Abstract
Purpose
To investigate the safety and efficacy of intravitreal injection of melphalan for retinoblastoma.
Methods
A retrospective chart review of all patients who were administered intravitreal injections of melphalan for retinoblastoma between 1990 and 2011. A total of 264 eyes of 250 patients were included. All ocular adverse events, systemic prognosis, ocular prognosis, and visual acuity were investigated.
Results
The total number of intravitreal injections administered was 1,067; each eye received between one and 25 injections. A postoperative subconjunctival tumor developed in one eye. None of the eyes suffered infections or uveitis, and all other adverse events including chorioretinal atrophy displayed incidences of less than 1.5 %. At 5 postoperative years, the cumulative incidence of cataract surgery was 3.1 % among the eyes that were treated without ocular hyperthermia. Distant metastasis or intracranial invasion occurred in 11 patients, all of whom had high-risk pathological factors for metastasis such as optic nerve invasion, but refused to receive adjuvant chemotherapy. Sixty-eight percent of the eyes achieved complete vitreous seed remission, but recurrence occurred in 19 % of these eyes after 10.0 ± 4.9 months. In addition, 47 and 27 % of the eyes without primary macular tumors retained visual acuity of >0.5 and >1.0, respectively.
Conclusions
The risk of extraocular tumor spreading following intravitreal injections is low, and other adverse events are rare. Sixty-eight percent of the treated eyes achieved complete vitreous seed remission, and about half of them retained practical levels of vision. The intravitreal injection of melphalan is a safe and effective treatment for vitreous seeds.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Vitreous seeding, defined as the spread of viable tumor cells within the vitreous cavity, is a form of intraocular retinoblastoma in which it is difficult to salvage the eye [1]. The condition is classified as a form of advanced stage disease; i.e., into group Vb in the Reese–Ellsworth classification and into T2 or higher in the TNM classification system [2]. Some eyes in which vitreous seeding develops can be salvaged with external beam radiotherapy, and Abramson [3] reports a 5-year eye preservation rate of 53.4 % for the technique. Systemic chemotherapy is also an effective eye salvage treatment, and Shields [4, 5] reports that at 5 post-treatment years neither external beam radiotherapy nor enucleation had been required in 47 % of patients treated with systemic chemotherapy. Recently, intra-arterial chemotherapy was also demonstrated as effective eye salvage treatment; one study found that it achieved complete responses in 67 % of eyes in which vitreous seeds developed [6] and another obtained a 2-year ocular salvage rate of 64 % for naive eyes containing vitreous seeds [7]. It also resulted in the complete or partial regression of vitreous seeds in 10 of 15 eyes in an Asian population [8].
Vitreous seeding is difficult to treat due to the presence of the blood-retinal barrier and the fact that, as there is no vasculature in the normal vitreous cavity, only low concentrations of anti-cancer drugs reach the vitreous cavity. Various treatment approaches for vitreous seeding have been reported, e.g., the application of cryotherapy just before intravenous chemotherapy to destroy the blood-retinal barrier [9], subconjunctival injections [10], iontophoresis [11], adenovirus-mediated delivery of thymidine kinase and ganciclovir [12] and direct intravitreal injection of melphalan [1].
For ophthalmologists, intravitreal drug injection is both a simple and a familiar treatment method, but it carries a risk of infection, bleeding and retinal damage [13]. Extraocular spread of tumor cells via the needle tract is the most severe adverse event associated with intravitreal injections for intraocular malignancies and can result in orbital disease or distant metastasis. Due to the danger of the extraocular spread of cancer cells, intravitreal injections for retinoblastoma were initially considered very risky or contraindicated, and only a few cases involving the procedure are reported in the literature [1].
We started administering intravitreal injections of melphalan during clinical practice in 1990, initially as a salvage therapy for refractory vitreous seeding after external beam radiotherapy [1]. Recently, some promising results have been reported for intravitreal injection therapy [14–20]; however, there are no long-term data about the technique. Herein, we describe our long-term results for intravitreal injection therapy, including the safety of the technique and the incidence rates of adverse events.
Materials and methods
This study involved a retrospective, non-comparative, interventional case series. Institutional review board approval was obtained from the National Cancer Center, and the study was conducted in accordance with the Declaration of Helsinki. Written informed consent was obtained from all patients. All patients who received intravitreal injection therapy before the end of December 2011 were included in this study. A retrospective medical chart review was performed, and clinical data including information about the age of the patients at the time of primary treatment, the laterality of each patient’s condition, the pre-treatment tumor stage, the primary treatment modality, any additional treatment, the condition of each eye at the time of the initial intravitreal injection, the total number of intravitreal injections, drug doses, adverse events, ocular prognosis, visual acuity and systemic prognosis, including the risk of extraocular tumors developing, were collected.
The primary endpoint of this study was to clarify the safety of intravitreal injections and the incidence of adverse events. The efficacy of intravitreal injection therapy was employed as a secondary endpoint.
Treatment strategy
At our institution, until 1998 external beam radiotherapy was used as the main primary treatment for salvaging eyes containing tumors, when it was replaced with systemic intravenous chemotherapy consisting of vincristine, etoposide and carboplatin. In addition, some eyes were treated with primary intra-arterial chemotherapy. Eyes containing small tumors were treated with primary local treatment including laser therapy, cryotherapy, or plaque radiotherapy. After the primary treatment, additional treatment, including laser therapy, cryotherapy, plaque radiotherapy, intra-arterial chemotherapy delivered using a balloon catheter [21], external beam radiotherapy and systemic chemotherapy, were applied depending on the status of the tumor. Ocular hyperthermia, performed according to the Lagendijk method [22], was also employed before 2002.
Intravitreal injections were only administered as adjuvant treatment in cases involving vitreous seeds. The number of intravitreal injections was not determined beforehand; instead, the injections were repeated until funduscopy demonstrated that the vitreous seeds had disappeared; had been totally calcified, or seemed to be inactive, e.g., if they were membranous or sand-like. In cases in which vitreous seeds went into remission, we examined the affected eye periodically, usually every month for 6 months and then bimonthly for 12 months. Additional intravitreal injections were administered in cases in which recurrent vitreous seeds developed.
During local treatment, eyes that exhibited dense intraocular hemorrhage, refractory vitreous seeds after several rounds of intravitreal injections, residual or recurrent tumors involving the optic nerve head, or suspected optic nerve invasion were enucleated. Eyes that demonstrated anterior chamber invasion were recommended for enucleation, but some eyes were treated with a combination of radiotherapy, intra-arterial chemotherapy, ocular hyperthermia, and intravitreal injections. Post-enucleation systemic adjuvant chemotherapy was recommended for patients with high-risk pathological factors, e.g., post-laminar optic nerve invasion, scleral or extra-scleral invasion, massive choroidal invasion, or cut-end optic nerve invasion.
Drugs used and intravitreal injection dose
We used only melphalan (Alkeran®, GlaxoSmithKline, Tokyo, Japan) for the intravitreal injection therapy. Under sterile conditions, melphalan was diluted with natural saline just prior to its injection in the operating room. Until 2001, the standard dose of melphalan was 8 μg in 0.2 ml solution; from 2001 to 2008 it was changed to 8 μg in 0.1 ml solution, and thereafter to 16 μg in 0.05 ml solution. The eyes that remained refractory to treatment after several intravitreal injections at the standard dose were treated with a higher dose of 24 μg.
Intravitreal injection procedure
All intravitreal injections were performed under general anesthesia. Prior to each injection, the pupil was dilated, and the fundus was examined in detail to assess the size and location of any retinal tumors, the degree of vitreous seeding, and the condition of the pars plana. The eyelid and ocular surface were disinfected using 0.025 % benzalkonium chloride solution (Germitol® Water, Maruishi Pharmaceutical, Osaka, Japan) according to the standard method for ocular operations. After draping the surgical field, the eye was opened with a Bangerter solid blade speculum to direct the eyelashes away from the operative field. The eye was then fixed in place with forceps, and the needle was inserted at 3 mm from the corneal limbus toward the center of the eye. The tip of the needle was inserted into the eye in such a manner that it did not enter any dense regions of vitreous seeds.
Until 2001 pre-injection paracentesis involving the injection of 0.2 ml solution was employed, but was not performed thereafter. Diluted melphalan was directly injected into the vitreous cavity as a bolus; then, the injection site was grasped with forceps, the needle was removed quickly, and the injection site was rubbed with forceps to facilitate the closure of the needle tract. The eyeball was then shaken for several seconds to facilitate the distribution of the drug within the vitreous cavity, before a scleral massage was performed to normalize the intraocular pressure. Paracentesis was performed whenever it was difficult to reduce the intraocular pressure. After the intraocular pressure had been normalized, betamethasone sodium phosphate ointment containing fradiomycin sulfate (Rinderon A®, Shionogi & Co., LTD, Osaka, Japan) was applied, and betamethasone sodium phosphate eye drops containing fradiomycin sulfate (Rinderon A®, Shionogi & Co.) were administered 3 times a day for 1 week as a prophylactic treatment against uveitis and infection.
The injection site was usually located in the region around the 12 o’clock meridian. However, if dense vitreous seeds or retinal tumors were detected at this location, the ophthalmologist performed the injection at another site in the superior half of the eye.
Until October 1998, 27-gauge needles were used for the intravitreal injections, and from October 1998 until December 2002, 30-gauge needles were used. After December 2002, 32-gauge custom-made needles were employed. The 32-gauge needles measured 20 mm in length, which made them easy to use for intravitreal injections and reduced the risk of retinal injuries caused by the needle being inserted too far.
Results
Between 1990 and 2011, 906 retinoblastoma patients visited our hospital, and 264 eyes in 250 patients were subjected to eye-preserving treatment involving intravitreal injection therapy. There were 128 male and 122 female subjects, and the mean age at the first intravitreal injection was 29 ± 14 months (range: 3–236 months, median: 26 months). Of these, 110 patients had unilateral disease and 140 patients had bilateral disease, and 14 patients received intravitreal injections OU. In total, 1,067 injections were administered. External beam radiotherapy (144 eyes), systemic chemotherapy (90 eyes), intra-arterial chemotherapy (25 eyes), or other local therapies (5 eyes) were used as initial treatment.
The initial tumor stage was distributed from A to E according to the International Classification for Intraocular Retinoblastoma and is shown according to needle gauge in Fig. 1. There was no difference in tumor stage among any of the needle gauge groups. Each eye received one to 25 intravitreal injections (Fig. 2), depending on the status of the patient’s tumor (mean: 3.9, median: 3).
Ocular adverse events
The ocular adverse events experienced by our patients are summarized according to needle gauge in Table 1. None of the eyes in this cohort suffered infections or uveitis.
A postoperative subconjunctival tumor developed in one eye, which contained a residual tumor and vitreous seeds in the superior region near the ora serrata after the initial round of external beam radiotherapy. The eye had to be enucleated after 5 intravitreal injections and 4 sessions of intra-arterial chemotherapy. The subconjunctival tumor was detected intraoperatively and confirmed pathologically to have been caused by the extraocular spread of retinoblastoma cells around the puncture site. The patient was treated with additional chemotherapy without exenteration, and at the time of writing has been doing well for more than 10 years and remains metastasis-free.
Diffuse chorioretinal atrophy occurred in two eyes. One of these eyes had received external beam radiotherapy combined with ocular hyperthermia and one round of intra-arterial chemotherapy. In this case, diffuse chorioretinal atrophy occurred several months after the administration of three intravitreal injections. Whilst no tumor recurrence has occurred after 19 years, the eye cannot perceive light. The other eye was treated with external beam radiotherapy, and 3 intravitreal injections were administered for residual vitreous seeds. Diffuse chorioretinal atrophy occurred 1 month after the last treatment. However, no recurrent tumors have developed after 10 years, and the eye retains visual acuity of 0.05.
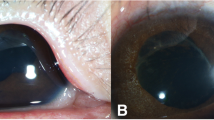
Iris atrophy or de-pigmentation occurred in 3 eyes, which had received 9, 16, and 18 intravitreal injections. Two of these eyes were salvaged, and one was enucleated.
No rhegmatogenous retinal detachment occurred, but proliferative retinal detachment occurred in one eye. This eye contained a group E tumor, and after initial external beam radiotherapy, 2 sessions of cryotherapy and one session of combination therapy involving intra-arterial chemotherapy and an intravitreal injection were administered. However, proliferative vitreoretinopathy developed, resulting in total retinal detachment.
Vitreous hemorrhaging developed immediately after intravitreal injections in two eyes. Both eyes had received treatment, including external beam radiotherapy and intra-arterial chemotherapy, and were eventually removed because the hemorrhages had not been absorbed after more than 6 months.
Twenty eyes required cataract surgery due to the difficulty of examining the fundus or a reduction in visual acuity. Most of these eyes had diffuse cortical cataracts and initially exhibited posterior subcapsular opacity. Nineteen of the 20 eyes had received external beam radiotherapy. Seventeen of these eyes (85 %) had also received ocular hyperthermia, which was performed using the Lagendijk method [22]. The incidences of cataract surgery among the patients that did and did not undergo ocular hyperthermia are shown in Fig. 3. The 5-year cumulative incidence of cataract surgery was 0.159 in the ocular hyperthermia group and 0.031 in the no ocular hyperthermia group (p = 0.0019). Postoperative tumor recurrence occurred in one eye after external beam radiotherapy combined with ocular hyperthermia. As a result, 6 sessions of combined treatment involving intravitreal injections and intra-arterial chemotherapy were administered. During the last operation, the tumor seemed to be inactive, but a mature cataract subsequently developed and was extracted 3 months later. Thirteen months later, the tumor recurred in the anterior chamber, and the eye was enucleated. No extraocular tumor recurrence or metastasis has developed after 15 years.
Systemic outcomes
Distant metastasis or direct invasion into the brain occurred in 11 patients in this cohort, and 5 of them also suffered orbital recurrence. All had high-risk pathological factors for metastasis (ciliary body or anterior chamber invasion: 6 eyes, scleral invasion: 2 eyes, massive choroidal invasion: 2 eyes, post-laminar optic nerve invasion: 1 eye), but refused to receive adjuvant chemotherapy. Five of the 11 patients are currently healthy after having received adjuvant chemotherapy and/or radiotherapy, 5 patients died, and one patient dropped out from follow-up whilst receiving adjuvant chemotherapy. Another 2 patients who had refused to undergo enucleation and stopped visiting our hospital, subsequently returned with massive intraocular tumors and orbital invasion. These were treated with intensive adjuvant chemotherapy, but the patients died due to brain invasion.
Eleven secondary neoplasms developed in 10 patients, and all of these had also received external beam radiotherapy and intra-arterial chemotherapy [21]. Nine patients had bilateral retinoblastoma, and one had unilateral retinoblastoma. These neoplasms included 6 osteosarcomas (within the radiation field: 2, outside the radiation field: 4), 2 rhabdomyosarcomas (both within the radiation field), 1 sarcoma (unspecified type, within the radiation field), 1 Ewing’s sarcoma (within the radiation field), and 1 case of acute myeloid leukemia.
Efficacy of intravitreal injections
Among the 264 eyes treated with intravitreal injections, 19 eyes from 19 patients were excluded from the efficacy study. Of these, 17 patients received additional treatment at another hospital and dropped out from our follow-up program, and two patients refused to have the affected eye enucleated, which resulted in orbital invasion. As a result, 245 eyes from 231 patients were included in this part of the study.
Each eye received one or more treatments including external radiotherapy, systemic chemotherapy, and intra-arterial chemotherapy (Table 2). In total, 149 eyes received external radiotherapy, 91 eyes received systemic chemotherapy, and 221 eyes received intra-arterial chemotherapy.
At the time of the initial intravitreal injection, some eyes were also suffering from additional tumor-based conditions including anterior chamber invasion (6 eyes), diffuse subretinal seeds (29 eyes), massive retinal tumors (156 eyes), or minimal residual retinal tumors that were controllable with local treatment (54 eyes) (Table 3).
Four of the 6 (67 %) eyes with anterior chamber invasion were eventually enucleated. The other two eyes received intravitreal injections and ocular hyperthermia (one eye) or intravitreal injections combined with intra-arterial chemotherapy and ocular hyperthermia (one eye). Both of these eyes were salvaged, and neither of them suffered any subsequent recurrence or metastasis.
The efficacy of the intravitreal injection of melphalan was analyzed in the 239 eyes that did not exhibit primary anterior chamber invasion (Fig. 4). In total, 72 eyes were enucleated due to residual tumors, 4 eyes were enucleated due to secondary anterior chamber invasion, and 163 eyes (68 %) achieved complete vitreous seed remission. At the last follow-up, 132 out of 163 eyes were still in complete remission, and the mean period from the last intravitreal injection to the last follow-up was 124.7 ± 49.5 months (range: 8–269 months, median: 124 months). Recurrent vitreous seeds developed in 31 eyes, and the mean period from the last intravitreal injection to recurrence was 10.0 ± 4.9 months (range: 3–33 months, median: 9 months). Additional treatment including intravitreal injections was administered in these cases, and 9 eyes achieved secondary remission. Seven out of the 9 eyes were still in remission at the last follow-up, and the mean follow-up period after the last intravitreal injection was 126.1 ± 52.5 months (range: 33–256 months, median: 118 months). Recurrent vitreous seeds developed in the other 2 eyes, but remission was achieved for a third time in both eyes after additional intravitreal injections, and no recurrence has occurred for 56 and 66 months, respectively, in these cases.
The best corrected visual acuity scores of the patients with and without primary macular tumors are shown in Fig. 5. Any subjects whose visual acuity could not be determined due to mental retardation or very young age were excluded. Thirty (47 %) of the 64 eyes without macular tumors maintained practical levels of visual acuity; i.e., better than 0.5, and 17 eyes (27 %) retained normal visual acuity; i.e., better than 1.0. The subjects with macular tumors had limited vision, and 44 (83 %) out of 53 eyes retained visual acuity of less than 0.1.
Discussion
We first started performing intravitreal injection therapy in July 1990. The first patient to be treated with this technique had bilateral retinoblastoma, and his right eye was enucleated. After 24 Gy proton radiotherapy, photodynamic therapy, and three sessions of intra-arterial melphalan-based chemotherapy, his right eye still contained active vitreous seeds, and three intravitreal injections of melphalan were administered. Eventually, the eye had to be removed, but a good initial response to the intravitreal injection therapy was observed.
Intravitreal injection is a very simple method that allows specified intravitreal drug concentrations to be achieved. Higher drug doses are advantageous for tumor control, but can damage the retina or intraocular structures. We only use melphalan for intravitreal injections, and no data is reported about the intravitreal injection of other drugs. Inomata and Kaneko [23] investigated the sensitivity of retinoblastoma to 12 anti-cancer drugs including l-phenylalanine mustard (melphalan), adriamycin, cisplatin, and vincristine and found that 0.4 μg/ml melphalan had the greatest effect. Ueda et al. [24] studied the optimal dose of melphalan for intravitreal injections using rabbit retinas and electroretinography. They found that the injection of 10 μg melphalan did not cause electroretinographic or histopathological changes, whereas the administration of 20 μg melphalan induced minimal electroretinography and histopathological changes. Injecting 10 μg melphalan into a rabbit eye results in an intravitreal concentration of about 5.9 μg/ml, assuming that the drug is homogenously distributed throughout the vitreous cavity. We started administering intravitreal injections of 8 μg melphalan, equivalent to an intravitreal concentration of 2 μg/ml in adult eyes, 3 μg/ml in the eyes of 1-year-olds, and 4 μg/ml in the eyes of newborns. However, some eyes displayed a poor response to 8 μg melphalan, so, in 2008, we increased the dose to 16 μg, which is equivalent to an intravitreal concentration of 5.3 μg/ml in the eyes of 1-year-olds and 8 μg/ml in those of newborns. We used intravitreal injections as a salvage treatment, and most patients who received intravitreal injections were older than 6 months of age; therefore, we consider that a dose of 16 μg is reasonable.
Intravitreal injections can cause the extraocular spread of tumor cells via the needle tract, infection, bleeding, and uveitis. The extraocular spread of tumor cells is the most serious adverse event associated with intravitreal injections in eyes with intraocular tumors. Among the 1,067 intravitreal injections we administered to 264 eyes, only one eye developed a postoperative subconjunctival tumor. That eye contained active retinal and vitreous seeds around the injection site, which could have contributed to the extraocular spread experienced in this case. Thereafter, we selected the injection sites more carefully via detailed fundus examinations and ensured that they did not contain any vitreous or retinal tumors and were located as far away from vitreous seeds as possible. As a result, no further extraocular tumors were experienced. To reduce the risk of extraocular tumor spread, Munier [17] recommends that cryoapplication should be performed at the injection site just after the removal of the needle. This might reduce the risk of the extraocular spread of tumor cells, yet, according to the present study, extraocular tumor cell spreading only occurs in 0.4 % of cases, so the risk is minimal.
Munier [17] also recommends performing paracentesis before intravitreal injections. Vitreous tapping was possible in our early cases in which we used 27-gauge needles, but was not possible in the cases in which 30- or 32-gauge needles were used. In the latter cases, we did not perform paracentesis before the intravitreal injections, and directly injected a volume of 0.05 ml of diluted melphalan. To decrease the risk of reflux, we rubbed the injection site with forceps and massaged the eye to push the tissue surrounding the injection site together and facilitate closure of the needle tract. The benefits and risks of paracentesis should be investigated in a future study.
We used 27-, 30-, and 32-gauge needles during the study period; the needles were mainly selected based on their availability rather than the comparative advantages of each gauge. The eyes treated with 27-gauge needles suffered relatively high rates of adverse ocular events, as shown in Table 1, including one case of extrascleral spread; thus, the use of thick needles might facilitate tumor cell reflux from the needle tract. To minimize the risk of reflux from the needle tract, the use of thinner needles is recommended. We have used 32-gauge custom-made needles from December 2002 onwards, and such needles are now commercially available in Japan (Dentronics®, Handaya Co., Ltd, Tokyo, Japan).
Anterior chamber involvement refers to tumors that have invaded beyond the ora serrata, pars plana invasion, or posterior chamber seeds. The 6 eyes that exhibited anterior chamber involvement did not suffer extraocular tumor spread after the intravitreal injections, which might mean that there is a low risk of tumor spread via the needle tract, even in cases exhibiting anterior chamber involvement. However, such eyes should be treated very cautiously with intravitreal injections because of the risk of extraocular spread if aqueous humor reflux occurs.
We encountered 11 patients who developed extraocular disease after intravitreal injections, but all the treated eyes had histopathological or imaging risk factors for metastasis. It is impossible to exclude the possibility of tumor spread via the needle tract having occurred in these cases, but we consider that it was unlikely because all of the patients suffered metastasis without subconjunctival tumor formation.
Endophthalmitis is another severe ocular adverse event associated with intravitreal injections. Aiello et al. [13] produced guidelines for intravitreal injections, which recommended the selection of a pars plana injection site in the inferotemporal quadrant. Injection sites in the inferotemporal quadrant are easy to approach and make it possible to prevent the patient’s eyelashes coming into contact with the needle. Intravitreal injections for retinoblastoma are always administered under general anesthesia, so approaching from the superior quadrant is also easy in such cases. In addition, we use a Bangerter solid blade speculum to direct the eyelashes away from the surgical field in order to reduce the risk of infection.
Two eyes suffered diffuse chorioretinal atrophy, which may be due to adverse drug reactions; however, the eyes in question had only received three intravitreal injections, and no chorioretinal atrophy occurred in the eyes that were administered more frequent intravitreal injections. Other possible causes for the chorioretinal atrophy experienced in these cases include vascular spasms or reduced choroidal blood flow due to increased intraocular pressure. Adverse drug reactions are unavoidable, but it is recommended that the intraocular pressure should be checked and a fundus examination should be performed to assess retinal blood flow immediately after intravitreal injections to reduce the risk of vascular problems.
Twenty (8.0 %) of the treated eyes required cataract surgery, which is a relatively high proportion. External radiotherapy is known to facilitate cataract formation, and 19 of these 20 eyes had also received external radiotherapy. Seventeen of the 20 eyes had undergone ocular hyperthermia using the Lagendijk method [22], in which the whole eye is heated with microwaves to 45 °C. There is no accurate lens temperature data for this method, but it does warm the lens, possibly resulting in cataract formation. The 5-year morbidity rate of cataract surgery without ocular hyperthermia was 3.1 %, which is acceptable. Most of the cataracts we experienced initially presented as posterior subcapsular opacity, which was not limited to the lesion around the injection site, so it is hardly conceivable that the mechanical damage caused by the injection needle contributed to their formation. We consider it reasonable that external radiotherapy and ocular hyperthermia were the main causes of these cataracts.
Assessing the efficacy of intravitreal injections from our data is very difficult because this study involved a retrospective analysis of data for patients with various eye conditions. Eyes with simple vitreous seeds are rare, and most of the eyes we encountered also contained active retinal tumors, which would have reduced the ocular survival rate, and many of the eyes were subjected to concomitant treatments including radiotherapy and other chemotherapeutic modalities. In total, 163 out of 239 eyes (68 %) achieved complete vitreous seed remission. Thirty-one of these eyes developed recurrent seeds, and complete remission was achieved for a second time in 9 of the 31 eyes. Two of the 9 eyes subsequently developed recurrent seeds, and complete remission was achieved for a third time in both. It was considered that the intravitreal injections were the main instigator of the complete remission achieved in these cases. To evaluate the true effect of intravitreal injections, a prospective study involving eyes containing vitreous seeds without retinal tumors or with minimal retinal tumors should be carried out.
The assessment of vitreous seed activity is another problem. It is evaluated using funduscopy, which is subjective; therefore, it is sometimes difficult to determine an appropriate course of injections and/or the optimal time to stop treatment. We administered intravitreal injections until the vitreous seeds disappeared or were inactivated, and one additional injection was usually administered for consolidation. More than 80 % of the treated eyes remained in remission, but about 20 % suffered vitreous seed recurrence. The mean period from the last intravitreal injection to the detection of recurrent vitreous seeds was 10.0 ± 4.9 months (range: 3–33 months, median: 9 months), and 10 (32 %), eyes suffered recurrence within 6 months, 22 eyes (70 %) within 12 months, and 30 eyes (97 %) within 24 months. Therefore, careful fundus examinations should be performed for at least 24 months after intravitreal melphalan injections for retinoblastoma.
Maintaining sufficient visual acuity is one of the most important purposes of eye preservation. Good visual acuity requires good retinal function; therefore, any administered treatments should exhibit low toxicity to intraocular structures. Visual acuity is influenced by tumor location and size, concomitant retinal detachment, and treatment-induced retinal damage. Of the eyes without primary macular tumors, 47 % retained practical levels of vision: a visual acuity better than 0.5. However, some of these eyes suffered macular implantation or retinal detachment, which will have affected the latter results. The follow-up period from the last treatment was longer than 5 years in most cases (longest: 138 months). Thus, this study did not obtain any prognostic data for patients that had been followed-up for 12 years or more, but our findings indicate that intravitreal injections do not cause severe retinal damage in the medium term. A previous study describes the retinal function (according to electroretinography) of a patient who had received intravitreal melphalan injections for retinoblastoma [25], and optical coherence tomography-based studies will provide further information about postoperative retinal function in such cases.
In conclusion, intravitreal injections carry a minimal risk of extraocular spread, and the ocular damage they cause is very limited. It is clear that intravitreal injections have positive effects against vitreous seeds, but these effects should be investigated further.
References
Kaneko A, Suzuki S. Eye-preservation treatment of retinoblastoma with vitreous seeding. Jpn J Clin Oncol. 2003;33:601–7.
Sobin LH, Gospodarowics MK, Wittekind C, editors. Retinoblastoma. In: TNM classification of malignant tumors. 7th ed. UK: Wiley-Blackwell; 2010. p. 291–7.
Abramson DH, Beaverson KL, Chang ST, Dunkel IJ, McCormick B. Outcome following initial external beam radiotherapy in patients with Reese-Ellsworth group Vb retinoblastoma. Arch Ophthalmol. 2004;122:1316–23.
Shields CL, Honavar SG, Meadows AT, Shields JA, Demirci H, Singh A, et al. Chemoreduction plus focal therapy for retinoblastoma: factors predictive of need for treatment with external beam radiotherapy or enucleation. Am J Ophthalmol. 2002;133:657–64.
Shields CL, Mashayekhi A, Au AK, Czyz C, Leahey A, Meadows AT, et al. The international classification of retinoblastoma predicts chemoreduction success. Ophthalmology. 2006;113:276–80.
Shields CL, Bianciotto CG, Jabbour P, Ramasubramanian A, Lally SE, Griffin GC, et al. Intra-arterial chemotherapy for retinoblastoma: report No. 1, control of retinal tumors, subretinal seeds, and vitreous seeds. Arch Ophthalmol. 2011;129:1399–406.
Abramson DH, Marr BP, Dunkel IJ, Brodie S, Zabor EC, Driscoll SJ, et al. Intra-arterial chemotherapy for retinoblastoma in eyes with vitreous and/or subretinal seeding: 2-year results. Br J Ophthalmol. 2012;96:499–502.
Ong SJ, Chao AN, Wong HF, Liou KL, Kao LY. Selective ophthalmic arterial injection of melphalan for intraocular retinoblastoma: a 4-year review. Jpn J Ophthalmol. 2014 [Epub ahead].
Wilson TW, Chan HS, Moselhy GM, Heydt DD Jr, Frey CM, Gallie BL. Penetration of chemotherapy into vitreous is increased by cryotherapy and cyclosporine in rabbits. Arch Ophthalmol. 1996;114:1390–5.
Abramson DH, Frank CM, Dunkel IJ. A phase I/II study of subconjunctival carboplatin for intraocular retinoblastoma. Ophthalmology. 1999;106:1947–50.
Eljarrat-Binstock E, Domb AJ, Orucov F, Dagan A, Frucht-Pery J, Pe’er J. In vitro and in vivo evaluation of carboplatin delivery to the eye using hydrogel-iontophoresis. Curr Eye Res. 2008;33:269–75.
Chévez-Barrios P, Chintagumpala M, Mieler W, Paysse E, Boniuk M, Kozinetz C, et al. Response of retinoblastoma with vitreous tumor seeding to adenovirus-mediated delivery of thymidine kinase followed by ganciclovir. J Clin Oncol. 2005;23:7927–35.
Aiello LP, Bruchker AJ, Chang S, Cunningham ET Jr, D’Amico DJ, Flynn HW Jr, et al. Evolving guidelines for intravitreous injections. Retina. 2004;24:S3–19.
Kivelä T, Eskelin S, Paloheimo M. Intravitreal methotrexate for retinoblastoma. Ophthalmology. 2011;118:1689–90.
Ghassemi F, Shields CL. Intravitreal melphalan for refractory or recurrent vitreous seeding from retinoblastoma. Arch Ophthalmol. 2012;130:1268–71.
Smith SJ, Pulido JS, Salomao DR, Smith BD, Mohney B. Combined intravitreal and subconjunctival carboplatin for retinoblastoma with vitreous seeds. Br J Ophthalmol. 2012;96:1073–7.
Munier FL, Gaillard MC, Balmer A, Soliman S, Podilsky G, Moulin AP, et al. Intravitreal chemotherapy for vitreous disease in retinoblastoma revisited: from prohibition to conditional indications. Br J Ophthalmol. 2012;96:1078–83.
Munier FL, Soliman S, Moulin AP, Gaillard MC, Balmer A, Beck-Popovic M. Profiling safety of intravitreal injections for retinoblastoma using an anti-reflux procedure and sterilisation of the needle track. Br J Ophthalmol. 2012;96:1084–7.
Smith SJ, Smith BD, Mohney BG. Ocular side effects following intravitreal injection therapy for retinoblastoma: a systematic review. Br J Ophthalmol. 2014;98:292–7.
Shields CL, Manjandavida FP, Arepalli S, Kaliki S, Lally SE, Shields JA. Intravitreal melphalan for persistent or recurrent retinoblastoma vitreous seeds: preliminary results. JAMA Ophthalmol. 2014;132:319–25.
Suzuki S, Yamane T, Mohri M, Kaneko A. Selective ophthalmic arterial injection therapy for intraocular retinoblastoma: the long-term prognosis. Ophthalmology. 2011;118:2081–7.
Kaneko Akihiro. Management of retinoblastoma—how to preserve eyeballs of children with retinoblastoma [in Japanese]. J Eye. 2002;19:585–91.
Inomata M, Kaneko A. Chemosensitivity profiles of primary and cultured human retinoblastoma cells in a human tumor clonogenic assay. Jpn J Cancer Res. 1987;78:858–68.
Ueda M, Tanabe J, Inomata M, Kaneko A, Kimura T. Study on conservative treatment of retinoblastoma—effect of intravitreal injection of melphalan on the rabbit retina. Nippon Ganka Gakkai Zasshi. 1995;99:1230–5 [in Japanese].
Brodie SE, Munier FL, Francis JH, Marr B, Gobin YP, Abramson DH. Persistence of retinal function after intravitreal melphalan injection for retinoblastoma. Doc Ophthalmol. 2013;126:79–84.
Acknowledgments
This study was supported by the National Cancer Center Research and Development Fund (26-A-25).
Conflicts of interest
S. Suzuki, None; Y. Aihara, None; M. Fujiwara, None; S. Sano, None; A. Kaneko, None.
Author information
Authors and Affiliations
Corresponding author
About this article
Cite this article
Suzuki, S., Aihara, Y., Fujiwara, M. et al. Intravitreal injection of melphalan for intraocular retinoblastoma. Jpn J Ophthalmol 59, 164–172 (2015). https://doi.org/10.1007/s10384-015-0378-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10384-015-0378-0