Abstract
Background
It is necessary to re-examine the optimal phosphate (P) and calcium (Ca) target values in the contemporary management of chronic kidney disease–mineral and bone disorder to reduce the risks of cardiovascular events in patients receiving hemodialysis.
Methods
We performed a post-hoc analysis of the LANDMARK study. The outcomes were defined as cardiovascular events and all-cause death. Data from 2135 patients receiving hemodialysis at risk of vascular calcification were analyzed using a time-dependent Cox proportional hazard model adjusted for background factors.
Results
On the hazard ratio (HR) curve, the ranges where the lower 95% confidence interval (CI) were below the minimum of HR (= 1.00) were as follows: P = 3.5–5.5 mg/dL; albumin-adjusted Ca < 9.1 mg/dL for cardiovascular events; and P = 3.6–5.3 mg/dL; albumin-adjusted Ca < 9.1 mg/dL for all-cause mortality. In stratified analysis, the HRs for cardiovascular events in P < 3.5 mg/dL and P ≥ 5.5 mg/dL were similar to that of P = 3.5–5.5 mg/dL (P ≥ 0.05), and albumin-adjusted Ca ≥ 9.1 mg/dL had higher HR than values < 9.1 mg/dL [1.30 (95% CI 1.00–1.68; P = 0.046)]. For all-cause mortality, the HR in P < 3.6 mg/dL was higher than that in P = 3.6–5.3 mg/dL [1.76 (95% CI 1.25–2.48; P = 0.001)], while the HRs between P ≥ 5.3 mg/dL and P = 3.6–5.3 mg/dL as well as those between albumin-adjusted Ca ≥ 9.1 and < 9.1 mg/dL were not significantly different (P ≥ 0.05).
Conclusions
Managing albumin-adjusted Ca < 9.1 mg/dL may reduce the cardiovascular risk among patients undergoing hemodialysis. Hypophosphatemia < 3.6 mg/dL may be associated with mortality.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Cardiovascular disease is highly prevalent and a leading cause of death among patients with chronic kidney disease (CKD) who undergo hemodialysis [1]. Many factors contribute to the development of cardiovascular disease in patients undergoing hemodialysis, including classical risk factors such as hypertension, dyslipidemia, and chronic inflammation, in addition to risk factors specific to CKD and dialysis therapy. Among these, CKD–mineral and bone disorder (MBD) likely plays an important role in the pathogenesis of cardiovascular disease among patients with end-stage kidney disease [2, 3]. Large-scale observational studies consistently show that serum levels of phosphate (P) and calcium (Ca) are significantly associated with cardiovascular risk and all-cause mortality in patients receiving dialysis [4,5,6,7]. In most patients undergoing dialysis, even with dietary P restrictions, hyperphosphatemia is inevitable and requires a P binder to control serum P levels [8]. Unfortunately, there is no randomized clinical trial (RCT) comparing the effects of P binders and a placebo on hard outcomes, including cardiovascular events and all-cause mortality. However, observational studies have shown that P binder use improved survival rate among patients undergoing hemodialysis [4, 9, 10]. However, the optimal serum P level range remains unclear. Based on data from observational studies, the Kidney Disease Outcomes Quality Initiative (K/DOQI) clinical practice guidelines recommend that patients undergoing dialysis achieve the following target ranges for biochemical markers of CKD–MBD: 3.5–5.5 mg/dL for serum P, 8.4–9.5 mg/dL for albumin-adjusted Ca, and 150–300 pg/L for intact parathyroid hormone (iPTH) [11]. The Japanese Society for Dialysis Therapy (JSDT) clinical practice guidelines recommend the following ranges: 3.5–6 mg/dL for serum P, 8.4–10 mg/dL for albumin-adjusted Ca, and 60–240 pg/L for iPTH [12]. The updated 2017 kidney disease: improving global outcomes (KDIGO) guidelines recommend that elevated serum P levels should be lowered towards the normal range in patients with CKD irrespective of hemodialysis [8]. The results of the COSMOS study show that serum P and Ca levels of 4.4 and 8.8 mg/dL, respectively, were associated with the minimum relative risk of mortality among European patients undergoing hemodialysis [10]. In addition, a recent RCT in Japan reported that strict P control using non-Ca-based P binders with P-binding affinity inhibited the progression of coronary artery calcification (CAC) [13]—which is a reliable surrogate marker for cardiovascular disease [14]—over conventional control in patients undergoing hemodialysis. Observational cohorts have examined the relationship between CKD–MBD biomarkers and cardiovascular risk or mortality; however, neither calcimimetic agents nor non-Ca-based P binders, both of which can facilitate serum P concentration management without increasing Ca load, have been used in clinical practice [4,5,6,7]. We conducted a post-hoc analysis of the LANDMARK study [15], which is an RCT comparing Ca carbonate-based and lanthanum carbonate-based treatment for hyperphosphatemia among patients undergoing hemodialysis at risk of vascular calcification, to clarify the optimal target levels of P and Ca to reduce the risk of cardiovascular events and all-cause mortality.
Materials and methods
Study design and population
We examined participants enrolled in the LANDMARK study, which is a randomized, open-label, blinded clinical trial comparing lanthanum carbonate-based treatment with Ca carbonate-based treatment among patients with hyperphosphatemia undergoing hemodialysis with at least one vascular calcification risk factor (age ≥ 65 years, post menopause, diabetes). The patients were recruited from a total of 273 dialysis facilities across Japan between November 2011 and June 2018. The LANDMARK study design and its results have been previously published [15]. The eligibility criteria are shown in Online Resource 1. The LANDMARK study was approved by the local ethics committees and all participants provided written informed consent. The study procedures adhered to the Declaration of Helsinki. A total of 2374 patients were screened for enrollment, and data from 2135 patients formed the full analysis set (Online Resource 2) and were analyzed.
Outcomes
The primary outcome was defined as a composite of cardiovascular events that included: (1) death due to a cardiovascular event (myocardial infarction or stroke), including cardiac death; (2) nonfatal myocardial infarction; (3) nonfatal stroke, including transient ischemic attack; (4) unstable angina; (5) hospitalization for heart failure; and (6) hospitalization for ventricular arrhythmia (Online Resource 3). All-cause mortality was evaluated as the secondary outcome.
Statistical analyses
A Cox proportional hazard model with time-dependent variables was used to evaluate the association between P, Ca, and the incidence of cardiovascular events and all-cause mortality, with results expressed as hazard ratios (HRs) and 95% confidence intervals (CIs). P and albumin-adjusted Ca concentrations were incorporated into the Cox model as continuous variables and smoothed using natural cubic splines for visualization. Models for adjustment were as follows: Model 1 was unadjusted, Model 2 was adjusted for some background factors, and Model 3 was the full model. The minimum HRs of P and Ca concentrations were used as a reference (HR = 1.00), HR curves were drawn for P and albumin-adjusted Ca, and three-dimensional HR curves were generated for the combination of P and albumin-adjusted Ca. Then, a stratified analysis was performed using a time-dependent Cox proportional hazard model with grouping by the concentration at which the lower 95% CI crossed HR = 1.00 threshold in the HR curves. The range where the lower 95% CI was less than 1.00 threshold in the HR curve was used as the reference, and the HR was adjusted by the variables in Model 3. Finally, HR curves were drawn for the change in P and albumin-adjusted Ca concentrations from baseline with that grouping.
All analyses were performed using R version 4.1.2, the ‘survival’ package. The significance level was set to P < 0.05 (two-tailed). Albumin-adjusted Ca was calculated using serum albumin levels with Payne’s formula [16].
Results
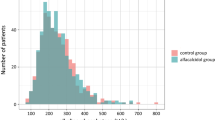
Data from 2135 patients were analyzed. The baseline characteristics are shown in Table 1. The median age of the patients was 69 years, 40.5% were female, the median dialysis vintage was 4.7 years, and 56.1% of the patients had diabetes. During a median follow-up period of 3.16 [interquartile range (IQR) 2.47–3.86] years, cardiovascular events occurred in 281 patients [4.55/100 person-years (95% CI 4.03–5.11)] and 307 patients did not survive [4.74/100 person-years (95% CI 4.23–5.30)] (Table 2).
Hazard ratios for cardiovascular events and all-cause mortality
Figure 1a shows the association of the relative risk of cardiovascular events with serum P concentration. The relationship between serum P concentrations and the HR for cardiovascular event risk appeared as U-shaped curves, consistent with previous studies [4,5,6,7, 10]. Model 1 was unadjusted and Model 2 was adjusted for age, sex, years of hemodialysis, diabetes, and albumin concentration. Model 3 was the full model adjusted for the Model 2 variables plus current smoking, either P or albumin-adjusted Ca concentration, hemoglobin concentration, platelet count, iPTH concentration, potassium concentration, Kt/V (estimated using the second generation Daugirdas equation [17]), and prescription of active vitamin D, cinacalcet hydrochloride, statins, and renin-angiotensin system inhibitors. In the association between the relative risk for cardiovascular events and albumin-adjusted Ca concentrations, a U-shaped trend was also observed (Fig. 1b). The lowest HR was noted at serum P and Ca levels of 4.7 and 8.5 mg/dL, respectively (Fig. 1a, b). The lower 95% CI of the HR crossed the HR = 1.00 threshold at 3.5 and 5.5 mg/dL for P, and 9.1 mg/dL for albumin-adjusted Ca (Fig. 1a, b). All-cause mortality was assessed and is shown in Fig. 1c, d. The lowest HR was noted at serum P and Ca levels of 4.7 and 8.6 mg/dL, respectively (Fig. 1c, d). The lower 95% CI of the HR crossed the HR = 1.0 threshold at 3.6 and 5.3 mg/dL for P, and 9.1 mg/dL for albumin-adjusted Ca (Fig. 1c, d). Online Resource 4 shows the HR curves for uncorrected calcium concentration.
Hazard ratio curve for phosphorus and calcium concentration, respectively. Hazard ratios (HRs) using a time-dependent Cox proportional hazard model incorporating phosphorus and calcium concentration respectively. a and b show HRs for cardiovascular events, c and d show HRs for all-cause mortality. The serum value with the lowest HR is shown in blue and designated as the reference (HR = 1.0). The serum values at which the lower 95% CI of the HR crosses the HR = 1.0 threshold are shown in light blue. Model 1: unadjusted; Model 2: adjusted for age, sex, years undergoing hemodialysis, diabetes, and albumin concentration; and Model 3: adjusted for the Model 2 variables plus current smoking, either phosphate or albumin-adjusted calcium concentration, hemoglobin concentration, platelet count, intact parathyroid hormone concentration, potassium concentration, Kt/V, and prescription of active vitamin D, cinacalcet hydrochloride, statins, and renin-angiotensin system inhibitors. HR hazard ratio, P phosphate, ACa albumin-adjusted calcium
In the combined P and Ca analysis, the lowest HR of the cardiovascular events was noted at serum P and Ca levels of 4.7 and 8.5 mg/dL, respectively (Fig. 2a). The lowest HR for all-cause mortality was noted at serum P and albumin-adjusted Ca levels of 4.7 and 8.6 mg/dL, respectively (Fig. 2b).
Three-dimensional curve of the hazard ratio for the combination of phosphorus and albumin-adjusted calcium concentration. The three-dimensional curve of the hazard ratio (HR) using a time-dependent Cox proportional hazard model for the combination of phosphorus and albumin-adjusted calcium concentration. a shows HRs for cardiovascular events, b shows HRs for all-cause mortality. The serum value with the lowest HR is shown in blue and designated as the reference (HR = 1.0). Model 1: unadjusted; Model 2: adjusted for age, sex, years undergoing hemodialysis, diabetes, and albumin concentration; and Model 3: adjusted for the Model 2 variables plus current smoking, either phosphate or albumin-adjusted calcium concentration, hemoglobin concentration, platelet count, intact parathyroid hormone concentration, potassium concentration, Kt/V, and prescription of active vitamin D, cinacalcet hydrochloride, statins, and renin-angiotensin system inhibitors. HR hazard ratio, P phosphate, ACa albumin-adjusted calcium
Stratifications of phosphate and calcium
The HRs stratified by serum P and Ca are shown in Tables 3 and 4. For cardiovascular events, the HRs in P < 3.5 mg/dL and P ≥ 5.5 mg/dL were similar to that in P = 3.5–5.5 mg/dL [adjusted HR 1.41 (95% CI 0.91–2.19; P = 0.124) in P < 3.5 mg/dL; and 1.10 (95% CI 0.84–1.43; P = 0.479) in P ≥ 5.5 mg/dL]. The albumin-adjusted Ca ≥ 9.1 mg/dL was associated with a higher risk of cardiovascular events compared with < 9.1 mg/dL [adjusted HR 1.30 (95% CI 1.00–1.68; P = 0.046)]. For all-cause mortality, the HR in P < 3.6 mg/dL was higher than that in P = 3.6–5.3 mg/dL [adjusted HR 1.76 (95% CI 1.25–2.48; P = 0.001)], while there was no difference between P ≥ 5.3 mg/dL and P = 3.6–5.3 mg/dL [adjusted HR 1.23 (95% CI 0.95–1.60; P = 0.121)]. The HR for all-cause mortality in albumin-adjusted Ca ≥ 9.1 mg/dL was similar to that in < 9.1 mg/dL [adjusted HR 1.14 (95% CI 0.89–1.45; P = 0.309)].
In the combined P and Ca analysis (Table 5), the risk for cardiovascular events was higher in the group with P < 3.5 mg/dL and albumin-adjusted Ca ≥ 9.1 mg/dL than in the group with P = 3.5–5.5 mg/dL and albumin-adjusted Ca < 9.1 mg/dL [adjusted HR 1.86 (95% CI 1.03–3.36; P = 0.038)]. For all-cause mortality, the HRs were higher in the groups with P < 3.6 mg/dL and albumin-adjusted Ca < 9.1 mg/dL, as well as in groups with P < 3.6 mg/dL and albumin-adjusted Ca ≥ 9.1 mg/dL than in the group with P = 3.6–5.3 mg/dL and albumin-adjusted Ca < 9.1 mg/dL [adjusted HR 2.01 (95% CI 1.17–3.45; P = 0.012); and 1.82 (95% CI 1.12–2.97; P = 0.016), respectively] (Table 6).
Changes from baseline and hazard ratio
Online Resource 5, 6 show HR curves for changes in P and albumin-adjusted Ca concentrations from baseline. In patients with baseline albumin-adjusted Ca ≥ 9.1 mg/dL, the upper 95% CI was partially below the HR 1.00 threshold (i.e., 0.3–1.2 mg/dL reduction in albumin-adjusted Ca concentration was associated with a reduced risk of cardiovascular events) (Online Resource 5e).
Comparison with current guidelines
Online Resource 7 shows the risk of cardiovascular events and all-cause mortality in the group with an average P and albumin-adjusted Ca concentration until the event occurred within the current guideline range (P = 3.5–6. mg/dL; albumin-adjusted Ca = 8.4–10.0 mg/dL) and in the group with new target range from this study (P = 3.5–5.5 mg/dL for cardiovascular events, 3.6–5.3 mg/dL for all-cause mortality, and albumin-adjusted Ca < 9.1 mg/dL).
Discussion
Serum P and albumin-adjusted Ca concentrations are strong predictors of cardiovascular events and survival among patients undergoing dialysis. Target values for serum P and albumin-adjusted Ca are based on the results from observational studies conducted between the late 1980s and late 2000s [4, 7, 18,19,20,21]. However, at that time, neither calcimimetics nor Ca-free P binders, both of which allow for stringent control of CKD–MBD biomarkers, were clinically available. A recent large-scale observational study across European countries suggests that stringent management of CKD–MBD biomarkers is likely to be associated with better survival in patients undergoing dialysis [10]. An RCT comparing standard and stringent control of serum P concentrations (5.0–6.0 vs. 3.5–4.5 mg/dL) showed that stringent P control significantly delayed coronary artery calcification progression in patients undergoing dialysis [13]. Based on the results from these studies, it is important to consider setting stringent targets for serum P and albumin-adjusted Ca concentrations.
The present study, which is a post-hoc analysis of the LANDMARK study, examined the association between serum P, or albumin-adjusted Ca concentrations and cardiovascular events, or all-cause death. For serum P concentrations, the HR curve suggested that a range of 3.5–5.5 mg/dL would reduce the risk of cardiovascular events, but stratified analysis showed no significant HR differences. For all-cause mortality, the HR curve proposed a range of 3.6–5.3 mg/dL, and stratified analysis showed that P < 3.6 mg/dL was significantly associated with the risk of death. However, the possibility that this is a result of the effects of undernutrition cannot be ruled out. For albumin-adjusted calcium, both the HR curve and the stratified analysis suggest that < 9.1 mg/dL is associated with a reduced risk of cardiovascular events. The HR for change in concentration from baseline suggests that for patients with albumin-adjusted Ca > 9.1 mg/dL, lowering albumin-adjusted Ca may be associated with a lower risk of cardiovascular events. This suggests that it is important to lower the albumin-adjusted calcium to a more stringent target range than the current guidelines. Recent studies have suggested that hypercalcemia has a poor prognosis, and the results of this study support this notion [22].
Cinacalcet facilitates strict control of PTH levels without increasing Ca load, leading to improved control of serum P and Ca concentrations because of reduced P and Ca efflux from bone due to decreased PTH concentrations [23]. In addition, novel non-Ca-based P binders with strong P-lowering action, including lanthanum carbonate and sucroferric oxyhydroxide, are likely to decrease serum P concentrations even in patients with refractory hyperphosphatemia [24]. However, stringent management of serum P and albumin-adjusted Ca concentration for CKD–MBD in patients undergoing dialysis remains challenging. Patients with end-stage kidney disease are generally prescribed many drugs due to the risk of complications of the disease, including antihypertensive drugs, statins, antiplatelet agents, and P binders. Polypharmacy is another challenging issue to address not only from the perspective of the patients undergoing dialysis but also in terms of minimizing healthcare costs [24]. Daily doses of P binders generally include multiple tablets, and these account for approximately half the number of prescribed tablets taken by patients undergoing dialysis [25]. Thus, there is concern that stringent CKD–MBD management may exacerbate polypharmacy, even with the use of expensive novel P binders with high efficacy. Recently, novel drugs that inhibit active intestinal P transport have been developed. Tenapanor is likely to improve serum P control with lesser pill burden compared to conventional P binder therapy [26]. The present study suggests that restricting albumin-adjusted Ca concentration is associated with better clinical outcomes among Japanese patients undergoing dialysis with at least one risk factor for vascular calcification. However, this is a post-hoc analysis of an RCT and, therefore, we could not confirm that stringent management can improve clinical outcomes. It is important that recommendations for stringent P control are based on robust data derived from an RCT.
Strengths and limitations
The strength of this study is that the LANDMARK study had a long follow-up period and included the collection and adjudication of important clinical events in modern clinical practice [15, 27]. Additionally, an independent event evaluation committee evaluated individual events with credibility to the definition of events. Furthermore, measurements for P and Ca were taken at multiple times during the study period, allowing for analysis in a time-dependent Cox proportional hazard model. This model can include in its analysis not only baseline data but also all data gathered during the study period.
However, this study had some limitations. This study may have lacked power due to the lower incidence of cardiovascular events in the LANDMARK study compared to that in previous studies. Moreover, this was a single-country study and included patients with an iPTH concentration less than 240 pg/mL; thus, it is unclear whether the trial findings can be generalized to different populations.
Conclusions
In a post-hoc analysis of the LANDMARK study, managing albumin-adjusted Ca concentrations < 9.1 mg/dL may reduce cardiovascular risk among patients undergoing hemodialysis. Hypophosphatemia < 3.6 mg/dL may be associated with mortality.
Data availability
The data underlying this article will be shared on reasonable request to the corresponding author.
References
Sarnak MJ, Levey AS, Schoolwerth AC, et al. Kidney disease as a risk factor for development of cardiovascular disease: a statement from the American heart association councils on kidney in cardiovascular disease, high blood pressure research, clinical cardiology, and epidemiology and prevention. Hypertension. 2003;42:1050–65. https://doi.org/10.1161/01.HYP.0000102971.85504.7c.
Goodman WG, Goldin J, Kuizon BD, et al. Coronary-artery calcification in young adults with end-stage renal disease who are undergoing dialysis. New Engl J Med. 2000;342:1478–83. https://doi.org/10.1056/NEJM200005183422003.
Qunibi WY, Nolan CA, Ayus JC. Cardiovascular calcification in patients with end-stage renal disease: a century-old phenomenon. Kidney Int Suppl. 2002;82:S73-80. https://doi.org/10.1046/j.1523-1755.62.s82.15.x.
Young EW, Albert JM, Satayathum S, et al. Predictors and consequences of altered mineral metabolism: the dialysis outcomes and practice patterns study. Kidney Int. 2005;67:1179–87. https://doi.org/10.1111/j.1523-1755.2005.00185.x.
Tentori F, Blayney MJ, Albert JM, et al. Mortality risk for dialysis patients with different levels of serum calcium, phosphorus, and PTH: the dialysis outcomes and practice patterns study (DOPPS). Am J Kidney Dis. 2008;52:519–30. https://doi.org/10.1053/j.ajkd.2008.03.020.
Floege J, Kim J, Ireland E, et al. Serum iPTH, calcium and phosphate, and the risk of mortality in a European haemodialysis population. Nephrol Dial Transplant. 2011;26:1948–55. https://doi.org/10.1093/ndt/gfq219.
Taniguchi M, Fukagawa M, Fujii N, et al. Serum phosphate and calcium should be primarily and consistently controlled in prevalent hemodialysis patients. Ther Apher Dial. 2013;17:221–8. https://doi.org/10.1111/1744-9987.12030.
Kidney disease: improving global outcomes CKDMBD. KDIGO 2017 clinical practice guideline update for the diagnosis, evaluation, prevention, and treatment of chronic kidney disease-mineral and bone disorder (CKD–MBD). Kidney Int Suppl. 2017;7:1–59.
Isakova T, Gutiérrez OM, Chang Y, et al. Phosphorus binders and survival on hemodialysis. J Am Soc Nephrol. 2009;20:388–96. https://doi.org/10.1681/ASN.2008060609.
Fernández-Martín JL, Martínez-Camblor P, Dionisi MP, et al. Improvement of mineral and bone metabolism markers is associated with better survival in haemodialysis patients: the COSMOS study. Nephrol Dial Transplant. 2015;30:1542–51. https://doi.org/10.1093/ndt/gfv099.
National Kidney Foundation. K/DOQI clinical practice guidelines for bone metabolism and disease in chronic kidney disease. Am J Kidney Dis. 2003;42:S1-201.
Fukagawa M, Yokoyama K, Koiwa F, et al. Clinical practice guideline for the management of chronic kidney disease-mineral and bone disorder. Ther Apher Dial. 2013;17:247–88. https://doi.org/10.1111/1744-9987.12058.
Isaka Y, Hamano T, Fujii H, et al. Optimal phosphate control related to coronary artery calcification in dialysis patients. J Am Soc Nephrol. 2021;32:723–35. https://doi.org/10.1681/ASN.2020050598.
Greenland P, LaBree L, Azen SP, Doherty TM, Detrano RC. Coronary artery calcium score combined with Framingham score for risk prediction in asymptomatic individuals. JAMA. 2004;291:210–5. https://doi.org/10.1001/jama.291.2.210.
Ogata H, Fukagawa M, Hirakata H, et al. Effect of treating hyperphosphatemia with lanthanum carbonate vs. calcium carbonate on cardiovascular events in patients with chronic kidney disease undergoing hemodialysis: the LANDMARK randomized clinical trial. JAMA. 2021;325:1946–54. https://doi.org/10.1001/jama.2021.4807.
Payne RB, Little AJ, Williams RB, Milner JR. Interpretation of serum calcium in patients with abnormal serum proteins. Br Med J. 1973;4:643–6. https://doi.org/10.1136/bmj.4.5893.643.
Daugirdas JT. Second generation logarithmic estimates of single-pool variable volume Kt/V: an analysis of error. J Am Soc Nephrol. 1993;4:1205–13. https://doi.org/10.1681/ASN.V451205.
Lowrie EG, Lew NL. Death risk in hemodialysis patients: the predictive value of commonly measured variables and an evaluation of death rate differences between facilities. Am J Kidney Dis. 1990;15:458–82. https://doi.org/10.1016/s0272-6386(12)70364-5.
Block GA, Hulbert-Shearon TE, Levin NW, Port FK. Association of serum phosphorus and calcium x phosphate product with mortality risk in chronic hemodialysis patients: a national study. Am J Kidney Dis. 1998;31:607–17. https://doi.org/10.1053/ajkd.1998.v31.pm9531176.
Greene SV, Falciglia G, Rademacher R. Relationship between serum phosphorus levels and various outcome measures in adult hemodialysis patients. J Ren Nutr. 1998;8:77–82. https://doi.org/10.1016/s1051-2276(98)90046-2.
Marchais SJ, Metivier F, Guerin AP, London GM. Association of hyperphosphataemia with haemodynamic disturbances in end-stage renal disease. Nephrol Dial Transplant. 1999;14:2178–83. https://doi.org/10.1093/ndt/14.9.2178.
Kato C, Fujii N, Miyakoshi C, Asada S, Onishi Y, Fukuma S, et al. Changes in 3-month mineral and bone disorder patterns were associated with all-cause mortality in prevalent hemodialysis patients with secondary hyperparathyroidism. BMC Nephrol. 2020;21(1):432. https://doi.org/10.1186/s12882-020-02088-x.
Koizumi M, Komaba H, Nakanishi S, Fujimori A, Fukagawa M. Cinacalcet treatment and serum FGF23 levels in haemodialysis patients with secondary hyperparathyroidism. Nephrol Dial Transplant. 2012;27:784–90. https://doi.org/10.1093/ndt/gfr384.
Ogata H, Takeshima A, Ito H. An update on phosphate binders for the treatment of hyperphosphatemia in chronic kidney disease patients on dialysis: a review of safety profiles. Expert Opin Drug Saf. 2022;21:1–9. https://doi.org/10.1080/14740338.2022.2044472.
Chiu YW, Teitelbaum I, Misra M, de Leon EM, Adzize T, Mehrotra R. Pill burden, adherence, hyperphosphatemia, and quality of life in maintenance dialysis patients. Clin J Am Soc Nephrol. 2009;4:1089–96. https://doi.org/10.2215/CJN.00290109.
Akizawa T, Sato Y, Ikejiri K, Kanda H, Fukagawa M. Effect of tenapanor on phosphate binder pill burden in hemodialysis patients. Kidney Int Rep. 2021;6:2371–80. https://doi.org/10.1016/j.ekir.2021.06.030.
Ogata H, Fukagawa M, Hirakata H, et al. Design and baseline characteristics of the LANDMARK study. Clin Exp Nephrol. 2017;21:531–7. https://doi.org/10.1007/s10157-016-1310-8.
Funding
This analysis received no funding. The LANDMARK study was funded by Bayer Yakuhin Ltd.
Author information
Authors and Affiliations
Consortia
Contributions
KY, TM, HM and HO had roles in the study design and statistical analysis. KY, TM, and HO had roles in the drafting of the manuscript. KY, TM, MF, TA, HM, TS, HI, HO and NU had roles in the critical revision of the manuscript for important intellectual content.
Corresponding author
Ethics declarations
Conflict of interest
TM reported receiving consultancy fees from Zeon Medical Inc.; research grants from Boston Scientific; and speaker fees from Abbott Vascular, Cathworks, and Boston Scientific. MF reported receiving lecture fees from Bayer Yakuhin, Kyowa Kirin, Kissei, Ono Pharmaceutical and Sanwa Kagaku; and grants from Kyowa Kirin, Chugai, and Torii. TA reported receiving consulting and lecture fees from Bayer Yakuhin, Astellas, Kyowa Kirin, Kissei Pharmaceutical, Ono Pharmaceutical, Fuso Pharmaceutical Industry, and Torii Pharmaceutical; consulting fees from GlaxoSmithKline, JT Pharmaceutical, Nipro Corporation, Otsuka, and Sanwa Kagaku; and lecture fees from Chugai Pharmaceutical and Mitsubishi Tanabe Pharma. HO reported receiving lecture fees from Bayer Yakuhin, Kyowa Kirin, Torii Pharmaceutical, Otsuka, Kissei Pharmaceutical, Mitsubishi Tanabe Pharma, Sumitomo Dainippon Pharm, Daiichi Sankyo, Kowa, and Ono Pharmaceutical; grants from Torii Pharmaceutical and Ono Pharmaceutical; and consulting fees from YL Biologics. NU reported receiving consultancy fees from TOA EIYO, Meiji Seika Pharma, AstraZeneca, Daiichi Sankyo Company Ltd, Eisai Co., Ltd, Sanwa Kagaku Kenkyusho Co., Ltd, Kyorin Pharmaceutical Co., Ltd., Sanofi K.K., NapaJen Pharma, GC Showayakuhin Corporation, Ito Life Science, Takata Pharmaceutical Co., Ltd., and SSP Co., Ltd.; and lecture fees from TOA EIYO, Meiji Seika Pharma, AstraZeneca, Daiichi Sankyo Company Ltd, and NapaJen Pharma. No other disclosures were reported.
Ethical approval
All procedures performed in the LANDMARK study involving human participants were in accordance with the ethical standards of the institutional and/or national research committee at which the studies were conducted and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. This post-hoc analysis was approved by the ethics committee of Showa University (approval number 21-059-B).
Informed consent
Informed consent was obtained from all individual participants included in the LANDMARK study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
About this article
Cite this article
Yoshida, K., Mizukami, T., Fukagawa, M. et al. Target phosphate and calcium levels in patients undergoing hemodialysis: a post-hoc analysis of the LANDMARK study. Clin Exp Nephrol 27, 179–187 (2023). https://doi.org/10.1007/s10157-022-02288-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10157-022-02288-9