Abstract
The downstream cascade of the inflammatory response to gliadin in celiac intestinal mucosa encompasses the early activation of the innate immunity that triggers the adaptive response. Therefore, the in vitro study of the pathogenic mechanism of celiac disease (CD) on enterocytes alone or mucosal T lymphocytes alone does not fully consider all the aspects of gliadin-dependent inflammation. Although the in vitro culture of specimens of intestinal mucosa obtained from celiac patients is the gold standard for the study of CD, this technique presents several technical challenges and the bioptic specimens are not easily available. So, in this paper, we described the gliadin-dependent cytokine production in a bidimensional cellular system, which is able to mimic both the innate and the adaptive steps of the mucosal immune response of CD. In the upper compartment, the intestinal epithelial cells are grown on a filter, and in the lower compartment, the mononuclear cells isolated from peripheral blood of celiac patients are cultured. Cells were apically exposed to the toxic gliadin peptide p31–43 for 3 h and then with the immunodominant gliadin fragment pα-9 for 21 h. The incubation with gliadin peptides resulted in increased levels of IL-15, INF-γ, IL-6, tumor necrosis factor (TNF)-α, IL-1β, and CCL 2, 3 and 4 in the basal supernatants, with respect to cells exposed to medium alone. The p31–43-driven epithelial priming of mucosal response consists of transglutaminase (TG2)-mediated deamidation of the immunostimulatory gliadin peptides, as demonstrated by the inhibition of pα-9 activity, when the system is exposed to blocking anti-TG2 antibody.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Celiac disease (CD) is a permanent autoimmune enteropathy, triggered in genetically predisposed individuals by dietary gluten [1, 2]. Gluten is the alcohol-soluble protein fraction of some cereals, such as wheat, rye, and barley. Gliadin is the main protein of wheat gluten [3].
In recent years, a growing body of evidence has shown that the peptides derived from the gastrointestinal hydrolysis of the gliadin are able to elicit selectively the innate or the adaptive immune response in celiac intestinal mucosa. The so-called toxic peptides, such as p31–43 and the longer p31–49, trigger, within 3 h since the contact with the mucosa, the cellular and molecular mechanisms of innate immunity, as demonstrated by the increased production of interleukin (IL)-15, the density of CD83+ and CD25+ cells, cyclooxygenase (COX)-2+ level, and the expression and activity of the cellular transglutaminase 2 (TG2) in the enterocytes [4, 5]. This early stage of the response to gliadin sets the tone, and it is necessary for the downstream inflammatory events, with the most relevant being the presentation of gliadin epitopes, such as p33mer, by DQ2/8+ antigen-presenting cells to CD4+ T cells. Thus, the activated T lymphocytes release interferon (INF)-γ, a Th-1 cytokine responsible for the destruction of the celiac intestinal mucosa [6, 7]. In this frame, the deamidation of gliadin epitopes by TG2 is a crucial step of T-cell response [8].
Pro-inflammatory cytokines are pivotal to regulate both the adaptive and immune responses in CD: IL-15 dominates the innate response, whereas INF-γ, along with tumor necrosis factor (TNF)-α, IL-2, IL-4, and IL-12 control the adaptive response [1, 9–12]. The key role of IL-15 and INF-γ in CD pathogenesis is confirmed by the finding that the abrogation of the mucosal production of both these molecules prevents the gliadin-dependent inflammation [13]. Paradoxically, an increase in production of the immunomodulatory cytokines IL-10 and tumor growth factor (TGF)-β has been found in intestinal mucosa of untreated CD patients with respect to treated celiacs and healthy controls. The incremented production of these immunomodulatory cytokines might be due to an inefficient attempt of regulating the mucosal inflammation [9, 14].
Thus, the in vitro study of the response of CD4+ T cells isolated from mucosa of celiac patients to gliadin epitopes is not able to fully understand all the aspects of gliadin-dependent inflammation and to identify all the gliadin peptides able to start and maintain the celiac mucosal response to gliadin. This model, even widely used in the literature, does not consider the early events of celiac inflammation and focuses on the adaptive response only. Likewise, the study of gliadin toxic effect on intestinal epithelial cells partially explores the pathogenesis of CD [15].
Therefore, the in vitro culture of duodenal mucosa withdrawn from celiac patients during intestinal endoscopy is still the gold standard to study in depth all the phases of the downstream cascade of the gliadin-dependent inflammation. However, this model presents some technical difficulties: the correct orientation of the specimen during the culture, the inclusion in the cutting medium and the required atmosphere to prevent the tissue necrosis during the culture. In addition, the mucosal samples are not easily available [4].
In this paper, we describe a bidimensional cellular in vitro system to study the cytokine production involved in both the innate and the adaptive steps of the CD immunity. In the upper compartment, the intestinal epithelial cells are grown to confluence and allowed to differentiate on an insert, and in the lower compartment, the mononuclear cells isolated from peripheral blood of celiac patients are cultured (Table 1).
Materials and methods
Culture of intestinal epithelial cells
Human colon carcinoma T84 cells (ATCC, CCL-248; passage 56) were cultured in 25-cm2 culture flasks (Falcon) in Dulbecco’s modified Eagle’s medium/F-12 (DMEM/F-12, 1:1) supplemented with 10 % heat-inactivated FCS and penicillin (100 U/ml)/streptomycin (100 μg/ml) (all from Life Technologies, Grand Island, NY). Cells were kept in an incubator at 37 °C and 5 % CO2. Medium was refreshed every 2–3 days, and cells were passaged once a week.
Purification of PBMC
Five ml of peripheral blood have been withdrawn from six untreated celiac patients (five females and three males, age range 6.4–14.8 years) and from 3 DQ2+ positive not CD-affected controls (healthy first-grade relatives of celiac patients). The Ethics Committee of ISS approved the protocol, and the patients’ parents signed the informed consent. Peripheral blood mononuclear cells were isolated using lympholite (Cederlane, UK) density gradient overlaid by heparin blood diluted 1:1 in PBS and centrifuged (20 min at 900 rpm). After being washed three times, PBMCs were resuspended in complete RPMI 1,640 supplemented with 25 mM HEPES, 10 % (v/v) heat-inactivated FBS, 100U/ml penicillin, 100 mg/ml streptomycin, and 1 % 2 mM l-glutamine.
Transwell co-culture model
For transwell experiments using polarized T84 cells, 3 weeks prior to the experiment, T84 cells were seeded at a density of 80 × 103 cells x cm2 on 0.4-μm, 1-cm2 tissue culture inserts (BD Falcon, USA). Transwell cultures (12-well) with confluent T84 monolayers were used for co-culture with 1 ml PBMC (1.5 × 106 cells/ml) using PBMC medium and kept in an incubator at 37 °C and 5 % CO2. Cells were allowed to settle for 1 h before the starting of the experiment. The permeability of the epithelial monolayer was assessed just before the experiments, measuring the transwell electrical resistance between the upper and lower compartments. A value of transwell resistance >800 Ω × cm2 has been considered index of a fully formed epithelial monolayer, not allowing the paracellular passage of molecules.
Peptides and cell treatments
P31–43, pα-9, and deamidated pα-9 were synthesized by Inbios (Napoli, Italy) using a HPLC (431C model; Applied Biosystems, Foster City, CA) and 99 % purified with reverse-phase HPLC (5,020 system; Varian Inc. Walnut Creek, CA). T84 cells were apically exposed for 3 h with p31–43 peptide (40 μg/ml) and then treated with pα-9 or its deamidate form (40 μg/ml). As negative control, cells were treated with medium alone, and with pα-9 or deamidated pα-9 alone. After 21 h from the addition of pα-9 to the culture, supernatants from the basolateral compartment were collected, centrifuged, and stored at −20 °C until cytokine measurement. At the same time, T84 cells from the apical compartment were harvested, lysated, and stored at −80 °C. In the inhibition experiments, the CUB7402 (NeoMarkers, Freemont, CA, USA) antibody was added in the upper compartment 30 min before the p31–43 at a concentration of 10 μg/ml.
Measurement of cytokine levels in culture medium
Cytokine levels in culture medium from the lower compartment were measured with a colorimetric ELISA kit (Qiagen, Hilden, Germany), according to the manufacturer’s instruction.
Western blotting
Whole T84 cell extracts were washed twice in ice-cold PBS, resuspended in 150 mM NaCl, 1 % Triton X-100 1 % (Sigma, St Louis, MO, USA) and a mixture of protease inhibitors (1:50; Sigma), and incubated on ice for 20 min and then centrifuged for 5 min at 4 °C. The supernatant was stored at −70 °C as whole-cell protein lysate. SDS–PAGE (sodium dodecyl sulfate–polyacrylamide gel electrophoresis) was carried out on 4 % stacking and 7.5 % resolving gel (Bio-Rad, Hercules, CA, USA). Equal amounts of protein (50 mg) were loaded in each lane with loading buffer containing 0.1 Tris (pH 6.8), 20 % glycerol, 10 % mercaptoethanol, 4 % SDS, and 0.2 % bromophenol blue (Bio-Rad). Samples were heated at 100 °C for 5 min before gel loading. After electrophoresis, the proteins were transferred to a PVDF membrane (Bio-Rad). Membranes were blocked for 1 h with 5 % non-fat milk in TBS (100 mM NaCl, 5 mM KCl, 100 mM Tris–HCl, pH 7.4, and 0.05 % Tween 20, Bio-Rad) and incubated overnight with IL-15 antibody (mouse, dilution 1:100, Abcam, Cambridge, MA, USA) and then washed three times for 5 min in TBST. Secondary antibody (goat anti-mouse, conjugated to horseradish peroxidase, HRP) (Bio-Rad) was diluted 1:15,000 in the blocking solution, added to membranes for 1 h at RT, and then washed three times in TBS for 5 min. Proteins on membranes were revealed by the chemiluminescence detection kit (Bio-Rad), according to manufacturer’s instructions. Intensity of protein bands on blots was measured using the Bio-Rad ChemiDoc densitometer, and the analysis was made using ImageJ software. Membranes were stripped and reprobed with β-actin antibody (Abcam) diluted 1:400 to verify equal loading of proteins. The density of the band was measured by a J densitometric software.
Statistical analysis
Statistical analysis was performed using SPSS version 15.0 software (SPSS Inc., Chicago, IL, USA). Data are expressed as mean ± SD; a multivariate ANOVA was used to compare means. p < 0.05 was considered significant.
Results
We know from previous studies that the preincubation with the toxic gliadin peptide p31–43 enables immunodominant epitopes such as pα-9, spanning the amino acids in position 57–68 of α-gliadin sequence, to induce T-cell activation in organ culture of mucosal samples from celiac patients [4, 5]. In order to mimic the microenvironment wherein the cascade of the events can activate the immune response, a bidimensional model was set up, consisting in a co-culture of intestinal T84 cells in the apical compartment and PBMC from celiac patients in the basolateral compartment. Then, we challenged this system by adding in the apical compartment the p31–43 for 3 h and then pα-9 for 21 h. In addition, aiming at discriminating the effect of each of these two peptides on the production of the cytokines, we also added to our bidimensional model p31–43 or the deamidated or not deamidated form of pα-9 alone.
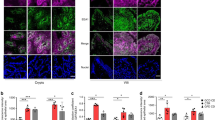
As shown in Fig. 1a, the INF-γ concentration in the supernatants collected in the lower compartment results to be increased with respect to the negative control (medium only) by the sequential addition of p31–43 and pα-9 in the apical chamber. The incubation of the cells with each of p31–43 or pα-9 alone does not exert such an increase. Interestingly, the deamidated form of pα-9 added alone in the upper compartment is able to increase the levels of INF-γ in the medium of lower compartment. As expected, the cytokine release in the basal compartment after the exposure of the bidimensional systems to gliadin peptides is CD specific. When PBMCs from healthy controls are added in the lower compartment, we did not notice any increase in INF-γ concentration after the treatment with p31–43 and pα-9 in combination or deamidated pα-9 alone (medium 21.3 ± 3.9 vs. 25.1 ± 4.9 vs. 27.1 ± 8.5; p = 0.4). In a similar manner, IL-6 requires the presence of both p31–43 and pα-9 or deamidated pα-9 to be increased in the supernatants; the incubation with pα-9 alone is not able to exert any effect on IL-6 concentration (Fig. 1b).
INF-γ (a), IL-6 (b), TNF-α (c), TGF- β (d), and IL-1 (e) concentration in the basal compartment of the bidimensional cellular system, measured by a commercial ELISA kit, after incubation with indicated peptides at a concentration of 40 μg/ml or medium alone (ctr). Data are expressed as mean ± S.D. of three separate experiments, each performed in triplicate. # p < 0.05. Statistical differences were calculated by multivariate ANOVA
On the contrary, we also found a series of cytokines, whose concentration is increased by the presence of p31–43 alone and not when the bidimensional system is challenged with deamidated pα-9: TNF- α, IL-1β, and the chemokine ligands (CCL) 2, 3 and 4. These cytokines are likely to be produced by the epithelial cells after the exposure to p31–43 and drive the very early events of the gliadin-dependent downstream cascade (Figs. 1c–e and 2a–c).
CCL2 (a), CCL3 (b), and CCL4 (c) concentration in the basal compartment of the bidimensional cellular system, measured by a commercial ELISA kit, after incubation with indicated peptides at a concentration of 40 μg/ml or medium alone (ctr). Data are expressed as mean ± S.D. of three separate experiments, each performed in triplicate. # p < 0.05. Statistical differences were calculated by multivariate ANOVA
Additionally, we measured by means of ELISA kit the concentration of IL-4, IL-10, and IL-15 in the basal supernatant, and we did not obtained significant difference in the concentration of this cytokine after the treatment with the different peptides with respect to cells exposed to medium alone (data not shown). So, we studied the cellular level of IL-15 in T84 cells by Western blotting. As shown in Fig. 3, the exposure of T84 cells to p31–43 alone and p31–43 before pα-9 or deamidated pα-9 determines a significant increase in cellular level of IL-15 in as short as 3 h. Pα-9 or deamidated pα-9 alone does not increase the concentration of IL-15 in T84 cells.
Expression of IL-15 in T84 cells exposed in vitro to indicated peptides at a concentration of 40 μg/ml or medium alone (ctr) as resulted by a Western blotting analysis. a The figure represents the result of an experiment out of the three WB performed. b The density of the blots was quantified with Image J densitometry software, and results are expressed as mean of density of the bands, normalized for the corresponding actin density. # p < 0.05. Statistical differences were calculated by multivariate ANOVA
To test the hypothesis that p31–43 triggers the pα-9 deamidation, by activating the cellular TG2 in the enterocytes, we measured the INF-γ production in the basal compartment of this bidimensional system challenged with p31–43 and pα-9, after a 30-min incubation with the anti-TG2 blocking antibody CUB7402. As shown in Fig. 4, a 30-min preincubation of the epithelial cells with the blocking anti-TG2 antibodies prevents the ability of pα-9 of increasing the levels of INF-γ in the basal compartment. On the contrary, the CUB7402 antibody does not affect the immunostimulatory activity of the deamidated form of pα-9.
INF-γ concentration in the basal compartment of the bidimensional cellular system, measured by a commercial ELISA kit, after incubation with indicated peptides at a concentration of 40 μg/ml and preincubation with blocking anti-TG2 at a concentration of 10 μg/ml or medium alone (ctr). Data are expressed as mean ± S.D. of three separate experiments, each performed in triplicate. # p < 0.05. Statistical differences were calculated by multivariate ANOVA
Discussion
In the present paper, we describe a bidimensional co-culture cellular system, which mimics the sequential involvement of enterocytes and T cells in the intestinal mucosal response to gliadin. Although the in vitro organ culture of specimens of intestinal mucosa obtained from celiac patients is the gold standard for the study of the pathogenic mechanisms of CD, this cellular system has some advantage, since: (1) it allows to discriminate the contribution of each of the two branches of immunity to the overall gliadin-dependent response, (2) it is cheap and finally (3) it offers less technical challenges than the organ culture of the intestinal mucosa.
A bidimensional model with the intestinal epithelial cells grown in the upper compartment has been already described as a tool to study the absorption of nutrients and xenobiotic in the human intestine. Some of the authors of this paper have already described how the p31–43 impacts the permeability of a monolayer of human intestinal epithelial cells grown on a polycarbonate filter [16]. De Palma et al. [17] have set up a co-culture model similar to ours, with human intestinal cell line Caco-2 forming the epithelial monolayer and celiac PBMCs in the lower compartment. These authors, however, have challenged the system with the whole gliadin digest, and they have not discriminated the effect of toxic and immunodominant gliadin peptides.
The mucosal response to gliadin peptides in CD is characterized by increased levels of several cytokines, both inflammatory and immunomodulatory [9–12]. Our results have confirmed previous seminal studies reporting that the toxic gliadin fragment p31–43 exerts a direct effect on intestinal epithelial cells [16, 18, 19], thus setting the tone for the mucosal adaptive response to gliadin epitopes [5]. The incubation of p31–43 alone is sufficient to induce the production of epithelial-derived cytokines, whereas the incubation with the immunostimulatory pα-9 alone does not exert any effect on the levels of T-cell-derived cytokines, such as INF-γ. This molecule is the main mediator of the Th1 inflammation of celiac mucosa, and it is mainly responsible for the tissue destruction and the consequent rearrangement [1, 2]. The intracellular levels of IL-15 in T84 cells, on the contrary, are affected only by the incubation with the p31–43 alone or in combination. The profile of the increase in INF-γ and IL-15 upon the incubation with gliadin peptides shows that our system is able to fully mimic the cytokine-mediated response to gliadin, and it might be used to study in laboratory some aspect of CD pathogenesis and the preventive effect of some molecules toward the celiac inflammation.
The ELISA determination has not detected any differences in IL-15 concentration in the cell culture supernatants after the treatment with the different peptides, whereas the determination by Western blotting with monoclonal anti-IL-15 antibodies has showed a significant increase in IL-15 after the cell treatment with p31–43. IL-15 production has an intracellular control, at post-transcriptional and trafficking level [20]; so the intracellular level and not the concentration of this cytokine in the culture medium is affected by an in vitro stimulation. As a matter of the fact, other authors in their studies have measured the intracellular, and not the extra-cellular level, of IL-15 [21, 22].
Our results have clearly showed that the priming of intestinal mucosa by gliadin peptides consists, besides the activation of innate immunity, in the deamidation of the gliadin epitopes also. This confirms the previous findings that the peripheral T-cell response in CD is directed against deamidated, but not native gliadin epitopes [23]. The incubation with the deamidated form of pα-9 gives the same results of the exposure in combination with p31–43 and pα-9 in inducing the release of INF-γ. This effect might be driven by IL-15, since it has been demonstrated that blocking IL-15 prevents the gliadin-dependent T-cell activation [4]. Our results demonstrate that the deamidation of the immunomodulatory gliadin peptides occurs in the upper compartment, since the preincubation of our system with blocking anti-TG2 CUB7402 prevents the ability of pα-9 of eliciting the production of INF-γ, whereas it does not affect the immunodominant capacity of the deamidated pα-9. So, it is clear that the deamidation of immunomodulatory gliadin peptides is catalyzed by epithelial cells-related TG2 and not only by TG2 present in the stromal of intestinal mucosa, as assumed so far [24]. Some important previous studies have reported that the expression and activity of TG2 are increased in enterocytes upon the exposure to p31–43; thus, the deamidation of gliadin is catalyzed into or on the surface of the enterocytes [5].
In the herein described system, the incubation with gliadin peptides has also increased IL-6, TGF- β, TNF-α, and IL-1 concentration. Discussing the role of each of those molecules in the celiac inflammation is beyond the scope of this paper; we measured them to test the reproducibility on our system of the cytokine network triggered by gliadin peptides in celiac mucosa and peripheral blood. On the contrary, we failed to obtain an increase in IL-4 and IL-10. Probably, the basal levels of those two cytokines in the supernatants of activated T cells were so high that the effect of the gliadin peptides was not detectable.
Interestingly, we have also found that the incubation with p31–43 alone dramatically increases the release of some molecules of the chemokine ligands superfamily, such as CCL-2, 3, and 4. There have been similar previous findings that some CCL-related cytokines, such as IL-8, are overexpressed in serum and intestinal mucosa of active CD patients with respect to treated celiacs and healthy controls [25, 26]. In addition, another gliadin fragment with toxic activity, p270–286, induces the CXCR-3 dependent release of IL-8 from celiac peripheral blood mononuclear cells [27]. We have already shown that the exposure of intestinal epithelia cells to gliadin peptides induces the production of IL-8 [28]. Likely, the cytokines of CCL family set the inflammatory environment in intestinal mucosa during the very early stages of the response to gliadin, attracting the monocytes/dendritic cells and the granulocytes and thus arming the effector CD4+ T cells.
References
Meresse B, Malamut G, Cerf-Bensussan N. Celiac disease: an immunological jigsaw. Immunity. 2012;36:907–19.
Sollid LM, Jabri B. Triggers and drivers of autoimmunity: lessons from coeliac disease. Nat Rev Immunol. 2013;13:294–302.
Jabri B, Kasarda DD, Green PH. Innate and adaptive immunity: the yin and yang of celiac disease. Immunol Rev. 2005;206:219–31.
Maiuri L, Ciacci C, Ricciardelli I, et al. Association between innate response to gliadin and activation of pathogenic T cells in coeliac disease. Lancet. 2003;362:30–7.
Maiuri L, Ciacci C, Ricciardelli I, et al. Unexpected role of surface transglutaminase type II in celiac disease. Gastroenterology. 2005;129:1400–13.
Petersen J, Montserrat V, Mujico JR, et al. T-cell receptor recognition of HLA-DQ2–gliadin complexes associated with celiac disease. Nat Struct Mol Biol. 2014;21:480–8.
Tollefsen S, Arentz-Hansen H, Fleckenstein B, et al. HLA-DQ2 and -DQ8 signatures of gluten T cell epitopes in celiac disease. J Clin Invest. 2006;116:2226–36.
Sollid LM, Jabri B. Celiac disease and transglutaminase 2: a model for post-translational modification of antigens and HLA association in the pathogenesis of autoimmune disorders. Curr Opin Immunol. 2011;23:732–8.
Forsberg G, Hernell O, Melgar S, et al. Paradoxical coexpression of proinflammatory and down-regulatory cytokines in intestinal T cells in childhood celiac disease. Gastroenterology. 2002;123:667–78.
Nilsen EM, Jahnsen FL, Lundin KE, et al. Gluten induces an intestinal cytokine response strongly dominated by interferon gamma in patients with celiac disease. Gastroenterology. 1998;115:551–63.
Garrote JA, Gómez-González E, Bernardo D, Arrantz E, Chirdo F. Celiac disease pathogenesis: the proinflammatory cytokine network. J Pediatr Gastroenterol Nutr. 2008;47:S27–32.
Nanayakkara M, Lania G, Maglio M, et al. An undigested gliadin peptide activates innate immunity and proliferative signaling in enterocytes: the role in celiac disease. Am J Clin Nutr. 2013;98:1123–35.
Schuppan D, Junker Y, Barisani D. Celiac disease: from pathogenesis to novel therapies. Gastroenterology. 2009;137:1912–33.
Salvati VM, Mazzarella G, Gianfrani C, et al. Recombinant human interleukin 10 suppresses gliadin dependent T cell activation in ex vivo cultured coeliac intestinal mucosa. Gut. 2005;54:46–53.
Lindfors K, Rauhavirta T, Stenman S, Mäki M, Kaukinen K. In vitro models for gluten toxicity: relevance for celiac disease pathogenesis and development of novel treatment options. Exp Biol Med. 2012;237:119–25.
Silano M, Vincentini O, Luciani A, et al. Early tissue transglutaminase-mediated response underlies K562(S)-cell gliadin—dependent agglutination. Pediatr Res. 2012;71:532–8.
De Palma G, Kamanova J, Cinova JL, et al. Modulation of phenotypic and functional maturation of dendritic cells by intestinal bacteria and gliadin: relevance for celiac disease. J Leukoc Biol. 2012;92:1043–54.
Luciani A, Villella VR, Vasaturo A, et al. Lysosomal accumulation of gliadin p31–43 peptide induces oxidative stress and tissue transglutaminase-mediated PPARgamma downregulation in intestinal epithelial cells and coeliac mucosa. Gut. 2010;59:311–9.
Barone MV, Zanzi D, Maglio M, et al. Gliadin-mediated proliferation and innate immune activation in celiac disease are due to alterations in vesicular trafficking. PLoS One. 2011;6:e17039.
Pagliari D, Cianci R, Frosali S, et al. The role of IL-15 in gastrointestinal diseases: a bridge between innate and adaptive immune response. Cytokine Growth Factor Rev. 2013;24:455–66.
DePaolo RW, Abadie V, Tang F, et al. Co-adjuvant effects of retinoic acid and IL-15 induce inflammatory immunity to dietary antigens. Nature. 2011;471:220–34.
Camarca A, Radano G, Di Mase R, et al. Short wheat challenge is a reproducible in-vivo assay to detect immune response to gluten. Clin Exp Immunol. 2012;169:129–36.
Lammi A, Arikoski P, Vaarala O, Kinnunen T, Ilonen J. Increased peripheral blood CD4+ T cell responses to deamidated but not to native gliadin in children with coeliac disease. Clin Exp Immunol. 2012;168:207–14.
Esposito C, Paparo F, Caputo I, et al. Expression and enzymatic activity of small intestinal tissue transglutaminase in celiac disease. Am J Gastroenterol. 2003;8:1813–20.
Tack GJ, van Wanrooij RL, Von Blomberg BM, et al. Serum parameters in the spectrum of coeliac disease: beyond standard antibody testing–a cohort study. BMC Gastroenterol. 2012;12:159.
Kalliomäki M, Satokari R, Lähteenoja H, et al. Expression of microbiota, toll-like receptors, and their regulators in the small intestinal mucosa in celiac disease. J Pediatr Gastroenterol Nutr. 2012;54:727–32.
Lammers KM, Khandelwal S, Chaudhry F, et al. Identification of a novel immunomodulatory gliadin peptide that causes interleukin-8 release in a chemokine receptor CXCR3-dependent manner only in patients with coeliac disease. Immunology. 2011;132:432–40.
Vincentini O, Quaranta MG, Viora M, Agostoni C, Silano M. Docosahexaenoic acid modulates in vitro the inflammation of celiac disease in intestinal epithelial cells via the inhibition of cPLA2. Clin Nutr. 2011;30:541–6.
Conflict of interest
None to be declared.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Vincentini, O., Maialetti, F., Gonnelli, E. et al. Gliadin-dependent cytokine production in a bidimensional cellular model of celiac intestinal mucosa. Clin Exp Med 15, 447–454 (2015). https://doi.org/10.1007/s10238-014-0325-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10238-014-0325-2