Abstract
Background
Genetic nephrotic syndrome is caused by pathogenic variants in genes encoding proteins necessary for the stability and functionality of the glomerular filtration barrier. To date, more than 70 genes associated with steroid-resistant nephrotic syndrome have been identified.
Summary
We review the clinical and molecular aspects of genetic nephrotic syndrome with a particular focus on genes associated with slit membrane and podocyte cytoskeleton defects. Sanger sequencing and next-generation sequencing are widely used in the identification of novel gene variants and help us gain a better understanding of the disease. Despite these findings, therapy is mainly supportive and focused on the reduction of proteinuria and management of chronic kidney disease with an unfavorable outcome for a significant proportion of cases. Positive therapeutic effects of immunosuppressive drugs have been reported in some patients; however, their long-time administration cannot be generally recommended.
Conclusion
Personalized treatment based on understanding the distinct disease pathogenesis is needed. With this, it will be possible to avoid harmful immunosuppressive therapy and improve outcomes and quality of life for pediatric patients suffering from genetic nephrotic syndrome.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Nephrotic syndrome (NS) in children is a group of disorders characterized by nephrotic proteinuria (> 200 mg/mmol), hypoalbuminemia (< 30 g/l), edema, and hyperlipidemia [1]. It is caused by disruption of the glomerular filtration barrier integrity. This barrier is composed of three major components: fenestrated endothelium, glomerular basal membrane, and epithelial layer of podocytes [2]. Podocytes are differentiated epithelial cells which have long foot processes called pediceles that enwrap the glomerular capillaries. There is a special cell–cell junction called the slit diaphragm bridging the foot processes. This membrane contains many important proteins which are fundamental for the proper function of the barrier. Podocyte effacement with the loss of its architecture leads to pathological proteinuria (Fig. 1) [2]. Heavy urinary protein loss leads to significant hypoalbuminemia, hypogammaglobulinemia, and decreasing level of antithrombin III resulting in the risk of thromboembolic complications and severe bacterial infections (peritonitis, respiratory infections, sepsis). NS is classified based on response to steroid therapy, as steroid sensitive NS (SSNS) and steroid resistant NS (SRNS). Most patients are steroid sensitive (around 80%) and go into remission from proteinuria within 4–6 weeks of steroid administration [3]. The absence of complete remission in this time frame is characteristic for SRNS. Therapeutic response to steroids is the main determinant of the outcome for children with NS. Overall, the prognosis for SSNS is quite favorable in the majority of cases; however, half of all patients relapse frequently and need prolonged treatment with corticosteroids and/or other immunosuppressants [4]. On the other hand, steroid resistance is associated with a worse prognosis. It is known that more than 50% of children with SRNS progress to end-stage kidney disease (ESKD) within 15 years [3]. Based on the age of detection, congenital NS (CNS) (0–3 months), infantile NS (3 months to 1 year), and childhood onset (> 1 year) can be differentiated [5]. NS is rare with an incidence of 2–7:100 000 children with regional variability and it can affect children of any age. According to the etiology, NS is divided into primary and secondary types (secondary is caused by infections, medication or identifiable systemic or renal diseases) [6]. Most cases of primary NS are accounted for by idiopathic NS with unknown pathogenesis. It has been hypothesized for decades that immune dysregulation (both T and B cells) plays an important role in disease development. There is also a theory of systemic circulating factors leading to NS; however, the causative molecule has not been found yet [5]. There is a minor group of patients with primary NS due to causal pathogenic variant/variants in a gene that affects the stability and function of the filtration barrier [6]. The causes of monogenic NS will be reviewed in our paper with special focus on genes responsible for the proper structure and function of the podocyte slit membrane and cytoskeleton [5].
a Image of glomerulus in physiological condition and location of genes which encode proteins of slit diaphragm or proteins essential for function or structure of podocytes. b Image of glomerulus in genetic nephrotic syndrome with mutations of these genes. Mutations lead to collapsing of podocytes and defective slit diaphragm that leads to pathologic albuminuria (adapted from Ebefors et al.) [45]
Genetic causes of nephrotic syndrome
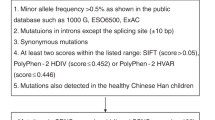
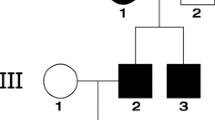
Monogenic NS represents a significant proportion of pediatric SRNS (10–40%) depending on regional variability and whether or not syndromic NS are included [7, 8]. Identification of the etiology of genetic NS is important as this absolutely influences the course of the disease and prognosis. It is essential in predicting posttransplant disease recurrence and also in selecting a kidney donor [9]. Medical history focused on renal and extrarenal features of SRNS for the child and his family members is the first step in the diagnosis along with physical examination of the patient with special attention paid to extrarenal signs of SRNS. Generally, a renal biopsy cannot distinguish between genetic and non-genetic forms of NS; however, the most common histological findings in genetic forms are focal segmental glomerulosclerosis (FSGS) or diffuse mesangial sclerosis (DMS) [10]. Genetic testing includes Sanger sequencing of single genes or next-generation sequencing (NGS), which includes multigene panel testing, whole exome sequencing (WES), and whole genome sequencing (WGS)). While Sanger sequencing is a preferred method for patients with highly suggestive phenotypes, the NGS with higher diagnostic yield is used in patients with nonspecific presentation. The NGS has significant technical advantages over Sanger testing (cheaper and much faster methods for sequencing of gene panels, whole exome or genome). Moreover, WES and WGS have the potential to identify causal variants in novel genes. On the other hand, Sanger sequencing is more accurate; therefore, this method verifies the gene variant detected by NGS analysis [11]. Indications for molecular genetic testing for children with NS are summarized in Table 1. Ideally, genetic examination in children with CNS and INS should be performed prior to the initialization of immunosuppressive therapy [10]; however, it usually takes more time in a routine clinical practice. Of note, there is a negative correlation between the likelihood of finding the causative variants and the age of NS presentation (Table 2).
Overview of genes encoding proteins of the slit diaphragm and podocyte cytoskeleton
Although the scientific community suspected a possible genetic basis for some forms of NS for a long time before the nineties, the first gene NPHS1 was described in 1998 as a genetic cause of CNS of the Finnish type [12]. So far, over 70 genes associated with genetic SRNS have been identified [13]. It is useful to divide the causal variants of genes associated with NS into groups based on the function of the encoded proteins. Various proteins in the podocyte are affected including slit membrane structures, podocyte cytoskeleton components, glomerular basement membrane elements, nuclear transcription factors, mitochondrial proteins, lysosomal enzymes, and others [9]. NPHS2, WT1, and NPHS1 represent the most common genes associated with SRNS [8, 14]. Causal variants of these genes along with LAMB2 are responsible for > 80% of CNS. On the other hand, pathogenic variants in INF2, TRPC6, and the genes associated with Alport syndrome are the main cause of adult onset NS [15]. Based on current recommendations, discontinuation of ineffective immunosuppressive therapy in children with genetic SRNS and continuing renin–angiotensin–aldosterone system inhibitors (RAASi) are recommended. Interestingly, 35% of the children with genetic SRNS go into partial or full remission on immunosuppressive therapy with calcineurin inhibitors (CNI), which were found to stabilize the cytoskeleton of podocytes [16]. Therefore, in children with partial or full response to CNI therapy, the decision to continue or discontinue immunosuppressive therapy should be made after parental counseling on a case by case basis. In some cases, such as patients with causal variants in genes involved in coenzyme Q10 (Co Q10) biosynthesis, a genetic finding can help determine individualized treatment. These patients benefit from CoQ10 supplementation, which significantly decreases proteinuria and preserves kidney function in affected individuals [17]. Unfortunately, in the majority of cases, individualized treatment has not been developed yet and these patients remain on existing treatments. This therapy could be ineffective and the patients undergo renal transplantation with insignificant risk of disease recurrence (negligible risk of post-transplant recurrence of nephrotic syndrome in patients with genetic SRNS compared with around 50% of patients with non-genetic idiopathic forms of SRNS) [18]. Dialysis is used to replace kidney function before transplantation in the majority of children. Only some children with the pathogenic NPHS1 gene (homozygotes for Fin-major mutation) are at risk of disease recurrence. The complete summary of the SRNS management is reviewed in IPNA clinical practice recommendations published in 2020 [19]. Our review outlines clinical features and current treatment options for patients with genetic NS associated with slit membrane and cytoskeleton defects. The course of the disease depends on the affected gene in a patient and phenotypic disease manifestations differ in individuals with different causal variants in the same gene [9]. Most clinically significant genes are reviewed here in detail.
NPHS1
NPHS1 gene is localized on chromosome 19 and encodes protein called nephrin, an essential component of a slit diaphragm, which has a crucial role in signaling pathways with other proteins of podocytes. Pathogenic variants associated with CNS were first described in 1998 by Kestilä et al. [12] The two most common variants in NPHS1 gene leading to the disruption of nephrin synthesis have been described: Fin-major and Fin-minor. Variants in NPHS1 are responsible for 90% cases of autosomal-recessive CNS in Finland and for around 30% of cases in other countries. More than 200 NPHS1 pathogenic variants with variable clinical pictures have been identified to date [20,21,22]. Diagnosis is sometimes suspected early if prenatal screening captures a significantly enlarged placenta due to proteinuria in the fetus as well as an increased maternal serum alpha-fetoprotein concentration (secondary effect of proteinuria). These children are often born prematurely with a low birth weight [23]. A typical clinical manifestation is generalized edema either at birth or shortly afterward. Affected individuals develop ESKD in early childhood. It is not necessary to perform a renal biopsy to confirm the diagnosis [20]. Kidney histology is not specific and reveals dilatation and microcystic formation of proximal tubules and mesangial matrix expansion of glomeruli. Tubular atrophy occurs later with sclerosis of glomeruli [24].
Some patients with the pathogenic NPHS1 gene responded to immunosuppressive therapy [16]; however, due to severe hypogammaglobulinemia inducing high susceptibility to bacterial infections, such treatment could be injurious. Current scientific evidence suggests using symptomatic treatment, the same for patients with other genetic forms of SRNS. Albumin infusions are administered to maintain adequate intravascular volume, but the indication should be based on clinical indicators of hypovolemia, not on serum albumin level. Maintenance of electrolyte balance, immunoglobulin replacement, high protein and caloric nutritional diet, vitamin supplementation, infection prevention, thromboprophylaxis, and RAASi inhibition are the main conservative therapeutic measures used in CNS [25]. The combination of angiotensin-converting enzyme inhibitors (ACEi) and the prostaglandin inhibitors (indometacin) is successfully used to reduce proteinuria and slow down the progression of illness [13, 25]. Diuretics should be administered with caution only in patients with intravascular fluid overload or severe edemas. Neonates with hyperbilirubinemia should be closely monitored due to severe hypoalbuminemia as they are at high risk for the development of kernicterus. If a conservative treatment fails, bilateral nephrectomy should be considered, a routine nephrectomy in early infancy is no longer recommended [25]. Dialysis is started in patients who develop ESKD or in patients after bilateral nephrectomies. Both the conservative approach and more aggressive management with early nephrectomies are used in children with CNS and there is no data showing a difference in the patient's outcome. Kidney transplantation is performed when a patient weighs at least 8–10 kg, with excellent results. Further studies are needed to compare different treatment strategies for these patients [13, 19, 25]. Importantly, the patients with Fin-major pathogenic variants and a total absence of nephrin in native kidneys can develop anti-nephrin antibodies because a new antigen nephrin expressed in the graft can trigger immunological response that is responsible for the recurrence of NS after transplantation [18].
NPHS2
NPHS2 is the most common affected gene in children and adolescents with SRNS [9, 14, 26]. NPHS2 gene is located on chromosome 1 and encodes a protein called podocin, which plays an important role in the structural integrity of the slit diaphragm required for nephrin recruitment [26]. The pathogenic NPHS2 gene causes non-syndromic autosomal recessive or sporadic SRNS often during the first weeks of life or in an early childhood, maximum within 6 years of age [21, 22]. The age of a patient with the first manifestation of SRNS depends on the type of causal variant in NPHS2. Affected children with homozygous or compound heterozygous causal variants progress rapidly to ESKD by the end of the first decade of life [21, 27]. More than 100 causal variants in NPHS2 gene have been identified that involve mainly missense and frameshift mutations; however, not all of them are clinically significant and associated with the onset of SRNS. While mutated NPHS2 is a common cause of CNS (15–39%), a mild disease course with typical clinical signs in later age has also been described [28].
Interestingly, a common NPHS2 polymorphism p.Arg229Gln, which has a high frequency in healthy populations (A = 0.030447 (7639/250894, GnomAD_exome), is likely pathogenic in combination with causal variant in exon 7 or 8 and this autosomal-recessive association can cause NS with later onset. This rare cause of NS leads to an altered heterodimerization and mislocalization of podocin [26]. The association of p.Arg229Gln with variants found in other exons is not clinically significant and there are no changes in podocin in comparison with wild-type one [26, 29]. Kidney histology in NPHS2 SRNS shows a typically minimal change disease or FSGS [9]. The management of patient is similar to other genetic SRNS in preference of conservative approach. Partial or full clinical response to CNI was observed in 30% of children with pathogenic NPHS2 [30]. Anti-podocin antibodies have never been found, and a risk of disease recurrence after renal transplantation is negligible [27, 30].
CD2AP
CD2AP encodes CD2-associated protein, which forms a bridge between a slit diaphragm and cytoskeleton of podocyte. It closely interacts with nephrin and podocin, and maintains cytoskeletal architecture of podocytes [31]. Heterozygous mutations of CD2AP are linked to proteinuria or the clinical picture of SRNS due to FSGS in pediatric and young adult patients [32].
PLCE1
PLCE1 encodes phospholipase C epsilon, responsible for the generation of second messengers, which have an important role in intracellular signaling for cell growth and differentiation of podocytes in normal glomerular development [33]. It also interacts with GTPase-activating protein that is essential in podocyte cell junction [21]. The mutation in PLCE1 gene is usually associated with an early onset NS [33]. The most common kidney histologic findings in affected individuals are DMS and FSGS. Affected children are born in term with normal birth weight and size of a placenta. Typically, proteinuria occurs postnatally and SRNS develops during the first months of a patient's life. A few affected patients with just missense mutations of PLCE1 suffer from later onset FSGS [34]. The treatment’s goals should focus on preserving both electrolyte and fluid balance, sufficient nutrition, and the prevention of infection. The administration of an ACEi and indomethacin lead to better outcomes [25]. In some cases, a complete remission of proteinuria by cyclosporine A has been observed [16].
ACTN4
The ACTN4 gene encodes a protein called alpha-actinin 4, which is necessary for the proper dynamics of the cytoskeleton in podocytes. This protein is crucial for correct spatial configuration of podocytes, enabling flawless functioning of slit diaphragm. Pathogenic variants in ACTN4 are responsible for autosomal-dominant SRNS; kidney biopsy shows typically FSGS, even unique features such as the formation of podocyte aggregates by electron microscopy was observed [35]. Clinical presentation may range from isolated proteinuria to SRNS in adolescence or early adulthood, until 25 years of age at the latest. The disease slowly progresses toward ESKD, approximately in the fifties [36]. In addition, patients with earlier onset of proteinuria in a childhood with rapid development of ESKD were reported [22].
TRPC6
TRPC6 encodes a transient receptor for potential calcium channels that maintain podocyte membrane homeostasis. Pathogenic TRPC6 variants cause dysregulation of calcium channels leading to incorrect function of podocytes with a risk of SRNS development [37]. Mutated TRPC6 is associated with autosomal-dominant FSGS manifested as SRNS in young adulthood with a quite rapid progression to ESKD [22]. Furthermore, several authors reported cases with TRPC6 causal variants who presented with proteinuria range from subnephrotic to nephrotic in an infancy or in an early childhood with variable severity of the disease [22, 38]. Some patients went into partial remission with immunosuppressive agents [16, 38]. The effect of cyclosporin A on the nuclear factor of activated T cells was reported; therefore, CNI therapy for these patients should be further studied [39].
INF2
INF2 encodes inverted formin 2, a member of actin-regulating proteins securing cytoskeleton presence in podocytes by polymerization of actin. The most commonly described mutations in INF2 gene are heterozygous missense variants for the N-terminal part of the diaphanous inhibitory domain [40]. The phenotypic spectrum of children with mutated INF2 ranges from isolated proteinuria to fully expressed SRNS with fast or gradual progression to ESKD. Later manifestation in adulthood has been reported. FSGS is the predominant histologic pattern in affected individuals [41]. It is assumed that corticosteroids may have a stabilizing effect on the podocyte cytoskeleton, so this treatment can be effective in some patients with INF2 pathogenic variants [42, 43]. Moreover, a heterozygous variant in INF2 gene can be associated with chronic motor and sensory peripheral neuropathy called Charcot–Marie–Tooth, but the neurological phenotype is not typical for INF2 SRNS cases [44].
There are other genes encoding proteins resulting in podocytopathies associated with the onset of SRNS in children, rarely encountered in a clinical practice, summarized in Table 3. With the advances in molecular genetics, it is just a matter of time when further novel proteins necessary for the proper function of podocytes and slit diaphragm will be identified. Hopefully, in the future, targeted therapy based on the pathogenesis of genetic forms of NS will be available [40].
Conclusion
It is essential to recognize the genetic etiology of SRNS, because a clinical course and treatment response may differ. The results of molecular genetic testing are necessary for the proper management and for genetic counseling of the patient and the family. With the development of methods for genome, exon, and individual gene sequencing, new genes with a potential role in the development of SRNS and new pathological variants of already known genes are constantly being identified. However, to confirm the pathogenicity of a specific variant, additional functional studies are necessary. These technologies may be expensive and demanding. This is the only way we can really confirm the pathogenicity of specific variants in the development of SRNS, and thus potentially find individualized therapy and predict the prognosis of diseases. Thanks to the findings so far, we can say that SRNS is a complex disease and that the most common variants in different genes have different mechanisms of pathogenesis that lead to the manifestation of the disease.
Nephrologists should provide therapy to patients with SRNS in the tertiary centers with the cooperation of other medical specialties. Although there are many research teams dedicated to SRNS coming up with new insights, the treatment for most patients with SRNS has not fundamentally changed. In case of CKD progression, conservative therapy should be initiated and dialysis is used in ESKD as a bridging method to kidney transplantation as the best treatment of ESKD. Therefore, the greatest potential of genetic sequencing methods (NGS, subsequently confirmed by Sanger) is the discovery of the exact genetic essence of the disease; within functional studies, the understanding of the role of a specific gene in the pathogenesis of the disease, which in the future will enable us to develop individualized therapy for the patient, thereby avoiding standard treatment associated with a number of side effects and uncertain results, thereby significantly improving the quality of life of patients and their prognosis.
Data Availability
All data generated or analysed during this study are included in this published article.
Abbreviations
- ACEi:
-
Angiotensin converting enzyme inhibitor
- Co Q10:
-
Coenzyme Q10
- CNI:
-
Calcineurin inhibitors
- CNS:
-
Congenital nephrotic syndrome
- DMS:
-
Diffuse mesangial sclerosis
- ESKD:
-
End-stage kidney disease
- FSGS:
-
Focal segmental glomerulosclerosis
- NGS:
-
Next-generation sequencing
- NS:
-
Nephrotic syndrome
- RAASi:
-
Renin–angiotensin–aldosterone system inhibitors
- SSNS:
-
Steroid sensitive nephrotic syndrome
- SRNS:
-
Steroid resistant nephrotic syndrome
- WGS:
-
Whole genome sequencing
- WES:
-
Whole exome sequencing
References
Rovin BH, Adler SG, Barratt J, Bridoux F, Burdge KA, Chan TM, et al. Executive summary of the KDIGO 2021 guideline for the management of glomerular diseases. Kidney Int. 2021;100(4):753–79.
Menon MC, Chuang PY, He CJ. The glomerular filtration barrier: components and crosstalk. Int J Nephrol. 2012;2012: 749010.
Mekahli D, Liutkus A, Ranchin B, Yu A, Bessenay L, Girardin E, et al. Long-term outcome of idiopathic steroid-resistant nephrotic syndrome: a multicenter study. Pediatr Nephrol. 2009;24(8):1525–32.
Sureshkumar P, Hodson EM, Willis NS, Barzi F, Craig JC. Predictors of remission and relapse in idiopathic nephrotic syndrome: a prospective cohort study. Pediatr Nephrol. 2014;29(6):1039–46.
Noone DG, Iijima K, Parekh R. Idiopathic nephrotic syndrome in children. Lancet. 2018;392(10141):61–74.
Tapia C, Bashir K. Nephrotic syndrome. In: StatPearls. Treasure Island: StatPearls Publishing; 2022.
Bezdíčka M, Štolbová Š, Seeman T, Cinek O, Malina M, Šimánková N, et al. Genetic diagnosis of steroid-resistant nephrotic syndrome in a longitudinal collection of Czech and Slovak patients: a high proportion of causative variants in NUP93. Pediatr Nephrol. 2018;33(8):1347–63.
Trautmann A, Lipska-Ziętkiewicz BS, Schaefer F. Exploring the clinical and genetic spectrum of steroid resistant nephrotic syndrome: the PodoNet registry. Front Pediatr. 2018;6:200.
Rheault MN, Gbadegesin RA. The genetics of nephrotic syndrome. J Pediatr Genet. 2016;5(1):15–24.
Preston R, Stuart HM, Lennon R. Genetic testing in steroid-resistant nephrotic syndrome: why, who, when and how? Pediatr Nephrol. 2019;34(2):195–210.
Harita Y. Application of next-generation sequencing technology to diagnosis and treatment of focal segmental glomerulosclerosis. Clin Exp Nephrol. 2018;22(3):491–500.
Kestilä M, Lenkkeri U, Männikkö M, Lamerdin J, McCready P, Putaala H, et al. Positionally cloned gene for a novel glomerular protein–nephrin–is mutated in congenital nephrotic syndrome. Mol Cell. 1998;1(4):575–82.
Sachdeva S, Khan S, Davalos C, Avanthika C, Jhaveri S, Babu A, et al. Management of steroid-resistant nephrotic syndrome in children. Cureus. 2021;13(11): e19363.
Sadowski CE, Lovric S, Ashraf S, Pabst WL, Gee HY, Kohl S, et al. A single-gene cause in 29.5% of cases of steroid-resistant nephrotic syndrome. J Am Soc Nephrol. 2015;26(6):1279–89.
Lipska-Ziętkiewicz BS, Ozaltin F, Hölttä T, Bockenhauer D, Bérody S, Levtchenko E, et al. Genetic aspects of congenital nephrotic syndrome: a consensus statement from the ERKNet–ESPN inherited glomerulopathy working group. Eur J Hum Genet. 2020;28(10):1368–78.
Malakasioti G, Iancu D, Tullus K. Calcineurin inhibitors in nephrotic syndrome secondary to podocyte gene mutations: a systematic review. Pediatr Nephrol. 2021;36(6):1353–64.
Drovandi S, Lipska-Ziętkiewicz BS, Ozaltin F, Emma F, Gulhan B, Boyer O, et al. Oral coenzyme Q10 supplementation leads to better preservation of kidney function in steroid-resistant nephrotic syndrome due to primary coenzyme Q10 deficiency. Kidney Int. 2022;102(3):604–12.
Bierzynska A, Saleem MA. Deriving and understanding the risk of post-transplant recurrence of nephrotic syndrome in the light of current molecular and genetic advances. Pediatr Nephrol. 2018;33(11):2027–35.
Trautmann A, Vivarelli M, Samuel S, Gipson D, Sinha A, Schaefer F, et al. IPNA clinical practice recommendations for the diagnosis and management of children with steroid-resistant nephrotic syndrome. Pediatr Nephrol. 2020;35(8):1529–61.
Bérody S, Heidet L, Gribouval O, Harambat J, Niaudet P, Baudouin V, et al. Treatment and outcome of congenital nephrotic syndrome. Nephrol Dial Transplant. 2019;34(3):458–67.
Hinkes BG, Mucha B, Vlangos CN, Gbadegesin R, Liu J, Hasselbacher K, et al. Nephrotic syndrome in the first year of life: two thirds of cases are caused by mutations in 4 genes (NPHS1, NPHS2, WT1, and LAMB2). Pediatrics. 2007;119(4):e907–19.
Bierzynska A, McCarthy HJ, Soderquest K, Sen ES, Colby E, Ding WY, et al. Genomic and clinical profiling of a national nephrotic syndrome cohort advocates a precision medicine approach to disease management. Kidney Int. 2017;91(4):937–47.
Patrakka J, Martin P, Salonen R, Kestilä M, Ruotsalainen V, Männikkö M, et al. Proteinuria and prenatal diagnosis of congenital nephrosis in fetal carriers of nephrin gene mutations. Lancet. 2002;359(9317):1575–7.
Huttunen NP, Rapola J, Vilska J, Hallman N. Renal pathology in congenital nephrotic syndrome of Finnish type: a quantitative light microscopic study on 50 patients. Int J Pediatr Nephrol. 1980;1(1):10–6.
Boyer O, Schaefer F, Haffner D, Bockenhauer D, Hölttä T, Bérody S, et al. Management of congenital nephrotic syndrome: consensus recommendations of the ERKNet-ESPN working group. Nat Rev Nephrol. 2021;17(4):277–89.
Tory K, Menyhárd DK, Woerner S, Nevo F, Gribouval O, Kerti A, et al. Mutation-dependent recessive inheritance of NPHS2-associated steroid-resistant nephrotic syndrome. Nat Genet. 2014;46(3):299–304.
Weber S, Gribouval O, Esquivel EL, Morinière V, Tête MJ, Legendre C, et al. NPHS2 mutation analysis shows genetic heterogeneity of steroid-resistant nephrotic syndrome and low post-transplant recurrence. Kidney Int. 2004;66(2):571–9.
Bouchireb K, Boyer O, Gribouval O, Nevo F, Huynh-Cong E, Morinière V, et al. NPHS2 mutations in steroid-resistant nephrotic syndrome: a mutation update and the associated phenotypic spectrum. Hum Mutat. 2014;35(2):178–86.
Rood IM, Deegens JKJ, Lugtenberg D, Bongers E, Wetzels JFM. Nephrotic syndrome with mutations in NPHS2: the role of R229Q and implications for genetic counseling. Am J Kidney Dis. 2019;73(3):400–3.
Büscher AK, Beck BB, Melk A, Hoefele J, Kranz B, Bamborschke D, et al. Rapid response to cyclosporin A and favorable renal outcome in nongenetic versus genetic steroid-resistant nephrotic syndrome. Clin J Am Soc Nephrol. 2016;11(2):245–53.
Kim JM, Wu H, Green G, Winkler CA, Kopp JB, Miner JH, et al. CD2-associated protein haploinsufficiency is linked to glomerular disease susceptibility. Science. 2003;300(5623):1298–300.
Löwik M, Levtchenko E, Westra D, Groenen P, Steenbergen E, Weening J, et al. Bigenic heterozygosity and the development of steroid-resistant focal segmental glomerulosclerosis. Nephrol Dial Transplant. 2008;23(10):3146–51.
Hinkes B, Wiggins RC, Gbadegesin R, Vlangos CN, Seelow D, Nürnberg G, et al. Positional cloning uncovers mutations in PLCE1 responsible for a nephrotic syndrome variant that may be reversible. Nat Genet. 2006;38(12):1397–405.
Boyer O, Benoit G, Gribouval O, Nevo F, Pawtowski A, Bilge I, et al. Mutational analysis of the PLCE1 gene in steroid resistant nephrotic syndrome. J Med Genet. 2010;47(7):445–52.
Henderson JM, Alexander MP, Pollak MR. Patients with ACTN4 mutations demonstrate distinctive features of glomerular injury. J Am Soc Nephrol. 2009;20(5):961–8.
Pollak MR, Alexander MP, Henderson JM. A case of familial kidney disease. Clin J Am Soc Nephrol. 2007;2(6):1367–74.
Ilatovskaya DV, Staruschenko A. TRPC6 channel as an emerging determinant of the podocyte injury susceptibility in kidney diseases. Am J Physiol Renal Physiol. 2015;309(5):F393–7.
Santín S, Ars E, Rossetti S, Salido E, Silva I, García-Maset R, et al. TRPC6 mutational analysis in a large cohort of patients with focal segmental glomerulosclerosis. Nephrol Dial Transplant. 2009;24(10):3089–96.
Schlöndorff J, Del Camino D, Carrasquillo R, Lacey V, Pollak MR. TRPC6 mutations associated with focal segmental glomerulosclerosis cause constitutive activation of NFAT-dependent transcription. Am J Physiol Cell Physiol. 2009;296(3):C558–69.
Akchurin O, Reidy KJ. Genetic causes of proteinuria and nephrotic syndrome: impact on podocyte pathobiology. Pediatr Nephrol. 2015;30(2):221–33.
Boyer O, Benoit G, Gribouval O, Nevo F, Tête MJ, Dantal J, et al. Mutations in INF2 are a major cause of autosomal dominant focal segmental glomerulosclerosis. J Am Soc Nephrol. 2011;22(2):239–45.
Hahn D, Hodson EM, Willis NS, Craig JC. Corticosteroid therapy for nephrotic syndrome in children. Cochrane Database Syst Rev. 2015;2015(3):Cd001533.
Zhao X, Hwang DY, Kao HY. The role of glucocorticoid receptors in podocytes and nephrotic syndrome. Nucl Receptor Res. 2018. https://doi.org/10.11131/2018/101323.
Boyer O, Nevo F, Plaisier E, Funalot B, Gribouval O, Benoit G, et al. INF2 mutations in Charcot-Marie-Tooth disease with glomerulopathy. N Engl J Med. 2011;365(25):2377–88.
Ebefors K, Lassén E, Anandakrishnan N, Azeloglu EU, Daehn IS. Modeling the glomerular filtration barrier and intercellular crosstalk. Front Physiol. 2021;12: 689083.
Funding
This work was supported by the VEGA grant 1/0311/21 (the grant of the Ministry of education, science, research and sport of the Slovak republic).
Author information
Authors and Affiliations
Contributions
All authors contributed to the manuscript and reviewed the manuscript critically and approved the final version. BP drafted and edited the manuscript; JZ supervised, edited, and reviewed the manuscript; MB edited and reviewed the manuscript; PK, JB, and PB reviewed the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors have indicated they have no potential conflict of interest to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
About this article
Cite this article
Pitekova, B., Bezdicka, M., Konopasek, P. et al. Genetic nephrotic syndrome associated with disturbed function of glomerular slit membrane and podocyte cytoskeleton in children. Clin Exp Nephrol 27, 101–109 (2023). https://doi.org/10.1007/s10157-022-02305-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10157-022-02305-x