Abstract
Background
Different countries have different preferences regarding health, and there are different value sets for popular preference-based measures across different countries. However, the cost of collecting data to generate country-specific value sets can be prohibitive for countries with smaller population size or low- and middle-income countries (LMIC). This paper explores whether existing preference weights could be modelled alongside a small own country valuation study to generate representative estimates. This is explored using a case study modelling UK data alongside smaller US samples to generate US estimates.
Methods
We analyse EQ-5D valuation data derived from representative samples of the US and UK populations using time trade-off to value 42 health states. A nonparametric Bayesian model was applied to estimate a US value set using the full UK dataset and subsets of the US dataset for 10, 15, 20 and 25 health states. Estimates are compared to a US value set estimated using US values alone using mean predictions and root mean square error.
Results
The results suggest that using US data elicited for 20 health states alongside the existing UK data produces similar predicted mean valuations and RMSE as the US value set, while 25 health states produce the exact features.
Conclusions
The promising results suggest that existing preference data could be combined with a small valuation study in a new country to generate preference weights, making own country value sets more achievable for LMIC. Further research is encouraged.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Health resource allocation is becoming increasingly important in an economic climate of increasing demands on healthcare systems with constrained budgets. Economic evaluation using cost–utility analysis is becoming a widely popular technique internationally to inform resource allocation decisions. Cost–utility analysis measures benefits using Quality Adjusted Life Years (QALYs), a commonly used measure that multiplies a quality adjustment for health by the duration of that state of health [1]. The quality adjustment weight is generated using utility values where 1 represents perfect health and 0 represents dead, and is most often generated using an existing preference-based measure. A preference-based measure consists of a classification system used to describe health (patients report their own health and this is assigned to a health state using a classification system) and a value set that generates a utility value for every health state defined by the classification system.
Currently, a number of preference-based measures of health-related quality of life (HRQoL) are available, including EQ-5D [2], HUI2 and 3 [3, 4], AQoL [5], QWB [6], and SF-6D [7], though there are an increasing number of condition-specific measures available [8]. The EQ-5D has become a popular measure of HRQoL and there are many different value sets available for two reasons. First, different countries can have different preferences. Different countries have different population compositions, different types of work, different cultures, and these can all impact on the relative values given to different dimensions of health (for example, self-care and anxiety/depression) as well as where on the 1–0 full health–dead scale each health state lies. The ordering of health states can vary across countries, as well as the position on the scale in relation to dead. Although Badia et al. [9] reported quite small and unimportant differences in EQ-5D valuations between UK, US and Spain, it is shown in Johnson et al. [10] that differences between the US and UK were potentially important. Second, international agencies that review cost–utility analyses to inform resource allocation decisions typically prefer QALYs to be generated using their own country value set (see Rowen et al. [11] for an overview). This is related to the first reason, as if different countries have different preferences it is important to take into account the country’s own citizens’ views when making resource allocation decisions. However, the cost of collecting data to generate country-specific value sets can be prohibitive for countries with smaller population size or low- and middle-income countries (LMIC). For example, if valuation data are collected via face-to-face interview, this can be costly and time consuming and the number of interviews would be in the hundreds. Although valuation data can be collected online, making the data collection quicker and cheaper, this is not feasible for all countries. For some LMIC, the use of an online survey may be impractical and may not achieve a representative sample of the general population by sociodemographic characteristics. In addition, understanding of valuation tasks cannot be monitored in an online environment which is a disadvantage for data collection in countries where valuation tasks have not been undertaken previously. This can mean that for these countries that value sets of alternative countries are used instead to generate QALYs, such as UK or US values, yet these values may not be representative of the country’s own citizens, and this could potentially impact on the validity of the resource allocation decisions made.
There is now an increasing number of datasets of preference data, where preferences have been elicited for the same measure for different countries. In Kharroubi et al. [12], a nonparametric Bayesian method is used to model the differences in EQ-5D valuations between the US and UK as an alternative approach to the parametric random-effects model of Johnson et al. [10]. Recently, this model has also been applied to the joint UK–Hong Kong and UK–Japan SF-6D data set ([13, 14]).
Such a model offers a major added advantage as it permits the utilization of the already existing results of one country to improve those of another, and as such generated utility estimates of the second country will be more precise than would have been the case if that country’s data were collected and analysed on its own. Such an analysis (drawing extra information from country 1) may allow a reduction in the sample size in country 2 to attain the same precision as achieved with a complete valuations in that country.
The aim of the paper is to determine whether an accurate value set can be generated for a country using only a small sample of data collected in that country, through jointly modelling the data with data collected for another country. This is explored using a case study for US and UK data, where a range of subsets of the health states valued in the US study are modelled alongside the full UK dataset, and the estimates are compared to the estimates generated modelling US data alone.
First, the US and UK EQ-5D valuation studies as well as the datasets used here are summarized. Second, the Bayesian nonparametric model is described and third, the results are presented. Finally, the results are discussed, including limitations and suggestions of possible directions for future research.
EQ-5D data set
The EQ-5D is a descriptive system defined by five health dimensions: mobility, self-care, usual activities, pain/discomfort and anxiety/depression. Each is assigned to three levels of health-related problems: “no problem” (level 1), “moderate or some problem” (level 2) and “severe problem” (level 3). Different combinations result in 243 possible health states, which are associated with a five-digit descriptor ranging from 11111 for perfect health and 33333 for the worst state possible. For example, state 13232 translates into no problems in mobility, severe problems in self-care, moderate problems in usual activities, extreme pain or discomfort and moderate anxiety or depression [15].
For EQ-5D to be used as a preference-based measure of HRQoL, a single utility value is assigned to each health state; by convention, utility value of 1 designates full health with all the rest having values less than one. Immediate death is conventionally assigned the utility zero and is considered as a baseline against the different health states that can possibly assume negative value had they felt worse than death. These utility indexes have been elicited from the valuation survey undertaken by the Measurement and Valuation of Health (MVH) group at York, using the time trade-off (TTO) technique [16]. A representative sample of 3395 members of the UK general population were interviewed in their own homes, where they were asked to value 12 health states. The valuation did not include all 243 states defined by the EQ-5D and chose to value a sample of 42 states. Further details on this study are provided elsewhere [17].
The US valuation study valued an identical set of states using the same UK valuation methods. However, a different approach was used to sample respondents, where a four-stage clustering sampling strategy was used, that focused on the Hispanics and non-Hispanic blacks [18]. One further difference was that respondents were interviewed in English in the UK whereas in the US respondents had the choice of being interviewed in either English or Spanish. The UK study interviewed a sample of 3395 respondents (response rate: 64%) whereas a sample of 4048 (response rate 59.4%) respondents was interviewed in the US study. However, respondents were not included due to missing and/or inconsistent responses. This results in a total of 2997 UK respondents and 3773 US respondents. Both samples represented their populations in regard to sociodemographic characteristics [17, 18].
Both studies elicited TTO valuations for the 42 EQ-5D health states [17, 18]. Briefly, respondents were first asked whether an impaired health state is better or worse than immediate death. For health states regarded as better than dead, respondents were asked to choose between living full health for x years (x ≤ 10) and 10 years spent in the impaired health state. For states regarded as worse than being dead, respondents were provided the choice of living in that state for (10 − x) years. This is followed by living in perfect health for x years (x < 10) or immediate death. The valuation scores were then transformed using the equation x/10, if states considered as better than death, and in the UK study − x/10, if states regarded worse than death, to bound them on the [− 1, 1] scale [19], and in the US study (− x/(10 − x))/ − z, where z is the worst value produced by − x/10, which is − 39 in this case [18].
The UK and US valuation studies also differed in procedures for assigning health states (i.e. 12 states for each respondent). The US individuals were randomized to receive 1 of 5 groups of pre-defined health states, where 4 groups included 33333 in addition to 2 randomly selected very mild states and 9 states randomly selected from the remaining 36 EQ-5D states. The 5th group included 33333 and 11 health states selected randomly from the remaining 41 states. In the UK, however, 41 health states (excluding 33333) were stratified into 4 classes according to severity of problems, where each individual was randomly assigned 2 very mild, 3 mild, 3 moderate, and 3 severe states, plus 33333. Further details on the UK and US studies have been reported elsewhere [17, 18].
Modelling
The modelling approach is described in Kharroubi et al. [12], where a nonparametric Bayesian model was used to model the differences between the US and UK EQ-5D health state valuations, providing an alternative approach to the conventional parametric model. Using the full US and UK data, Kharroubi et al. [12] found potentially important differences between the US and UK valuations of EQ-5D. In particular, Kharroubi et al. [12] found that US individuals give bigger utility values on all of the 42 health states. Because the covariates and respondent random effects enter the nonparametric Bayesian model multiplicatively, the difference between the two countries was shown to be minor for good and moderate health states and at its major for the worst health state. In addition, there seemed to be a substantial interaction between nationality and gender. Kharroubi et al. [12] found that the tendency to give bigger utilities is stronger for females than for males in the UK, while this is not the case for the US respondents. Finally, Kharroubi et al. [12] showed that the US respondents are more sensitive to poor health in mobility and self-care, but less sensitive in the dimensions of usual activities, pain and anxiety. A detailed description of the analysis is provided in Kharroubi et al. [12].
In this article, we follow on from this work to examine whether the adoption of a range of sample sizes of US health states (10, 15, 20, 25 states), while borrowing extra evidence from the UK study, generates the same valuations as analysing the full US data by itself. The model is estimated using a restricted sample of the US health states (10, 15, 20 and 25) alongside the full UK sample. These estimates are compared to those estimated using all US data excluding the UK data using different prediction criterion, including predicted versus actual mean health state valuations, mean predicted error, root mean squared error and an out-of-sample prediction.
For combined analysis, data from the US and UK studies were combined as being derived from one study with m = 6770 respondents. For i = 1, 2, …, \({n_j}\) and j = 1,2, …, m, xij is the ith health state valued by respondent j and the dependent variable yij is the TTO valuation given by respondent j for that health state. Finally, let tj be a vector of covariates for respondent j. In particular, tj includes not only a dummy variable to differentiate respondents’ national identity, but it also includes the respondent’s age and sex.
Kharroubi et al. [12] model the ith valuation by respondent j as
where \(h({{\mathbf{t}}_j})\) being a vector of functions of covariates tj and γ is a vector of unknown coefficients, \({\alpha _j}\) is a random individual effect, \({\varepsilon _{ij}}\) is the usual random error, \({u_c}({\mathbf{x}})\) is the base utility for the health state vector x and the subscript c represents the respondent’s country, where c = 1 if respondent j is in the US sample, and c = 0 if he/she is in the UK sample. It is perhaps easier to understand (1) by writing it in terms of disutilities \({z_{ij}}=1 - {y_{ij}}\) and \({v_c}\left( {{{\mathbf{x}}_{ij}}} \right)=1 - {u_c}\left( {{{\mathbf{x}}_{ij}}} \right)\) as \({z_{ij}}=\exp \left( {{\gamma ^\prime }{\text{h}}\left( {{{\varvec{t}}_j}} \right)+{\alpha _j}} \right){v_c}\left( {{{\mathbf{x}}_{ij}}} \right)+{\varepsilon _{ij}}~,\) i.e. simply a multiplicative model with zero intercept. Then we see that the observed disutility \({z_{ij}}\) is modelled as the base disutility \({v_c}\left( {{{\mathbf{x}}_{ij}}} \right)~\) for the respondent’s country c, multiplied by the respondent’s effect and then with random error applied. For perfect health, \({u_c}\left( {{{\mathbf{x}}_{ij}}} \right)=1,~\) i.e. \({v_c}\left( {{{\mathbf{x}}_{ij}}} \right)=0,~\)and all respondents value it as such apart from the random elicitation errors \({\varepsilon _{ij}}\). For poorer health states, \({v_c}\left( {{{\mathbf{x}}_{ij}}} \right)\) is larger and respondent covariate and random effects produce larger variations in the elicited values, thereby accounting for the observed greater variability in respondents’ utilities for poorer health states.
The interpretation of the base utility \({u_c}\left( {\mathbf{x}} \right)~\) for country c is that this is the utility function for a respondent from that country with respondent effect \({\lambda _j}=\exp \left( {{\gamma ^\prime }{\text{h}}\left( {{{\varvec{t}}_j}} \right)+{\alpha _j}} \right)=1\). A respondent with \({\lambda _j}\) > 1 will exhibit greater disutility and hence lower utility than the base utility for all states x. The differential is greater for states with low utility than for those with higher utility (and is zero for perfect health). Conversely, a respondent with \({\lambda _j}\) < 1 will have higher utilities than the base function for all x, also with increasing differential the lower the base utility of x. This is a key feature of model (1) that is observed in valuation data, and is one way in which it better represents reality than that of previous analysis (see Kharroubi et al. [12] for more details).
Kharroubi et al. [12] formally assumed normal distributions for the random terms
where \({\tau ^2}\)and \({v^2}\) are further parameters to be estimated. The distribution of \({\lambda _j}\) is then log-normal, resulting in a skewness that is also typically observed in valuation data. Note that ts are centred to ensure that they have zero means, and hence that the value of \({\lambda _j}\) for a typical person is 1.
Kharroubi et al. [12] model the relationship between the two base utility functions through
where \({\mu _0}\), \({\mu _1}\), \({\varvec{\beta}_0}\) and \({\varvec{\beta}_1}\) are unknown coefficients and \(d({\mathbf{x}})\) denotes a shift of the utility function from the linear regression form. The expression\({\mu _0}+\varvec{\beta}_{0}^{\prime }{\mathbf{x}}\) in (2) expresses a prior belief that the utility function \({u_0}({\mathbf{x}})\) for UK respondents will be approximately linear and additive in the various dimensions. The corresponding expression in (3) modifies (2) with additional coefficients \({\varvec{\beta}_1}\) to reflect dimension-specific differences between the US and UK [12], but notice they share the same \(d({\mathbf{x}})\) function. Hence, we suppose that the utility functions for the two nationalities have the same basic shape but can nevertheless differ in important respects.
The term \(d({\mathbf{x}})\) is dealt with as an unknown function and so in Bayesian context it will be treated as a random variable. Kharroubi et al. [12] assign independent normal distribution to \(d({\mathbf{x}})\) as
for all x and
where for d = 1, 2, …, 5, \({x_d}\) and \(x_{d}^{\prime }\) are the levels of dimension d in the health states x and \({\mathbf{x^{\prime}}}\), respectively, and bd is a roughness parameter that controls how closely the true utility function is expected to adhere to a linear form in dimension d [20]. The effect of this function is to assert that if x and \({\mathbf{x^{\prime}}}\) describe very similar, their utilities will be almost the same, and so the preference function varies smoothly as the health state changes. The key point about this model is that it allows \(d({\mathbf{x}})\) to take any values and hence the utility functions are not constrained in the way that they are with parametric regression models. It is in this sense that we describe our model as nonparametric, and we believe that this is another way in which our model is more realistic than that of previous analysis. For more details on this part of the model, see Kharroubi et al. [20].
Subsets of the US sample were selected using systematic random sampling. The sample of 10 US health states was chosen using systematic random sampling as follows: we first sorted the 42 US health states in increasing order, then, we selected 1 health state from the list at random. Every 4th health state from then on has been selected. The systematic random sampling method was adopted to make sure that each sampled health state is a fixed distance apart from those that surround it.
The sampling technique of the 15 US health states is similar selecting each 3rd health state, with a randomly selected health state as starting point. The sampling of the 20 US health states uses the same approach, but with each 2nd health state selected. The sample of 25 US health states was selected as above; that is, with every other health state being chosen starting from the random selection (baseline).
Given the overall aim of the models is to predict health state valuations, model performance is assessed using predictive ability, presented using plots of predicted to actual values, calculations of the mean predicted error, root mean squared error (RMSE) and plots of the standardized residuals.
Results
10 US health states
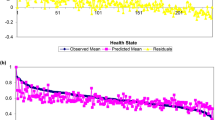
Column 2 of Table 1 displays the actual mean health state utility values of the US data. Columns 3 and 4 show the predicted mean health state utility values and standard deviation for the US population on its own, while columns 5 and 6 show the predicted population mean health state utility and standard deviation using the 10 health states valued in the US (in bold font) and UK data (which we shall refer to henceforth as US/UK). As can be seen, the predicted mean valuations ranged from − 0.3082 (33333) to 1 (11111) for the US and from − 0.3426 (33333) to 1 (11111) for the (US/UK) population. Figure 1 presents the estimated mean valuations (pink line) for the US population alone and the observed (blue line) along with the yellow line reflecting the difference between both values. Figure 2a presents the corresponding plots for US/UK population. As depicted in Fig. 2a, the predicted valuations by employing only ten health states from the US population, while adopting all the UK data do not fall in agreement with the observed US valuations. It also shows obvious fluctuations in the predicted US/UK valuations which in turn justifies the non-steady trend of the difference line. Additionally, the observed RMSE for the US population by itself is 0.0576, whereas the US/UK achieves a 0.1021, which is almost of double size. Based on these results, we believe that a sample of ten US health state is too little and hence more US states are required to get results that are in agreement with those attained with the complete US valuations.
15 US health states
Columns 7 and 8 of Table 1 show the estimated population mean valuations and standard deviation using the 15 health states valued in the US/UK (in bold font) data. The predicted mean valuations varied from − 0.3337 (33333) to 1 (11111) for the (US/UK) population. Figure 2b presents the estimated valuations (pink line) for the US/UK population and the observed mean valuations of the US population (blue line), along with the difference between the two valuations (yellow line). In comparison with Fig. 2a, the results presented in Fig. 2b show a little improvement, although there are still some fluctuations in the predicted US/UK valuations. This is also the case with RMSE of 0.0883 for the US/UK valuations compared to 0.0576 for the US only. This suggests that 15 US health states is still a small sample and hence more US states are required to get results that are in agreement with those attained with the complete US valuations.
20 US health states
Columns 9 and 10 of Table 1 show the estimated population mean valuations and standard deviation using the 20 health states valued in the US/UK (in bold font) data. The predicted mean valuations varied from − 0.3105 (33333) to 1 (11111) for the (US/UK) population. Figure 2c represents the estimated valuations (pink line) for the US/UK population and the observed mean valuations of the US population (blue line) as well as the difference between the two valuations (yellow line). We see from Fig. 2c that both valuations are very close for most of the 42 health states. In comparison with Fig. 1, the predicted valuations by employing only 20 health states from the US population while adopting all the UK data are in good agreement with those obtained with the full US sample. Additionally, the observed RMSE for the US/UK is 0.0665, which is very close to the one obtained using the US data only (0.0576). Based on these results, we believe a sample of 20 US health states in addition to the whole UK data might be sufficient to get results that are in quite good agreement with those attained with the complete US study.
25 US health states
To be more cautious, we take a step further and look at 25 US health states together with the 42 UK health states. This is to ensure we get good answers (or even better) as those obtained with the full US study. Columns 11 and 12 in Table 1 show the predicted population mean valuations and standard deviation using the 25 health states valued in the US/UK (in bold font) data. The predicted mean valuations varied from − 0.3242 (33333) to 1 (11111) for the (US/UK) population. Figure 2d represents the predicted valuations (pink line) for the US/UK population and the observed mean valuation of the US population (blue line). The yellow line represents their difference. We see from Fig. 2d that both valuations are very close for most of the 42 health states. In comparison with Fig. 1, the predicted valuations by employing 25 health states from the US population while adopting all the UK data are in perfect agreement. Additionally, the observed RMSE for the US/UK is 0.0554, which is very similar to the one obtained using the US data only (0.0576). This implies that a sample of 25 US health states in addition to the whole UK data is the ideal scenario needed to be adopted to obtain results that are in excellent agreement with those obtained with the full US sample.
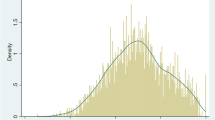
Another comparison of the two approaches is to conduct an out-of-sample prediction for the remaining health states that were included in the US valuation survey but not included in the model. Given that 25 US health states were used for model fitting, we make use of this model to predict for the remaining 17 health states. Table 2 displays the true sample means for these 17 missing states, together with the posterior means and standard deviations for these means in the (US/UK) as well as the US valuations only. It is clear that both estimated value sets are close to most of the health states. However, the predictive performance of the US/UK model is slightly better since the mean and variance of the standardized prediction errors are 0.275 and 0.443, respectively, for US/UK versus 0.3604 and 0.524 for the US only. Additionally, RMSE is slightly better as well, with 0.099 for the US/UK data and 0.1055 for the US only. The better predictions may be observed because the Bayesian model is able to borrow strength from the UK data (as informative priors), and as such better estimation of the US population utility function are obtained. For visual checking, Fig. 3 shows the standardized prediction errors in two Q–Q normal plots. Panel (a) plots the errors for estimating the 17 sample means using the US data only, while panel (b) shows the corresponding errors using the US/UK data. In each case, the solid line represents the theoretical N (0,1) distribution. In theory, we would expect the quantiles of the standardized predictive errors to lie roughly on the theoretical line, i.e. have the same distribution. It is clear that the both predictions are pretty similar though the combined analysis is slightly better. This implies that the results obtained are in line with our hypothesis and that there is no need to adopt more than 25 health states from the US data to obtain the results we are seeking in health state valuation studies.
Discussion
Here we have applied a nonparametric Bayesian method to the existing US–UK EQ-5D valuations in an attempt to determine what size sample in the US EQ-5D health states, while also borrowing extra strength from the UK data, is needed to get answers that are as well as those attained with the full US study. We have shown that, with the increased number of states considered, we were able to develop a higher accuracy of the results obtained for all criteria used, including predicted versus actual mean health state valuations, mean predicted error, root mean square error and an out-of-sample prediction. Furthermore, we have concluded that a sample of 25 (or even 20) US health states as well as the whole UK data is the ideal scenario needed to be adopted to obtain results that are in excellent agreement with those obtained with the full US sample, based on predictive ability of the models. This is a promising approach that suggests that existing preference data could be combined with a small valuation study in a new country to generate preference weights, making own country value sets more achievable for LMIC.
The novelty of the analysis presented here was to use the pooled data when we have a large quantity of observations on one country and limited observations on another. In the analysis presented here, we have shown that drawing extra information from the first country allows us to reduce the sample size in the second country, and for this to attain the same precision as we would obtain with a complete data in that country. This kind of analysis could be extremely important in countries without the same ability to conduct large evaluation studies.
The nonparametric Bayesian model offers a major added advantage. In the existence of lots of observations on one country and limited on another, it permits the utilization of results of country 1 to improve the results of country 2, and as such generated utility estimates of the second country may be better than would have been the case if that country’s data were collected and analysed on its own. This in turn would reduce the need for undertaking large surveys in every country using costly and more often time-consuming face-to-face interviews with techniques such as SG and TTO. To our knowledge, this concept has not been investigated properly yet, but clearly it has a lot of potential value. Further research is underway to assess this.
Limitations of this study include the use of only two datasets as a case study. Value sets can differ across countries both in terms of the ordering of health states due to differences in relative preferences of the dimensions, and the location of states on the 1–0 full health–dead scale. Different population compositions, types of work, cultures and languages can all have an impact, suggesting that this approach may not always produce accurate estimates. The UK and US populations have different population compositions, yet may be more culturally similar than, for example, high-income and low-income countries. This approach may be of most benefit where the samples that are combined have cultural similarities, as in the case of the UK and US. This approach could be used by LMIC to combine resources to generate value sets for each individual country generated by combining data collected across different countries with cultural similarities. The accuracy of estimates may not be at an acceptable level for countries where there may be larger differences in their health valuations to the larger country whose data are modelled alongside. Further research is encouraged to examine whether this approach is appropriate using countries which have greater cultural differences, where relative preferences across different dimensions may differ leading to a different ordering of mean valuations of health states. This will be useful for informing under what circumstances one country’s values may be qualified to be modelled alongside the country of interest to generate their value set. In addition, the location of dead may be a limiting factor, where even if the ordering of states is similar there may be differences in where these states are located on the 1–0 full health–dead scale. Further research is underway to assess this. In particular, ongoing research on exploring whether using the UK data might help with the design and analysis of a valuation study for SF-6D in Hong Kong has preliminary results that are very promising.
One limitation of the approach used to select health states is that the selection was not restricted to the subsample of states valued by a small sample of people. In the US study, there were five groups that each valued a different set of states, and hence here states could have been selected using one group alone, two groups, and then three groups. However, this should not impact on the results since if new data were being collected with the aim of being analysed using the Bayesian approach reported here, health state selection could be informed by these analyses.
An additional limitation is that the approach does not explore whether the same results could have been achieved through keeping the same number of health states and reducing the sample size. However, it is not anticipated that this would impact on the results though this can be explored in future research. Furthermore, the Bayesian nonparametric value sets reported here differ from parametric value sets generated for the EQ-5D that are commonly used to generate QALYs [17, 18] though it is possible that a similar approach could be used to generate parametric estimates.
Furthermore, as many international agencies recommend the use of country own value sets to generate QALYs, it is unclear whether a value set generated using own country data modelled alongside another country’s dataset would be acceptable. However, this may not be a concern if the estimates are accurate and the ordering of health states and location on the 1–0 full health–dead scale is similar to those achieved using a large-scale valuation study.
In conclusion, the simple idea of pooling the US and UK data proves to be significant in terms of reducing the need for EQ-5D to be valued separately in each country. The model used in this article could be applied to other preference-based measures such as SF-6D, 15D and HUI-II, in addition to disease-specific measures where this approach could be particularly promising. Further research is underway to apply this to SF-6D.
References
Drummond, M.F., Sculpher, M., O’Brien, B., Stoddart, G.L., Torrance, G.W.: Methods for the economic evaluation of health care programmes. Oxford Medical Publications: Oxford (2005)
Brooks, R.: EuroQol: the current state of play. Health Pol. 37, 53(72 (1996). https://doi.org/10.1016/0168-8510(96)00822-6
Torrance, G.W., Feeny, D.H., Furlong, W.J., et al.: Multi-attribute utility function for a comprehensive health status classification system: health utilities index mark 2. Med. Care. 34(7), 702–722 (1996). https://doi.org/10.1097/00005650-199607000-00004
Feeny, D.H., Furlong, W.J., Torrance, G.W., et al.: Multi-attribute and single-attribute utility function for the health utility index mark 3 system. Medical care 40(20), 113(128 (2002)
Hawthorne, G., Richardson, G., Atherton_Day, N.: A comparison of the assessment of quality of life (AQoL) with four other generic utility instruments. Ann. Med. 33, 358–370 (2001). https://doi.org/10.3109/07853890109002090
Kaplan, R.M., Anderson, JP: A general health policy model: update and application. Health Serv. Res. 23, 203–235 (1988)
Brazier, J.E., Roberts, J., Deverill, M.: The estimation of a preference based measure of health from the SF-36. J. Health Econ. 21, 271(292 (2002). https://doi.org/10.1016/S0167-6296(01)00130-8
Rowen, D.L., Brazier, J., Ara, R., Azzabi Zouraq, I.: The role of condition-specific preference-based measures in health technology assessment. PharmacoEconomics 35(Suppl 1), 33–41 (2017)
Badia, X., Roset, M., Herdman, M., et al.: A comparison of United Kingdom and Spanish general population time trade-off values for EQ-5D health states. Med. Decis. Making. 20, 7–16 (2001). https://doi.org/10.1177/0272989X0102100102
Johnson, J.A., Luo, N., Shaw, J.W., et al.: Valuations of EQ-5D Health States: are the United States and United Kingdom different. Med. Care. 43, 221–228 (2005). https://doi.org/10.1097/00005650-200503000-00004
Rowen, D.L., Azzabi Zouraq, I., Chevrou-Severac, H., van Hout, B.: International regulations and recommendations for utility data for health technology assessment. PharmacoEconomics 35(Suppl 1), 11–19 (2017)
Kharroubi, S.A., O’Hagan, A., Brazier, J.E.: A comparison of United States and United Kingdom EQ-5D health state valuations using a non-parametric Bayesian method. Stat. Med. 29, 1622–1634 (2010). https://doi.org/10.1002/sim.3874
Kharroubi, S.A., Brazier, J., McGhee, S.: A comparison of Hong Kong and United Kingdom SF-6D health states valuations using a non-parametric Bayesian method. Value Health. 17(4), 397–405 (2014). https://doi.org/10.1016/j.jval.2014.02.011 (PMid: 24969000).
Kharroubi, S.A.: A comparison of Japan and United Kingdom SF-6D health states valuations using a non-parametric Bayesian method. Appl. Health Econ. Pol. 13, 409–420 (2015). https://doi.org/10.1007/s40258-015-0171-8. (PMid: 25896874)
The EuroQol Group (1990) EuroQol—a new facility for the measurement of health-related quality of life. Health Policy 16(3), 199–208
Brazier, J.E., Ratcliffe, J., Tsuchiya, A., Solomon, J.: Measuring and valuing health for economic evaluation. Oxford University Press, Oxford (2007)
Dolan, P.: Modeling valuation for Euroqol health states. Med. Care 35, 351–363 (1997)
Shaw, J.W., Johnson, J.A., Coons, S.J.: US valuation of the EQ-5D health states: development and testing of the D1 valuation model. Med. Care 43(3), 203–220 (2005)
Patrick, D.L., Starks, H.E., Cain, K.C., Uhlmann, R.F., Pearlman, R.A.: Measuring preferences for health states worse than death. Med. Decis. Making 14, 9–18 (1994)
Kharroubi, S.A., O’Hagan, A., Brazier, J.E.: Estimating utilities from individual health state preference data: a nonparametric Bayesian approach. Appl. Stat. 54, 879–895 (2005). https://doi.org/10.1111/j.1467-9876.2005.00511.x
Acknowledgements
The leading author would like to thank the University Research Bureau (URB) at the American University of Beirut, Lebanon, for funding this study. The authors would particularly like to thank Prof. John E Brazier for all his continual support and useful guidance during their time working on this manuscript. This work was supported by American University of Beirut (103366).
Funding
This study was funded by the University Research Bureau (URB) at the American University of Beirut, Lebanon.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
This article does not contain any studies with human participants or animals performed by the authors.
Rights and permissions
About this article
Cite this article
Kharroubi, S.A., Rowen, D. Valuation of preference-based measures: can existing preference data be used to select a smaller sample of health states?. Eur J Health Econ 20, 245–255 (2019). https://doi.org/10.1007/s10198-018-0991-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10198-018-0991-1