Abstract
Purpose
Echinococcosis, also known as hydatidosis, is a zoonosis that is endemic in many countries worldwide. Liver hydatid cysts have a wide variety of clinical manifestations, among which obstructive jaundice is one of the rarer forms. The aims of the study were to analyze the preoperative management of these patients and to record the kind of surgical treatment performed and the short- and long-term postoperative results.
Methods
A retrospective two-center observational study of patients operated upon for liver hydatidosis with initial symptoms of obstructive jaundice. Preoperative characteristics, surgical data, and postoperative complications, including biliary fistula, were recorded.
Results
Of 353 patients operated upon for liver hydatidosis, 44 were included in the study. Thirty-five patients (79.6%) were defined as CE2 or CE3 in the World Health Organization (WHO) classification. Preoperative endoscopic retrograde cholangiopancreatography (ERCP) was performed in 25 patients (56.8%) and identified intrabiliary communication in 29. Radical surgery was carried out in 29 of the total sample (65.9%). Severe postoperative complications (Clavien-Dindo grade IIIA or higher) were recorded in 25% of patients. The factors associated with greater postoperative morbidity were age above 65 (HR 8.76 [95% CI 0.78–97.85]), cyst location (HR 4.77 [95% CI 0.93–24.42]), multiple cysts (HR 14.58 [95% CI 1.42–149.96]), and cyst size greater than 5 cm (HR 6.88 [95% CI 0.95–50]).
Conclusion
The presentation as obstructive jaundice causes greater postoperative morbidity. The main postoperative complication in these cases, despite radical surgery, is biliary fistula. In our series, routine preoperative ERCP did not show any benefit.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Hydatid disease, also known as echinococcosis, is a zoonosis that is endemic in many parts of the world, caused by the larvae of the Echinococcus tapeworm. Humans become intermediate hosts in the parasite’s life cycle by entering into contact with infested animals [1,2,3]. Despite progress in controlling the disease, echinococcosis continues to be a major health problem in endemic areas [1, 3]; although its course is generally mild, some of its complications are serious and potentially lethal [4].
Liver echinococcosis is usually asymptomatic. Depending on the stage of the disease, its clinical presentation at the time of diagnosis may vary widely. Around one-third of patients present a range of complications [2]. Depending on their size and location, the cysts can cause symptoms such as abdominal pain and discomfort due to the compression of adjacent structures [1]; they may cause obstructive jaundice, either by compressing the bile duct or by rupturing it and creating a communication through which it is invaded by daughter hydatids or remains of hydatid membrane [5], with clinical manifestations such as cholangitis or biliary fistulas [1]. This cystobiliary communication is the most common complication, occurring in between 2 and 42% of patients (the wide range is due to the absence of a clear definition) [6]. It occurs more frequently in cysts located in the central area of the liver or near the hilum, and in large and/or multivesicular cysts [7].
Around 10–12% of patients have jaundice as the main symptom at the time of diagnosis. In these cases, surgery is indicated to avoid secondary complications such as new episodes of cholangitis and/or sepsis [5]. Although there is lack of evidence that supports different treatment options, the evidence supporting pharmacological treatment is weak. Medical treatment is used to reduce cysts, decrease infectiveness, and avoid relapses, and is based on drugs of the benzimidazole family, usually albendazole or mebendazole [8].
Preoperative endoscopic retrograde cholangiopancreatography (ERCP) is not routinely performed. Some centers recommend its use in order to fully determine the anatomy of the bile ducts and to establish whether there is communication between the bile ducts and the cyst [9].
The aims of this study were to evaluate the preoperative management of these patients, postoperative results, and postoperative morbidity in patients with hepatic hydatidosis presenting obstructive jaundice as the main symptom at diagnosis, and to assess the value of performing preoperative ERCP.
Material and methods
The work has been reported in line with the PROCESS criteria [10] and has been registered in ClinicalTrials.gov with identification number NCT04271176. The study was approved by the ethical committee of our institutions.
Data collection
The retrospective two-center observational study of prospectively recorded data on liver hydatidosis in patients with jaundice at the time of diagnosis was carried out at hepatopancreatobiliary surgical units at two hospitals between January 2006 and September 2018. The hospitals have catchment areas of 250,000 and 1,000,000, respectively.
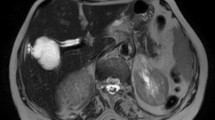
Patients diagnosed with hepatic hydatidosis whose main symptom at diagnosis was obstructive jaundice were included in this study. Demographic and clinical data of the patients were taken from their clinical histories, including age, sex, medical history of hydatidosis, clinical findings, laboratory data, radiological findings, preoperative or postoperative endoscopic treatment, and surgical treatment. Preoperative diagnosis was based on abdominal ultrasound (US) and computerized tomography (CT) scan. Hydatid cysts were grouped into subtypes based on the World Health Organization (WHO) classification. Radiological findings suggestive of cystobiliary communication were biliary dilatation and the presence of echogenic material in the biliary tree without posterior acoustic shadows [2].
Usually, in patients with complicated hydatid cysts, e.g., patients with obstructive jaundice at diagnosis, albendazole 1 month before surgery is prescribed.
Preoperative ERCP was not protocolized, and the decision to perform it was taken on a patient-to-patient basis. This was also the case of the indication of sphincterotomy and the use of a biliary stent. In patients with high preoperative bilirubin or confirmed cystobiliary communication, preoperative ERCP allows the cleaning of the bile duct, thus avoiding its opening during the surgery and reducing the risk of postoperative biliary fistula. The Endoscopist makes the decision to place the prosthesis based on the state of clearance of cyst material, the difficulty of cannulation, and the presence or absence of bile infection.
Postoperative evolution, hospital stay, treatment administered, and general and specific complications such as the appearance of biliary fistula were recorded. Postoperative morbidity was classified according to the Clavien-Dindo score [11]. Complications classified as IIIa or above on the Clavien-Dindo scale were defined as severe. Bile leakage is defined according to ISGLS definition [12].
Sometimes, in patients with high preoperative bilirubin, cholangitis, large or multiple cysts, or confirmed frank cystobiliary communication, preoperative treatment with albendazole 1 month before surgery is applied.
Surgical technique
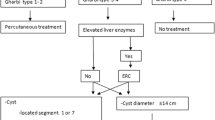
Precautions were taken to avoid spillage of the parasite into the abdominal cavity. The peritoneal cavity was liberally protected with scolicidal agents. All patients underwent intraoperative ultrasound in order to locate any cysts which might have been missed in the preoperative imaging and also to establish the relation of the cyst to the large vessels. All patients underwent open surgery. The type of surgery to be performed was decided based on the intraoperative findings and on the location and size of the cyst: either radical (closed and open total cystopericystectomy, or hepatic resection) or conservative (partial cystopericystectomy, extraction of the vesicles with external or internal drainage) (Fig. 1). We usually prefer to perform parenchymal sparing techniques; however, a hepatectomy was performed when the cyst affected a total lobe and/or the main pedicles. A partial cystectomy was performed when the cyst wall abutted important vascular and biliary structures and risked causing injury.
Follow-up
Patients were followed up with ultrasound or CT scan and hydatid serology for at least 6 months. Relapse was defined as the appearance of new active liver cysts after the patient had undergone surgery to treat the disease [3].
Statistical analysis
Categorical (demographic and clinical) variables were compared using the chi-square test, and interval variables using Student’s t test or the ANOVA test. For univariate and multivariate analyses, logistic regression models were applied, estimating the respective odds ratio (OR) and its 95% confidence interval. The Kaplan-Meier method was used to evaluate patients’ overall survival. A p value of < 0.05 was considered significant. Statistical studies were performed using Statistical Package for the Social Sciences (SPSS) v. 21.0.
Results
Out of 353 patients with liver hydatidosis, 44 had jaundice (12.5%): nine out of 75 patients from one hospital (12%) and 35 out of 278 from the other (12.6%). Of the 44 patients, 16 were women (36.4%) and 28 men (63.6%), with a median age of 47.86 years (range 14.87–89.8). In the population areas at our two centers, the incidence was 30 and 27.8 cases per 100,000 inhabitants, respectively.
Nine patients (20.5%) had a previous history of interventions for pulmonary or hepatic hydatidosis. Thirty-three (75%) presented a complicated cyst at diagnosis (Table 1). Of the patients with uncomplicated hydatid cysts, only one patient had a history of prior hydatidosis and all cysts were single. Most cysts were classified as CE2 or CE3 according to the WHO classification (Table 2). Hydatid serology was performed in 17 patients (38.6%) and was positive in 15 (88.2%).
Regarding cyst location, 23 patients presented cysts in the right liver (52.3%) and 17 in the left liver (38.6%) and four were bilobar. The median number of cysts was 1 (IQR 1–2) with 72.7% of the sample presenting a single cyst. The median size of the cysts was 7 (IQR 5–10) cm.
Preoperative ERCP was performed in 25 cases (56.8%). In 20 (45.5%), intraoperative sphincterotomy was performed, and in six of these patients, a biliary prosthesis was inserted. In the remaining five cases with preoperative ERCP, no hydatid material was observed in the bile duct during the procedure; nor was any communication with the bile duct recorded. The mean maximum bilirubin prior to surgery or biliary drainage was 4.7 mg/dl (IQR 2.6–7.6).
As Tables 3 and 4 show, the groups of patients undergoing/not undergoing ERCP, and those administered conservative or radical treatment, were homogeneous, and just more proportion of patients with recurrence in the group with conservative surgery was observed.
Surgery was partial cystectomy in 15 cases (34.1%) and total cystectomy in 29 (65.9%). Thus, radical surgery was performed in 29 patients (65.9%) and resection of the closed cyst in 23 (79.3%), and the rest were opened (20.7%). In eight cases (18.2%), hepatectomy was performed.
Global postoperative morbidity was 63.6%, and 11 patients (25%) presented major complications (≥ IIIa). The postoperative biliary fistula rate was 36.4% (16 patients). Fistulas were treated conservatively in six cases (37.5%) with the maintenance of drainage, achieving spontaneous closure; in four cases (25%), an ERCP was performed; in three (18.8%), a percutaneous drainage of a bilioma; and in three (18.8%), reintervention was required for bilioperitoneum. Nine patients (20.5%) had residual cavity infection. Compared with a control group without jaundice, these patients presented higher proportions of cystobiliary communication (65.9% vs 19.8%; p < 0.0001) and greater postoperative morbidity (65.9% vs 38.3%; p = 0.001), with higher rates of severe complications (25% vs 9.9%; p = 0.005) and postoperative biliary fistula (36.4% vs 17.7%; p = 0.005).
The median length of hospitalization was 12 days (IQR 8–19). Only one patient died in the postoperative period (on day 85) after a readmission for poor fistula evolution, with bilioperitoneum, sepsis, and finally, exitus.
Five patients presented recurrence during follow-up (11.4%). Prior surgery performed was a hepatectomy in one case and partial pericystectomies in the rest. The average follow-up time was 83.69 months (2.79–162.07).
Table 5 displays the results of the univariate and multivariate analyses of the association between the various variables and postoperative morbidity.
Table 6 displays the results of patients with obstructive jaundice at diagnosis with a control group without jaundice from the overall series.
Discussion
Hydatidosis is an endemic disease in certain areas of the world and is still a major health problem today [3, 13]. The incidence rates at the two units in this study were 27.8 and 30 cases per 100,000 inhabitants. Due to their slow growth, most cysts are asymptomatic and are diagnosed only incidentally. Clinical symptoms, if present, depend on the cyst size and location [3, 5]. Hepatic hydatid cysts may increase gradually in size by about 1 cm in the first 6 months and then by 2–3 cm each year depending on the compressibility of the surrounding structures. The growth of the cysts may have a significant mass effect on adjacent structures, including the biliary tree [2].
Obstructive jaundice is a rare manifestation at the time of diagnosis [5]. In our complete series of hydatid cysts [3], jaundice was present in 12.6% of cases. As the cysts grow, they may increase the intrabiliary pressure, causing bile stasis and eventually producing a fissure through which they communicate with the biliary tree [5, 14]. In most cases, these communications are asymptomatic, although this depends on the size [14, 15]. Smaller communications (which account for 10–37% of cases) present only indirect symptoms such as dilation of the bile ducts or biliary colic, and on many occasions, they are discovered postoperatively in the form of a biliary fistula [6, 9, 14]. On the other hand, larger communications (representing 3–17% of cases) between the cyst wall and the biliary tree are frequently diagnosed in the preoperative period [6, 9]. The contents of the cyst may empty into the biliary tree, causing jaundice, cholangitis, or cyst superinfection with the formation of liver abscess, septicemia, or anaphylaxis [9]. In this study, 65.9% of patients presented cystobiliary communication either prior to or during surgery.
Frank intrabiliary rupture of a hydatid cyst is one of the most frequent complications of this pathology, occurring in 9–42% of cases [6, 9, 15]. It is most common in large cysts (occurring in up to 80% of cysts larger than 7.5 cm), located in the central segments, and in advanced stages of the disease [2], but the frequency of cholangiohydatidosis and secondary cholangitis is unclear [15]. This complication is favored by prior surgery or percutaneous treatment for echinococcosis, with an incidence of up to 50% in these cases [2]. Nine of the patients in our series had a history of previous hydatidosis surgery, and median cyst size was 7 (IQR 5–10) cm.
These complications have been linked to an increase in postoperative morbidity [14, 15]. Both surgical teams in our study have many years of experience with liver hydatidosis and liver resection. In the literature, the postoperative morbidity rate is sometimes underrated, or only severe complications are reported; this would account for the wide range of morbidity published [16]. Furthermore, comparing this group of patients with the control group, we observed a higher rate of postoperative complications, higher severity, and above all, a higher frequency of postoperative biliary fistula.
In series around the world, the postoperative morbidity reported is 10–26%, even exceeding 60% in some studies [17]. In our series, postoperative morbidity was higher than that in our global liver hydatidosis series published elsewhere (63.6% vs 41.4%) [3]. In comparison with our previous study, we observed a greater number of residual cavity infections (20.5% vs 10.4%) and a higher percentage of postoperative biliary fistulas (36.4% vs 19.8%) [3]. In our patients with jaundice at diagnosis, age > 65 years, cyst location, multiple cysts, and cyst size greater than 5 cm showed more postoperative morbidity.
There is no consensus on the value of preoperative ERCP for diagnosing and/or treating suspected communication with the biliary tree [9]. Preoperative ERCP was performed in 25 of the patients recorded in our database (56.8%), and these patients did not present differences with regard to their peers who did not undergo this procedure. It is generally agreed that ERCP should be used in cases of obstructive jaundice with elevated bilirubin or cholestasis or in cases with frank preoperative intrabiliary rupture (either suspected on clinical or biochemical grounds due to cholestasis or demonstrated radiologically in the form of a dilated biliary tree or as evident hydatid elements in bile ducts). In 0–30% of patients undergoing ERCP due to suspected intrabiliary rupture, only bile duct compression by the cyst was observed [9]; similarly, in our series, six of the cases with ERCP did not present intrabiliary communication or occupation of the bile duct by hydatid cyst material. Preoperative ERCP also allows the cleaning of bile duct, avoiding the need for a choledocotomy T tube, and reducing bile duct pressure during the postoperative period [9].
ERCP has a high sensitivity (86–100%) for the diagnosis of intrabiliary rupture, as it directly identifies linear wavy filling defects of laminated hydatid membrane in the common bile duct and the duodenum or protruding from the ampulla of Vater, and can demonstrate the communication with the introduction of a catheter from the biliary ducts directly into the hepatic hydatid cyst [2].
Endoscopic sphincterotomy, extraction by balloon or basket catheter, nasobiliary drainage, and biliary stenting are some of the therapeutic methods that can be performed by ERCP. However, the value of routine use of preoperative ERCP with prophylactic sphincterotomy in patients with a low suspicion of cystobiliary communication is not clearly defined [9]. Of the 25 patients in our database who underwent ERCP, endoscopic sphincterotomy was performed in only 20, and in six of these cases, a plastic prosthesis was inserted.
There are no guidelines for specific management in cases of hydatidosis with jaundice. The information available is based on retrospective studies, case series, or individual clinical cases [6]. Nevertheless, surgery is the treatment of choice for avoiding complications of biliary communication such as cholangitis and/or sepsis [5]. Two factors influence the choice of technique: the anatomical relationship between the cyst and the vasculobiliary structures, and the biliary anatomy. In patients with intrabiliary rupture of the cyst, open cystectomy may be easier to perform in order to identify the communication and its relationship with vascular and biliary hilar structures [6]. There are not any randomized clinical trials comparing radical surgery with other techniques; however, some authors consider that radical surgery, though sometimes more complex, has the advantage of treating both the cyst and the communication, and closing the communication in healthy tissue is considered to reduce morbidity [4, 7]. In certain cases, hepatectomy could be the best technical solution for complete treatment of the cyst and the communication, especially when the right or left intrahepatic bile duct is involved and there is no possibility of reconstruction, or when there is lobular atrophy or cyst recurrence: the postoperative results are good, and morbidity is low [18]. However, especially for uncomplicated cases, parenchyma-sparing methods such as endocystectomy if performing in a standard manner could be favorable due to imposing minor invasive procedure to the liver, minimizing the complication rates [19]. In our series, we found no differences between patients undergoing one or other surgical techniques: surgery was radical in most patients (65.9%) and conservative in the rest. Within the cystectomies, resection was open in 21 patients (47.7%). In all, eight hepatectomies were performed (18.2%).
Postoperative biliary fistula was the most frequent and challenging complication in our series, with an incidence of 36.4%, although this figure is lower than the range described in the literature (50–63%) [9]. Conservative measures can be applied in small fistulas or fistulas with decreasing amounts of drainage, but in persistent fistulas with high output or little change over time, an ERCP is required [9]. It has been reported that a preoperative endoscopic sphincterotomy may lower the incidence of postoperative biliary fistula from 11.1 to 7.6% and may reduce the incidence of infection of the residual cavity in patients with frank intrabiliary rupture [9, 20], but we were unable to confirm this in our study. In our series, six cases (37.5%) were managed conservatively, while four (36.4%) required an ERCP, three (18.8%) percutaneous drainage of a bilioma, and three (18.8%) repeat surgery due to bilioperitoneum.
The limitations of our study include its retrospective design, the small sample size, and the variations in the surgical treatment used. Nor can we draw conclusions about the value of routine preoperative ERCP because of the lack of an established protocol. The use of ERCP seems like an interesting intervention, but its effectiveness needs to be further evaluated in the future to determine its true value.
Conclusions
Patients with liver hydatidosis whose initial symptom is jaundice have a higher postoperative morbidity. Age > 65 years, cyst location, multiple cysts, and cyst size greater than 5 cm could be considered factors that increase morbidity. The main postoperative complication in these cases is biliary fistula despite radical surgery treatment. Preoperative ERCP is not associated with a reduced incidence of postoperative biliary fistula.
Data availability
All data generated or analyzed during this study are included in this published article (and its supplementary information files). I confirmed that the data are real and you can get them by consulting correspondence author.
References
Bhutani N, Kajal P (2018) Hepatic echinococcosis: a review. Ann Med Surg 36:99–105. https://doi.org/10.1016/j.amsu.2018.10.032
Greco S, Cannella R, Giambelluca D, Pecoraro G, Battaglia E, Midiri M, Brancatelli G, Vernuccio F (2019) Complications of hepatic echinococcosis: multimodality imaging approach. Insights Imaging 10:113. https://doi.org/10.1186/s13244-019-0805-8
Jaen-Torrejimeno I, Lopez-Guerra D, Prada-Villaverde A, Blanco-Fernandez G (2019) Pattern of relapse in hepatic hydatidosis: analysis of 238 cases in a single hospital. J Gastrointest Surg 24:361–367. https://doi.org/10.1007/s11605-019-04163-7
Toumi O, Ammar H, Gupta R, Ben Jabra S, Hamida B, Noomen F, Zouari K, Golli M (2018) Management of liver hydatid cyst with cystobiliary communication and acute cholangitis: a 27-year experience. Eur J Trauma Emerg Surg 45:1115–1119. https://doi.org/10.1007/s00068-018-0995-7
Yahya AI, Shwereif HE, Thoboot AS et al (2016) Hepatic hydatid induced obstructive jaundice. Ann Clin Pathol 4:1–5
Ramia JM, De-La-Plaza R, Quiñónes J et al (2014) Frank intrabiliary rupture in liver hydatidosis located in the hilar plate: a surgical challenge. Dig Surg 30:439–443. https://doi.org/10.1159/000356148
Ramia JM, Figueras J, De la Plaza R, García-Parreño J (2012) Cysto-biliary communication in liver hydatidosis. Langenbeck's Arch Surg 397:881–887. https://doi.org/10.1007/s00423-012-0926-8
Velasco-Tirado V, Alonso-Sardón M, Lopez-Bernus A, Romero-Alegría Á, Burguillo FJ, Muro A, Carpio-Pérez A, Muñoz Bellido JL, Pardo-Lledias J, Cordero M, Belhassen-García M (2018) Medical treatment of cystic echinococcosis: systematic review and meta-analysis. BMC Infect Dis 18:306. https://doi.org/10.1186/s12879-018-3201-y
Dolay K, Akbulut S (2014) Role of endoscopic retrograde cholangiopancreatography in the management of hepatic hydatid disease. World J Gastroenterol 20:15253–15261. https://doi.org/10.3748/wjg.v20.i41.15253
Agha RA, Borrelli MR, Farwana R et al (2018) The PROCESS 2018 statement: updating consensus Preferred Reporting Of CasE Series in Surgery (PROCESS) guidelines. Int J Surg (London, England) 60:279–282. https://doi.org/10.1016/j.ijsu.2018.10.031
Clavien PA, Barkun J, de Oliveira ML, Vauthey JN, Dindo D, Schulick RD, de Santibañes E, Pekolj J, Slankamenac K, Bassi C, Graf R, Vonlanthen R, Padbury R, Cameron JL, Makuuchi M (2009) The Clavien-Dindo classification of surgical complications: five-year experience. Ann Surg 250:187–196. https://doi.org/10.1097/SLA.0b013e3181b13ca2
Brooke-Smith M, Figueras J, Ullah S, Rees M, Vauthey JN, Hugh TJ, Garden OJ, Fan ST, Crawford M, Makuuchi M, Yokoyama Y, Büchler M, Weitz J, Padbury R (2015) Prospective evaluation of the International Study Group for Liver Surgery definition of bile leak after a liver resection and the role of routine operative drainage: an international multicentre study. Hpb 17:46–51. https://doi.org/10.1111/hpb.12322
Avgerinos ED, Pavlakis E, Stathoulopoulos A, Manoukas E, Skarpas G, Tsatsoulis P (2006) Clinical presentations and surgical management of liver hydatidosis: our 20 year experience. HPB 8:189–193. https://doi.org/10.1080/13651820500539495
Symeonidis N, Pavlidis T, Baltatzis M, Ballas K, Psarras K, Marakis G, Sakantamis A (2013) Complicated liver echinococcosis: 30 years of experience from an endemic area. Scand J Surg 102:171–177. https://doi.org/10.1177/1457496913491877
Manterola C, Otzen T (2017) Cholangiohydatidosis: an infrequent cause of obstructive jaundice and acute cholangitis. Ann Hepatol 16:436–441. https://doi.org/10.5604/01.3001.0009.8599
De la Plaza LR, Ramia Ángel JM, Bellón JM et al (2018) Clinical validation of the comprehensive complication index as a measure of postoperative morbidity at a surgical department: a prospective study. Ann Surg 268:838–844. https://doi.org/10.1097/SLA.0000000000002839
Baraket O, Moussa M, Ayed K, Kort B, Bouchoucha S (2014) Predictive factors of morbidity after surgical treatment of hydatid cyst of the liver. Arab J Gastroenterol 15:119–122. https://doi.org/10.1016/j.ajg.2014.05.004
Ramia JM, Serrablo A, Serradilla M, Lopez-Marcano A, de la Plaza R, Palomares A (2018) Major hepatectomies in liver cystic echinococcosis: a bi-centric experience. Retrospective cohort study. Int J Surg 54:182–186. https://doi.org/10.1016/j.ijsu.2018.04.049
Al-Saeedi M, Khajeh E, Hoffmann K et al (2019) Standardized endocystectomy technique for surgical treatment of uncomplicated hepatic cystic echinococcosis. PLoS Negl Trop Dis 13:1–14. https://doi.org/10.1371/journal.pntd.0007516
i Gavara CG, López-Andújar R, Ibáñez TB et al (2015) Review of the treatment of liver hydatid cysts. World J Gastroenterol 21:124–131
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
Study conception and design: Gerardo Blanco-Fernández, José Manuel Ramia-Angel, Raquel Latorre-Fragua, Diego López-Guerra, and Isabel Jaén-Torrejimeno.
Acquisition of the data: Raquel Latorre-Fragua, Alba Manuel-Vázquez, Gerardo Blanco-Fernández, Adela Rojas-Holguín, Diego López-Guerra, and Isabel Jaén-Torrejimeno.
Analysis and interpretation of the data: José Manuel Ramia-Angel, Gerardo Blanco-Fernández, Raquel Latorre-Fragua, Diego López-Guerra, and Isabel Jaén-Torrejimeno.
Drafting of the manuscript: Isabel Jaén-Torrejimeno, Raquel Latorre-Fragua, Gerardo Blanco-Fernández, Adela Rojas-Holguín, José Manuel Ramia-Angel, and Diego López-Guerra.
Critical revision of the manuscript: Isabel Jaén-Torrejimeno, Gerardo Blanco-Fernández, Diego López-Guerra, Adela Rojas-Holguín, Alba Manuel-Vázquez, Gerardo Blanco-Fernández, and José Manuel Ramia-Angel.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
The study was approved by the ethical committee of our institution.
Consent to participate
Not applicable
Consent for publication
All authors of the study have consented for publication of this work.
Code availability
IBM SPSS Statistics 21.0 software
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Jaén-Torrejimeno, I., Latorre-Fragua, R., López-Guerra, D. et al. Jaundice as a clinical presentation in liver hydatidosis increases the risk of postoperative biliary fistula. Langenbecks Arch Surg 406, 1139–1147 (2021). https://doi.org/10.1007/s00423-020-02070-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00423-020-02070-z