Abstract
A condition-specific preference-based measure (CSPBM) is a measure of health-related quality of life (HRQOL) that is specific to a certain condition or disease and that can be used to obtain the quality adjustment weight of the quality-adjusted life-year (QALY) for use in economic models. This article provides an overview of the role and the development of CSPBMs, and presents a description of existing CSPBMs in the literature. The article also provides an overview of the psychometric properties of CSPBMs in comparison with generic preference-based measures (generic PBMs), and considers the advantages and disadvantages of CSPBMs in comparison with generic PBMs. CSPBMs typically include dimensions that are important for that condition but may not be important across all patient groups. There are a large number of CSPBMs across a wide range of conditions, and these vary from covering a wide range of dimensions to more symptomatic or uni-dimensional measures. Psychometric evidence is limited but suggests that CSPBMs offer an advantage in more accurate measurement of milder health states. The mean change and standard deviation can differ for CSPBMs and generic PBMs, and this may impact on incremental cost-effectiveness ratios. CSPBMs have a useful role in HTA where a generic PBM is not appropriate, sensitive or responsive. However, due to issues of comparability across different patient groups and interventions, their usage in health technology assessment is often limited to conditions where it is inappropriate to use a generic PBM or sensitivity analyses.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
A condition-specific preference-based measure (CSPBM) is a measure of HRQOL that is specific to a condition or disease that also has a set of preference weights that enable a health state utility value to be generated each time the measure is completed. |
CSPBMs have a useful role in health technology assessment (HTA) where a generic preference-based measure (generic PBM) is not appropriate, sensitive or responsive as they can provide appropriate health state utility values that capture change in that condition. |
Due to issues of comparability across different patient groups and interventions, the usage of CSPBMs in HTA is generally limited to interventions where it is inappropriate to use a generic PBM. |
1 What is a Condition-Specific Preference-Based Measure of Health?
This paper provides a definition of a condition-specific preference-based measure (CSPBM) of health or health-related quality of life (HRQOL) and critically examines its role in health technology assessment (HTA) and beyond. The paper provides an overview and summary of all existing CSPBMs, thus providing a resource of references for all CSPBMs across all conditions that have been derived in the literature. The paper also summarises available psychometric evidence on the performance of CSPBMs, and provides guidance on the advantages and disadvantages of using CSPBMs for HTA in comparison with generic preference-based measures (PBMs) such as the EQ-5D.
A CSPBM is a measure of HRQOL that is specific to a certain condition or disease and that also has a set of preference weights that enables a utility value to be generated from responses to the measure. Analogously to generic measures, a CSPBM consists of (1) items or questions that are typically completed by the patient to report their own health, (2) a classification system which is used to classify the self-reported health of the patient into a health state and (3) a value set that enables a utility value to be produced for every health state described by the classification system. CSPBMs typically include dimensions that are important for that condition but generally not important across all patient groups. Each CSPBM is unique and their content varies substantially. Some CSPBMs include a range of dimensions covering both generic and condition-specific aspects (e.g. a cancer-specific measure with dimensions of physical functioning, role functioning, pain, emotional functioning, social functioning, fatigue and sleep disturbance, nausea, and constipation and diarrhoea [2]), whereas others are focussed upon symptoms (e.g. a measure for flushing [a side effect of niacin medications] with dimensions of redness of skin, warmth of skin, tingling of skin, itching of skin, and difficulty sleeping [3]). Some CSPBMs are uni-dimensional and have several items relating to the same dimension (e.g. the measure for flushing [3]), whereas others are multi-dimensional (e.g. the measure for cancer [2]). CSPBMs can be developed from new, ‘de novo’, or can be derived from an existing condition-specific measure.
2 What is the Role of Condition-Specific Preference-Based Measures?
CSPBMs have a role in HTA where a generic PBM is not appropriate, or has poor psychometric performance in a condition or patient group, as they provide appropriate utility values under these circumstances. Where a generic PBM has been shown to perform poorly in terms of sensitivity or responsiveness (e.g. vision and hearing, severe and complex mental health problems and dementia, as discussed in Sect. 2), it is not expected that it will accurately capture the impact of an intervention on the HRQOL of the patient. For example, if a generic PBM has been shown to suffer from ceiling effects for a condition then an improvement in HRQOL following an intervention cannot be captured. In addition, a generic PBM may fail to capture all aspects of HRQOL that are important for that patient group. In contrast, CSPBMs are designed to capture the aspects of HRQOL that are important for that condition, and unlike a generic PBM this is likely to include symptoms, sometimes alongside more generic dimensions of HRQOL (e.g. a cancer-specific measure with dimensions of physical functioning, role functioning, pain, emotional functioning, social functioning, fatigue and sleep disturbance, nausea, and constipation and diarrhoea [2]).
In circumstances where a generic PBM has been shown to be appropriate for a condition, CSPBMs can be used in sensitivity analyses of the economic model to indicate how the use of the generic PBM, which although appropriate may be less sensitive or responsive to changes in health, may have impacted on incremental cost-effectiveness ratios.
CSPBMs have a role in HTA external to the economic model to demonstrate additional benefits that may not be captured by the generic PBM and provide additional supporting evidence. CSPBMs also have a wide role outside of economic evaluation where they can be used to compare health and treatment effects across different studies within a patient group. The inclusion of CSPBMs in a wide range of studies provide utility values that are relevant for that condition as they take into consideration the specific aspects of health that are important for that condition. These utility values can be reported alongside the detailed HRQOL data provided from the condition-specific measure that the CSPBM is derived from (e.g. reporting condition-specific EORTC QLQ-C30 HRQOL data alongside CSPBM data from the EORTC-8D for patients with prostate cancer [4]).
3 Development Issues
3.1 Development from an Existing Condition-Specific Measure
The advantage of deriving a PBM from an existing condition-specific measure is that the existing measure has already been used in many studies, and therefore existing datasets can be used to generate utility values. In addition, the existing measure is likely to have been validated and is likely to have evidence of good psychometric performance.
Figure 1 outlines the six-stage process developed by researchers at the University of Sheffield to derive a CSPBM from an existing condition-specific measure [1]. Stages I–IV derive the classification system and stages V–VI derive the value set for every health state described by the classification system. The classification system consists of multiple dimensions with typically one item to reflect that dimension, with several levels of severity.

Modified from Brazier et al. [1]
Six stages for deriving a condition-specific preference-based measure from an existing condition-specific (non-preference-based) measure
Stages I–IV derive the classification system using a combination of factor analysis, Rasch analysis and classical psychometric analysis. Factor analysis can be used to either confirm the dimensional structure of the existing condition-specific measure, to propose a different dimensional structure indicating where dimensions are not independent or where items within the same dimension capture different concepts [1], or to propose a dimension structure for the existing condition-specific measure that does not have one proposed by the instrument developer [5, 6]. Rasch analysis is a mathematical technique that enables qualitative data to be converted onto a continuous latent scale using a logit model [7, 8]. Classical psychometric analyses are used to indicate the performance of each item within each dimension and include floor and ceiling effects, correlation between items and dimensions, responsiveness over time and levels of missing data.
Stage I involves the derivation of the dimensions using a combination of factor analysis and the existing factor structure of the measure, and stage II uses Rasch analysis or item response theory and classical psychometric analysis to select the best item(s) to reflect each dimension in terms of coverage, ordering of levels, no differential item functioning across different groups, low floor and ceiling effects and good responsiveness. Stage III considers reducing the item levels to ensure that readers can accurately distinguish between each item level. Stage IV validates stages I–III, preferably on an independent dataset, to ensure the classification system has not been impacted on by the choice of dataset used to derive the classification system.
Stage V entails a valuation study typically with members of the general population to value a sample of health states, as it is generally not feasible to value all health states within the full classification system as typically there are too many. Stage VI involves regression analysis of the valuation data to produce a decrement from the reference level for every level of every dimension. This enables a utility value to be generated for every health state described by the classification system. Stages V and VI typically involve the same procedure as valuation of a generic PBM (see Sect. 2 for an overview). One additional challenge is that some CSPBMs may be uni-dimensional, or have a uni-dimensional component; for example, a CSPBM for flushing or common mental health problems. For uni-dimensional measures or components, valuation can be adapted to take this uni-dimensionality into consideration through the selection of health states for valuation using Rasch analysis, which does not require independence of items [3, 9].
At every stage, clinical input is used and often the instrument developer of the existing condition-specific measure is also involved. Some measures have also involved patients to ensure that the classification system includes all aspects that are important to patients (e.g. see [10]). Other measures have been developed using psychometric analyses on multiple existing condition-specific measures in order to select the best performing dimensions and items across these measures (e.g. [11]).
3.2 Developing a New Measure ‘De Novo’
The advantage of developing a new measure is that it does not have to be based on an existing condition-specific measure, as for some patient groups existing measures may not cover all important aspects of HRQOL. However, there will be no pre-existing evidence on the psychometric performance of the new measure, which can be important for some international agencies when they are examining the appropriateness of the usage of a CSPBM. It may therefore be necessary to establish the psychometric properties of the measure before it can be recommended for usage.
Developing a new measure involves a modification of the six-stage process. Guidelines for the development of dimensions and items for new measures are available from the US Food and Drug Administration (FDA) [12]. Patient involvement is emphasised at every stage of developing a classification system for a new measure, including both the generation and the validation of the content. Approaches in the literature include qualitative research with patients to identify dimensions, items and item wording, (e.g. [13]). The valuation of the measure is as described above in stages V and VI used to value a CSPBM derived from an existing condition-specific measure.
4 Description of Condition-Specific Preference-Based Measures
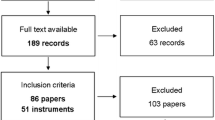
Papers developing CSPBMs either from existing condition-specific measures or ‘de novo’ that were published in English were identified using (1) a literature search conducted in December 2010 [1] and updated in March 2016 for the purpose of this paper and (2) a recent review of the literature [14]. Measures have been excluded that do not provide utility weights; that do not anchor utilities on the 1–0 full-health–dead scale; that derive utilities by mapping from a condition-specific measure to own utility values (as this is mapping, not a PBM). In total, 36 CSPBMs were identified across a range of 29 conditions. The CSPBMs are summarised in Table 1 and further details are provided in Appendix 3 (see electronic supplementary material, Table updated and modified from [63]).
5 Psychometric Properties of Condition-Specific Preference-Based Measures
5.1 Psychometric Performance of Condition-Specific Preference-Based Measures in Comparison with Existing Condition-Specific Measures
There is limited evidence comparing CSPBMs to the existing condition-specific measure they are derived from [1, 14]. However, evidence suggests largely comparable psychometric performance in terms of discrimination across severity groups and responsiveness to change over time between the existing condition-specific measure and CSPBMs for asthma, cancer, common mental health problems and overactive bladder [1].
5.2 Psychometric Performance of Condition-Specific Preference-Based Measures in Comparison with Generic Preference-Based Measures
There is limited evidence comparing CSPBMs and generic PBMs [1, 14]. However, evidence suggests that CSPBMs in asthma, cancer, common mental health problems and overactive bladder offer an advantage for measuring milder health states, and are less prone to ceiling effects than the EQ-5D [1]. The ceiling effects of EQ-5D have been widely reported in the general literature examining the performance of EQ-5D (see for example [41]), and therefore for patients with mild health problems CSPBMs may be more likely to provide a more accurate measurement of HRQOL and capture change in HRQOL. The evidence also suggests that these CSPBMs and a measure in vision better discriminated across severity groups than the generic PBM they were compared with [1, 42,43,44]. It is recommended that the psychometric properties of any CSPBM are examined prior to their usage to inform HTA, and preferably compared with a generic PBM to confirm where they offer an advantage.
Mean change over time and differences in utility values between different severity groups have been found to be smaller for CSPBMs than generic PBMs, with smaller standard deviation, in particular in comparison with EQ-5D [1] (although this may not always be the case [43, 45]). Any differences may impact on incremental cost-effectiveness ratios, and may potentially impact upon whether interventions are considered cost effective. However, research in this area has been limited to a small number of datasets on a small number of conditions, CSPBMs and generic PBMs, and the existing published evidence is unlikely to be representative across all CSPBMs. Further research in this area is encouraged.
6 Selecting a Measure for Economic Evaluation
Recent ISPOR taskforce guidance provides a framework for researchers considering the collection of utility data for HTA [46]. An important consideration is the appropriateness of the measure for the condition and population, and the choice will also depend on the requirements of the agency to which the economic evaluation will be submitted (see [47]). However, an important consideration is whether to use a generic PBM or a CSPBM. Table 2 outlines the advantages and disadvantages of generic PBMs and CSPBMs with reference to different criteria: completion of the measure by the patient, psychometric performance, HRQOL coverage, issues with the valuation process used to elicit the utility values and comparability of values for use in HTA.
Overall, CSPBMs offer the advantages of lower patient burden for completion, they are more relevant to the patient, are less likely to suffer from ceiling effects, and the existing condition-specific measures they are derived from are typically sensitive and responsive. However, there are disadvantages in that they may not be able to capture the impact of all side effects and comorbidities, their elicited utility values may be prone to exaggeration from focussing effects, the values they generate are not directly comparable across different conditions, and they are not accepted in the base-case cost-effectiveness analyses by many international agencies.
It is important to note that the advantages and disadvantages of CSPBMs vary both by the exact measure and the patient group it is administered to. The content of CSPBMs varies widely, where for example a CSPBM in cancer [2, 10] may be perceived as more generic in its dimensions, and could even have ‘bolt-on’ dimensions for certain cancers, whereas other CSPBMs such as for flushing are uni-dimensional [3]. It is also important to note that the psychometric performance of measures differs across patient groups, and hence a measure that is appropriate for use in some patient groups is not necessarily appropriate in all patient groups.
Generic PBMs have the advantage that they offer comparability across patient groups and interventions, have no issues in their valuation and can arguably capture comorbidities where these occur in the generic dimensions of HRQOL. However, they may not be responsive or sensitive and suffer from ceiling effects, and may not be relevant to the patient and potentially increase patient burden where they are included in addition to the condition-specific measures that are included for multiple reasons unrelated to populating the economic model.
It has been argued that CSPBMs can provide utility values that are comparable to generic PBMs as they can be derived using the same methodology as a generic PBM (e.g. a large number of CSPBMs have been derived using a time trade-off interview with the UK general population as also used by the EQ-5D UK value set), and utility values are anchored on a comparable 1–0 full-health–dead scale required to generate QALYs. However, there remains the issue of the differences in descriptive systems, and issues in the valuation of CSPBMs due to labelling the condition (disease labelling of health states can impact on elicited values [48]) and focussing effects (respondents focus only on the areas of HRQOL mentioned and exaggerate their importance) that may mean that there are important underlying issues of comparability. For this reason, to enable comparability in HTA conducted across interventions and patient groups a generic PBM is typically recommended for use in base-case analyses, and a CSPBM is typically only recommended where evidence demonstrates a generic PBM is inappropriate (see for example prescriptive guidance by NICE [49]), or for use alongside a generic PBM in sensitivity analyses.
7 Summary
The paper provides an overview and summary of all existing CSPBMs, providing a resource for researchers. There are a large number of CSPBMs across a wide range of conditions, and the coverage of these measures varies from covering a wide range of dimensions to more symptomatic or uni-dimensional measures. CSPBMs have a useful role in HTA where a generic PBM is not appropriate, sensitive or responsive. Due to issues of comparability across different patient groups and interventions, their usage in HTA is typically limited to conditions where it is inappropriate to use a generic PBM, or in sensitivity analyses. Widespread use of CSPBMs rather than generic PBMs in HTA would reduce comparability of evaluations of interventions across different patient groups. For this reason CSPBMs are not recommended as a common replacement for generic PBMs, rather they offer important evidence alongside generic PBMs or where generic PBMs are inappropriate. Evidence suggests that CSPBMs offer an advantage in more accurate measurement of milder health states. However, CSPBMs can fail to capture comorbidities and all side effects. Mean change and standard deviation can differ from generic PBMs, and this may impact on incremental cost-effectiveness ratios.
References
Brazier JE, et al. Developing and testing methods for deriving preference-based measures of health from condition-specific measures (and other patient-based measures of outcome). Health Technol Assess. 2012;16(32):1–113.
Rowen D, et al. Deriving a preference-based measure for cancer using the EORTC QLQ-C30. Value Health. 2011;14(5):721–31.
Young TA, et al. Developing preference-based health measures: using Rasch analysis to generate health state values. Qual Life Res. 2010;19(6):907–17.
Lloyd A, et al. Health-related quality of life and health utilities in metastatic castrate-resistant prostate cancer: a survey capturing experiences from a diverse sample of UK patients. Value Health. 2015;18:1152–7.
Young T, et al. The first stage of developing preference-based measures: constructing a health-state classification using Rasch analysis. Qual Life Res. 2009;18(2):253–65.
Stevens KJ, et al. The development of a preference-based measure of health in children with atopic dermatitis. Br J Dermatol. 2005;153(2):372–7.
Rasch G. Probabilistic models for some intelligence and attainment tests. Chicago: University of Chicago Press; 1960.
Tesio L. Measuring behaviours and perceptions: Rasch analysis as a tool for rehabilitation research. J Rehabil Med. 2003;35(3):105–15.
Mavranezouli I, et al. Estimating a preference-based index from the clinical outcomes in routine evaluation-outcome measure (CORE-OM): valuation of CORE-6D. Med Decis Mak. 2013;33(3):381–95.
King MT, Costa DSJ, Aaronson NK, Brazier JE, Cella DF, Fayers PM, Grimison P, Janda M, Kemmler G, Norman R, Pickard AS, Rowen D, Velikova G, Young TA, Viney R. QLU-C10D: a health state classification system for a multi-attribute utility measure based on the EORTC QLQ-C30. Qual. Life Res. 2016;25(3):625–36.
Mukuria C, et al. Deriving a preference-based measure for myelofibrosis from the EORTC QLQ-C30 and the MF-SAF. Value Health J Int Soc Pharmacoecon Outcomes Res. 2015;18(6):846–55.
(FDA), U.D.o.H.a.H.S.F.a.D.A. Guidance for industry: patient-reported outcome measures: use in medical product development to support labeling claims. Maryland: FDA; 2009.
Palfreyman S. The SPVU-5D: a preference-based measure of health related quality of life for use with venous leg ulceration. PRO Newsletter, 2012 (45 (Spring Issue)).
Goodwin E, Green C. A systematic review of the literature on the development of condition-specific preference-based measures of health. Appl Health Econ Health Policy. 2016;14:161–83.
Beusterien K, et al. Integrating preferences into health status assessment for amyotrophic lateral sclerosis: the ALS Utility Index. Amyotroph Lateral Scler Other Motor Neuron Disord. 2005;6(3):169–76.
Versteegh MM et al. Condition-specific preference-based measures: benefit or burden? Value Health. 2012 (Forthcoming).
Young T, et al. The use of rasch analysis in reducing a large condition-specific instrument for preference valuation: the case of moving from AQLQ to AQL-5D. Med Decis Mak. 2011;31(1):195–210.
Yang Y, et al. Estimating a preference-based index for a 5-dimensional health state classification for asthma derived from the Asthma Quality of Life Questionnaire. Med Decis Mak. 2011;31:281–91.
Norman R, Viney R, Aaronson NK, Brazier JE, Cella D, Costa DSJ, Fayers PM, Kemmler G, Peacock S, Pickard AS, Rowen D, Street D, Velikova G, Young TA, King MT. Using a discrete choice experiment to value the QLU-C10D: feasibility and sensitivity to presentation format. Qual. Life Res. 2016;25(3):637–49.
Kularatna S, et al. Development of an EORTC-8D utility algorithm for Sri Lanka. Med Decis Mak. 2015;35(3):361–70.
Petrillo J, Cairns J. Development of the EXACT-U: a preference-based measure to report COPD exacerbation utilities. Value Health. 2011;14:546–54.
Mavranezouli I, et al. Using Rasch analysis to form plausible health states amenable to valuation: the development of the CORE-6D from a measure of common mental health problems (CORE-OM). Qual Life Res. 2011;20(3):321–33.
Rowen D, et al. Estimating preference-based single index measures for dementia using DEMQOL and DEMQOL-Proxy. Value Health. 2012;15:346–56.
Mulhern B, et al. Improving the measurement of QALYs in Dementia: developing patient- and carer-reported health state classification systems using Rasch analysis. Value Health. 2012;15:323–33.
Mulhern B, Rowen D, Brazier J, Smith S, Romeo R. Development of DEMQOL-U and DEMQOL-PROXY-U: generation of preference-based indices from DEMQOL and DEMQOL-PROXY for use in economic evaluation. Health Technol Assess. 2013;17(5).
Sundaram M, et al. Estimation of a valuation function for a diabetes mellitus-specific preference-based measure of health the diabetes utility index (R). Pharmacoeconomics. 2010;28(3):201–16.
Sundaram M, et al. Rasch analysis informed the development of a classification system for a diabetes-specific preference-based measure of health. J Clin Epidemiol. 2009;62(8):845–56.
Mulhern B, et al. The development of a QALY measure for epilepsy: NEWQOL-6D. Epilepsy Behav E&B. 2012;24(1):36–43.
Stolk EA, Busschbach J. Validity and feasibility of the use of condition-specific outcome measures in economic evaluation. Qual Life Res. 2003;12(4):363–71.
Kerr C, et al. Developing a utility index for the Aberrant behavior checklist (ABC-C) for fragile X syndrome. Qual Life Res. 2015;24:305–14.
Kind P, Macran S. Eliciting social preference weights for functional assessment of cancer therapy-lung health states. PharmacoEconomics. 2005;23(11):1143–53.
Lamers LM, Uyl-de Groot CA, Buijt I. The use of disease-specific outcome measures in cost-utility analysis: The development of Dutch societal preference weights for the FACT-L scale. PharmacoEconomics. 2007;25(7):591–603.
Brazier JE, et al. Estimating a preference-based index for a menopause specific health quality of life questionnaire. Health Qual. Life Outcomes. 2005;3:13.
Yang Y, et al. Estimating a preference-based single index from the overactive bladder questionnaire. Value Health. 2009;12(1):159–66.
Choiu CF, et al. Development of the multi-attribute Paediatric Asthma Health Outcome Measure (PAHOM). Int J Qual Health Care. 2005;17(1):23–30.
Palmer CS, et al. Patient preferences and utilities for ‘off-time’ outcomes in the treatment of Parkinson’s disease. Qual Life Res. 2000;9(7):819–27.
Tomlinson G, et al. Development and validation of a utility weighting function for the patient-oriented prostate utility scale (PORPUS). Med Decis Mak. 2012;32(1):11–30.
Krahn MR. Construction of the Patient-Oriented Prostate Utility Scale (PORPUS): A multiattribute health state classification system for prostate cancer. J Clin Epidemiol. 2000;53(9):920–30.
McKenna SP, et al. Development and validation of a preference based measure derived from the Cambridge Pulmonary Hypertension Outcome Review (CAMPHOR) for use in cost utility analyses. Health Qual Life Outcomes. 2008;6:65.
Montejo AL, et al. Estimation of a multiattribute utility function for the Spanish Version of the TooL Questionnaire. Value Health. 2011;14:564–70.
Bharmal M, Thomas J. Comparing the EQ-5D and the SF-6D descriptive systems to assess their ceiling effects in the us general population. Value Health. 2006;9(4):262–71.
Finger RP, et al. Evaluation of a vision-related utility instrument: the German Vision and Quality of Life Index. Invest Ophthalmol Vis Sci. 2013;54:1289–94.
Desroziers K, et al. Estimating EQ-5D and OAB-5D health state utilities for patients with overactive bladder. Health Qual Life Outcomes. 2013;11:9.
McTaggart-Cowan HM, et al. The validity of generic and condition-specific preference-based instruments: the ability to discriminate asthma control status. Qual Life Res. 2008;17(3):453–62.
Hatswell AJ, Pennington B, Pericleous L, Rowen D, Lebmeier M, Lee D. Patient-reported utilities in advanced or metastatic melanoma, including analysis of utilities by time to death. Health Qual Life Outcomes. 2014;12(1):140.
Wolowacz S, et al. Estimating health-state utility for economic models in clinical studies: an ISPOR good research practices task force report. Value Health. 2016;19:704–19.
Brazier J, et al. A review of generic preference-based measures for use in cost-effectiveness models. PharmacoEconomics. 2017. doi:10.1007/s40273-017-0545-x.
Rowen D, et al. It’s all in the name, or is it? The impact of labelling on health state values. Med Decis Mak. 2012;32(1):31–40.
NICE; National Institute of Health and Care Excellence. Guide to the methods of technology appraisal. London: NICE; 2013.
Longworth L, et al. Use of generic and condition-specific measures of health-related quality of life in NICE decision-making: a systematic review, statistical modelling and survey. Health Technol Assess. 2014;18(9):1–224.
Brazier J, Tsuchiya A. Preference-based condition-specific measures of health: what happens to cross programme comparability? Health Econ. 2010;19:125–9.
Rowen D, et al. International regulations and recommendations for utility data for health technology assessment. PharmacoEconomics. 2017. doi:10.1007/s40273-017-0544-y.
Scholzel-Dorenbos CJM, et al. Validation study of the prototype of a disease-specific index measure for health-related quality of life in dementia. Health Qual Life Outcomes. 2012;10:11.
Arons AMM, et al. A simple and practical index to measure dementia-related quality of life. Value Health. 2016;19:60–5.
Goodwin E, Green C. A quality-adjusted life-year measure for multiple sclerosis: developing a patient-reported health state classification system for a multiple sclerosis-specific preference-based measure. Value Health J Int Soc Pharmacoecon Outcomes Res. 2015;18(8):1016–24.
Ratcliffe J, et al. Using DCE and ranking data to estimate cardinal values for health states for deriving a preference-based single index from the sexual quality of life questionnaire. Health Econ. 2009;18(11):1261–76.
LLoyd A, et al. Economic evaluation in short bowel syndrome (SBS): an algorithm to estimate utility scores for a patient-reported SBS-specific quality of life scale (SBS-QoL(TM)). Qual Life Res. 2014;23:449–58.
Brazier JE, et al. Estimation of a preference-based index from a condition-specific measure: the King’s health questionnaire. Med Decis Mak. 2008;28(1):113–26.
Cuervo J, et al. Development of the Incontinence Utility Index: estimating population-based utilities associated with urinary problems from the Incontinence Quality of Life Questionnaire and Neurogenic Module. Health Qual Life Outcomes. 2014;12:147.
Kok ET, et al. The valuation of the International Prostate Symptom Score (IPSS) for use in economic evaluations. Eur Urol. 2002;42:491–7.
Misajon R, et al. Vision and quality of life: the development of a utility measure. Invest Ophthalmol Vis Sci. 2005;46(11):4007–15.
Kowalski JW, et al. Rasch analysis in the development of a simplified version of the national eye institute visual-function questionnaire-25 for utility estimation. Qual Life Res. 2011 (Forthcoming).
Rowen D, Brazier JE. Multi-attribute utility instruments: condition-specific versions. In: Culyer AJ, editor. Encyclopaedia of health economics. San Diego: Elsevier; 2014. P. 358–365.
Yang Y, et al. Estimating a preference-based index for a 5-dimensional health state classification for asthma derived from the asthma quality of life questionnaire. Med Dec Mak. 2011;31(2):281–91.
Rowen D, et al. Estimating preference-based single index measures for dementia using DEMQOL and DEMQOL-Proxy. Value Health J Int Soc Pharmacoecon Outcomes Res. 2012;15(2):346–56.
Peacock S, et al. Vision and quality of life: development of methods for the VisQoL vision-related utility instrument. Ophthalmic Epidemiol. 2008;15(4):218–23.
Rentz AM, et al. Development of a preference-based index from the national eye institute visual function questionnaire-25. JAMA Ophthalmol. 2014;132:310–8.
Acknowledgements
The authors would like to thank Prof. Jon Karnon, PhD, of The University of Adelaide and Dr Andrew Lloyd, PhD, of Bladen Associates Ltd for their editorial review.
Author information
Authors and Affiliations
Contributions
DR reviewed the literature and wrote the first draft of the manuscript and subsequent versions. JEB, RA and IA contributed to draft and final versions of the manuscript.
Corresponding author
Ethics declarations
Funding
This study was funded by an unrestricted grant from Takeda Pharmaceuticals International AG.
Conflict of interest
Ismail Azzabi Zouraq is employed by Takeda Pharmaceuticals International AG. Donna Rowen, John Brazier and Roberta Ara have no conflicts of interest.
Disclosure statement
This article is published in a special edition journal supplement wholly funded by Takeda Pharmaceutical International AG, Zurich, Switzerland.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Rowen, D., Brazier, J., Ara, R. et al. The Role of Condition-Specific Preference-Based Measures in Health Technology Assessment. PharmacoEconomics 35 (Suppl 1), 33–41 (2017). https://doi.org/10.1007/s40273-017-0546-9
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40273-017-0546-9