Abstract
Purpose
To evaluate clinical outcomes and enucleation rates after intravitreal melphalan (IVM) alone and after IVM combined with intravitreal topotecan (IVT) for the treatment of vitreous disease, and to a lesser extent subretinal and retrohyaloid seeds, in patients with retinoblastoma.
Study design
A retrospective analysis of 77 eyes of 72 consecutive patients.
Methods
Demographic data, classification of tumors, seed type (dust, sphere or cloud) before injection and at the end of follow-up, injection type (IVM or IVM+IVT), doses of IVM and IVT, number of injections, follow-up time, enucleation status and side effects were recorded. Cox regression analysis and log-rank test for Kaplan-Meier curves were performed.
Results
Of 77 eyes, 40 received IVM alone (group 1) and 37 received IVM+IVT (group 2). Enucleation rates were 62.5% (n=25) in group 1 and 10.8% (n=4) in group 2 (p=0.001). Median eye survival was 23.6 months in group 1 and 25.6 months in group 2. Mantel-Cox test revealed statistically significant differences between Kaplan-Meier curves of group 1 and 2 (p=0.022). Multiple Cox regression analysis showed a significantly elevated enucleation rate associated with: IVM only treatment group (p=0.019) and pre-injection cloud type of seeding (p=0.014).
Conclusion
The combined use of intravitreal melphalan and topotecan provides significantly better results in terms of avoiding enucleation and vitreal and subretinal seed control.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The earliest documented descriptions of clinical and histopathological features of vitreous seeding in retinoblastoma can be traced in the seminal work of Hugo Wintersteiner published in 1897. In his book, Wintersteiner alluded in great details to cases reported by Da Gama Pinto, Iwanoff, Treitel, Grolmann, Bock, Agnew and Eno, and Wolff but cited Franz Rompe as the first to have ever reported “retinal gliomas metastasizing to the vitreous body” [1]. Rompe described a 1-year-old girl whose left eye had a large number of white, small glioma clumps in the vitreous. The eye was enucleated and 2/3 of the vitreous was found to be filled with friable retinal tumor [2]. The girl was followed for 2.5 years without any recurrence [2]. In the modern era, the interest in vitreous seeds was rekindled by Amemiya et al. [3] who demonstrated that most of the vitreous seeds were composed of necrotic cells around a blood vessels which had fibrocytes but no pericytes, and that seeding was most frequently associated with undifferentiated endophytic-type retinoblastomas. They concluded that since most of the seeds were made up of “neuroephithelial” type retinoblastoma cells, not all seeds were malignant [3].
Attempts to save eyes with vitreous disease have always been challenging and often frustrating. Cassady et al. [4] observed local tumor control in 15% of group Vb eyes following supervoltage radiotherapy. A later study used improved radiotherapy techniques and reports an ocular survival rate of 53.4% at 10 years for Vb eyes [5]. Plaque brachytherapy was found effective only for localized seeds but not for extensive seeding involving multiple quadrants [6].While standard systemic chemotherapy had negligible effects on vitreous seeds, intra-arterial chemotherapy was able to salvage 65% of eyes with Group C and 45% of Group D disease, which encompass subretinal and/or vitreous retinoblastoma seeding by definition [7]. Intravitreal chemotherapy ushered a new era in the management of vitreous diseases and several studies report remarkably high salvage rates for eyes that would have otherwise been enucleated [8,9,10,11,12]. The current knowledge on intravitreal injections mostly come from studies with melphalan, though there are few reports on the combination of melphalan and topotecan [9, 12].
The aim of this study was to determine whether the combination of intravitreal melphalan and topotecan yielded better results in the management of vitreous and subretinal seeds associated with retinoblastoma in terms of ocular survival and seeding control compared to intravitreal melphalan alone.
Materials and methods
This was a non-randomized retrospective study of 77 eyes of 72 patients who received intravitreal injections in the form of either intravitreal melphalan (IVM) alone or IVM combined with intravitreal topotecan (IVT) for vitreous disease associated with retinoblastoma, between March 2012 and May 2018. An institutional board review approval was obtained for intravitreal injection of melphalan (Alkeran, GlaxoSmithKline) and topotecan (Hycamtin, GlaxoSmithKline).In addition, legal permission was also obtained from the Turkish Ministry of Health for each patient and for each procedure. The study adhered to the tenets of the Declaration of Helsinki.
Collected data included age at injection, gender, laterality of the tumor and injections, grouping of the tumors according to Los Angeles version of the international classification of retinoblastoma (IIRC) [13], presence of history for additional systemic or intraarterial chemotherapy, type of injection (IVM or IVM+IVT), mean doses of melphalan and topotecan, type and location of seeding before injection and at the end of follow-up, clinical response of seeds at the end of follow-up, follow-up time, number of injections, enucleation status and time to enucleation from first injection. The vitreous seeds were morphologically grouped as dust, sphere and cloud, based on the classification devised by Munier [14]. If more than one type of seeding were present, the predominant type with highest category was recorded. The location of the seeds was noted as: retrohyaloid, intravitreal, subretinal or intracameral. The follow-up time for each eye was defined as the time from the first injection to last visit; or to enucleation, if the eye had to be enucleated. Clinical response to treatment of seeds was recorded in compliance with the patterns previously described by Munier [14] (type 0: complete disappearance of the seeds, type I: conversion into refringent and/or calcified residues, type II: conversion into amorphous, non-spherical inactive residues, and type III: a combination of types I and II), stable seeds, or progression of the seeds. Eyes which received anterior chamber injections were excluded from analysis.
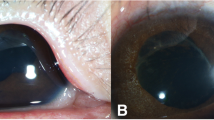
All injections were performed under general anesthesia and under operating microscope. In order to improve outcomes with fewer injections, between 2012 and 2015 we only used IVM, from 2016 on we routinely switched to IVM+IVT. Between 2012-2015, we performed 1-2 minutes of digital ocular massage before IVM in order to attain ocular hypotony and to avoid possible post-injection reflux. From 2016 with the start of combined IVM and IVT, we performed anterior chamber paracentesis uniformly to all eyes with a 30G needle. Melphalan was prepared at a concentration of 10-20 µg/0.1 ml, and topotecan at 20 µg/0.1ml. Absence of retinal detachment and a viable tumor at the needle entry site were ensured with indirect ophthalmoscopy prior to any injection. A visible optic nerve head was a prerequisite in all cases. All injections were carried out through the parsplana using a 30-gauge needle. First, melphalan was given, only the syringe was removed and then topotecan in the second syringe was administered through the same needle. Transconjunctival cryotherapy over the entry site was initiated while the needle was retrieved from the eye. The eye was then gently shaken with cotton-tip applicator to achieve a wider drug distribution. Seed response was assessed qualitatively and reinjection was considered if viable seeds were present after follow-up examinations every two weeks. Side effects, if any, were noted and retinal toxicity was graded according to the system proposed by Munier [14]. Indications to cease intravitreal treatment were similar to those of Suzuki et al. [15] and can be summarized as: observation of one of the regression patterns defined by Munier (Types 0, 1, 2, 3) [14] and progression of seeding. Seed progression despite injections was either managed by intravenous/intraarterial chemotherapy or enucleation.
Descriptive statistics for quantitative and qualitative variables are shown as median (25th and 75th percentiles) and numbers and percentages, respectively. Shapiro-Wilk normality tests were assessed for quantitative variables in each IVM and IVM+IVT groups. To compare quantitative variables for IVM and IVM+IVT groups, the Mann-Whitney U test statistic was chosen since it was observed that there are no significant results showing the normality assumption. Chi-Square test and Fisher’s exact test were performed to determine the association between groups and quantitative variables.
Survival probabilities were estimated via Kaplan-Meier method for IVM and IVM+IVT groups and compared via log-rank test statistic. Univariate Cox proportional hazards models were constructed whenever p-value was less than 0.25 the variable is chosen as candidate variable. With candidate variables, multiple Cox proportional hazard models with backward elimination were conducted. Besides, hazard ratios with 95% confidence intervals were presented. A receiver operating characteristics (ROC) analysis to determine the dose of melphalan to be used to avoid enucleation was observed.
The level of statistical significance was set at p<0.05. All reported p-values are 2-sided. Data were analyzed using IBM SPSS Statistics for Windows v.23.0 (IBM Corp.). Kaplan-Meier curves were drawn by using the survminer package in RStudio (2018) version 1.0.136.
Results
Of 72 enrolled patients, 41 (56.9%) were men and 31 (43.1%) were women. The median age at injection was 35 months (23.5, 35.0 and 47.0 months for 25th, 50th and 75th percentile, respectively). Bilateral disease was found in 33 (45.8%) patients. The classification of tumors at the time of retinoblastoma diagnosis in the injected eyes was group B in 6 eyes (7.8%), group C in 35 eyes (45.5%), and group D in 36 eyes (46.8%). Among these patients, 49 eyes (63.6%) had undergone systemic chemotherapy, 67 eyes (87.0%) had received intraarterial chemotherapy at some time during follow-up for the injected eye, and 41 eyes (53.2%) had received both. There was no time preference with respect to last chemotherapy and the injections were performed whenever seeding was detected and continued until complete disappearance or complete calcification and inactivation was achieved. The median number of injections was 1 (range:1-7). A single injection was performed in 42 (54.5%) eyes, 2 injections in 17 (22.1%) eyes, and 3 injections in 9 (11.7%) eyes. The median dose of melphalan per injection was 30 µg (range: 10-50 µg) and for topotecan it was 13 µg (range: 5-20 µg). Only one eye, in the IVM group, had received 50 µg IVM injection as an extreme salvage measure because the other eye had been enucleated due to advanced disease, and the injected eye was preserved during the 5-month follow up period. In the rest of the eyes the upper limit of injected melphalan range was 40 µg. The type and location of seeds at the time of injection and at the last follow-up are shown in Figure 1. Pre-injection location of the seeds was mainly vitreous (88.3%, n=68), 2 eyes had mainly retrohyaloid seeds upon fundoscopy and 6 had predominantly subretinal seeds. The only eye which had anterior chamber seeding at the time of injection was in the IVM+IVT group, and the injection of chemotherapy in that eye was carried out intravitreally for vitreal disease, followed by additional melphalan injection to anterior chamber. Enucleation was performed in this eye one month later due to disease progression. Eyes with post-injection anterior chamber seeding were managed with enucleation. Complete regression, calcification, amorphous inactive residue or a combination of the last two were observed in 44 (57.1%) eyes, progression in 21 (27.3%) eyes, and no change in 12 (15.6%) eyes at the last follow-up. Aforementioned variables of the IVM and the IVM+IVT groups are listed in Table 1. The median follow-up time was 9 months (range: 6-54 months). Eventually 29 of 77 eyes (37.6%) had to be enucleated, and median time from the first injection to enucleation was 8 months (range: 2-54 months). Twenty-five of the enucleated eyes were in the IVM group and 4 in the IVM+T group. The reasons for enucleation were extensive progression of the vitreous disease in 10 eyes, progression of retinal tumors in 10 eyes, massive anterior chamber invasion in 6 eyes, and dense vitreous hemorrhage that did not clear after 2 months in 3 eyes. At initial diagnosis, 17 of these eyes had group D, 10 had group C, and 2 had group B tumors. Before the start of intravitreal injections, 14 eyes had sphere type, 9 had cloud type, and 6 had dust types of seeding. The median number of injections in the enucleated eyes was 2 (range: 1-6).
Seed frequency distribution. Frequency distribution of a type of seed frequency b frequency of dominant seed location at the time of first injection (pre-injection) and at the end of follow-up (post-injection) in 67 eyes. a Frequency of cloud, sphere and dust types in the pre-injection column are: 27.3% (n=21), 48.1% (n=37), 24.7% (n=19); that of post-injection column are: 14.3% (n=11), 23.4% (n=18), 62.3 (n=48), respectively. b Frequency of retrohyaloid, vitreal, sub-retinal, and intracameral seeds in the pre-injection column are: 2.6% (n=2), 88.3% (n=68), 7.8% (n=6), 1.3% (n=1); that of post-injection column are: 2.6% (n=2), 83.1% (n=64), 5.2% (n=4), 9.1% (n=7), respectively
The IVM and IVM+T groups had no statistically significant differences in terms of median age at injection, laterality, frequency of systemic chemotherapy or intraarterial chemotherapy, median number of injections, pre- and post- injection seed type, and clinical response patterns. However, the two groups differed significantly in gender (p=0.032), median melphalan dose (<0.001), median follow-up time (0.028), and enucleation rate (0.001).
Kaplan-Meier analysis (Fig. 2) showed that the median ocular survival was 28.0 months (standard error: 6.4, 95% CI:15.5-40.5), 23.6 months in the IVM group (standard error: 3.6, 95% CI:16.6-30.6) and 25.6 months in the IVM+IVT group (standard error: 2.2, 95% CI:21.4-29.9). Mantel-Cox test revealed statistically significant differences between ocular survival curves of these two groups, favoring the IVM+IVT group (p=0.022).
To determine which variables among the ones listed in Table 2 affected the enucleation rates, backward elimination Cox regression was performed in order to define the parameters to be included in the multiple Cox regression analysis. Based on the regression analysis, enucleation rates were found to be significantly related to the treatment group (IVM or IVM+IVT) (p=0.019) and pre-injection type of seeding (p=0.014). More explicitly, the IVM group had a 3.633 fold risk for enucleation compared to IVM+IVT (p=0.019, 95% CI: 1.241-10.639) and pre-injection cloud type of seeding represented 3.864 times increase in the risk of enucleation compared to dust type (p=0.014, 95% CI: 1.310-11.399) (Table 2).
The study had not been primarily designed to obtain a cut-off value, rather the data was reviewed retrospectively and the results of ROC analyses including all 77 eyes were used to determine a cut-off value for melphalan dose related to enucleation; a threshold value of 29 µg melphalan was found to predict enucleation with 0.467 sensitivity and 0.894 specificity (area under the curve=0.727, standard error=0.061).
Treatment complications were encountered in 20 eyes (10 in the IVM and 10 in the IVM+T groups) and included vitreous hemorrhage in 8 eyes, peripheral retinal pigment epithelial mottling in 3 eyes (grade 3), retinal pigment epithelial atrophy in the macular area in 4 eyes (grade 4), wide chorioretinal atrophy in 2 eyes (grade 5), posterior synechiae in 2 eyes, and sectoral iris depigmentation in 1 eye. All complications occurred in eyes receiving more melphalan than 33.5 µg. There was no case of extraocular extension, metastasis, or death at a median follow-up of 9 months.
Discussion
Topotecan, a camptothecin analogue, is a selective topoisomerase I inhibitor ultimately causing cellular apoptosis through irreversible DNA damage, and is also an inhibitor of hypoxia inducible factor [16, 17]. A study on a three-dimensional organoid model derived from human retinoblastoma cell lines demonstrates higher efficacy of combined melphalan (20 µg) and topotecan (30 µg) compared with melphalan alone on vitreous seeds [18]. A study of 9 human eyes 3 of which had group E tumors, reports complete response of vitreal seeds in all cases following a combination of 8-20 µg topotecan and 30 µg melphalan administration with a median number of 2 intravitreal injections [12]. Shields et al. [9] note a 100% control rate 3 years after administering combined IVM+IVT in 11 eyes. They achieved these results in 98% of eyes using melphalan< 30 µg, and in 90% of eyes using topotecan< 20 µg [9]. In a report on 17 eyes with refractory and recurrent seeds, Rao et al. [17] suggest that intravitreal topotecan alone at the dose of 30 µg can cause total seed regression in all eyes following a median number of 3 injections. Our study showed that compared to intravitreal melphalan alone, the combined use of intravitreal melphalan and topotecan significantly improved intravitreal and subretinal seed control and significantly decreased the enucleation rate (62.5% in the IVM group vs. 10.8% in the IVM+IVT group). The unexpectedly high failure rate in the IVM group in the present study deserves further comment since we previously reported an enucleation rate of 44% in a different cohort of patients receiving IVM alone for vitreous disease [11]. In that study, we performed more injections (median: 2 injections) and more than 51% of eyes received between 30-40 µg of melphalan, marginally higher than the IVM alone group in the current study [11]. Furthermore, routine anterior chamber paracentesis in the combined treatment group allowed delivering significantly higher doses of melphalan compared to the mono agent group (median dose of melphalan: 36 µg, and 30 µg in IVM+IVT and IVM groups respectively, p< 0.001). Therefore, the concomitant use of topotecan and a higher dose of melphalan may account for the significantly increased globe salvage rate in the combined treatment group of our study.
In our series, eyes with sphere type of seeds had the highest number of enucleations, however, we found that the risk of enucleation increased 4-fold when the vitreous disease was predominantly cloud type before intravitreal treatment, and almost 8- fold if cloud type seeding persisted following intravitreal injections. It is demonstrated that class 3 clouds that develop at a relatively older age and in unilateral cases, are more common between ora and equator, and show diffuse distribution [19]. Francis et al.[20] show that compared to dust and spheres, clouds responded significantly later taking 30 to 32 weeks to regress, required significantly more injections (median: 8), and the highest cumulative melphalan dose. Similarly, Berry et al. [21] report that a median number of 6 injections, and a cumulative dose of 195 µg were needed for total regression of clouds. A recent histopathological study reveals that clouds were composed mainly of necrotic material and that viable cells were only found at the outer rim [22]. The authors relate the limited response of clouds to treatment to the relative lack of viable cells [22]. They then conclude that “clouds may not necessitate treatment with the same vigor of spheres or dust given their low burden and peripheral location of viable tumor cells” [22]. This important observation challenges the commonly accepted fear of clouds, and we believe that in a small subset of our patients with persistent clouds, enucleations were prematurely performed. Therefore, the statistically significant increase of enucleation risks associated with clouds in our study must be interpreted with caution. Although clouds received considerable attention in recent literature, it is worth to note that recurrences, and enucleations are most commonly associated with spheres [11, 19,20,21, 23]. Our current results are in line with these observations.
We observed a clinical trend of gradual morphological disintegration of seeds from cloud and sphere to dust after each consecutive injection, as a general response pattern, suggesting a mechanical breakdown of seeds. This finding may invalidate our policy of managing with the least possible number of injections, and particularly with a single injection. A single injection must be considered unsafe and unreliable in most instances, given 100% success rates after a median number of 3 injections for dust, 5 injections for spheres, and 8 injections for cloud types of seeds [20]. This is confirmed by several other studies [8,9,10, 18, 19, 21]. As shown in Figure 1B, the location of the seeds, their debris following treatment, and recurrences, i.e. vitreal, subretinal or retrohyaloid, did not change throughout the follow-up in the majority of our patients. Similar to the results of Abramson et al. [24], we found IVM or IVM+T highly effective against subretinal, if not vitreal seeds.
The weaknesses of this study are its retrospective nature and lack of randomization. The ocular salvage rate of 37.5% in the IVM group and 89.2% in the IVM+T group of our study may appear modest compared to other recently published studies. This may perhaps be explained by the lesser number of injections performed at our center. More studies are needed for the optimization of melphalan and topotecan doses and injection intervals. As a future direction, globe volumes, which can be calculated from MRI studies, can be used to individualize intravitreal drug doses. A limitation in terms of statistical analysis was that repeat injections were not taken as time varying covariates because more than half of the eyes (54.5%) had received a single injection.
In conclusion, our study demonstrates significant improvements in terms of ocular survival, vitreous disease, and subretinal seed control with the use of combined intravitreal melphalan and topotecan injections compared to melphalan alone. Also, a melphalan dose of less than 29 µg per single injection was associated with higher enucleation rates, and a dose exceeding 33.5 µg per single injection caused more frequent retinal toxicity.
References
Wintersteiner H. Das Neuroëpitheliomaretinae; eine anatomische und klinische Studie. Franz Deuticke, Leipzig, 1897:66–67. (Accessed through Bayerische StaatsBibliothek, http://daten.digitale-sammlungen.de/bsb00071808/image_80) (in German).
Wintersteiner H. Das Neuroëpitheliomaretinae; eine anatomische und klinische Studie. Franz Deuticke, Leipzig, 1897:368–369. (Accessed through Bayerische StaatsBibliothek, http://daten.digitale-sammlungen.de/bsb00071808/image_382) (in German).
Amemiya T, Yoshida H, Ishigooka H. Vitreous seeds in retinoblastoma, clinical significance and ultrastructure. Albrecht v Graefes ArchKlin Exp Ophthalmol. 1979;211:205–13.
Cassady JR, Sagerman RH, Tretter P, Ellsworth RM. Radiation therapy in retinoblastoma. An analysis of 230 cases. Radiology. 1969;93:405–9.
Abramson DH, Beaverson KL, Chang ST, Dunkel IJ, McCormick B. Outcome following initial external beam radiotherapy in patients with Reese-Ellsworth group Vb retinoblastoma. Arch Ophthalmol. 2004;122:1316–23.
Shields JA, Shields CL, DePotter P, Hernandez JC, Brady LW. Plaque brachytherapy for residual or recurrent retinoblastoma in 91 cases. J Pediatr Ophthalmol Strabismus. 1994;31:242–5.
Suzuki S, Yamane T, Mohri M, Kaneko A. Selective ophthalmic arterial injection therapy for intraocular retinoblastoma: the long-term prognosis. Ophthalmology. 2011;118:2081–7.
Munier FL, Gaillard MC, Balmer A, Soliman S, Podilsky G, Moulin AP, et al. Intravitreal chemotherapy for vitreous disease in retinoblastoma revisited: from prohibition to conditional indications. Br J Ophthalmol. 2012;96:1078–83.
Shields CL, Douglass AM, Beggache M, Say EA, Shields JA. Intravitreous chemotherapy for active vitreous seeding from retinoblastoma: Outcomes after 192 consecutive injections. The 2015 Howard Naquin Lecture. Retina. 2016;2016(36):1184–90.
Francis JH, Brodie SE, Marr B, Zabor EC, Mondesire-Crump I, Abramson DH. Efficacy and toxicity of intravitreous chemotherapy for retinoblastoma: four-year experience. Ophthalmology. 2017;124:488–95.
Kiratli H, Koc I, Varan A, Akyuz C. Intravitreal chemotherapy in the management of vitreous disease in retinoblastoma. Eur J Ophthalmol. 2017;27:423–7.
Ghassemi F, Shields CL, Ghadimi H, Khodabandeh A, Roohipoor R. Combined intravitreal melphalan and topotecan for refractory or recurrent vitreous seeding from retinoblastoma. JAMA Ophthalmol. 2014;132:936–41.
Murphree LA. Intraocular retinoblastoma: the case for a new group classification. Ophthalmol Clin N Am. 2005;18:41–53.
Munier FL. Classification and management of seeds in retinoblastoma. Ellsworth lecture Ghent August 24th 2013. Ophthalm Genet. 2014;35:193–207.
Suzuki S, Aihara Y, Fujiwara M, Sano S, Kaneko A. Intravitreal injection of melphalan for intraocular retinoblastoma. Jpn J Ophthalmol. 2015;59:164–72.
Yuan S, Friedman DL, Daniels AB. Alternative chemotherapeutic agents for the treatment of retinoblastoma using the intra-arterial and intravitreal routes: a path forward toward drug discovery. Int Ophthalmol Clin. 2017;57:129–41.
Rao R, Honavar SG, Sharma V, Reddy VAP. Intravitrealtopotecan in the management of refractory and recurrent seeds in retinoblastoma. Br J Ophthalmol. 2018;102:490–5.
Saengwimol D, Rojanaporn D, ChaitankarV, Chittavanich P, Aroonroch R, Boontawon T, et al. A three-dimensional organoid model recapitulates tumorigenic aspects and drug responses of advanced human retinoblastoma. Sci Rep. 2018;8:15664.
Francis JH, Marr BP, Abramson DH. Classification of vitreous seeds in retinoblastoma: correlations with patient, tumor, and treatment characteristics. Ophthalmology. 2016;123:1061–5.
Francis JH, Abramson DH, Gaillard M-C, Marr BP, Beck-Popovic M, Munier FL. Classification of vitreous seeds in retinoblastoma and response to intravitrealmelphalan. Ophthalmology. 2015;122:1173–9.
Berry JL, Bechtold M, Shah S, Zolfaghari E, Reid M, Jubran R, et al. Not all seeds are created equal: seed classification is predictive of outcomes in retinoblastoma. Ophthalmology. 2017;124:1817–25.
Amram AL, Rico G, Kim JW, Chintagumpala M, Herzog CE, Gombos DS, et al. Vitreous seeds in retinoblastoma: clinicopathologic classification and correlation. Ophthalmology. 2017;124:1540–7.
Francis JH, Iyer S, Gobin YP, Brodie SE, Abramson DH. Retinoblastoma vitreous seed clouds (class 3). A comparison of treatment with ophthalmic artery chemosurgery with or without intravitreous and periocular chemotherapy. Ophthalmology. 2017;124:1548–55.
Abramson DH, Ji X, Francis JH, Catalanotti F, Brodie SE, Habib L. Intravitreal chemotherapy in retinoblastoma: expanded use beyond intravitreal seeds. Br J Ophthalmol. 2018. https://doi.org/10.1136/bjophthalmol-2018-312037.
Acknowledgements
The authors thank Professor Tero Kivelä from Helsinki, Finland, for his invaluable contribution in providing historical material.
Funding
No financial support was received for this submission.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
H. Kiratli, None; I. Koç, None; E. Öztürk, None; A. Varan, None; C. Akyüz, None.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Corresponding Author: Hayyam Kiratli
About this article
Cite this article
Kiratli, H., Koç, I., Öztürk, E. et al. Comparison of intravitreal melphalan with and without topotecan in the management of vitreous disease in retinoblastoma. Jpn J Ophthalmol 64, 351–358 (2020). https://doi.org/10.1007/s10384-020-00743-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10384-020-00743-2