Abstract
Background
Coronary artery calcification (CAC) is predictive of cardiovascular events. We assessed whether a non-calcium-based phosphate binder, lanthanum carbonate (LC), could delay CAC progression compared with a calcium-based phosphate binder, calcium carbonate (CC), in hemodialysis patients.
Methods
This was a subsidiary of the LANDMARK study, which is a multicenter, open-label, randomized control study comparing LC and CC for cardiovascular events among Japanese hemodialysis patients with hyperphosphatemia who were at risk of vascular calcification. Participants were randomly assigned (1:1) to receive LC or CC. The changes in the total Agatston score of CAC 2 years from baseline were the primary outcome. Secondary outcomes included the changes in the total Agatston score at 1 year from baseline and the changes in serum phosphate, corrected calcium, and intact parathyroid hormone concentrations.
Results
Of 239 patients, 123 comprised the full analysis set. The median daily drug dose (mg) was 750 [interquartile range (IQR), 750‒1500] in the LC group and 3000 (IQR, 3000‒3000) in the CC group; it remained constant throughout the study period. There was no significant difference in the change in total Agatston score from baseline to 2 years between the LC and CC groups [368 (95% confidence interval, 57–680) in the LC group vs. 611 (105–1118) in the CC group; difference, 243 (− 352–838)].
Conclusions
LC-based treatment for hyperphosphatemia did not delay CAC for 2 years compared with CC-based treatment in hemodialysis patients with at least one risk factor for vascular calcification.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Vascular calcification is significantly associated with increased cardiovascular events among patients with or without chronic kidney disease (CKD) and is caused by various factors [1,2,3,4,5,6,7]. In patients with CKD, both hyperphosphatemia and calcium burden play a critical role in the pathogenesis of vascular calcification, in addition to diabetes, aging, hyperlipidemia, inflammation, and uremic toxins [8, 9]. Although phosphate binders are essential for managing hyperphosphatemia among dialysis patients, calcium-based phosphate binders accelerate vascular calcification by increasing the calcium burden, as compared with non-calcium-based phosphate binders. Consequently, the use of calcium-based phosphate binders might increase the risk for cardiovascular events.
The updated Kidney Disease: Improving Global Outcomes (KDIGO) 2017 Clinical Practice Guideline for CKD-mineral and bone disorder (MBD) recommends restricting the dose of calcium-based phosphate binders in adults with CKD G3a-G5D [10]. However, there is insufficient evidence to conclusively demonstrate that non-calcium-based phosphate binders improve vascular calcification progression and cardiovascular risk compared with calcium-based phosphate binders [11]. A recent randomized control trial did not show the superiority of lanthanum carbonate (LC) over calcium carbonate (CC) in reducing cardiovascular events among hemodialysis patients with vascular risk [12].
We conducted a randomized controlled trial comparing the progression of coronary artery calcification (CAC), which is the most reliable index of vascular calcification [13, 14], between LC and CC in hemodialysis patients with hyperphosphatemia, with at least one risk factor for vascular calcification.
Patients and methods
Study design and patients
The LANDMARK-SS is a subsidiary study of the LANDMARK study [12], which is an academic investigator-led, prospective, randomized, open-label, endpoint-blinded, controlled trial comparing composite cardiovascular events between LC and CC groups among dialysis patients with vascular calcification risk (UMIN000006816). The trial protocol of the LANDMARK study was previously published [15] and was approved by the institutional review board.
A total of 2,309 patients were enrolled in the LANDMARK study, and patients who provided written informed consent for measuring CAC were included in the LANDMARK-SS study at 23 sites across Japan. This study aimed to assess the difference in the progression of CAC between LC-based and CC-based treatment for hyperphosphatemia in hemodialysis patients with at least one risk factor for vascular calcification.
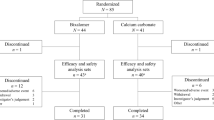
Enrolled patients were randomly assigned (1:1) to the LC or CC groups using a web-based randomizer provided by the trial data center. Randomization was performed using the minimization method with age (≤ 65 vs. > 65 years), sex, diabetes (absence vs. presence), and study site. During the study, patients were managed based on the Clinical Practice Guideline for the Management of CKD-MBD published by the Japanese Society for Dialysis Therapy (JSDT) [16]. The treatment regimen is shown in Fig. 1. Changes in the daily dosages of LC and CC, concomitant treatment for CKD-MBD, serum levels of phosphate, corrected calcium, calcium × phosphate product, intact parathyroid hormone (iPTH), and alkaline phosphatase (ALP) during the study period were recorded.
Treatment regimens. In the LC group, patients were initially administered a dose of 750 mg/day (3 times immediately after meals) or the previously used dose. To achieve a target serum phosphate concentration of 3.5‒6.0 mg/dL (JSDT guidelines [14]), patients were titrated with up to a maximum of 2250 mg/day. If the phosphate concentration was not achieved at 2250 mg/day or the maximum tolerated dose, other non-Ca-based phosphate binders were added. CC use was not prohibited in the LC group. In the CC group, patients were administered a dose of 3000 mg/day (3 times immediately after meals) or the previously used dose. To achieve the desired phosphate concentration, patients were titrated, and if the phosphate concentration was not achieved with the maximum tolerated dose, non-calcium-based phosphate binders were added. LC use was not prohibited in the CC group. JSDT Japanese Society for Dialysis Therapy, Ca calcium, LC lanthanum carbonate, CC calcium carbonate, P serum phosphate
Eligible patients were included in the study protocol (Online Resource 1). In brief, patients undergoing maintenance hemodialysis (duration ≥ 3 months), with at least one vascular calcification risk (age ≥ 65 years, menopause, or type II diabetes mellitus), serum iPTH levels ≤ 240 pg/mL, and life expectancies ≥ 1 year were enrolled in the LANDMARK study. The exclusion criteria are shown in Table S1 (Online Resource 2).
The primary outcome was defined as the change in the total Agatston score of CAC [17] 2 years after baseline. The secondary outcomes were the changes in the total Agatston score at 1 year from baseline and those in log-transformed total Agatston scores at 1 and 2 years from baseline. We also assessed the changes in serum phosphate, corrected calcium, and iPTH concentrations during the study period. The safety evaluation was not performed in this study because it was comprehensively assessed in the main study [12, 15].
In this subsidiary study, as well as in the LANDMARK study, regular safety surveillance was performed by an independent data and safety monitoring committee. Data were collected using electronic case report forms provided by the investigators, and an independent trial data center, the Translational Research Center for Medical Innovation (Kobe, Japan), provided data management and statistical analysis services.
Coronary artery calcification score measurement
The CAC score was measured at study entry, and thereafter at 12 and 24 months, at each site, using multi-detector row computed tomography (MDCT). Quantitative CAC scoring was calculated according to a previously published method [17]. The Agatston score was used to aggregate all calcification scores within the area of interest. We assessed changes in the Agatston score from baseline among all patients, as well as those with a total Agatston score of ≥ 30, because a previous study suggested that patients with absent or low CAC scores were unlikely to have progressive CAC over the next few years [18].
Sample size
As no prior data directly compared changes in CAC (Agatston) score 2 years after registration of the LC and CC groups, we assumed a sample size based on results from past randomized controlled trials comparing the progression of Agatston scores between a non-calcium-based phosphate binder, sevelamer hydrochloride, and calcium-based phosphate binders among patients receiving hemodialysis [19, 20]. Details are provided in the study protocol (Online Resource 1).
Statistical analyses
The full analysis set (FAS) included the patients enrolled in this study, excluding patients who were not treated with the study drug, did not undergo MDCT, and had no measurement results for the CAC score. The per-protocol set (PPS) was based on the FAS, excluding patients who received CC combination therapy in the LC allocation group or LC combination therapy in the CC allocation group, had missing CAC score measurements in some points, or did not complete the 2-year observation. Changes in the total Agatston score from baseline were analyzed using a mixed-effects model with repeated measures (MMRM), with time points of 1 and 2 years as factors, the baseline value as a covariate, and patients as a random effect. Imputation of missing values was not performed in the MMRM analysis.
As a sensitivity analysis, an analysis of covariance was performed using the values at the time of the final measurement at 1 and 2 years as the last observation carried forward (LOCF) analysis, with the amount of change as the objective variable and the baseline value as the covariate. For logarithmic conversion of the total Agatston score, we used the natural logarithm. Analysis of the secondary endpoints was similar to that of the primary endpoints. Data are expressed as means (standard deviations) or medians (interquartile ranges) for continuous variables and as frequencies and percentages for discrete variables. The significance level was set at P < 0.05 (two-tailed). All analyses were predefined in the statistical analysis plan (Online Resource 1) before the database was locked and were conducted using SAS version 9.3 (SAS Institute Inc, Cary, NC, USA.).
Results
Patients
The study was conducted between November 2011 and July 2016. A total of 239 patients (121 and 118 in the LC and CC groups, respectively) enrolled in the LANDMARK study were registered in the present trial (Fig. S1, in Online Resource 2). The numbers of eligible patients for the FAS were 61 and 62 in the two groups, respectively. We analyzed 123 patients as the FAS, and 87 consecutive patients were included in the PPS. Unfortunately, the study was unable to recruit the prespecified target number of patients because the main LANDMARK study limited the study period as specified in the study protocol. This prevented us from extending the deadline and increasing the number of patients to be included in the current study.
The average age and dialysis vintage were 67.7 and 6.9 years, respectively; of all patients, 43.9% were female, and 55.2% were diabetic. The baseline demographic and medical characteristics of patients were well-balanced between the two groups (Table 1) and did not differ from those of patients enrolled in the LANDMARK study (n = 2135). The prevalence rates of diabetes, hypertension, and hyperlipidemia were similar between the two groups, and the use of concomitant drugs, including vitamin D receptor activators (VDRAs), cinacalcet, renin-angiotensin system inhibitors, aspirin, and statin, was comparable (Table 1).
The daily doses of LC and CC over time are presented in Table S2 (Online Resource 2). The daily doses of LC and CC were 750 and 3000 mg, respectively, during the study period. Concomitant treatments, including other non-calcium-based phosphate binders, VDRAs, and cinacalcet, are described in Table S3 (Online Resource 2). The number of sevelamer users in both groups was comparable during the study period. The number of VDRA users gradually increased in the LC group and that of cinacalcet users increased in the CC group.
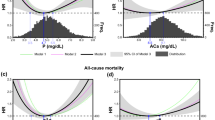
Coronary artery calcification
The distribution of the total Agatston score of CAC at baseline was similar between the LC and CC groups (P = 0.8) (Fig. S2, in Online Resource 2). There was no significant difference in the Agatston score of the calcification of the total coronary artery or each branch at baseline (Table S4, in Online Resource 2). Figure 2 shows the changes in the total Agatston score over time. Changes in the least square mean of the total CAC score from baseline in both groups are illustrated in Fig. 3a–d. In the FAS model, the scores at 12 or 24 months significantly increased from baseline in both groups {LC group, month 12: + 360 [95% confidence interval (CI, 180–541], month 24: + 368 [57–680]; CC group, month 12: + 221 [77–366], month 24: + 611 [105–1118]} (Fig. 3a). In the PPS model, although the score at 24 months increased significantly from baseline in the CC group [591 (7–1175), P = 0.05], it did not increase in the LC group [+ 230 (− 141–600), P = 0.2] (Fig. 3b). The between-group differences in scores at 12 and 24 months were not significant (P = 0.2 and P = 0.4, respectively; Table 2). This result was consistent with those of other models. In addition, the total Agatston score at the LOCF was similar between the 2 groups (P = 0.5; Table 2). In other models, there was no significant difference in the total Agatston score of CAC from baseline between the LC and CC groups. There were no significant differences in the change in Agatston score of each branch from baseline at 12 and 24 months and LOCF between the two treatment arms (Table S5, in Online Resource 2). The results were consistent with those from the prespecified analysis stratified by various factors at baseline (Table S6, in Online Resource 2).
Changes in total Agatston score from baseline during the study period are shown as least square means ± 95% confidence intervals (a–d). In various models, the differences between both groups at 12 or 24 months were compared by a mixed-effects model repeated measure with time point, treatment, and interaction as fixed effects, previous values as a covariate, and patients as a mixed-effect. Differences between the LC and CC groups at LOCF were compared by analysis of covariance, with previous values as covariate and treatment as a factor. LC lanthanum carbonate, CC calcium carbonate, LOCF last observation carried forward, LS mean, least square mean, SE standard error
CKD-MBD markers
Changes in the serum concentrations of phosphate, corrected calcium, calcium × phosphate products, and iPTH are illustrated in Fig. 4. Differences in serum phosphate concentrations at 6 months and serum corrected calcium concentrations at 3 and 6 months between the two treatments were significant [phosphate: − 0.49 mg/dL (95% CI − 0.93 to − 0.04 mg/dL) at 6 months, P = 0.03; corrected calcium: 0.21 (0.03–0.39) at 3 months, P = 0.02 and 0.29 (0.08–0.49) at 6 months, P = 0.01] (Fig. 4a-2, b-2). There were no significant differences in the calcium × phosphate products at any measurement between the two groups (Fig. 4c-2). Although there was a significant difference in serum iPTH concentrations at 3, 6, and 12 months between the LC and CC groups, no significant difference was observed at 24 months [− 23.5 (− 66.9–19.9), P = 0.3] (Fig. 4d-2).
Changes in serum phosphate (P) (a-1), corrected calcium (Ca) (b-1), Ca × P products (c-1), and intact parathyroid hormone (iPTH) (d-1) concentrations are shown as medians ± IQRs in the column. The column shows differences in serum P (a-2), corrected Ca (b-2), Ca × P products (c-2), and iPTH (d-2) concentrations between both groups over time. IQR interquartile range, LSmean least square mean, SE standard error
Discussion
We assessed whether a non-calcium-based phosphate binder, LC, delayed CAC progression compared with a calcium-based phosphate binder, CC, in hemodialysis patients. We found that LC-based treatment for hyperphosphatemia did not delay CAC for 2 years, as compared with CC-based treatment, in hemodialysis patients with at least one risk factor for vascular calcification.
The recently updated KDIGO guidelines for CKD-MBD suggest restricting the dose of calcium-based phosphate binders among adult patients with CKD because their use is likely to accelerate vascular calcification, which is a predictive factor for cardiovascular disease [10]. Previous randomized controlled trials reported that sevelamer delayed the progression of aortic calcification or CAC more than calcium-based phosphate binders did in hemodialysis patients [19, 21, 22]. Because sevelamer is the most widely used non-calcium-based phosphate binder in clinical practice and has low-density-lipoprotein cholesterol-lowering and anti-inflammatory actions, which other classes of non-calcium-based phosphate binders do not have [23], the effect of sevelamer on vascular calcification might not always be attributable to its less calcemic property. LC is unlikely to inhibit vascular calcification by any other means than by its phosphate-lowering action.
Several randomized controlled trials have shown that LC delays the progression of the total CAC score in hemodialysis patients, as compared with CC [24,25,26]. In contrast, LC does not suppress calcification of the superficial femoral artery compared with calcium-based phosphate binders, as assessed by computed tomography [27]. Wada et al. reported that annual changes in the aortic calcification index between LC and CC were comparable among hemodialysis patients with type II diabetes mellitus [28]. A Cochrane Database systemic review from 2018 reported that the suppression effect of non-calcium-based phosphate binders on the progression of the CAC score, compared with that of calcium-based phosphate binders, remained unelucidated [11].
This study demonstrated that there was no significant difference in the progression of the CAC score between the LC- and CC-treated groups of hemodialysis patients with at least one vascular calcification risk during 2 years. The CAC score at baseline and annual changes in the CAC score during the study were not considerably different from those in previous studies involving hemodialysis patients [22, 25, 29]. Baseline or annual changes in the total CAC score were comparable to past studies that assessed CAC score progression among hemodialysis patients [22, 24, 25, 30]. In terms of biochemical markers of CKD-MBD, serum phosphate levels increased and serum calcium levels decreased significantly more in the LC group than in the CC group within 6 months from the start of the study. However, there was no significant difference in serum calcium or phosphate levels between the groups at 12 and 24 months; the calcium × phosphate products, which are associated with vascular calcification, were comparable throughout the study period. Recent clinical practice guidelines recommend aggressively maintaining a target range of serum phosphate concentration, without increasing the calcium burden [10, 16]. The JSDT guidelines recommend restricting the maximum dose of CC to no more than 3000 mg/day. In this study, the concomitant use of non-calcium-based phosphate binders, other than LC, was allowed. The median dose of CC in the present trial was lower than those in most previous studies [22, 24, 25, 30]. CC should be restrictively titrated to avoid hyperphosphatemia, as well as hypercalcemia, according to the JSDT guidelines and recently accumulated evidence. In this study, concomitant use of sevelamer, which is a non-calcium-based phosphate binder, was allowed in both groups. However, the number of sevelamer users was comparable during the study period except for that at 24 months (Table S2, in Online Resource 2). VDRA use might be associated with the progression of vascular calcification due to increased intestinal calcium absorption. In contrast, cinacalcet ameliorated CAC progression, with a decrease in the level of serum phosphate, calcium concentrations, and calcium × phosphate products, compared to VDRA [29]. VDRA use gradually increased in the LC group; cinacalcet use was more prevalent in the CC group than in the LC group (Table S2, in Online Resource 2). Taken together, both phosphate binders and concomitant drugs may affect CAC progression. Currently, various drugs are clinically available for CKD-MBD management.
This study has several strengths. First, although the targeted number of analyzed patients was not achieved, the number of analyzed patients was larger than those in previous randomized controlled trials comparing the total CAC score between LC and CC. In addition, compared to previous studies, the 24-month study duration was long enough to assess CAC progression [22, 23, 28]. Second, the LANDMARK-SS study was a subsidiary study of the LANDMARK study, which compared composite cardiovascular events between LC and CC among hemodialysis patients with at least one vascular calcification risk. It has demonstrated no significant difference in cardiovascular events between the two phosphate binders [12]. In the near future, we plan to assess the relationship between CAC progression and cardiovascular events by cross-referencing the results from these two randomized controlled trials.
This trial also has some limitations. First, the prespecified target number of enrolled patients for the primary endpoint was not achieved. If the assumed number of study patients were enrolled, the superiority of either treatment for CAC progression may have been detected. Moreover, all participants were recruited from 23 facilities in Japan. Therefore, it is unclear whether the findings from this study could be adequately generalized to hemodialysis patients in other areas. As previously shown, cardiovascular morbidity and mortality among not only the general population but also hemodialysis patients in Japan were considerably lower than those in Western countries [31]. In general, dietary calcium intake in Asian and African countries is reported to be markedly lower than that in Western countries [32]. Although a dietary survey was not performed in this study, dietary calcium intake might be lower in this study than in previous studies in Western countries. Dialysate calcium concentrations also affect the calcium balance. Interestingly, prespecified stratified analysis revealed that CAC progression was comparable between the two groups in the higher dialysate calcium concentration group (≥ 2.8 mEq/L), probably increasing calcium influx into the body (Table S6, in Online Resource 2). As discussed above, baseline or annual changes in the total CAC score were comparable with those in previous trials. However, patients with CAC > 1000, who might behave refractory to any intervention to reduce progression, accounted for more than 30% of the study population, perhaps reflecting that the mean dialysis vintage was as long as 7 years. We defined the study population as patients with vascular calcification risks, including age ≥ 65 years, post-menopause, and diabetes, based on the results of previous studies [12, 15], but whether this was justified needs to be verified.
Second, this trial did not make a head-to-head comparison between LC alone and CC alone, and adjunctive sevelamer use was allowed in both groups. In the real world, combined treatment with more than phosphate binders, regardless of whether calcium is present, is used to achieve serum phosphate levels within the targeted range. Concomitant sevelamer use may affect the progression of CAC. No difference in concomitant use of sevelamer other than at month 24 was statistically significant between the two groups (Table S3, in Online Resource 2). In addition, we did not evaluate changes in calcification progression of arteries other than the coronary artery and heart valves. Therefore, the effects of LC- and CC-based treatments for hyperphosphatemia remain unknown.
In conclusion, we found that LC-based treatment for hyperphosphatemia did not delay CAC over 2 years, as compared with CC-based treatment, in hemodialysis patients with at least one vascular calcification. This provides further evidence that non-calcium-based phosphate binders do not suppress the progression of vascular calcification and cardiovascular risk as compared with calcium-based phosphate binders.
References
Goodman WG. Vascular calcification in end-stage renal disease. J Nephrol. 2002;15(Suppl 6):S82–5.
Goodman WG, London G, Amann K, et al. Vascular calcification in chronic kidney disease. Am J Kidney Dis. 2004;43:572–9.
London GM, Marchais SJ, Guérin AP, Métivier F. Arteriosclerosis, vascular calcifications and cardiovascular disease in uremia. Curr Opin Nephrol Hypertens. 2005;14:525–31.
Block GA, Raggi P, Bellasi A, Kooienga L, Spiegel DM. Mortality effect of coronary calcification and phosphate binder choice in incident hemodialysis patients. Kidney Int. 2007;71:438–41.
Russo D, Corrao S, Battaglia Y, et al. Progression of coronary artery calcification and cardiac events in patients with chronic renal disease not receiving dialysis. Kidney Int. 2011;80:112–8.
Floege J, Ketteler M. Vascular calcification in patients with end-stage renal disease. Nephrol Dial Transplant. 2004;19(Suppl 5):V59-66.
Yamada K, Fujimoto S, Nishiura R, et al. Risk factors of the progression of abdominal aortic calcification in patients on chronic haemodialysis. Nephrol Dial Transplant. 2007;22:2032–7.
Amann K. Media calcification and intima calcification are distinct entities in chronic kidney disease. Clin J Am Soc Nephrol. 2008;3:1599–605.
Shroff R, Long DA, Shanahan C. Mechanistic insights into vascular calcification in CKD. J Am Soc Nephrol. 2013;24:179–89.
Kidney disease: Improving global outcomes CKD-MBD Working Group. KDIGO clinical practice guideline update for the diagnosis, evaluation, prevention, and treatment of chronic kidney disease-mineral and bone disorder (CKD-MBD). Kidney Int Suppl (2011). 2017;7:1–59.
Ruospo M, Palmer SC, Natale P, et al. Phosphate binders for preventing and treating chronic kidney disease-mineral and bone disorder (CKD-MBD). Cochrane Database Syst Rev. 2018;8:CD006023.
Ogata H, Fukagawa M, Hirakata H, et al. Effect of treating hyperphosphatemia with lanthanum carbonate vs calcium carbonate on cardiovascular events in patients with chronic kidney disease undergoing hemodialysis: the LANDMARK randomized clinical trial. JAMA. 2021;325:1946–54.
Budoff MJ, Hokanson JE, Nasir K, et al. Progression of coronary artery calcium predicts all-cause mortality. JACC Cardiovasc Imaging. 2010;3:1229–36.
Karohl C, D’Marco Gascón L, Raggi P. Noninvasive imaging for assessment of calcification in chronic kidney disease. Nat Rev Nephrol. 2011;7:567–77.
Ogata H, Fukagawa M, Hirakata H, et al. Design and baseline characteristics of the LANDMARK study. Clin Exp Nephrol. 2017;21:531–7.
Fukagawa M, Yokoyama K, Koiwa F, et al. Clinical practice guideline for the management of chronic kidney disease-mineral and bone disorder. Ther Apher Dial. 2013;17:247–88.
Agatston AS, Janowitz WR, Hildner FJ, et al. Quantification of coronary artery calcium using ultrafast computed tomography. J Am Coll Cardiol. 1990;15:827–32.
Bellasi A, Kooienga L, Block GA, et al. How long is the warranty period for nil or low coronary artery calcium in patients new to hemodialysis? J Nephrol. 2009;22:255–62.
Treat to Goal Working Group, Chertow GM, Burke SK, Raggi P. Sevelamer attenuates the progression of coronary and aortic calcification in hemodialysis patients. Kidney Int. 2002;62:245–52.
Qunibi W, Moustafa M, Muenz LR, et al. A 1-year randomized trial of calcium acetate versus sevelamer on progression of coronary artery calcification in hemodialysis patients with comparable lipid control: the calcium acetate Renagel Evaluation-2 (CARE-2) study. Am J Kidney Dis. 2008;51:952–65.
Block GA, Spiegel DM, Ehrlich J, et al. Effects of sevelamer and calcium on coronary artery calcification in patients new to hemodialysis. Kidney Int. 2005;68:1815–24.
Kakuta T, Tanaka R, Hyodo T, et al. Effect of sevelamer and calcium-based phosphate binders on coronary artery calcification and accumulation of circulating advanced glycation end products in hemodialysis patients. Am J Kidney Dis. 2011;57:422–31.
Patel L, Bernard LM, Elder GJ. Sevelamer versus calcium-based binders for treatment of hyperphosphatemia in CKD: a meta-analysis of randomized controlled trials. Clin J Am Soc Nephrol. 2016;11:232–44.
Toida T, Fukudome K, Fujimoto S, et al. Effect of lanthanum carbonate vs. calcium carbonate on serum calcium in hemodialysis patients: a crossover study. Clin Nephrol. 2012;78:216–23.
Zhang C, Wang S, Zhao S, Zhang X. Effect of lanthanum carbonate on coronary artery calcification and bone mineral density in maintenance hemodialysis patients with diabetes complicated with adynamic bone disease: a prospective pilot study. Medicine. 2017;96:e8664.
Fujii H, Kono K, Nakai K, et al. Effects of lanthanum carbonate on coronary artery calcification and cardiac abnormalities after initiating hemodialysis. Calcif Tissue Int. 2018;102:310–20.
Toussaint ND, Lau KK, Polkinghorne KR, Kerr PG. Attenuation of aortic calcification with lanthanum carbonate versus calcium-based phosphate binders in haemodialysis: a pilot randomized controlled trial. Nephrology. 2011;16:290–8.
Wada K, Wada Y. Evaluation of aortic calcification with lanthanum carbonate vs. calcium-based phosphate binders in maintenance hemodialysis patients with type 2 diabetes mellitus: an open-label randomized controlled trial. Ther Apher Dial. 2014;18:353–60.
Raggi P, Chertow GM, Torres PU, et al. The ADVANCE study: a randomized study to evaluate the effects of cinacalcet plus low-dose vitamin D on vascular calcification in patients on hemodialysis. Nephrol Dial Transplant. 2011;26:1327–39.
Dialysis Clinical Outcomes Revisited Investigators, Suki WN. Effects of sevelamer and calcium-based phosphate binders on mortality in hemodialysis patients: Results of a randomized clinical trial. J Ren Nutr. 2008;18:91–8.
Stirnadel-Farrant HA, Karaboyas A, Cizman B, et al. Cardiovascular event rates among hemodialysis patients across geographical regions-A snapshot from the dialysis outcomes and practice patterns study (DOPPS). Kidney Int Rep. 2019;4:864–72.
Kumssa DB, Joy EJ, Ander EL, et al. Dietary calcium and zinc deficiency risks are decreasing but remain prevalent. Sci Rep. 2015;5:10974.
Acknowledgements
We acknowledge the contribution of the LANDMARK Investigators and Committees.
Funding
This study was supported by Bayer Yakuhin, Ltd. Bayer Yakuhin, Ltd. had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication. However, the company was kept informed of the progress of the study. There were no confidentiality agreements regarding the data.
Author information
Authors and Affiliations
Consortia
Contributions
Research idea and study design: MF, HH, TA; data acquisition: TK; data analysis/interpretation: HO, MF, HH, TK, TA; statistical analysis: HO, TK; drafting of this manuscript: HO, TK; supervision or mentorship: MF, HH, TA. Each author contributed toward important intellectual content during manuscript drafting or revision and agrees to be personally accountable for the individual’s contributions and to ensure that questions pertaining to the accuracy or integrity of any portion of the work, even one in which the author was not directly involved, are appropriately investigated and resolved, including with documentation in the literature if appropriate.
Corresponding author
Ethics declarations
Conflict of interest
Dr Ogata reported receiving lecture fees from Bayer Yakuhin, Kyowa Kirin, Torii Pharmaceutical, Otsuka, Kissei Pharmaceutical, Mitsubishi Tanabe Pharma, Sumitomo Dainippon Pharm, Daiichi Sankyo, Kowa, Ono Pharmaceutical; grants from Torii Pharmaceutical and Ono Pharmaceutical; and consulting fees from YL Biologics. Dr Fukagawa reported receiving personal fees from Bayer Yakuhin and grants from Kyowa Kirin. Dr Hirakata reported receiving personal fees from Kyowa-Kirin, Chugai Pharma, Torii, Japan Tobacco, and Ono Yakuhin. Dr Kagimura reported receiving grants from Bayer Yakuhin. Dr Akizawa reported receiving consulting and lecture fees from Bayer Yakuhin, Astellas, Kyowa Kirin, Kissei Pharmaceutical, Ono Pharmaceutical, Fuso Pharmaceutical Industry, Torii Pharmaceutical; consulting fees from GlaxoSmithKline, JT Pharmaceutical, Nipro Corporation, Otsuka, and Sanwa Chemical; and lecture fees from Chugai Pharmaceutical. No other disclosures were reported.
Ethical approval
The trial protocol of the LANDMARK study was previously published and was approved by the Institutional Review Board. All patients enrolled in this LANDMARK-SS study provided written informed consent.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
About this article
Cite this article
Ogata, H., Fukagawa, M., Hirakata, H. et al. Effect of lanthanum carbonate and calcium carbonate on the progression of coronary artery calcification among hemodialysis patients with vascular calcification risk: a randomized controlled trial. Clin Exp Nephrol 26, 1223–1232 (2022). https://doi.org/10.1007/s10157-022-02270-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10157-022-02270-5