [33]. The authors demonstrated that retinal myeloid cells produce IL-1β and that the reduced severity of intraocular inflammation in IL-1 receptor deficient mice correlates with impaired Th17 cell differentiation and decreased recruitment of inflammatory cells into the retina. In our cohort, the significant reduction in the number of ocular inflammatory flares was associated with a significant short- and long-term improvement of retinal vasculitis in the majority of eyes. Consequently, although the exact role of IL-1 in the pathogenesis of BD-related vasculitis has yet to be fully elucidated, the prompt and sustained remission of retinal vasculitis observed in our cohort might indirectly support IL-1 involvement at a retinal level.
Our results meet EULAR recommendations [6] that prescribe prompt and aggressive treatment in patients with active vasculitis and/or macular involvement with at least two lines loss on the visual acuity chart in order to limit the onset of sight-threatening complications. In this context, our data have shown a rapid mode of action of IL-1 inhibitors in suppressing ocular inflammation.
In order to get results based on objective outcomes, the goal of our study was to grade signs of intraocular inflammation not only through reduction of ocular inflammatory flares, but also analyzing BCVA, macular OCT values, and FA imaging on the basis of the crucial use of clinical objective measures to properly evaluate BD uveitis and response to treatment. In this regard, ophthalmic imaging instruments such as FA and macular OCT have led to a better definition of visual prognosticators in ocular BD. Specifically, given its unique role in detecting vascular leakage from retinal vessels also in eyes with no ophthalmoscopic evidence, FA remains the gold standard for evaluating the activity of retinal vasculitis in BD. In our cohort, 64.5% of eyes showed active retinal vasculitis at baseline; however, the percentage of eyes involved by vasculitis decreased to 9.7% at 3-month follow-up, thus showing a prompt and dramatic improvement of FA findings. These positive results did not significantly change between 3- and 12-month follow-up visits thus asserting the sustained clinical efficacy of IL-1 inhibition in ocular BD manifestations. Conversely, beyond the substantial positive trend of amelioration in BCVA and OCT-CMT values between the start and the end of the study period, changes did not reach statistical significance when compared to baseline. However, these results were obtained from a limited extent of patients with refractory or long-lasting ocular disease.
In our study, combination therapy of IL-1 inhibitors with immunosuppressive agents led to no superior benefit compared to monotherapy. Noteworthy, our patients co-administered with DMARDs showed a higher rate of flares compared to patients receiving anti-IL-1 agents as monotherapy. This finding could be explained with the propensity to start a more aggressive treatment in patients with a higher disease severity at baseline. In support of this, BCVA values were significantly lower in patients also administered with DMARDs already at the start of anti-IL-1 therapy.
Twelve out of 19 patients received IL-1 inhibitors as second line biologic agent after a lack or loss of efficacy to a TNFα antagonist. However, we found no differences in clinical response regarding different lines of treatment in terms of frequency of ocular inflammatory flares, occurrence of retinal vasculitis, BCVA, or OCT variations. Consequently, as for switching from the first to the second anti-TNFα agent, the failure to a previously administered biologic does not affect the response to IL-1 inhibition [34–36].
Interestingly, as reported for anti-TNFα agents [37], IL-1 inhibition was able to induce a significant reduction of steroid dosage allowing an important steroid-sparing effect during the study period. This is an important finding to take into account in order to confine both systemic and ocular steroid-related side effects.
Finally, as no adverse events were reported, the present study confirms the excellent safety profile of IL-1 inhibitors.
There are several limitations due to the retrospective observational nature of the study. The role of IL-1 inhibitors in the treatment of BD-related uveitis deserves further investigation and should be evaluated in properly designed randomized clinical trials. However, as previous data showed variable rates of drug efficacy in relation to different disease manifestations or in regard to a generalized clinical response, assessment of specific organ inflammatory activity and response to treatment represent a main goal in BD [13, 32]. In this regard, the present study is the first specifically designed to determine ANA and CAN efficacy for BD uveitis. Our analysis has been based on measurable functional, morphological, and clinical parameters allowing an objective evaluation of the response to IL-1 inhibitors.
In conclusion, our data show that ANA and CAN represent an effective and safe therapeutic option for BD-related uveitis with a significant reduction of the rate of ocular inflammatory flares, the resolution of active retinal vasculitis, the preservation of visual acuity, and the significant decrease of steroid dosages.
References
Hatemi G, Seyahi E, Fresko I, Talarico R, Hamuryudan V (2014) Behçet’s syndrome: a critical digest of the 2013–2014 literature. Clin Exp Rheumatol 32:S112–S122
Tugal-Tutkun I, Onal S, Altan-Yaycioglu R, Huseyin Altunbas H, Urgancioglu M (2004) Uveitis in Behçet disease: an analysis of 880 patients. Am J Ophthalmol 138:373–380. doi:10.1016/j.ajo.2004.03.022
Kural-Seyahi E, Fresko I, Seyahi N, Ozyazgan Y, Mat C, Hamuryudan V et al (2003) The long-term mortality and morbidity of Behçet syndrome: a 2-decade outcome survey of 387 patients followed at a dedicated center. Medicine (Baltimore) 82:60–76
Wakefield D, Cunningham ET Jr, Tugal-Tutkun I, Khairallah M, Ohno S, Zierhut M (2012) Controversies in Behçet disease. Ocul Immunol Inflamm 20:6–11. doi:10.3109/09273948.2011.649153
Salvarani C, Pipitone N, Catanoso MG, Cimino L, Tumiati B, Macchioni P et al (2007) Epidemiology and clinical course of Behçet’s disease in the Reggio Emilia area of Northern Italy: a seventeen-year population-based study. Arthritis Rheumn 57:171–178. doi:10.1002/art.22500
Hatemi G, Silman A, Bang D, Bodaghi B, Chamberlain AM, Gul A et al (2008) EULAR recommendations for the management of Behçet disease. Ann Rheum Dis 67:1656–1662. doi:10.1136/ard.2007.080432
Fabiani C, Alió JL (2015) Local (topical and intraocular) therapy for ocular Adamantiades-Behçet’s disease. Curr Opin Ophthalmol 26:546–552. doi:10.1097/ICU.0000000000000210
Ozguler Y, Hatemi G (2016) Management of Behçet’s syndrome. Curr Opin Rheumatol 28:45–50. doi:10.1097/BOR.0000000000000231
Vitale A, Rigante D, Lopalco G, Selmi C, Galeazzi M, Iannone F et al (2016) Interleukin-1 inhibition in Behçet’s disease. Isr Med Assoc J 18:171–176
Gül A, Tugal-Tutkun I, Dinarello CA, Reznikov L, Esen BA, Mirza A et al (2012) Interleukin-1β-regulating antibody XOMA 052 (gevokizumab) in the treatment of acute exacerbations of resistant uveitis of Behcet’s disease: an open-label pilot study. Ann Rheum Dis 71:563–566. doi:10.1136/annrheumdis-2011-155143
Tugal-Tutkun I, Kadayifcilar S, Khairallah M, Lee SC, Ozdal P, Özyazgan Y et al (2016) Safety and efficacy of gevokizumab in patients with Behçet’s disease uveitis: results of an exploratory phase 2 study. Ocul Immunol Inflamm 30:1–9. doi:10.3109/09273948.2015.1092558
Knickelbein JE, Tucker WR, Bhatt N, Armbrust K, Valent D, Obiyor D et al (2016) Gevokizumab in the treatment of autoimmune, non-necrotizing, anterior scleritis: results of a phase I/II clinical trial. Am J Ophthalmol. doi:10.1016/j.ajo.2016.09.017
Cantarini L, Vitale A, Scalini P, Dinarello CA, Rigante D, Franceschini R et al (2015) Anakinra treatment in drug-resistant Behcet’s disease: a case series. Clin Rheumatol 34:1293–1301. doi:10.1007/s10067-013-2443-8
Emmi G, Silvestri E, Cameli AM, Bacherini D, Vannozzi L, Squatrito D et al (2013) Anakinra for resistant Behçet uveitis: why not? Clin Exp Rheumatol 31:152–153
Caso F, Rigante D, Vitale A, Lucherini OM, Cantarini L (2014) Efficacy of anakinra in refractory Behçet’s disease sacroiliitis. Clin Exp Rheumatol 32:S171
Ugurlu S, Ucar D, Seyahi E, Hatemi G, Yurdakul S (2012) Canakinumab in a patient with juvenile Behcet’s syndrome with refractory eye disease. Ann Rheum Dis 71:1589–1591. doi:10.1136/annrheumdis-2012-201383
Vitale A, Rigante D, Caso F, Brizi MG, Galeazzi M, Costa L et al (2014) Inhibition of interleukin-1 by canakinumab as a successful mono-drug strategy for the treatment of refractory Behçet’s disease: a case series. Dermatology 228:211–214. doi:10.1159/000358125
Cantarini L, Vitale A, Borri M, Galeazzi M, Franceschini R (2012) Successful use of canakinumab in a patient with resistant Behçet’s disease. Clin Exp Rheumatol 30:S115
Criteria for diagnosis of Behçet’s disease (1990) International study group for Behçet’s disease. Lancet 335:1078–1080
International Team for the Revision of the International Criteria for Behçet’s Disease (ITR-ICBD) (2014) The international criteria for Behçet’s disease (ICBD): a collaborative study of 27 countries on the sensitivity and specificity of the new criteria. J Eur Acad Dermatol Venereol 28:338–347. doi:10.1111/jdv.12107
Neves FS, Moraes JC, Kowalski SC, Goldenstein-Schainberg C, Lage LV, Gonçalves CR (2007) Cross-cultural adaptation of the Behçet’s Disease Current Activity Form (BDCAF) to Brazilian Portuguese language. Clin Rheumatol 26:1263–1267. doi:10.1007/s10067-006-0484-y
Gül A (2015) Pathogenesis of Behçet’s disease: autoinflammatory features and beyond. Semin Immunopathol 37:413–418. doi:10.1007/s00281-015-0502-8
Mege JL, Dilsen N, Sanguedolce V, Gul A, Bongrand P, Roux H et al (1993) Overproduction of monocyte derived tumor necrosis factor alpha, interleukin (IL) 6, IL-8 and increased neutrophil superoxide generation in Behçet’s disease A comparative study with familial Mediterranean fever and healthy subjects. J Rheumatol 20:1544–1549
Castrichini M, Lazzerini PE, Gamberucci A, Capecchi PL, Franceschini R, Natale M et al (2014) The purinergic P2×7 receptor is expressed on monocytes in Behçet’s disease and is modulated by TNF-α. Eur J Immunol 44:227–238. doi:10.1002/eji.201343353
Liang L, Tan X, Zhou Q, Zhu Y, Tian Y, Yu H et al (2013) IL-1β triggered by peptidoglycan and lipopolysaccharide through TLR2/4 and ROS-NLRP3 inflammasome-dependent pathways is involved in ocular Behçet’s disease. Invest Ophthalmol Vis Scib 54:402–414. doi:10.1167/iovs.12-11047
Vitale A, Insalaco A, Sfriso P, Lopalco G, Emmi G, Cattalini M et al (2016) A snapshot on the on-label and off-label use of the interleukin-1 inhibitors in Italy among rheumatologists and pediatric rheumatologists: a nationwide multi-center retrospective observational study. Front Pharmacol 7:380. doi:10.3389/fphar.2016.00380
Caso F, Costa L, Rigante D, Lucherini OM, Caso P, Bascherini V et al (2014) Biological treatments in Behçet’s disease: beyond anti-TNF therapy. Mediat Inflamm 2014:107421. doi:10.1155/2014/107421
Pagnini I, Bondi T, Simonini G, Giani T, Marino A, Cimaz R (2015) Successful treatment with canakinumab of a paediatric patient with resistant Behçet’s disease. Rheumatology (Oxford) 54:1327–1328. doi:10.1093/rheumatology/kev197
Cantarini L, Lopalco G, Caso F, Costa L, Iannone F, Lapadula G et al (2015) Effectiveness and tuberculosis-related safety profile of interleukin-1 blocking agents in the management of Behçet’s disease. Autoimmun Rev 14:1–9. doi:10.1016/j.autrev.2014.08.008
Bilginer Y, Ayaz NA, Ozen S (2010) Anti-IL-1 treatment for secondary amyloidosis in an adolescent with FMF and Behçet’s disease. Clin Rheumatol 29:209–210. doi:10.1007/s10067-009-1279-8
Botsios C, Sfriso P, Furlan A, Punzi L, Dinarello CA (2008) Resistant Behçet disease responsive to anakinra. Ann Intern Med 149:284–286
Emmi G, Talarico R, Lopalco G, Cimaz R, Cantini F, Viapiana O et al (2016) Efficacy and safety profile of anti-interleukin-1 treatment in Behçet’s disease: a multicenter retrospective study. Clin Rheumatol 35:1281–1286. doi:10.1007/s10067-015-3004-0
Wan CK, He C, Sun L, Egwuagu CE, Leonard WJ (2016) Cutting edge: IL-1 receptor signaling is critical for the development of autoimmune uveitis. J Immunol 196:543–546. doi:10.4049/jimmunol.1502080
Takase K, Ohno S, Ideguchi H, Uchio E, Takeno M, Ishigatsubo Y (2011) Successful switching to adalimumab in an infliximab-allergic patient with severe Behçet disease-related uveitis. Rheumatol Int 31:243–245. doi:10.1007/s00296-009-1178-y
Olivieri I, Leccese P, D’Angelo S, Padula A, Nigro A, Palazzi C et al (2011) Efficacy of adalimumab in patients with Behçet’s disease unsuccessfully treated with infliximab. Clin Exp Rheumatol 29:S54–S57
Yazici H, Hatemi G (2012) Empiricism in managing Behçet’s syndrome. Clin Exp Rheumatol 30:S79
Vitale A, Emmi G, Lopalco G, Gentileschi S, Silvestri E, Fabiani C et al (2016) Adalimumab effectiveness in Behçet’s disease: short and long-term data from a multicenter retrospective observational study. Clin Rheumatol [Epub ahead of print]. doi:10.1007/s10067-016-3417-4
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
None.
Rights and permissions
About this article
Cite this article
Fabiani, C., Vitale, A., Emmi, G. et al. Interleukin (IL)-1 inhibition with anakinra and canakinumab in Behçet’s disease-related uveitis: a multicenter retrospective observational study. Clin Rheumatol 36, 191–197 (2017). https://doi.org/10.1007/s10067-016-3506-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10067-016-3506-4