Abstract
The aim of this trial was to analyze the effect of implant surface decontamination procedures combined with reconstructive surgical treatment (RST) of peri-implantitis on gene expression levels of selected biomarkers in peri-implant crevicular fluid (PICF). Forty patients diagnosed with peri-implantitis were treated with RST + decontamination of the implant surface using sterile saline and ozone therapy (ozone group) or sterile saline alone (control group). The gene expression levels of interleukin (IL)-6, IL-8, IL-17, vascular endothelial growth factor (VEGF), sclerostin (SOST) and osteoprotegerin (OPG) were evaluated by qPCR analysis at baseline and 6-month follow-up. Changes in cytokine mRNA expression levels were analyzed and compared with clinical/radiographic parameters. Both decontamination methods lead to the downregulations of the selected gene expressions. Ozone group showed significantly higher clinical attachment level (CAL) and radiographic defect fill (DF) values at 6 months compared to the control group (p = 0.026 and p = 0.011). The downregulation of SOST levels was significantly associated with probing depth reduction and radiographic DF (p < 0.05). Implant surface decontamination procedures applied with the RST contribute to a notable reduction in immuno-inflammatory response. The additional use of ozone therapy could have favorable effects in anti-infective regimens of peri-implantitis therapy. SOST, which was found to have significant relationship with both clinical and radiographic outcomes, could be a valuable indicator for the progression of peri-implantitis and may aid the development of new therapeutic strategies for bone gain in the RST of peri-implantitis.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Peri-implantitis is a plaque-associated, destructive pathological disease in which microorganisms and the host immune response play a crucial role in the etiopathological mechanisms that lead to peri-implant soft tissue inflammation and a subsequent progressive supporting bone loss, moreover a complete loss of osseointegration [1, 2]. Peri-implantitis has been identified as a major biological complication of dental implants and the main reason for the failure of implant therapy [3, 4]. A recent data presented a peri-implantitis prevalence between 0.2 and 63% at implant level, and between 1 and 46% at patient level [4]. Considering its high prevalence rates, early diagnosis and appropriate treatment are critical for avoiding the progression of peri-implantitis lesions.
Anti-infective treatment strategies have been reported as successful modalities in decreasing inflammation of soft tissues and suppressing peri-implant disease progression [2]. Different mechanical methods such as curettes, polishing brushes, ultrasonic debridement, air-abrasive devices, and laser decontamination [5, 6] and their combination with chemical protocol treatments including local application of antibiotics and/or antiseptics [7, 8] have been introduced as potentially effective procedures to decrease the microbial load from contaminated implant surfaces. However, non-surgical therapy for peri-implantitis in combination with these procedures has been reported to be inadequate for disease resolution and the requirement to reconstructive approach for peri-implant bone defects. Therefore, for decontamination of an exposed implant surface and elimination or reconstruction of peri-implant bone defects, surgical management should be considered [9,10,11]. Recently, three-year results of a randomized clinical trial indicated that implant surface anti-infective surgical protocol yielded an improved peri-implant soft tissue health and stable peri-implant marginal bone level in severe peri-implantitis cases [12]. Furthermore, that study also revealed a notable reduction in terms of the total viable count (TVC) of bacteria at 1 year postoperatively [13]. Nevertheless, because of the imbalance between the host response and bacterial colonization at the soft tissue-implant interface, the immune modulation effects of the adjunctive therapies in peri-implantitis treatment strategies should also be considered [14].
Ozone therapy (O3), which has a potential as an adjunctive approach for inflammatory diseases like peri-implantitis, influences the cellular and humoral immune system by stimulating proliferation of immunocompetent cells and synthesis of immunoglobulins and biologically active substances including interleukins, leukotrienes, and prostaglandins [15, 16]. Ozone has also been suggested to activate the function of macrophages and to increase the sensitivity of microorganisms to phagocytosis [16]. Macrophage-derived mediators such as tumor necrosis factor α (TNF-α), interleukin (IL)-1 β, IL-6, and IL-8 contribute to the biological response to ozone which lead to the inflammatory response [17]. Ozone applications have also been reported to modulate implant surface obtaining a superhydrophilic surface which can improve interactions between implants and the biological environment [15, 18]. Surface photofunctionalization using gaseous ozone has been demonstrated to increase proliferation and differentiation of mesenchymal stem cells, and to mitigate proinflammatory cytokine including TNF-α and IL-6 production without altering titanium surface topography [18].
The clinical and radiographic assessments including bleeding on probing (BOP) and suppuration along with a loss of the supporting tissues (e.g., increases in probing pocket depths (PPDs), progressive radiographic bone loss) are commonly recommended for diagnosis of peri-implantitis [19]. Moreover, recent studies have concentrated on elucidating the genetic basis and identification of molecular biomarkers for prediction of peri-implantitis occurrence [20]. Biomarker analysis in peri-implant crevicular fluid (PICF) might serve as a prognostic and diagnostic tool for the onset and activity of peri-implantitis and detect distinct treatment approaches for target individuals [21]. It has been pointed out that increased levels of proinflammatory cytokine in PICF such as IL-1 β [22,23,24], IL-6 [24, 25], IL-17 [25], chemokines such as IL-8 [26, 27], angiogenic factors such as vascular endothelial growth factor (VEGF) [14, 27] and osteoclastogenesis-related cytokines such as osteoprotegerin (OPG) [8, 28] and sclerostin (SOST) [28] are associated with pathogenesis of peri-implantitis. It was also reported that peri-implantitis treatments could reduce these biomarkers in PICF [29, 30]. However, information about the changes in cytokine profiles before and after the treatment is scarcely available in the literature. Moreover, the effects of peri-implantitis treatment on their expression of genetic profiles have not been thoroughly analyzed in PICF. Therefore, the objectives of the current study were to analyze the effect of the use of different implant surface decontamination procedures combined with reconstructive surgical treatment (RST) of peri-implantitis which leads to downregulation of the expression of the selected inflammatory cytokines, chemokines and alveolar bone turnover/resorption markers (IL-6, IL-8, IL-17, VEGF, OPG and SOST) in PICF and to establish a correlation between the changes in the levels of these biomarkers and the clinical and radiographic data acquired following surgical therapies.
Material and methods
Subjects and study design
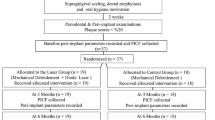
The prospective, parallel, randomized and test-control study of 6 months evaluated the efficacy of adjunctive ozone treatment on the change of mRNA expression levels of selected biomarkers after the RST of peri-implantitis. The study protocols were approved by the research ethics review committee of Gazi University, School of Medicine, Ankara, Turkey (25901600-2858) and conducted in accordance with the ethical principles, including Declaration of Helsinki of 1975, as revised in 2013. The trial was registered at ClinicalTrials.gov as NCT03018795. Prior to participation in the study, written informed consents were obtained from all the patients. All participants were selected from the patients who had previously been rehabilitated with dental implants and diagnosed with peri-implantitis and were required to be scheduled for reconstructive treatment between November 2014 and December 2017. The study population consisted of 40 patients who had at least one implant diagnosed with peri-implantitis, which was defined as increased probing depth (PD) compared to previous examinations with bleeding and/or suppuration on gentle probing and radiographic evidence of peri-implant bone loss beyond crestal bone-level changes resulting from initial bone remodeling [31] with a crater-like pattern (class Ib, class Ic, and class Ie) [32].
Patients having moderate or severe chronic periodontitis (i.e., bleeding and/or suppuration in more than 30% of the subgingival sites with PD ≥ 4 mm) and the patients with uncontrolled medical conditions such as diabetes mellitus (hemoglobin A1c ≥ 7.0), and antibiotic administration within 3 months prior to the surgical procedure were excluded.
The peri-implantitis defects were categorized into two treatment groups according to the implant surface decontamination procedure: ozone group received submucosal mechanical debridement using titanium curettes combined with saline irrigation + additional ozone therapy as a decontamination procedure; while, control group received submucosal mechanical debridement by using titanium curettes with saline irrigation alone. A computer-generated randomization table was used to randomize the treatment groups by a biostatistician (B.B). Allocation concealment was achieved by a sealed, coded opaque envelope containing the treatment procedure. Each envelope was assigned a number identifying an implant to receive the respective treatment. An examiner (B.U.) who was not involved in the surgical procedures and clinical examinations opened the envelopes and performed the adjunctive therapy.
In both ozone and control groups, submucosal mechanical debridement was performed followed by pocket irrigation with saline solution for 3 min at the affected peri-implantitis sites. In the ozone group, adjunctive gaseous ozone was applied following saline irrigation. Ozone was administered through a connected hand-piece using an ozone generator (DentaTec Dental AS, Hov, Norway) with 80% oxygen for 30 s as recommended by the instructions of the ozone generator manufacturer. It was delivered at 6 points circumferentially (mesiobuccal, midbuccal, distobuccal, mesiolingual, midlingual, and distolingual) at the time of operation and 3rd and 5th days after the operation. The patients allocated to the control group received sham ozone administration without starting the ozone generator.
Before the surgery, venous blood was drawn into 4 sterile 10-ml tubes without anticoagulant and centrifuged with a CGF centrifuge machine (Medifuge, Silfradentsr, Santa Sofia, Italy) at 2700 rpm for 2 min, at 2400 rpm for 4 min, at 2700 rpm for 4 min and at 3000 rpm for 3 min. All the surgical procedures were performed by the same operator (S.C.I). After local anesthesia (Ultracain DS Forte, Sanofi-Aventis, Frankfurt, Germany), a full-thickness mucoperiosteal flap preparation was performed towards the vestibular and the palatal sides of the implants. After flap elevation, granulation tissue was removed from the peri-implant defect and debridement of implant surface was done using a titanium curette (ImplaMate, Nordent Manufacturing Inc, Elk Grove Village, IL, USA). Implant surfaces were decontaminated according to the protocols mentioned above for the treatment groups. In both groups, the intraosseous component of the defects was filled with a bovine-derived bone xenograft (Bio-Oss® granules, 0.25–1 mm, Geistlich Biomaterials, Wolhusen, Switzerland) moistened in CGF liquid and mixed with small pieces of CGF. Two of CGF membranes were used to cover the entire of the defects and was adapted above the bone graft. The flaps were positioned coronally and were sutured with polyamide 5–0 sutures (Dogsan, Trabzon, Turkey) providing the primary wound closure.
Two weeks after the operations, the sutures were removed. During the postoperative period, the patients were received antibiotics including 500 mg of amoxicillin (Largopen; Bilim, İstanbul, Turkey) and 500 mg of metronidazole (Flagyl; Sanofi Aventis Pharm Inc Co, Istanbul, Turkey) 3 times a day for 7 days.
A single examiner (F.S.) who blinded to the treatment assignment was responsible for clinical registrations. All the clinical measurements were recorded after the supra-constructions were removed before the surgery (baseline) and at 6 months postoperatively, using a periodontal probe (Nordent, Manufacturing Inc., IL, USA). Clinical measurements that included plaque index (PI) [33], gingival index (GI) [34], BOP (presence/absence of bleeding 30 s after gentle probing), and PD (the distance from the mucosal margin to the bottom of the peri-implant sulcus) were performed at four sites per implant (i.e., mesial, buccal, distal, and, palatal/lingual). Clinical attachment level (CAL) was evaluated with respect to a fixed point on the neck of the implants and was measured as PD + mucosal recession.
The assessments of periapical radiographs were performed by an expert investigator according to the protocol reported by Isler et al. [35]. The periapical radiographs with the long-cone paralleling technique and an individualized film holder (Rinn bite film holder, Dentsply, York, PA) was performed at baseline and 6-month follow-up. The film holder was attached at the natural dentition with occlusal fixation using an impression material. The digitized images of the radiographs were examined using a computer software. Measurements, which was calibrated using implant length and width, were assessed between the first bone-to-implant contact and a well-defined reference point at the coronal part of the implant body. The measurement of vertical defect depth (VDD) was performed at both mesial and distal aspects of the affected implants and obtained by taking the average of those measurements. The defect fill (DF) was evaluated comparing the VDD measurements at baseline and the 6 months postoperatively.
Reproducibility analysis of the both clinical and radiographic evaluation method was conducted by selecting five implants, which were chosen using a random number table for the second analysis. The second measurements were performed more than 2 weeks after the first measurements. When comparing the two measurements, it was aimed to obtain an intra-examiner agreement of 90%.
PICF collection
PICF sampling was conducted by the examiner who performed the clinical examination. The PICF sample collection was performed before surgery and 6 months postoperatively. After the supramucosal oral biofilm and isolation were carefully removed with cotton wool rolls, two standard paper strips (Periopaper, Oraflow Inc, New York, NY, USA) were inserted approximately 3 mm into the peri-implant sulcus of the affected implants and were left for 30 s. The second collection was performed from the same site after 1 min. The paper strips were immediately transferred to different 2-ml screw-capped tubes containing the RNAlater® (Sigma-Aldrich, Germany) and were stored at − 80 °C until the RNA extraction stage.
mRNA extraction of the samples
Expression of selected biomarkers was analyzed by an oral microbiologist (G.A) who was blinded to the identity of the samples. The mRNA levels of IL-6, IL-8, IL-17, VEGF, OPG and SOST were analyzed. Total RNA was extracted from respective PICF samples using a TriPure® isolation kit (Roche Diagnostics Co., Indianapolis, USA) and the following protocol conducted as recommended by the manufacturer. RNA samples was suspended in diethylpyrocarbonate-treated water, DNAse-treated (Turbo DNA-free; Ambion Inc.), and stored at − 80 °C until use. The concentration of RNA/μl in the samples was determined by the microvolume spectrophotometer (Nanodrop 1000; Nanodrop Technologies LLC, Wilmington, NC, USA). For cDNA synthesis, 1 μg of total RNA, oligo(dT), nuclease-free water and a first-strand cDNA synthesis kit containing reverse transcriptase (Roche Diagnostics Co., Indianapolis, USA) as described by the manufacturer were used. The housekeeping gene of beta-actin (β-actin) was used as the control by performing both in-house PCR and qPCR methods. 2X SYBR Green dye with (10 pmol/μl) forward (F1) primer (0.5 pmol/μl) reverse (R1) primer (0.5 pmol/μl), deionized water (4 μl) and cDNA (5 μl) was added and the final volume was adjusted to 20 μl.
Real-time PCR assay
SYBR-green fluorescence quantification system was used to evaluate mRNA expressions corresponding to the B actin, IL-6, IL-8 IL-17, VEGF, OPG and SOST sequences for qPCR analysis. The primers were designed using the LightCycler (Roche Diagnostics GmbH, Mannheim, Germany) and CLC probe design Softwares (Qiagen Bioinformatics, Hilden, Germany). The primer sequences, the amplification profiles, and amplicon length are presented in Table 1. qPCR was carried out using the LightCycler System (Roche Diagnostics GmbH, Mannheim, Germany) as recommended by the manufacturer (FastStart DNA MasterPLUS SYBR Green; Roche Diagnostics Co., Indianapolis, IN, USA). The calculations were done according to the control gene expressions of the housekeeping gene of β-actin. Quantitation was performed using LightCycler® Nano Software 1.1 (Roche Diagnostics GmbH, Germany), and the data of the relative expressions of the selected genes in the study were computed according to the \(2^{{ - \Delta \Delta C_{{\text{t}}} }}\) method [36].
Statistical methods
The sample size was calculated based on our pilot study conducted using the current study design that demonstrated the mean CAL values at 6 months as 3.53 ± 1.79 mm and 2.11 ± 1.14 mm for the ozone and control groups, respectively. It was estimated that 19 patients would be enough per group to achieve a power of 0.8 with a significance level of 0.05 using Student’s t-test.
The quantitative variables were expressed as mean ± sd and median (min–max), while the categorical variables were shown as numbers (percentage) in the study. The Kolmogorov–Smirnov test was used to evaluate whether the compatibility of data was distributed normally. For the comparison of the quantitative variables between the groups, Student’s t-test was performed if the normal distribution assumption was met; if not, Mann–Whitney U test was used.
The Paired t test or Wilcoxon Sign Rank test was used where they were indicated for the relationship between two quantitative dependent variables within the groups. Associations between data were assessed using a Spearman rank-order correlation analysis because normal distribution assumptions were not provided. Potential effects of patient- and implant-related variables (gender, age, history of periodontitis, implant location, implant surface and implant function time) on treatment outcome were further explored using linear regression analysis. The cutoff for statistical significance was p ≤ 0.05 for each test.
Results
The patients’ demographic data and implant characteristics
All patients (22 women, 18 men; mean age: 55.08 ± 10.71 years) attended the follow-up study periods without missing any appointments, and completed the study successfully. No adverse effects related to ozone application were reported. The information about the patients’ demographic data and implant characteristics of the study groups are shown in Table 2. No significant differences were observed between the groups regarding these variables.
Clinical and radiographic assessments
Baseline and 6-month follow-up clinical and radiographic assessments are presented in Table 3. In both groups, all parameters exhibited statistically significant reductions between the baseline and 6 months postoperatively (p < 0.001). No significant difference was observed between the compared groups at the baseline for all parameters (p > 0.05). At the 6-month follow-up, both groups demonstrated comparable mean values with respect to PI, GI, PD, BOP and VDD values; while, a statistically significant difference was noticed between the groups only for the mean CAL values in favor of the ozone group (p = 0.026). Intergroup analysis failed to demonstrate the differences in clinical parameters between the baseline and 6 months postoperatively (p < 0.05). However, the radiographic evidence of DF at 6 months was significantly higher in the ozone group than in the control group (p = 0.011).
Effects of the implant surface decontamination methods on mRNA expression levels in PICF
Figure 1 presents the expressions of the gene markers in treatment groups by displaying the fold change of 6 months compared to baseline. Statistical analysis failed to reveal any significant difference between the ozone and control groups for all the selected mRNA expressions (p > 0.05). From the baseline to 6 months postoperatively, the fold downregulation was 7.96 ± 7.62 and 5.98 ± 6.83 for the IL-6 levels, 2.70 ± 3.91 and 2.29 ± 2.86 for the IL-8 levels, 3.63 ± 3.21 and 1.74 ± 3.56 for the IL-17 levels, 5.85 ± 7.00 and 5.14 ± 5.69 for the VEGF levels, 1.20 ± 1.78 and 0.90 ± 2.66 for the OPG levels, and 3.87 ± 3.29 and 3.15 ± 2.94 for the SOST levels in the ozone and control groups, respectively (Fig. 1).
Effects of peri-implantitis treatment on the fold changes of selected gene expressions in the ozone and control group. Data were expressed as the mean ± standard deviation. p < 0.05 considered statistically significant, Student’s t-test and Mann–Whitney U test. OPG osteoprotegerin, VEGF vascular endothelial growth factor, SOST sclerostin, IL-6 interleukin-6, IL-8 interleukin-8, IL-17 interleukin-17
Correlations between the fold changes of selected gene expressions and the change of clinical and radiographic data irrespective of treatment methods.
The significant positive correlations were found between the downregulation of IL-6 and OPG gene expressions (r = 0.534, p = 0.007) and between the downregulation of IL-6 and VEGF gene expressions at 6 months (r = 0.561, p = 0.004). Similarly, the downregulation of the IL-8 level was significantly correlated with the downregulation of SOST levels at 6 months (r = 0.654, p = 0.001). Furthermore, the reduced expression of IL-8 and SOST mRNA levels was positively correlated with PD reduction (r = 0.375, p = 0.041; r = 0.485, p = 0.016). On the other hand, a significant negative correlation was observed between the downregulation of SOST levels and the mean DF values (r = − 0.412, p = 0.045) (Table 4).
Assessment of variables affecting the primary outcome
Univariate linear regression analysis was used to analyze the patient and implant-related variables independently associated with the primary outcome. The independent variables were examined included decontamination methods, patient demographics, and implant characteristics. The results of univariate linear regression analysis are shown in Table 5. Implant function time was the only variable which was found to have a statistically significant relationship with the treatment outcome [odds ratio (OR) 1.390, 95% confidence interval 0.676–2.103, p = 0.001].
Discussion
Anti-infective regimens combined with non-surgical or surgical therapies of peri-implantitis have been proposed to assure a predictable treatment outcome by disrupting bacterial adhesion and colonization to implant surface [37, 38]. Nevertheless, the effects of surface decontamination methods on host immune response have not yet been comprehensively evaluated in peri-implantitis treatment. The present randomized controlled trial indicated that both decontamination methods improved clinical and radiographic outcomes and lead the downregulations of the selected gene expressions at 6-month follow-up; whereas, no significant differences were identified between the treatment methods except for the mean CAL and DF values at 6 months in favor of ozone therapy.
The efficacy of therapeutic approaches could be revealed by elucidation of the interactions of inflammatory and alveolar bone turnover/resorption markers in immune-regulatory mechanisms and their roles in disease progression processes [14, 29, 30]. The process of peri-implant bone regeneration is regulated by a sequence of complex and well-organized cellular and molecular signaling networks in which a variety of factors, such as hormones, cytokines and growth factors have a role [39]. Taking into account the present study findings, bone reconstruction treatment modalities of peri-implant defects presented reduced mRNA levels for all selected biomarkers at the end of the study. The present findings on the changes in biomarkers levels are similar to the results obtained from a previous study reported by Wohlfahrt et al. [29], which indicated that the RST of peri-implantitis treatment induced some reduction of proinflammatory and bone markers in PICF. On the other hand, different decontamination methods combined with regenerative or non-regenerative peri-implantitis treatment have been investigated by detecting microbiological and immunological profiles [30, 40]. In the present study, none of the decontamination procedures showed superiority to each other regarding changes in biomarker levels at 6-month follow-up. This finding is in agreement with the 6-month data presented in a recent study that demonstrated a reduction of IL1-b, IL-6, TNF-a, PDGFBB, and VEGF levels in PICF; while, treatment groups (PerioFlow® versus YAG: ER laser treatments) did not show any significant differences for the levels of these cytokines [30].
IL-6 is a proinflammatory cytokine and plays a critical role in the activation of CD4+ T helper (Th) cells [25], which may lead to the progression of the immune-inflammatory response [41], and indirectly, activate osteoclast activities [30]. In the present study, the fold change in IL-6 levels was found to be associated with the fold change in OPG levels, as well as VEGF levels. However, no relationship was demonstrated between the downregulation of mRNA levels of IL-6 and the changes in clinical and radiographic parameters. The present data are in contrast with those which were collected from a recent study that indicated a significant correlation between the reduced level of IL-6 concentration and BOP values after decontamination treatment in peri-implant infection [42]. Previous studies have identified that osteoclastogenesis is controlled by the interaction of the receptor activator of the NF-kB ligand (RANKL) and OPG, whose expressions are tightly regulated by the cytokines secreted by Th1 and Th2 cells (e.g., IL-6) contributing to peri-implantitis lesions [39, 43]. It was also reported that IL-6 could modulate the induction of VEGF which takes part in differentiation of hypertrophic chondrocytes, osteoblasts and osteoclasts by promoting angiogenesis and inhibition of both bone formation and resorption by blocking VEGF-mediated capillary invasion [44, 45].
IL-8 has chemotactic/activation effects on neutrophils under inflammatory conditions [46]. The reported findings on IL-8 concentration in peri-implantitis sites compared to healthy sites are conflicting. A higher concentration of this chemokine was observed in PICF from samples representing profuse bleeding in peri-implantitis sites [22, 27]. In contrast, no significant difference was indicated for IL-8 levels between peri-implantitis and healthy sites in some reports [24, 47]. In a recent study, upregulated IL-8 gene expression was demonstrated in PICF from peri-implantitis samples compared to healthy (fold change: 1.93) and mucositis samples (fold change: 2.31) [46]. Similar to these findings, both decontamination procedures in the RST of peri-implantitis exhibited downregulated IL-8 gene expression in treated peri-implantitis sites compared to non-treated sites in the present study (fold change: 2.70 and 2.29 for the ozone and control groups, respectively). On the other hand, the present study findings showed that the fold change in IL-8 levels was found to be associated with the fold change in SOST levels. This finding can be observed as a result of direct and indirect immune/bone-cell-mediated mechanisms by which osteoclasts may produce the osteoclastogenic chemokine IL-8 under pathological conditions [39].
Sclerostin encoded by the SOST gene is an osteocyte-derived negative regulator which suppresses osteoblastogenesis by inhibiting the Wnt/β-catenin pathway and also by blocking bone morphogenetic protein signaling [48, 49]. Recent evidence has indicated increased expression levels of the SOST gene in alveolar bone loss [50, 51]. In the present study, the downregulation of SOST gene expression was visibly noticed by a threefold decrease after the RST of peri-implantitis. Also, a significantly positive relationship was noted between the downregulated SOST mRNA level and PD reduction at 6 months; while, a negative correlation was observed between SOST mRNA level and the mean DF. Similarly, Rakic et al. [28] reported a significantly higher sclerostin level in peri-implantitis compared to mucositis and healthy sites. In that study, significant correlations were demonstrated between the same biomarker and BOP, PPD and CAL values at implant sites. In fact, systemic administration of sclerostin antibody has been suggested to have potential for conservative alveolar bone augmentation by enhancing bone formation and decreased bone resorption [51]. Based on the recent findings and current data, regulating the expression of SOST could provide a new therapeutic target in the RST of peri-implantitis.
It has been recently indicated that adjunctive ozone regimen in the RST of peri-implantitis exhibited a significant benefit in clinical and radiographic parameters [35]. Similarly, in the present study, additional ozone application presented a significantly higher radiographic DF at 6 months inconsistent with the previous animal model studies that demonstrated higher bone gain with ozone therapy [16, 52]. When the changes in clinical parameters are considered, the treatment modalities in both groups showed comparable results. However, a significant difference was noted in terms of the mean CAL value at the 6 months postoperatively. Nevertheless, topical gaseous ozone therapy could not demonstrate a significantly positive impact on the mRNA expression levels of selected biomarkers in PICF. This finding could be relevant with both duration and dosage of ozone application. Topical ozone was administered only for a short duration (during postoperative first week) as suggested by Kazancioglu et al. [53]. In addition, limited sample size might be one of the reasons for the lack of significance between the study groups.
Multiple factors related to peri-implantitis may also have an unfavorable effect on the both clinical and immunological outcomes of RST of peri-implantitis. To examine the possible effect of these factors on treatment outcome, a linear regression analysis was performed in this study. The recent evidence has identified that different implant surface treatments may influence the cytokine production in the progression of peri-implantitis. In an in vitro model, the secretion of interleukin IL-6, IL-8, IL-10, VEGF and monocyte chemoattractant protein-1 (MCP-1) in response to Porphyromonas gingivalis lipopolysaccharide (PgLPS) significantly increased with sandblasted and turned surfaces in comparison with anodized, acid-etched, TiO2-blasted/acid-etched, and grit-blasted/acid-etched surfaces [54]. Thus, the distribution of different implant systems and surface characteristics could be a limitation of the present study when analyzing the immunological profile. However, the regression analysis did not reveal implant surface characteristic as a significant factor affecting the treatment outcome in the present study. Implant function time was the only implant-related factor which was found to have a statistically significant relationship with the treatment outcome. The analysis indicated that implants having higher implant function time were related with higher 6-month CAL values. On the other hand, no significant difference was observed regarding to implant function time between the study groups.
Conclusion
Within the limitations of this study, it can be concluded that implant surface decontamination procedures applied with the RST contribute to a notable reduction in immuno-inflammatory response. The additional use of ozone therapy provided significantly higher CAL and radiographic DF at 6 months postoperatively. Downregulation of the SOST levels was significantly associated with PD reduction and radiographic DF in the treatment of peri-implantitis. Moreover, these findings may aid the development of new therapeutic strategies for bone gain in the RST of peri-implantitis.
References
Lindhe J, Meyle J, Periodontology EW. Peri-implant diseases: consensus report of the sixth European workshop on periodontology. J Clin Periodontol. 2008;35:282–5.
Berglundh T, Armitage G, Araujo MG, et al. Peri-implant diseases and conditions: consensus report of workgroup 4 of the 2017 World Workshop on the Classification of Periodontal and Peri-Implant Diseases and Conditions. J Periodontol. 2018;45:286–91.
Tonetti M, Palmer R. Clinical research in implant dentistry: study design, reporting and outcome measurements: consensus report of Working Group 2 of the VIII European Workshop on Periodontology. J Clin Periodontol. 2012;39:73–80.
Rakic M, Galindo-Moreno P, Monje A, et al. How frequent does peri-implantitis occur? A systematic review and meta-analysis. Clin Oral Investig. 2018;22:1805–16.
Gosau M, Hahnel S, Schwarz F, Gerlach T, Reichert TE, Burgers R. Effect of six different peri-implantitis disinfection methods on in vivo human oral biofilm. Clin Oral Implants Res. 2010;21:866–72.
Al-Hashedi AA, Laurenti M, Benhamou V, Tamimi F. Decontamination of titanium implants using physical methods. Clin Oral Implants Res. 2017;28:1013–21.
Patianna G, Valente NA, D'Addona A, Andreana S. In vitro evaluation of controlled-release 14% doxycycline gel for decontamination of machined and sandblasted acid-etched implants. J Periodontol. 2018;89:325–30.
Bernardi S, Bianchi S, Tomei AR, Continenza MA, Macchiarelli G. Microbiological and SEM-EDS evaluation of titanium surfaces exposed to periodontal gel: in vitro study. Materials. 2019;12:1448.
Roos-Jansåker AM, Persson GR, Lindahl C, Renvert S. Surgical treatment of peri-implantitis using a bone substitute with or without a resorbable membrane: a 5-year follow-up. J Clin Periodontol. 2014;41:1108–14.
Mahato N, Wu X, Wang L. Management of peri-implantitis: a systematic review, 2010–2015. Springerplus. 2016;5:105.
Renvert S, Roos-Jansåker AM, Persson GR. Surgical treatment of peri-implantitis lesions with or without the use of a bone substitute–a randomized clinical trial. J Clin Periodontol. 2018;45:1266–74.
Carcuac O, Derks J, Abrahamsson I, Wennström JL, Petzold M, Berglundh T. Surgical treatment of peri-implantitis: 3-year results from a randomized controlled clinical trial. J Clin Periodontol. 2017;44:1294–303.
Carcuac O, Derks J, Charalampakis G, Abrahamsson I, Wennström J, Berglundh T. Adjunctive systemic and local antimicrobial therapy in the surgical treatment of peri-implantitis: a randomized controlled clinical trial. J Dental Res. 2016;95:50–7.
Wang HL, Garaicoa-Pazmino C, Collins A, Ong HS, Chudri R, Giannobile WV. Protein biomarkers and microbial profiles in peri-implantitis. Clin Oral Implants Res. 2016;27:1129–36.
Hauser-Gerspach I, Vadaszan J, Deronjic I, et al. Influence of gaseous ozone in peri-implantitis: bactericidal efficacy and cellular response. An in vitro study using titanium and zirconia. Clin Oral Investig. 2012;16:1049–59.
Alpan AL, Toker H, Ozer H. Ozone therapy enhances osseous healing in rats with diabetes with calvarial defects: a morphometric and immunohistochemical study. J Periodontol. 2016;87:982–9.
Li Z, Tighe RM, Feng F, Ledford JG, Hollingsworth JW. Genes of innate immunity and the biological response to inhaled ozone. J Biochem Mol Toxicol. 2013;27:3–16.
Toita R, Tsuru K, Ishikawa K. A superhydrophilic titanium implant functionalized by ozone gas modulates bone marrow cell and macrophage responses. J Mater Sci Mater Med. 2016;27:127.
Sanz M, Chapple IL. Clinical research on peri-implant diseases: consensus report of Working Group 4. J Clin Periodontol. 2012;39:202–6.
Petkovic-Curcin A, Zeljic K, Cikota-Aleksic B, Dakovic D, Tatic Z, Magic Z. Association of cytokine gene polymorphism with peri-implantitis risk. Int J Oral Maxillofac Implants. 2017;32:241–8.
Zani SR, Moss K, Shibli JA, et al. Peri-implant crevicular fluid biomarkers as discriminants of peri-implant health and disease. J Clin Periodontol. 2016;43:825–32.
Melo RF, Lopes BM, Shibli JA, Marcantonio Junior E, Marcantonio RAC, Galli GMT. Interleukin-1β and interleukin-6 expression and gene polymorphisms in subjects with peri-implant disease. Clin Implant Dent Relat Res. 2012;14:905–14.
Casado PL, Canullo L, de Almeida FA, Granjeiro JM, Barboza EP, Duarte MEL. Interleukins 1β and 10 expressions in the periimplant crevicular fluid from patients with untreated periimplant disease. Implant Dent. 2013;22:143–50.
Ata-Ali J, Flichy-Fernández AJ, Alegre-Domingo T, Ata-Ali F, Palacio J, Peñarrocha-Diago M. Clinical, microbiological, and immunological aspects of healthy versus peri-implantitis tissue in full arch reconstruction patients: a prospective cross-sectional study. BMC Oral Health. 2015;15:43.
Severino VO, Beghini M, de Araújo MF, et al. Expression of IL-6, IL-10, IL-17 and IL-33 in the peri-implant crevicular fluid of patients with peri-implant mucositis and peri-implantitis. Arch Oral Biol. 2016;72:194–9.
Fonseca FJPO, Junior MM, Lourenço EJV, de Moraes TD, Figueredo CM. Cytokines expression in saliva and peri-implant crevicular fluid of patients with peri-implant disease. Clin Oral Implants Res. 2014;25:68–72.
Renvert S, Widén C, Persson GR. Cytokine expression in peri-implant crevicular fluid in relation to bacterial presence. J Clin Periodontol. 2015;42:697–702.
Rakic M, Struillou X, Petkovic-Curcin A, et al. Estimation of bone loss biomarkers as a diagnostic tool for peri-implantitis. J Periodontol. 2014;85:1566–74.
Wohlfahrt JC, Aass AM, Granfeldt F, Lyngstadaas SP, Reseland JE. Sulcus fluid bone marker levels and the outcome of surgical treatment of peri-implantitis. J Clin Periodontol. 2014;41:424–31.
Renvert S, Widén C, Persson RG. Cytokine and microbial profiles in relation to the clinical outcome following treatment of peri-implantitis. Clin Oral Implants Res. 2017;28:1127–32.
Berglundh T, Armitage G, Araujo MG, et al. Peri-implant diseases and conditions: consensus report of workgroup 4 of the 2017 World Workshop on the Classification of Periodontal and Peri-Implant Diseases and Conditions. J Periodontol. 2018;89:313–8.
Schwarz F, Sahm N, Schwarz K, Becker J. Impact of defect configuration on the clinical outcome following surgical regenerative therapy of peri-implantitis. J Clin Periodontol. 2010;37:449–55.
Silness J, Löe H. Periodontal disease in pregnancy II. Correlation between oral hygiene and periodontal condition. Acta Odontol Scand. 1964;22:121–35.
Löe H, Silness J. Periodontal disease in pregnancy I. Prevalence and severity. Acta Odontol Scand. 1963;21:533–51.
Isler SC, Unsal B, Soysal F, Ozcan G, Peker E, Karaca IR. The effects of ozone therapy as an adjunct to the surgical treatment of peri-implantitis. J Periodontal Implant Sci. 2018;48:136–51.
Schmittgen TD, Livak KJ. Analyzing real-time PCR data by the comparative C(T) method. Nat Protoc. 2008;3:1101–8.
Renvert S, Polyzois I. Treatment of pathologic peri-implant pockets. Periodontol. 2000;2018(76):180–90.
Ramanauskaite A, Daugela P, Juodzbalys G. Treatment of peri-implantitis: meta-analysis of findings in a systematic literature review and novel protocol proposal. Quintessence Int. 2016;47:379–93.
Fernandes MH, de Sousa GP. Bone cells dynamics during peri-implantitis: a theoretical analysis. Oral Maxillofac Res. 2016;7:e6.
Duarte PM, de Mendonça AC, Máximo MBB, Santos VR, Bastos MF, Nociti FH Jr. Effect of anti-infective mechanical therapy on clinical parameters and cytokine levels in human peri-implant diseases. J Periodontol. 2009;80:234–43.
Mardegan GP, Shibli JA, Roth LA, Faveri M, Giro G, Bastos MF. Transforming growth factor-β, interleukin-17, and IL-23 gene expression profiles associated with human peri-implantitis. Clin Oral Implants Res. 2017;28:10–5.
Al Ghazal L, O’Sullivan J, Claffey N, Polyzois I. Comparison of two different techniques used for the maintenance of peri-implant soft tissue health: a pilot randomized clinical trial. Acta Odontol Scand. 2017;75:542–9.
Duarte PM, De Mendonça AC, Máximo MBB, Santos VR, Bastos MF, Nociti Júnior FH. Differential cytokine expressions affect the severity of peri-implant disease. Clin Oral Implants Res. 2009;20:514–20.
Qu G, von Schroeder HP. Role of osterix in endothelin-1-induced downregulation of vascular endothelial growth factor in osteoblastic cells. Bone. 2006;38:21–9.
Mierzwinska-Nastalska E, Lomzynski L, Jaworska-Zaremba M, Kostrzewa-Janicka J. Vascular endothelial growth factor in gingival crevicular fluid around dental implants. Eur J Med Res. 2010;15:88–91.
Hall J, Pehrson NG, Ekestubbe A, Jemt T, Friberg B. A controlled, cross-sectional exploratory study on markers for the plasminogen system and inflammation in crevicular fluid samples from healthy, mucositis and peri-implantitis sites. Eur J Oral Implantol. 2015;8:153–66.
Severino VO, Napimoga MH, de Lima Pereira SA. Expression of IL-6, IL-10, IL-17 and IL-8 in the peri-implant crevicular fluid of patients with peri-implantitis. Arch Oral Biol. 2011;56:823–8.
Balli U, Aydogdu A, Dede FO, Turer CC, Guven B. Gingival crevicular fluid levels of sclerostin, osteoprotegerin, and receptor activator of nuclear factor-κB ligand in periodontitis. J Periodontol. 2015;86:1396–404.
Sebastian A, Loots GG. Transcriptional control of Sost in bone. Bone. 2017;96:76–84.
Kim JH, Kim AR, Choi YH, et al. Tumor necrosis factor-α antagonist diminishes osteocytic RANKL and sclerostin expression in diabetes rats with periodontitis. PLoS ONE. 2017;12:e0189702.
Liu M, Kurimoto P, Zhang J, et al. Sclerostin and DKK1 inhibition preserves and augments alveolar bone volume and architecture in rats with alveolar bone loss. J Dent Res. 2018;97:1031–8.
Ozdemir H, Toker H, Balcı H, Ozer H. Effect of ozone therapy on autogenous bone graft healing in calvarial defects: a histologic and histometric study in rats. J Periodontal Res. 2013;48:722–6.
Kazancioglu H, Kurklu E, Ezirganli S. Effects of ozone therapy on pain, swelling, and trismus following third molar surgery. Int J Oral Maxillofac Surg. 2014;43:644–8.
Stavroullakis A, Brito C, Chen HY, Bajenova E, Prakki A, Nogueira-Filho G. Dental implant surface treatments may modulate cytokine secretion in Porphyromonas gingivalis-stimulated human gingival fibroblasts: a comparative study. J Biomed Mater Res A. 2015;103:1131–40.
Funding
This study was financially supported by Gazi University Research Board, with project number 03/2017-03.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflicts of interest.
Ethical approval
The research protocol was approved by the Ethics Committee of the Faculty of Medicine, Gazi University, Ankara, Turkey, Ankara, Turkey in accordance with the ethical principles, including Declaration of Helsinki of 1975, as revised in 2013. (Protocol ID: 25901600-2858). The trial is registered at ClinicalTrials.gov NCT03018795.
Informed consent
The patients were informed about the protocol of the study and gave their written consent to the described procedures.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Isler, S.C., Soysal, F., Akca, G. et al. The effects of decontamination methods of dental implant surface on cytokine expression analysis in the reconstructive surgical treatment of peri-implantitis. Odontology 109, 103–113 (2021). https://doi.org/10.1007/s10266-020-00520-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10266-020-00520-0