Abstract
Direct current stimulation (DCS) is a non-invasive approach to stimulate the nervous system that is now considered a powerful tool for treating neurological diseases such as those affecting cognitive or locomotor functions. DCS, as applied clinically today, is an approach built on early uses in antiquity and knowledge gained over time. Its current use makes use of specific devices and takes into account knowledge of the mechanisms by which this approach modulates functioning of the nervous system at the cellular level. Over the last 20 years, although there are few studies, it has been shown that DCS can also modulate the breathing autonomic function. In this narrative review, after briefly providing the historical perspective and describing the principles and the main cellular and molecular effects, we summarize the currently available data regarding the modulation of ventilation, and propose that DCS could be used to treat autonomic or non-autonomic neurological disorders affecting breathing.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Breathing, whose main role is to enable the exchange of gases between the internal and external environments and thus ensure homeostasis through a continuous supply of O2, is an autonomous function. Autonomic functions, which ensure the body’s homeostasis, depend on neurovegetative regulation coordinated with somatic or hormonal processes. So, while the afferent neural control of breathing is associated with the autonomic nervous system, its efferent side is part of the somatic nervous system. The central ventilatory drive relies on two components (Fig. 1). First, an automatic component that depends on a network of neurons located in the brainstem, including rhythm generators, structures involved in “central ventilatory chemoreception” (detection of changes in CO2/H+ and the associated effects on breathing) and structures that integrate the rhythm from generators and changes in CO2/H+ and O2 into a command transmitted to motoneurons innervating ventilatory and upper airway muscles (Fig. 1A–C) [28, 73]. Second, a voluntary or behavioral component which has a suprapontine origin, allowing an adjustment of ventilation during voluntary or behavioral activities and also in certain pathophysiological situations (Fig. 1A, B) [19, 24, 29, 71, 79]. These two components interact to establish a rhythmic command which, in a healthy context, is adapted to the body’s needs and transmitted to motoneurons innervating respiratory muscles (Fig. 1A, B). Some pathologies of neurological (autonomic and/or somatic) or mixed neurological/peripheral origin affecting breathing, such as central hypoventilation, sleep apnea, or spinal cord injury, have few or no available therapies and result in inadequate ventilation [8, 41]. It is in this context that certain data obtained over the past 20 years have demonstrated that direct current stimulation (DCS) applied to the brain or spinal cord can modulate breathing, suggesting its future clinical use in the aforementioned pathophysiological situations.
Functional and anatomical organization of the central ventilatory command. Breathing depends on a central command that comprises two components, an automatic component elaborated in a ponto-medullary ventilatory network, and a voluntary or behavioral component originating from motor cortical areas; this command causes rhythmic contraction of the respiratory muscles of the thoracic cage and upper airways (A, B). The ponto-medullary ventilatory neuronal network has been characterized in detail in rodents in recent years (C). Abbreviations: 7N, facial nucleus; 12N, hypoglossal nucleus; Am, ambiguus nucleus; BötC, Bötzinger complex; c/mNTS, commissural and median parts of the nucleus of the solitary tract; cVRG, caudal ventral respiratory group; DRG, dorsal respiratory group; KF, Kolliker-Füse; lPB, lateral part of the parabrachial nucleus; LC, locus coeruleus; LRt, lateral reticular nucleus; mBP, median part of the parabrachial nucleus; pFRG, parafacial respiratory group; piCo, post-inspiratory complex; preBötC, pre-Bötzinger complex; PRG, pontine respiratory group; ROb, raphe obscurus nucleus; RPa, raphe pallidus nucleus; RTN, retrotrapezoid nucleus; scp, superior cerebellar peduncle; rVRG, rostral ventral respiratory group; vlNTS, ventrolateral subdivision of the nucleus of the solitary tract; VRG, ventral respiratory group. A, adapted from “brain (lateral view)”, “lateral spinal cord”, and “multipolar neuron, motor, curved”; B, adapted from “mouse brain (sagittal cut)” by BioRender.com 2024, retrieved from https://app.biorender.com/biorender-templates
Electrical currents as a therapeutic tool: from the historical use of the torpedo fish to the contemporary use of DCS procedures
Historical perspective
Electrical currents have been used as a therapeutic tool since start of the Common Era (CE). As reported, in 43–48 CE, Scribonius Largus used the electrical properties of the torpedo fish to treat patients suffering from gout and headaches [37]. However, it was not until the eighteenth century that the topic became a subject of study in biology, with the study of torpedo fish by John Walsh in 1773, whose work led to many discoveries by Luigi Galvani and Alessandro Volta [81]. Knowledge of the electrical properties of nerve cells led to the first applications of direct currents (DC) [3, 5]. In the early twentieth century, DCS at the transcranial level (transcranial DCS) started to be used, mainly in Russia, with electrosleep approaches, which consisted of stimulating the brains of patients who had suffered morphine poisoning [65]. In 1977, the US Food and Drug Administration (FDA) classified DCS as a class III device (defined by the FDA as a device for sustaining or supporting life that is high risk for the patient/user and requires premarket approval) used for insomnia, anxiety, and depression [25, 72].
Emergence of new psychiatric drugs in first half of the twentieth century had a negative impact on the interest in DCS up until the 1990s, after which DC regained significant interest as knowledge of the nervous system improved [59]. Discoveries in the late 1990s and throughout the 2000s, such as modulation of cortical excitability with low intensity stimulation through the scalp, were the basis for what is considered to be modern DCS [14, 39, 53].
Basic principles of DCS as used today
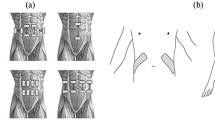
DCS consists of delivering an electrical current from an active (or target) electrode to a reference (or return) electrode. The active electrode must be as close as possible to the region of interest; the reference electrode must be placed appropriately to achieve the desired current flow direction. The positioning of electrodes is a determining factor in obtaining the desired effects, since the most intense stimulation is obtained in tissue that is closest to the active electrode [25]. The electrode through which a positive current enters the body is the anode, and the electrode through which the positive current leaves the body is the cathode. If the active electrode is an anode (positively charged because it is connected to the positive pole of the generator), stimulation is referred to as anodal (Fig. 2); if the active electrode is a cathode (negatively charged because it is connected to the negative pole of the generator), the stimulation is referred to as cathodal (Fig. 2). As specified above, if DCS is applied at the cephalic level, it is called transcranial DCS; if applied to the skin at the level of the spinal cord, it is called transcutaneous spinal DCS (Fig. 2).
Anodal and cathodal DCS and their respective effect on membrane polarization depending on the region of the central nervous system targeted. DCS is a non-invasive nervous system stimulation technique that consists of delivering a weak electrical current. If DCS is applied to the skin at the cephalic level, it is called transcranial DSC or transcranial DCS; if applied to the skin in front of the spinal cord, it is called transcutaneous spinal DCS. Two types of stimulation are possible, anodal or cathodal. The electrode through which a positive current enters the body is an anode (positively charged because connected to the positive pole of the generator) and the electrode through which the positive current leaves the body is a cathode (negatively charged because connected to the negative pole of the generator). Stimulation is named anodal when the anode is the electrode closest to the area of interest; conversely, if the cathode is the electrode closest to the zone of interest, stimulation is named cathodal. The weak current used leads to changes in membrane polarity that can result in either depolarization (and thus a stimulating effect) or hyperpolarization (and thus an inhibiting effect). On the left, configurations giving rise to membrane depolarization, i.e., anodal for the brain (the frontal cortex is the target in the illustrated example) and cathodal for the spinal cord (cervical segments are the target in the illustrated example). On the right, configurations giving rise to membrane hyperpolarization, i.e., cathodal for the brain and anodal for the spinal cord. All cell types present in the central nervous system can be modulated by DCS: neurons, astrocytes, microglia and also cells of the blood–brain barrier or oligodendrocytes, (although little data is yet available for the last two). Adapted from “brain (lateral view)”, “spine(lateral)”, “spinal cord (lateral, no nerve)”, “adult male head (lateral, hairless)”, “transcranial DCS device”, “motor neuron (curved) 3”, “microglia 2”, “astrocyte” by BioRender.com 2024, retrieved from https://app.biorender.com/biorender-templates
With the anatomical differences between the brain or spinal structures and between individuals, it is important to take the electric field induced by transcranial DCS/transcutaneous spinal DCS into account as the waveform direction and current strength can be detected up to a certain distance from the electrodes [35]. The distribution of current densities has been explored using models such as a sphere model for the head or a more realistic model such as that obtained with human magnetic resonance imaging, which takes into account the different tissues crossed by the current [21, 69]. The change in electrode size induced changes in the spatial distribution of current whereas a change in the current results in a change in field amplitude. Highest current densities were always observed under the active or reference electrode, but close densities were obtained in other areas of the brain, implying that observed effects may depend on the invasion of regions of the nervous system other than the primary targets.
Safety for the application of DCS
Numerous studies have characterized the conditions of use of DCS in humans, i.e., limitation of stimulation parameters for safe use and precautions associated with certain pathologies or pharmacological treatments. As reviewed by Bikson and colleagues, use of conventional DCS protocols in human trials (≤ 4 s to 40 min, ≤ 0.1 to 4 mA) has not produced any reports of a serious adverse effect (damage of brain tissue, significant, persistent, or permanent unwanted change in the patient’s body function/structure or quality of life) across over 33,200 sessions and 1000 subjects with repeated sessions [9]. However, there are specific recommendations for certain pathological situations. Notably, even though with intensities ≤ 4 mA transcranial DCS has been to be safe in treatment of strokes, to avoid adverse effects it is recommended to diminish the administration of anti-epileptic drugs prior to transcranial DCS sessions to avoid any risks of modulating the medication action [13].
Neurobiological mechanisms of DCS
DCS leads to non-invasive neuromodulation of central nervous system functioning by immediate effects and long-term synaptic plasticity that follows general mechanisms of long-term potentiation/long-term depression. DCS also appears to be responsible for neuroprotective effects. These different effects are linked to effects on neurons, glial cells, or both.
Anodal or cathodal transcranial DCS, opposite effects on neuronal cell excitability in cortical and spinal cord regions
DCS modulates neuronal cell excitability, i.e., it changes the synaptic strength between neurons but does not modify the nature of neuronal connections [63]. When the electrical field induced by DCS reaches the membrane of one of the compartments of the neuron, it will change the polarization of that portion of the membrane [16, 33, 48, 60, 62] (Fig. 2). At the level of a single neuron, the effect of DCS depends on the distance to the electrodes and the orientation of axonal arborization; these elements underpin the opposing effects of anodal and cathodal DCS between cerebral cortical areas and spinal cord (Fig. 2). Numerous studies carried out at the cortical level have established that anodal transcranial DCS increases neuronal excitability, while cathodal transcranial DCS decreases it [20, 32, 36]. Although far fewer studies have been carried out in the spinal cord than in brain cortical regions, data reported indicate that at the level of spinal cord, the influence of anodal vs cathodal transcutaneous spinal DCS is reversed from that described in the cortex. Facilitation of the corticospinal pathway and somatosensory evoked potentials by peripheral nerve stimulation is under cathodal but not anodal configuration, with cathodal transcutaneous spinal DCS enhancing and anodal transcutaneous spinal DCS reducing the firing rate of spinal neurons by respectively depolarizating or hyperpolarizating effects [1, 15, 74, 82].
Chemical synaptic remodeling
A growing number of animal and human studies in recent years have revealed DCS-induced changes in glutamatergic and GABAergic neurotransmission. Anodal transcranial DCS increases cortical excitability by an increase in synaptic strength involving NMDA or AMPA receptors, e.g., in the hippocampus [2, 66, 75]. The induction of plasticity with anodal transcranial DCS is enhanced in the presence of an NMDA agonist, while it is inhibited in the presence of an NMDA blocker [49]. Taking GABAergic systems as an example, after repeated anodal trans-spinal DCS a reduction of spasticity has been reported concomitant with a downregulation of the cotransporter NKCC1 involved in entry of Cl− into cells and thus in GABA/GABAA [42]. Administration of lorazepam, an allosteric GABAA modulator, enhances and prolongs the effects of anodal transcranial DCS [52]. In addition, monoaminergic systems have also been reported to be affected by DCS, e.g., anodal transcranial DCS stimulations have been shown to modulate dopaminergic systems and enhance serotonin transmission [23, 34, 50, 51].
Neurotrophins and other factors involved in synaptic functioning have been described to be modulated by transcranial DCS. It has been reported that anodal transcranial DCS increases the level of BDNF, expression of cFOS or CREB, and quantity of synapsin and CaMKII in the cortex or hippocampus in rats [31], and improves hearing ability of hearing-impaired rats through denser synapses and better synaptic transmissions related to increased levels of synaptophysin and BDNF [54].
Neurogenesis and neuronal migration
Evidence for cell proliferation has been observed under transcranial DCS applications in rodents: cathodal but not anodal transcranial DCS increased the number of proliferative cells and the number of neural stem cells on the ipsilateral side to the stimulation [67], transcranial DCS promoted cell proliferation and increased the number of neuroblasts on the ipsilateral side exposed to ischemic stroke whether anodal or cathodal [10], and two sessions of five consecutive days of cathodal transcranial DCS increased neurogenesis in both sides of the brain, whereas anodal transcranial DCS increased the number of neuroblasts only on the ipsilateral side to the stimulation [56]. Similar results were obtained with transcutaneous spinal DCS applied to the lumbar spinal cord [70].
Influences of DCS on glial cells
In 2012, the idea emerged that DCS could act not only on neurons but also on glial cells (Fig. 2) [68]. DCS induces a considerable surge of Ca2+ in cortical astrocytes that contributes to synaptic plasticity [45] and induces gene upregulation, which may constitute a glial-mediated plasticity pathway in cultured astrocytes [11]. Few studies have focused on the involvement of oligodendrocytes in DCS-induced plasticity (Fig. 2). However, it seems that cathodal DCS induces migration of oligodendrocyte precursors towards ischemic regions, where they allow remyelination [10], and transcutaneous spinal DCS has been reported to increase the number of oligodendrocyte progenitor cells [70]. Finally, some recent data support a modulation of microglial cells: anodal transcranial DCS increases microglial motility and migration [26] and in a stroke context it was observed that transcranial DCS regulates the phenotype transition of microglia [10]. Since neuroinflammation is negatively correlated to neuroplasticity, microglia constitute an interesting target for the prevention of long-term inflammation following tissue damage [27].
Anatomical and functional basis of central ventilatory control
Breathing depends on a central command that causes rhythmic contraction of the respiratory muscles of the thoracic cage, inspiratory muscles (diaphragm, external intercostal muscles), expiratory muscles (internal and external oblique and internal intercostal muscles), and upper airways muscles (genioglossus; Fig. 1A). Central ventilatory drive comprises two components: an automatic component elaborated in a ponto-medullary ventilatory network, and a voluntary or behavioral component originating from motor cortical areas (Fig. 1A, B) [19, 24, 28, 29, 71, 73]. While the automatic component is transmitted directly to respiratory motoneurons controlling ventilatory muscles, the voluntary or behavioral component can either be transmitted directly to these motoneurons or to the brainstem respiratory network (Fig. 1A). Ventilatory motoneurons innervating muscle of the thoracic cage are located in cervical (phrenic motoneurons), thoracic (internal and external intercostal motoneurons), and lumbar (internal and external abdominal motoneurons) segments of the spinal cord (Fig. 1B); those innervating the tongue genioglossus muscle are located in caudal medulla oblongata (hypoglossal motoneurons, Fig. 1B). The brainstem ventilatory neuronal network has been characterized in detail in rodents in recent years (Fig. 1C), but its precise characterization in humans is not yet fully established. It contains three respiratory rhythm generators in the ventral part of medulla oblongata: the pre-Bötzinger complex, considered as the inexorable generator of inspiration, and the parafacial respiratory group and post-inspiratory complex, both considered as conditional generators for expiration and post-inspiration, respectively. Rhythmic activity emerging from the interaction between the three respiratory generators is integrated in functional groups: the ventral respiratory group (a ventral column comprising the Bötzinger complex in its rostral part, and the reticular formation in alignment with the pre-Bötzinger complex in its caudal part), the dorsal respiratory group (corresponding to the ventrolateral subdivision of the nucleus of the solitary tract), and the pontine respiratory group (corresponding to the median subdivision of the parabrachial and Kolliker-Füse nucleus). Respiratory rhythm generators and/or functional ventral, dorsal, and pontine respiratory groups are permanently subject to chemosensitive inputs from brainstem CO2/H+ sensitive structures (main, retrotrapezoid nucleus and secondary, raphe pallidus and obscurus, locus coeruleus) or from brainstem structures relaying CO2/H+ or O2 chemosensitive information from peripheral (commissural and median subdivisions of the nucleus of the solitary tract) or suprapontine sources (lateral subdivision of the parabrachial nucleus).
Modulation of breathing by DCS
It is possible that breathing is modulated by DCS. This is supported by considerable evidence from the last 20 years that this function depends on a neural network displaying plasticity, whether in the automatic control emerging from the brainstem, in the cortical component of ventilatory control, or in motoneurons innervating the respiratory muscles of the thoracic cage or upper airways [18, 44, 46, 77].
Transcranial DCS application at the cephalic level in healthy subjects
The first studies to report a link between DCS and ventilation date back to the 1960s, when Lippold and colleagues described apnea followed by a decrease in respiratory frequency (fR) in a healthy volunteer subjected to a 3 mA session of cathodal DCS applied to the frontal cortex with an extra-encephalic reference electrode (Table 1) [40, 64]. The authors suggested that these respiratory effects were linked to the passage of current through the brainstem, since the observed effect corresponded to an alteration in respiratory rhythm, an element directly dependent on respiratory rhythm generators or, more broadly, the respiratory neuronal network in the brainstem (Fig. 1).
Although this initial observation could suggest that this approach might lead to potentially dangerous respiratory effects or, on the contrary, that it could provide a new means of non-invasively exploring the respiratory neural network in humans, in the years that followed numerous studies explored the effects of transcranial DCS on various functions, with no mention of the possible effects on ventilatory control. It was not until 2010 that the effect of this type of intervention on ventilatory drive was explored [80], with no observed effect of either anodal or cathodal configurations on fR (with no mention of tidal volume analysis) using a DCS configuration close to that used in the 1960s. In addition to modest differences in electrode positioning, the stimulation parameters chosen differed to those used in the first studies, and corresponded to those used in the majority of studies at the time (Table 1). It is therefore quite plausible that it is the difference in current intensity between these studies, separated by almost 50 years, that is at the root of these divergent effects. In line with the idea that a lack of effect is linked to low current intensity in brainstem regions containing the respiratory neural network, Parazzini and colleagues assessed current density in the brainstem using the setup developed by Vandermeeren and colleagues in 2010 [55, 80]. They used three realistic human models and concluded that current density was low in the medulla oblongata and pons [55].
Shortly after the study of Vandermeeren and collaborators, two other teams explored the effect of transcranial DCS on ventilation or its nerve pathways using “cephalic-cephalic” configurations. One of these studies concluded that transcranial DCS had no effect on fR (again without analysis of tidal volume); the active electrode (anode) was positioned over the C3 position and the reference over the right supraorbital region (Table 1) [61]. The absence of a breathing effect can be interpreted as associated with the absence of electric field propagation to rhythm generators in the brainstem. The second study examined the effect of transcranial DCS applied to the motor cortex on excitability of the diaphragmatic corticospinal pathway [7]. The active electrode was placed over the left diaphragmatic primary cortex (Table 1). The authors observed that in both anodal and cathodal configurations, transcranial DCS led to a decrease in amplitude of right hemidiaphragm motor-evoked potentials in response to transcranial magnetic stimulation (TMS) over the left diaphragmatic primary cortex. These observations may seem surprising as they suggest that both anodal and cathodal transcranial DCS decreased the excitability threshold of the corticodiaphragmatic pathway, whereas multiple data in the literature are in favor of cortical neuronal depolarization in the anodal configuration and moderation of neuronal activity at the cortical level in the cathodal configuration [53]. This discrepancy may depend on several factors, such as the distance between the active and reference electrodes, current density reaching the target tissue, or neuronal circuits involved.
A final study in healthy subjects explored the ability of transcranial DCS to modulate the cortical drive to the chest wall muscles, which are involved in voluntary control of expiration as part of phonation (Table 1) [78]. Activity of the internal intercostal and external oblique expiratory muscles was recorded and used to study intermuscular coherence only during expiration. The authors observed that anodal transcranial DCS applied on the motor cortex induced a significant increase in intermuscular coherence of the expiratory muscles during vital capacity expiration, whereas cathodal transcranial DCS had no effect. This work suggests that transcranial DCS, as applied by these authors, can be used to potentiate synchronized force development of the chest wall muscles during voluntary expiration, a possibility that could be of interest as a complement to conventional rehabilitation protocols in patients with neuromuscular deficits that affect voluntary breathing control.
Transcranial DCS application at the cephalic level in a pathophysiological context
A few years after the studies carried out in healthy subjects, the effects of transcranial DCS on ventilatory control were explored in pathophysiological situations according to two distinct objectives, to induce an improvement in a context of impaired breathing and to look for a possible side effect that could affect breathing.
Exploring the value of transcranial DCS for improving ventilation
To date, few studies have investigated use of transcranial DCS as a therapeutic alternative to improve ventilation in pathological contexts where this function is impaired. The reasons for this are undoubtedly both the difficulty of precisely targeting the caudal part of the brainstem (which contains respiratory network that is the origin of the automatic control of ventilation) and also because the voluntary component of ventilation, which has a suprapontine origin, remains insufficiently explored, even though recent work has highlighted its importance in various pathological contexts [19, 30, 58, 76].
Two studies have explored the benefits of using transcranial DCS in the context of nerve tissue damage in stroke and spinal cord injury (SCI; Table 1). Patients suffering from motor-impairing strokes often have impaired ventilation caused by abnormal posture or, more directly by weakened respiratory muscles, and restoration of more efficient ventilation through exercise is a therapy that has developed over the last decade. In this context, Lee and colleagues investigated the possibility that transcranial DCS targeting the primary motor cortex might improve the effect of exercise training on breathing in patients with stroke [38]. Ventilation was explored by measuring forced vital capacity and forced expiratory volume at 1 s, which were more effectively improved by the combination of anodal transcranial DCS with diaphragmatic breathing exercise than diaphragmatic breathing exercise alone. This work opens up interesting perspectives, but it should be noted that the context in which this improvement was observed lacks precision since neither the intensity and duration of stimulation nor the latency between stimulation and ventilatory measurements is specified. In the context of an SCI—a situation in which, as in the case of a stroke, the nerve tissue is damaged—patients may present ventilatory dysfunctions caused by direct damage to cell bodies of the motoneurons innervating respiratory muscles and/or by damage to descending nerve pathways projecting onto these motoneurons, which carry the respiratory rhythmic motor message. When the lesion is high and affects cervical segments of the spinal cord containing phrenic motoneurons that innervate the diaphragm, breathing insufficiency is significant. De Carvalho and collaborators reported the case of a patient with high-level C5–C7 SCI, tracheostomized for 41 days with difficult weaning due to ineffective cough. In this patient, improved respiratory volume and diaphragmatic activity and successful decannulation were achieved after daily repetition of anodal transcranial DCS applied on the supplementary motor area combined with sensory peripheral electrical stimulation (PES) applied on the abdomen and thorax [17]. It should be noted that prior to joint application of transcranial DCS and sensory PES, the patient was receiving respiratory physiotherapy including myotatic stimuli on the abdominal wall, manual therapy to stimulate synchronization of inspiratory muscles, and facilitation of lower rib cage movements and bronchial hygiene maneuvers. However, these procedures were not sufficient to improve the patient’s cough and enable effective ventilation. This study therefore reports that combined repeated transcranial DCS and sensory PES in a patient suffering from SCI is not damaging and led to an improvement in breathing. However, in the same study, the authors also described an improvement solely through use of repeated sensory PES in another patient with a T5–T8 lesion. As the authors point out, further studies are therefore needed to corroborate the combination of these two approaches to bring real respiratory benefit to patients.
The value of transcranial DCS has also been investigated in patients with resistant hypertension (RHT), to investigate the possible modulation of ventilatory variability (Table 1) [43]. Although the pathophysiology of RHT remains incomplete, it is accepted that autonomic nervous system dysfunction is involved in its initiation and maintenance. Cardiopulmonary exercise testing (CPET) has been used for many years to diagnose and prognose RHT. The authors observed that anodal transcranial DCS applied on the primary motor cortex improved cardiac variability during exercise. This work also showed that transcranial DCS led to an improvement in aerobic capacity without any change in fR or tidal volume. Also, it was shown that transcranial DCS as applied during CPET led to both an improvement in aerobic capacity without any change in fR and tidal volume, and to an attenuation of the exacerbation of the hemodynamic response.
Finally, the therapeutic value of transcranial DCS has also been questioned in the context of COVID-19 in three recent publications [4, 6, 57]. Two of these do not present any results: one describes a clinical study protocol investigating the value of using transcranial DCS to reduce dyspnea in patients with COVID-19 in intensive care units [6], and the other is a literature review focusing on the potential value of transcranial DCS in the management of acute and chronic symptoms of COVID-19 [57]. The third publication presents the results of a randomized clinical trial investigating respiratory rehabilitation using high-definition transcranial DCS (HD-transcranial DCS) in patients with moderate to severe acute respiratory distress syndrome due to COVID-19 (Table 1) [4]. Anodal HD-transcranial DCS targeting the left diaphragmatic motor cortex was applied concurrently with pulmonary rehabilitation. The main result of this study was that the mean number of days without mechanical ventilation during the first 28 days was greater in patients who received HD-transcranial DCS sessions than in sham patients. This finding suggested a clinically meaningful benefit for HD-transcranial DCS in these patients. As discussed by the authors, this benefit could be due to the restoration of correct excitability of the diaphragmatic primary motor cortex and/or a neuroprotective effect in this brain region owing to an enhancement of cerebral blood flow. Each of these could increase the efficiency of the cortical component of ventilation. This work therefore suggests that HD-transcranial DCS coupled with pulmonary rehabilitation can be considered for intensive care unit patients.
A possible ventilatory effect of transcranial DCS used in treatments unrelated to this function
Exploring possible repercussions of a transcranial DCS application for breathing is of major clinical interest, as this autonomic function, along with others, ensures homeostasis. Any modification of the ventilatory drive linked to neuromodulation of the respiratory network located in the brainstem, by secondary diffusion of the electric field applied at the cortical level, is likely to lead to significant disturbances in breathing. However, to our knowledge, this has been evaluated in only one study. Chang and collaborators investigated whether a bi-anodal transcranial DCS configuration over the prefrontal cortex with extra-encephalic reference placement, effective in improving disorders of patients with schizophrenia, could lead to modulation of certain functions, including breathing. Their objective was to determine whether such an effect could constitute a biomarker for a treatment response (Table 1) [12]. With such a configuration, the possibility of stimulation generating a significant current density in the brainstem was conceivable, and with it a modulation of functions controlled by this part of the brain, including breathing. In such a condition, the authors observed no change in fR.
DCS application to the spinal cord in healthy subjects
To evaluate the effect on breathing of DCS at the spinal cord level, we carried out a study in healthy subjects to explore the consequences of applying a single session of transcutaneous spinal DCS at the cervical level on ventilatory drive (Table 1) [47]. Anodal and cathodal transcutaneous spinal DCS were delivered to the cervical region and the effect of these stimulations on diaphragm motor-evoked potentials (DiMEPs; electromyography of the diaphragm with surface electrodes) and spontaneous ventilation (plethysmography) were explored. DiMEPs were triggered by application of a TMS near or above the vertex at the end of expiration, when phrenic motoneurons were not activated through automatic ventilatory drive from the brainstem or were inhibited by brainstem inputs; coil positioning was adjusted for each subject to obtain the largest DiMEPs. Once the location had been determined, TMS stimulation was set to generate a DiMEP at 50% of the observable maximum. It is important to note that evoking DiMEPs at this precise moment in the ventilatory cycle enabled exploration of cortical ventilatory drive without interference from the automatic ventilatory drive emanating from brainstem. This work revealed that both anodal and cathodal cervical transcutaneous spinal DCS increased amplitude of DiMEPs and that only cathodal transcutaneous spinal DCS led to an increase in spontaneous tidal volume with no change in spontaneous fR. These observations led to the hypothesis that the stimulatory effect of cervical transcutaneous spinal DCS depended on an effect at the level of phrenic motoneurons, but not at the level of the brainstem respiratory network. The latter would have led, in parallel to an effect on tidal volume, to a modulation of fR by modification of activity of respiratory rhythm generators. Thus, cervical transcutaneous spinal DCS, by modulating either the level of excitability of motoneurons or neurotransmission at their level, would make them more apt to be stimulated when receiving the descending respiratory command. The observation of such an effect of cathodal transcutaneous spinal DCS both in terms of DiMEPs amplitude and spontaneous tidal volume is in line with data obtained in recent years, which have suggested that this configuration produces stimulatory effects in the spinal cord [1, 15, 82]. Thus, cathodal transcutaneous spinal DCS would be effective in facilitating the passage not only of voluntary ventilatory control originating in the motor cortex but also of automatic ventilatory control emerging from the brainstem. This possibility is of particular interest as it suggests that cervical cathodal transcutaneous spinal DCS could be used to increase ventilation in pathological situations where the ventilatory drive delivered to respiratory muscles is not sufficient. Finally, to conclude on the interest of applying transcutaneous spinal DCS to the cervical region of the spinal cord to modulate breathing, Fernandes and collaborators modelled the electric field generated in our 2014 study [22]. Their work suggests that, in addition to logically affecting C3–C5 segments of the spinal cord, cervical transcutaneous spinal DCS would cause an electric field to diffuse into the brainstem. Such diffusion would be likely to lead to modulation of the brainstem respiratory network. These data suggest a possible effect of cervical transcutaneous spinal DCS not only on tidal volume, as observed in our study [47], but also on fR. Future investigations are needed to explore this possibility under physiological conditions different from those we have already explored in healthy subjects, or under pathophysiological conditions yet to be determined.
Conclusions
DCS is a tool that displays a range of potential uses regarding patient rehabilitation. Studies of the effects of DCS on breathing are scarce but those that are available show promise for future uses of this therapeutic tool. The use of DCS to rehabilitate or stimulate breathing is important in many situations where ventilation is inadequate, and where insufficient therapies are available to clinicians. As it is not easy to explore the effects of DCS on ventilation in patients and healthy subjects, especially as the respiratory neural network responsible for automatic control is located in the caudal part of the brainstem, pilot studies in preclinical models are needed to assess the feasibility of such procedures and to optimize the approach, as well as to decrypt cellular and molecular mechanisms involved in respiratory effects.
References
Ahmed Z (2011) Trans-spinal direct current stimulation modulates motor cortex-induced muscle contraction in mice. J Appl Physiol 110:1414–1424
Akcay G, Aslan M, Kipmen Korgun D, Ceker T, Akan E, Derin N (2024) Effects of transcranial direct current stimulation on the glutamatergic pathway in the male rat hippocampus after experimental focal cerebral ischemia. J Neurosci Res 102:e25247
Aldini G (1804) Essai théorique et expérimental sur le galvanisme, avec une série d’expériences faites devant des commissaires de l’Institut national de France, et en divers amphithéâtres anatomiques de Londres. Fournier Fils, Paris
Andrade SM, de Araujo C, Silvestre M, Tenorio de Franca EE, Bezerra Sales Queiroz MH, de Jesus SK, Lima Holmes Madruga ML, Torres Teixeira Mendes CK, Araujo de Oliveira E, Bezerra JF, Barreto RG, Fernandes A, da Silva SM, Alves de Sousa T, Medeiros de Sousa WC, Patricia da Silva M, Cintra Ribeiro VM, Lucena P, Beltrammi D, Catharino RR, Caparelli-Daquer E, Hampstead BM, Datta A, Teixeira AL, Fernandez-Calvo B, Sato JR, Bikson M (2022) Efficacy and safety of HD-tDCS and respiratory rehabilitation for critically ill patients with COVID-19 The HD-RECOVERY randomized clinical trial. Brain Stimul 15:780–788
Antal A, Alekseichuk I, Bikson M, Brockmoller J, Brunoni AR, Chen R, Cohen LG, Dowthwaite G, Ellrich J, Floel A, Fregni F, George MS, Hamilton R, Haueisen J, Herrmann CS, Hummel FC, Lefaucheur JP, Liebetanz D, Loo CK, McCaig CD, Miniussi C, Miranda PC, Moliadze V, Nitsche MA, Nowak R, Padberg F, Pascual-Leone A, Poppendieck W, Priori A, Rossi S, Rossini PM, Rothwell J, Rueger MA, Ruffini G, Schellhorn K, Siebner HR, Ugawa Y, Wexler A, Ziemann U, Hallett M, Paulus W (2017) Low intensity transcranial electric stimulation: safety, ethical, legal regulatory and application guidelines. Clin Neurophysiol 128:1774–1809
Azabou E, Bao G, Heming N, Bounab R, Moine P, Chevallier S, Chevret S, Resche-Rigon M, Siami S, Sharshar T, Lofaso F, Annane D (2020) Randomized controlled study evaluating efficiency of low intensity transcranial direct current stimulation (tDCS) for dyspnea relief in mechanically ventilated COVID-19 patients in ICU: the tDCS-DYSP-COVID protocol. Front Med (Lausanne) 7:372
Azabou E, Roche N, Sharshar T, Bussel B, Lofaso F, Petitjean M (2013) Transcranial direct-current stimulation reduced the excitability of diaphragmatic corticospinal pathways whatever the polarity used. Respir Physiol Neurobiol 189:183–187
Baughn JM, Matarese CA (2023) Control of breathing and central hypoventilation syndromes. Sleep Med Clin 18:161–171
Bikson M, Grossman P, Thomas C, Zannou AL, Jiang J, Adnan T, Mourdoukoutas AP, Kronberg G, Truong D, Boggio P, Brunoni AR, Charvet L, Fregni F, Fritsch B, Gillick B, Hamilton RH, Hampstead BM, Jankord R, Kirton A, Knotkova H, Liebetanz D, Liu A, Loo C, Nitsche MA, Reis J, Richardson JD, Rotenberg A, Turkeltaub PE, Woods AJ (2016) Safety of transcranial direct current stimulation: evidence based update 2016. Brain Stimul 9:641–661
Braun R, Klein R, Walter HL, Ohren M, Freudenmacher L, Getachew K, Ladwig A, Luelling J, Neumaier B, Endepols H, Graf R, Hoehn M, Fink GR, Schroeter M, Rueger MA (2016) Transcranial direct current stimulation accelerates recovery of function, induces neurogenesis and recruits oligodendrocyte precursors in a rat model of stroke. Exp Neurol 279:127–136
Cancel LM, Silas D, Bikson M, Tarbell JM (2022) Direct current stimulation modulates gene expression in isolated astrocytes with implications for glia-mediated plasticity. Sci Rep 12:17964
Chang CC, Kao YC, Chao CY, Tzeng NS, Chang HA (2021) The effects of Bi-anodal tDCS over the prefrontal cortex regions with extracephalic reference placement on insight levels and cardio-respiratory and autonomic functions in schizophrenia patients and exploratory biomarker analyses for treatment response. Int J Neuropsychopharmacol 24:40–53
Chhatbar PY, Chen R, Deardorff R, Dellenbach B, Kautz SA, George MS, Feng W (2017) Safety and tolerability of transcranial direct current stimulation to stroke patients—a phase I current escalation study. Brain Stimul 10:553–559
Clark VP, Coffman BA, Mayer AR, Weisend MP, Lane TD, Calhoun VD, Raybourn EM, Garcia CM, Wassermann EM (2012) TDCS guided using fMRI significantly accelerates learning to identify concealed objects. Neuroimage 59:117–128
Cogiamanian F, Vergari M, Pulecchi F, Marceglia S, Priori A (2008) Effect of spinal transcutaneous direct current stimulation on somatosensory evoked potentials in humans. Clin Neurophysiol 119:2636–2640
Datta A, Bansal V, Diaz J, Patel J, Reato D, Bikson M (2009) Gyri-precise head model of transcranial direct current stimulation: improved spatial focality using a ring electrode versus conventional rectangular pad. Brain Stimul 2(201–207):207.e201
De Carvalho P, Goulardins JB, de Sousa DMN, Barbosa C, Caetano TCC, Dos Santos LM, Ito CH, Hirota AS, Pereira RPR, Baptista AF, Tanaka C (2021) Noninvasive neuromodulation techniques in difficult tracheostomy weaning of patients with spinal cord injury: report of two cases. Chest 159:e299–e302
Demoule A, Verin E, Montcel ST, Similowski T (2008) Short-term training-dependent plasticity of the corticospinal diaphragm control in normal humans. Respir Physiol Neurobiol 160:172–180
Dubois M, Chenivesse C, Raux M, Morales-Robles A, Nierat MC, Garcia G, Navarro-Sune X, Chavez M, Martinerie J, Similowski T (2016) Neurophysiological evidence for a cortical contribution to the wakefulness-related drive to breathe explaining hypocapnia-resistant ventilation in humans. J Neurosci 36:10673–10682
Farahani F, Kronberg G, FallahRad M, Oviedo HV, Parra LC (2021) Effects of direct current stimulation on synaptic plasticity in a single neuron. Brain Stimul 14:588–597
Faria P, Hallett M, Miranda PC (2011) A finite element analysis of the effect of electrode area and inter-electrode distance on the spatial distribution of the current density in tDCS. J Neural Eng 8:066017
Fernandes SR, Pereira M, Salvador R, Miranda PC, de Carvalho M (2019) Cervical trans-spinal direct current stimulation: a modelling-experimental approach. J Neuroeng Rehabil 16:123
Fukai M, Bunai T, Hirosawa T, Kikuchi M, Ito S, Minabe Y, Ouchi Y (2019) Endogenous dopamine release under transcranial direct-current stimulation governs enhanced attention: a study with positron emission tomography. Transl Psychiatry 9:115
Gandevia SC, Rothwell JC (1987) Activation of the human diaphragm from the motor cortex. J Physiol 384:109–118
Gebodh N, Esmaeilpour Z, Adair D, Chelette K, Dmochowski J, Woods AJ, Kappenman ES, Parra LC, Bikson M (2019) Inherent physiological artifacts in EEG during tDCS. Neuroimage 185:408–424
Gellner AK, Reis J, Fiebich BL, Fritsch B (2021) Electrified microglia: impact of direct current stimulation on diverse properties of the most versatile brain cell. Brain Stimul 14:1248–1258
Golia MT, Poggini S, Alboni S, Garofalo S, Ciano Albanese N, Viglione A, Ajmone-Cat MA, St-Pierre A, Brunello N, Limatola C, Branchi I, Maggi L (2019) Interplay between inflammation and neural plasticity: Both immune activation and suppression impair LTP and BDNF expression. Brain Behav Immun 81:484–494
Guyenet PG, Bayliss DA (2022) Central respiratory chemoreception. Handb Clin Neurol 188:37–72
Horn EM, Waldrop TG (1998) Suprapontine control of respiration. Respir Physiol 114:201–211
Hudson AL, Nierat MC, Raux M, Similowski T (2018) The relationship between respiratory-related premotor potentials and small perturbations in ventilation. Front Physiol 9:621
Kim MS, Koo H, Han SW, Paulus W, Nitsche MA, Kim YH, Yoon JA, Shin YI (2017) Repeated anodal transcranial direct current stimulation induces neural plasticity-associated gene expression in the rat cortex and hippocampus. Restor Neurol Neurosci 35:137–146
Kronberg G, Bridi M, Abel T, Bikson M, Parra LC (2017) Direct current stimulation modulates LTP and LTD: activity dependence and dendritic effects. Brain Stimul 10:51–58
Kunori N, Takashima I (2019) Evaluation of acute anodal direct current stimulation-induced effects on somatosensory-evoked responses in the rat. Brain Res 1720:146318
Kuo MF, Paulus W, Nitsche MA (2008) Boosting focally-induced brain plasticity by dopamine. Cereb Cortex 18:648–51
Laakso I, Tanaka S, Mikkonen M, Koyama S, Sadato N, Hirata A (2016) Electric fields of motor and frontal tDCS in a standard brain space: a computer simulation study. Neuroimage 137:140–151
Lafon B, Rahman A, Bikson M, Parra LC (2017) Direct current stimulation alters neuronal input/output function. Brain Stimul 10:36–45
Largus SRJ (1529) De Compositionibus Medicamentorum [The Compositions of Drugs]. In: Ruello J (ed) De Compositionibus Medicamentorum. Liber Unus. Wechel, Paris
Lee DJ, Lee YS, Kim HJ, Seo TH (2017) The effects of exercise training using transcranial direct current stimulation (tDCS) on breathing in patients with chronic stroke patients. J Phys Ther Sci 29:527–530
Leite J, Carvalho S, Fregni F, Boggio PS, Goncalves OF (2013) The effects of cross-hemispheric dorsolateral prefrontal cortex transcranial direct current stimulation (tDCS) on task switching. Brain Stimul 6:660–667
Lippold OC, Redfearn JW (1964) Mental changes resulting from the passage of small direct currents through the human brain. Br J Psychiatry 110:768–772
Locke KC, Randelman ML, Hoh DJ, Zholudeva LV, Lane MA (2022) Respiratory plasticity following spinal cord injury: perspectives from mouse to man. Neural Regen Res 17:2141–2148
Mekhael W, Begum S, Samaddar S, Hassan M, Toruno P, Ahmed M, Gorin A, Maisano M, Ayad M, Ahmed Z (2019) Repeated anodal trans-spinal direct current stimulation results in long-term reduction of spasticity in mice with spinal cord injury. J Physiol 597:2201–2223
Ministro G, Castano JB, Barboza CA, Moura EG, Ferreira-Melo SE, Mostarda CT, Fattori A, Moreno-Junior H, Rodrigues B (2022) Acute transcranial direct current stimulation (tDCS) improves ventilatory variability and autonomic modulation in resistant hypertensive patients. Respir Physiol Neurobiol 297:103830
Mitchell GS, Baker TL (2022) Respiratory neuroplasticity: mechanisms and translational implications of phrenic motor plasticity. Handb Clin Neurol 188:409–432
Monai H, Ohkura M, Tanaka M, Oe Y, Konno A, Hirai H, Mikoshiba K, Itohara S, Nakai J, Iwai Y, Hirase H (2016) Calcium imaging reveals glial involvement in transcranial direct current stimulation-induced plasticity in mouse brain. Nat Commun 7:11100
Morris KF, Baekey DM, Nuding SC, Dick TE, Shannon R (1985) Invited review: neural network plasticity in respiratory control. J Appl Physiol 94:1242–1252
Nierat MC, Similowski T, Lamy JC (2014) Does trans-spinal direct current stimulation alter phrenic motoneurons and respiratory neuromechanical outputs in humans? A double-blind, sham-controlled, randomized, crossover study. J Neurosci 34:14420–14429
Nitsche MA, Cohen LG, Wassermann EM, Priori A, Lang N, Antal A, Paulus W, Hummel F, Boggio PS, Fregni F, Pascual-Leone A (2008) Transcranial direct current stimulation: state of the art 2008. Brain Stimul 1:206–223
Nitsche MA, Fricke K, Henschke U, Schlitterlau A, Liebetanz D, Lang N, Henning S, Tergau F, Paulus W (2003) Pharmacological modulation of cortical excitability shifts induced by transcranial direct current stimulation in humans. J Physiol 553:293–301
Nitsche MA, Grundey J, Liebetanz D, Lang N, Tergau F, Paulus W (2004) Catecholaminergic consolidation of motor cortical neuroplasticity in humans. Cereb Cortex 14:1240–1245
Nitsche MA, Kuo MF, Karrasch R, Wachter B, Liebetanz D, Paulus W (2009) Serotonin affects transcranial direct current-induced neuroplasticity in humans. Biol Psychiatry 66:503–508
Nitsche MA, Liebetanz D, Schlitterlau A, Henschke U, Fricke K, Frommann K, Lang N, Henning S, Paulus W, Tergau F (2004) GABAergic modulation of DC stimulation-induced motor cortex excitability shifts in humans. Eur J Neurosci 19:2720–2726
Nitsche MA, Paulus W (2000) Excitability changes induced in the human motor cortex by weak transcranial direct current stimulation. J Physiol 527(Pt 3):633–639
Paciello F, Podda MV, Rolesi R, Cocco S, Petrosini L, Troiani D, Fetoni AR, Paludetti G, Grassi C (2018) Anodal transcranial direct current stimulation affects auditory cortex plasticity in normal-hearing and noise-exposed rats. Brain Stimul 11:1008–1023
Parazzini M, Rossi E, Rossi L, Priori A, Ravazzani P (2013) Evaluation of the current density in the brainstem during transcranial direct current stimulation with extra-cephalic reference electrode. Clin Neurophysiol 124:1039–1040
Pikhovych A, Stolberg NP, Jessica Flitsch L, Walter HL, Graf R, Fink GR, Schroeter M, Rueger MA (2016) Transcranial direct current stimulation modulates neurogenesis and microglia activation in the mouse brain. Stem Cells Int 2016:2715196
Pilloni G, Bikson M, Badran BW, George MS, Kautz SA, Okano AH, Baptista AF, Charvet LE (2020) Update on the use of transcranial electrical brain stimulation to manage acute and chronic COVID-19 symptoms. Front Hum Neurosci 14:595567
Pouget P, Allard E, Poitou T, Raux M, Wattiez N, Similowski T (2018) Slower is higher: threshold modulation of cortical activity in voluntary control of breathing initiation. Front Neurosci 12:663
Priori A, Berardelli A, Rona S, Accornero N, Manfredi M (1998) Polarization of the human motor cortex through the scalp. Neuroreport 9:2257–60
Rahman A, Reato D, Arlotti M, Gasca F, Datta A, Parra LC, Bikson M (2013) Cellular effects of acute direct current stimulation: somatic and synaptic terminal effects. J Physiol 591:2563–2578
Raimundo RJS, Uribe CE, Brasil-Neto JP (2012) Lack of clinically detectable acute changes on autonomic or thermoregulatory functions in healthy subjects after transcranial direct current stimulation (tDCS). Brain Stimul 5:196–200
Reato D, Rahman A, Bikson M, Parra LC (2010) Low-intensity electrical stimulation affects network dynamics by modulating population rate and spike timing. J Neurosci 30:15067–15079
Reato D, Rahman A, Bikson M, Parra LC (2013) Effects of weak transcranial alternating current stimulation on brain activity-a review of known mechanisms from animal studies. Front Hum Neurosci 7:687
Redfearn JW, Lippold OC, Costain R (1964) A preliminary account of the clinical effects of polarizing the brain in certain psychiatric disorders. Br J Psychiatry 110:773–785
Robinovitch LG (1911) Electric analgesia, and electric resuscitation after heart failure under chloroform or electrocution. JAMA 56:478–481
Rohan JG, Carhuatanta KA, McInturf SM, Miklasevich MK, Jankord R (2015) Modulating hippocampal plasticity with in vivo brain stimulation. J Neurosci 35:12824–12832
Rueger MA, Keuters MH, Walberer M, Braun R, Klein R, Sparing R, Fink GR, Graf R, Schroeter M (2012) Multi-session transcranial direct current stimulation (tDCS) elicits inflammatory and regenerative processes in the rat brain. PLoS One 7:e43776
Ruohonen J, Karhu J (2012) tDCS possibly stimulates glial cells. Clin Neurophysiol 123:2006–2009
Sadleir RJ, Vannorsdall TD, Schretlen DJ, Gordon B (2010) Transcranial direct current stimulation (tDCS) in a realistic head model. Neuroimage 51:1310–1318
Samaddar S, Vazquez K, Ponkia D, Toruno P, Sahbani K, Begum S, Abouelela A, Mekhael W (1985) Transspinal direct current stimulation modulates migration and proliferation of adult newly born spinal cells in mice. J Appl Physiol 122:339–353
Schottelkotte KM, Crone SA (2022) Forebrain control of breathing: anatomy and potential functions. Front Neurol 13:1041887
Smith B (2006) Cranial electrotherapy stimulation: its first fifty years, plus three: a monograph. Taye, Mustang
Smith JC (2022) Respiratory rhythm and pattern generation: brainstem cellular and circuit mechanisms. Handb Clin Neurol 188:1–35
Song W, Martin JH (2017) Spinal cord direct current stimulation differentially modulates neuronal activity in the dorsal and ventral spinal cord. J Neurophysiol 117:1143–1155
Stafford J, Brownlow ML, Qualley A, Jankord R (2018) AMPA receptor translocation and phosphorylation are induced by transcranial direct current stimulation in rats. Neurobiol Learn Mem 150:36–41
Taytard J, Nierat MC, Gand C, Lavault S, Morelot-Panzini C, Patout M, Serresse L, Wattiez N, Bodineau L, Straus C, Similowski T (2023) Short-term cognitive loading deteriorates breathing pattern and gas exchange in adult patients with congenital central hypoventilation syndrome. ERJ Open Res. https://doi.org/10.1183/23120541.00408-2022
Tenorio-Lopes L, Kinkead R (2021) Sex-specific effects of stress on respiratory control: plasticity, adaptation, and dysfunction. Compr Physiol 11:2097–2134
Tomczak CR, Greidanus KR, Boliek CA (2013) Modulation of chest wall intermuscular coherence: effects of lung volume excursion and transcranial direct current stimulation. J Neurophysiol 110:680–687
Tremoureux L, Raux M, Hudson AL, Ranohavimparany A, Straus C, Similowski T (2014) Does the supplementary motor area keep patients with Ondine’s curse syndrome breathing while awake? PLoS One 9:e84534
Vandermeeren Y, Jamart J, Ossemann M (2010) Effect of tDCS with an extracephalic reference electrode on cardio-respiratory and autonomic functions. BMC Neurosci 11:38
Walsh JSS (1773) Of the electric property of the torpedo. In a Letter from John Walsh, Esq; F. R. S. to Benjamin Franklin, Esq; LL.D., F. R. S. In: Proceedings of the Royal Society of London, Philosophical Transactions of the Royal Society 63:461–480
Yamaguchi T, Moriya K, Tanabe S, Kondo K, Otaka Y, Tanaka S (2020) Transcranial direct-current stimulation combined with attention increases cortical excitability and improves motor learning in healthy volunteers. J Neuroeng Rehabil 17:23
Acknowledgements
Andrew Lane (Lane Medical Writing) edited the manuscript for English language and grammar.
Funding
The work was funded by Inserm, Sorbonne University and Fondation du Souffle (grant to LB and FC).
Author information
Authors and Affiliations
Contributions
All authors critically reviewed and approved the manuscript and are accountable its accuracy and integrity. Additionally, RDC contributed substantially to the drafting of the manuscript; MCN performed experiments, analyzed the data and discussed the results and their significance; AF contributed substantially to the synthesis of part of the literature; TS designed experiments and discussed the results and their significance; FC obtained funding, contributed substantially to the synthesis of part of the literature and wrote the manuscript; LB obtained funding, contributed substantially to the synthesis of part of the literature, constructed the figures and wrote the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no financial or proprietary interests in any material discussed in this article.
Ethical approval
The review of the literature and the interpretations we suggest have not involved any new human or animal experiments. Ethical considerations therefore apply to the various experimental studies mentioned in this literature review; they do not apply to this literature review.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Delucenay-Clarke, R., Niérat, MC., Frugière, A. et al. Direct current stimulation as a non-invasive therapeutic alternative for treating autonomic or non-autonomic neurological disorders affecting breathing. Clin Auton Res 34, 395–411 (2024). https://doi.org/10.1007/s10286-024-01055-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10286-024-01055-y