Abstract
Background
Inhibitors of vascular endothelial growth factor (VEGF)-VEGF receptor 2 (VEGFR2) signaling, such as bevacizumab (Bmab), are used for the treatment of various advanced cancers. However, these inhibitors induce renal thrombotic microangiopathy (TMA). Recently, two European cohort studies showed a distinctive histopathological pseudothrombotic pattern different from TMA in Bmab-treated patients.
Methods
We analyzed 9 renal biopsies from proteinuric cancer patients treated with VEGF-VEGFR2 inhibitors in our Japanese cohort. Clinical and laboratory features were also assessed in these patients.
Results
All 9 patients had moderate to heavy proteinuria with normal or slightly elevated serum creatinine levels. On light microscopy, a patchy pattern of hemispherical/spherical lesions along glomerular capillary walls was a characteristic finding. On immunofluorescence microscopy, staining for immunoglobulins (IgM dominant) at varying intensities was observed mainly along glomerular capillary walls. Especially, hemispherical/spherical positive staining for immunoglobulins was a characteristic pattern. Immunohistochemical studies showed positive staining for immunoglobulins and negative staining for CD61-positive platelets in capillary hemispherical/spherical lesions and positive VEGF staining in podocytes. On electron microscopy, variably electron-dense material in dilated glomerular capillaries and partial effacement of podocyte foot processes were observed. After the withdrawal of VEGF-VEGFR2 inhibitors, proteinuria improved without any specific treatment in 8 patients.
Conclusions
Histopathological findings in our patients treated with VEGF-VEGFR2 inhibitors were consistent with those observed in the recently described new form of Bmab-associated hyaline occlusive glomerular microangiopathy. This form should be considered in proteinuric cancer patients treated with VEGF-VEGFR2 inhibitors. Discontinuing VEGF-VEGFR2 inhibitors may lead to improvement of glomerular microangiopathy induced by these drugs.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Vascular endothelial growth factor (VEGF), also referred to as VEGF-A, is an essential growth factor for angiogenesis [1, 2]. There are at least 6 VEGF isoforms containing different numbers of amino acids, termed VEGF121, VEGF145, VEGF165, VEGF183, VEGF189, and VEGF206 [2]. The biological effects of VEGF isoforms are specifically mediated by two tyrosine kinase receptors, VEGF receptors 1 and 2 (VEGFR1 and VEGFR2), which are expressed almost exclusively in endothelial cells [1, 2].
As VEGF-VEGFR2 signaling plays an important role in cancer growth and metastasis, inhibition of this signaling is a common therapeutic strategy in current oncology [3]. VEGF-VEGFR2 inhibitors are classified as VEGF antibodies (such as Bevacizumab: Bmab), VEGF trap (Aflibercept: AFB), and VEGFR2 antibodies (such as Ramucirumab: RAM) [3]. It has been reported that Bmab increases risk for severe proteinuria in cancer patients [3, 4]. In 2008, Eremina et al. [5] reported that 6 cancer patients treated with Bmab developed glomerular disease characteristic of thrombotic microangiopathy (TMA). They suggested that glomerular injury in these patients is probably due to direct targeting of VEGF by anti-angiogenetic therapy, based on observations in a murine model. Thereafter, several studies have shown that the most notable morphological characteristic in Bmab-induced renal injury is glomerular TMA [6,7,8]. In contrast, tyrosine kinase inhibitors of VEGFR2, such as sunitinib [3], induce mainly minimal change disease/focal and segmental glomerulosclerosis [6, 8].
Recently, two European cohort studies showed a distinct Bmab-associated glomerulopathy with nephrotic range proteinuria (in most cases) [9, 10] different from the known Bmab-associated TMA [5,6,7,8]. This new form of Bmab-associated glomerulopathy is characterized by periodic acid-Schiff (PAS)-positive hyaline pseudothrombi on light microscopy, positive staining for immunoglobulins and complements on immunofluorescence microscopy, and variably electron-dense pseudothrombi in the dilated glomerular capillaries on electron microscopy [9, 10]. Person et al. [10] proposed the term “Bmab-associated glomerular microangiopathy” for this unique hyaline occlusive glomerulopathy. They suggested that this form can be diagnosed by light microscopy and is an important differential diagnosis in cancer patients with nephrotic syndrome (NS).
In the present Japanese single-center cohort study, we examined clinicopathological features in 9 patients with proteinuria who were treated with VEGF-VEGFR2 inhibitors, including Bmab, and observed characteristic findings matched with those in the recently proposed Bmab-associated glomerular microangiopathy [10] in all cases.
Patients and methods
Patients
This study was based on the renal histological records (from January 2017 to December 2020) of 962 patients studied at Akita University Hospital and its affiliated hospitals. Among 962 Japanese patients, 9 cancer patients treated with VEGF-VEGFR2 inhibitors were diagnosed with drug-associated hyaline occlusive glomerular microangiopathy as described below, giving a prevalence rate of 0.94% among all renal biopsies.
Clinicopathological analysis
Clinical data were collected from medical records for age, sex, urinalysis, serum albumin, and serum creatinine (Cr) at the time of renal biopsy. NS was defined as urinary protein ≥ 3.5 g/day or g/gCr and hypoalbuminemia (serum albumin ≤ 3.0 g/dL). Treatment information and follow-up data were collected via a questionnaire in order to determine the outcome of each patient after the biopsy.
Renal biopsy specimens from 9 proteinuric cancer patients treated with VEGF-VEGFR2 inhibitors were processed using standard techniques for light, immunofluorescence, and electron microscopies. Formalin-fixed, paraffin-embedded sections were stained with hematoxylin and eosin (HE), PAS, Masson trichrome (MT), and periodic acid-methenamine silver (PAM). PAS-positive hyaline occlusive pseudothrombi was graded as the percentage calculated by dividing the number of glomeruli containing pseudothrombi by the number of functioning glomeruli observed on PAS-stained sections: mild (< 25%), moderate (25–50%), and severe (> 50%). Tubulointerstitial damage and vascular lesions were categorized as mild (< 25%), moderate (25–50%), and severe (> 50%) as previously described [11, 12]. The sections were also processed for immunohistochemistry with rabbit polyclonal antibodies to human IgG, IgA, and IgM (Dako, Glostrup, Denmark), or with mouse monoclonal antibodies to human CD61 (platelet glycoprotein IIIa) (Dako) and VEGF (Santa Cruz Biotechnology, Santa Cruz, CA, USA). The sections were then stained using anti-rabbit immunoglobulins conjugated to a peroxidase-labeled polymer (Dako), or with the ImmPRESS™ Anti-Mouse Ig (peroxidase) Reagent (Vector Laboratories, Burlingame, CA, USA). Renal sections of autopsy specimens from a patient who died of acute TMA were used as a positive control for CD61 staining. VEGF expression was graded according to the intensity of staining as weak (1 +), moderate (2 +), and strong (3 +). Cryostat sections for immunofluorescence microscopy were stained with fluorescein isothiocyanate (FITC)-conjugated rabbit polyclonal antibodies to human IgG, IgA, IgM, κ, λ, C3, and C1q (Dako). For C4d staining, mouse monoclonal antibody to human C4d (Quidel, San Diego, CA, USA) and FITC-conjugated goat polyclonal antibody to mouse immunoglobulins (Dako/Agilent, Santa Clara, CA, USA) were used. In Case #9, paraffin immunofluorescence [13] was also performed. Immunofluorescence intensity was graded as negative (−), faint ( ±), weakly positive (1+), moderately positive (2+), and strongly positive (3+). Podocyte foot process effacement was graded as the percentage of total glomerular capillary surface area over which the podocytes foot processes were effaced on electron microscopy: mild (< 25%), moderate (25–50%), and severe (> 50%).
Statistical analysis
Pearson’s correlation coefficient test was used to examine the relationship between podocyte VEGF expression and podocyte foot process effacement.
Results
Clinical features
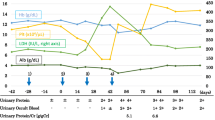
Clinical features in 9 patients (7 males and 2 females) with proteinuria who were treated with VEGF-VEGFR2 inhibitors are summarized in Table 1. The median age at the time of renal biopsy was 68 years (range 34–83). One patient (Case #9) had diabetic kidney disease. Cancer localizations were found in the colorectum in 4 patients, lung in 4 patients, and brain in one patient. Eight patients were treated with various anticancer drugs. All patients were initially treated with Bmab (the cumulative dose: 45–500 mg/kg), and 5 patients were treated with RAM (8–48 mg/kg) or AFB (20 mg/kg) following Bmab treatment. The median time from the beginning of Bmab treatment to the onset of renal disease was 11 months (range 3–44). Six patients were treated with antihypertensive drugs. Seven patients had leg edema or anasarca. Before Bmab treatment, 7 patients had no proteinuria. At the time of renal biopsy, all patients had moderate to heavy proteinuria, and 5 patients developed NS. All patients presented with normal or slightly elevated levels of serum creatinine (0.73–1.42 mg/dL). Laboratory data after discontinuing VEGF-VEGFR2 inhibitors are also summarized in Table 1. Specific treatment was not performed in any cases, except Case #4 was treated with prednisolone as a short-term diagnostic therapy. Proteinuria improved in 8 patients, and serum creatinine level was stable or decreased in 6 patients. Persistent heavy proteinuria in Case #9 was probably due to diabetic kidney disease. The median follow-up period was 11 months (range 2–38). Four patients died due to tumor progression.
Histopathological features
All nine biopsies from proteinuric patients treated with VEGF-VEGFR2 inhibitors showed variably PAS-positive hemispherical/spherical lesions along glomerular capillary walls and in para-mesangial areas on light microscopy (Fig. 1, Table 2). Colors of PAS-positive hemispherical/spherical lesions were different: some showed pale staining, whereas others showed dense staining (Fig. 1). Colors of these lesions were also variable on MT staining and PAM staining (Fig. 2). Double contours of the glomerular basement membranes and mesangiolysis were also observed on light microscopy (Figs. 1, 2). Tubulointerstitial alterations were commonly mild (Table 2). Immunofluorescence microscopy showed positive staining for immunoglobulins (IgM dominant) and compliments at varying intensities along glomerular capillary walls and in mesangial areas in a granular/fringe pattern (Fig. 3, Table 2). Characteristic hemispherical/spherical positive staining (IgM dominant) was also observed mainly along glomerular capillary walls in all cases (Fig. 3, Table 2). Immunohistochemical studies showed that hemispherical/spherical lesions along glomerular capillary walls were positive for immunoglobulins but negative for CD61-positive platelets (Fig. 4), and that podocytes were positive for VEGF (Fig. 4) in all cases. Electron microscopy showed variably electron-dense material in dilated glomerular capillaries, loss of endothelial fenestration, subendothelial material filling with double-contoured glomerular basement membranes, and partial effacement of podocyte foot processes (Fig. 5) in all cases, except for Case #9 with no glomeruli in the specimen. These findings were consistent with those of Bmab-associated glomerular microangiopathy [9, 10]. Based on the above-mentioned observations, PAS-positive hemispherical/spherical lesions along glomerular capillary walls were considered to be hyaline pseudothrombi occluding dilated glomerular capillaries. There was no correlation between podocyte VEGF expression and podocyte foot process effacement.
Light microscopic findings of VEGF-VEGFR2 inhibitor-associated glomerular microangiopathy. Representative findings are shown (Cases #1–#9). Variably PAS-positive hemispherical/spherical lesions (arrows) along glomerular capillary walls and the para-mesangial area are observed (PAS staining, original magnification 600×). The scale bars represent 20 μm
Light microscopic findings of VEGF-VEGFR2 inhibitor-associated glomerular microangiopathy. Representative findings are shown (Case #5). Hemispherical/spherical lesions (arrows), double contours of glomerular basement membranes, and mesangiolysis are observed (HE staining, MT staining, and PAM staining, original magnification 600×). The scale bars represent 20 μm
Immunofluorescence microscopy findings of VEGF-VEGFR2 inhibitor-associated glomerular microangiopathy. Representative findings are shown (Case #2). Positive staining for IgG, IgA, IgM, κ, λ, C4d, and C1q at varying intensities in a granular/fringe pattern are observed along glomerular capillary walls and in the mesangial area. Hemispherical/spherical positive staining (arrows) is also observed
Immunohistochemical findings of VEGF-VEGFR2 inhibitor-associated glomerular microangiopathy. Representative findings are shown (Case #5). Positive staining for immunoglobulins but negative staining for CD61 in dilated capillaries (arrows) and positive staining for VEGE in podocytes are observed (IgG staining, IgA staining, IgM staining, CD61 staining, and VEGF staining, original magnification 600×). In an autopsy case of glomerular TMA, positive staining for CD61 is observed in thrombi (CD61 staining, original magnification 600 ×). The scale bars represent 20 μm
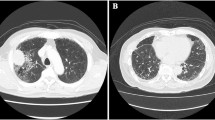
Electron microscopy findings of VEGF-VEGFR2 inhibitor-associated glomerular microangiopathy. Representative findings are shown (Case #7). A Variably electron-dense material without diagnostic secondary structures is observed in a dilated capillary loop with a collapsed endothelial cell (arrow). The scale bar represents 2 μm. B Loss of endothelial fenestration, subendothelial electron-dense material with double-contoured glomerular basement membrane (arrow), and podocyte foot process effacement are observed. The scale bar represents 2 μm
Discussion
VEGF-VEGFR2 inhibitors, including Bmab, may cause renal injury via complex mechanisms. In earlier cohort studies reported in 2012–2014, acute/chronic glomerular TMA was the main pathological type [6,7,8]. In this type, mild to moderate proteinuria and hypertension are often seen, but sometimes massive proteinuria and/or renal insufficiency develop [6,7,8]. As VEGF-VEGFR2 inhibitor-associated nephrotoxicity may mimic preeclampsia, there are pathophysiological similarities between renal involvement in preeclampsia and VEGF ablation therapy due to decreased levels of local and circulating VEGF [14]. In both preeclampsia and Bmab-induced renal injury, the VEGF-VEGFR2 pathway is either blocked by placental soluble fms-like tyrosine kinase-1 or anti-VEGF antibody (or VEGF trap). Blocking of this pathway may lead to glomerular endotheliosis and TMA by the same pathophysiological factors [14].
Recently, a new pathological form of Bmab-associated glomerulopathy, hyaline occlusive glomerular microangiopathy, has been recognized in two European cohort studies [9, 10]. This form is characterized by a patchy pattern of variably PAS-positive hyaline pseudothrombi occluding dilated glomerular capillaries. In these cohort studies [9, 10] as well as in our study, colors of PAS-positive hemispherical/spherical lesions were different. Colors of these lesions were also variable on MT staining and PAM staining in our study. This staining heterogeneity may be a diagnostic clue for VEGF-VEGFR2 inhibitor-associated hyaline occlusive glomerular microangiopathy.
To the best of our knowledge, there are two prior reports of probable Bmab-associated glomerular microangiopathy (published in 2013–2014) [15, 16] and a most recent case report of Bmab-associated glomerular microangiopathy [17]. Interestingly, all these cases were reported from Japanese institutes, and the above-mentioned characteristic histopathological findings of this glomerular microangiopathy were observed in these cases of Bmab-treated cancer patients. On the other hand, information on renal biopsy findings other than TMA and FSGS in patients with AFB- or RAM-induced renal diseases is still limited [18,19,20,21]. Tyrosine kinase inhibitors of VEGFR2, such as sunitinib and nintedanib, may also lead to hyaline occlusive glomerular microangiopathy [9, 22].
In the present Japanese cohort study, we analyzed 9 renal biopsies from proteinuric cancer patients treated with VEGF-VEGFR2 inhibitors (Bmab in all cases). All patients developed moderate to heavy proteinuria with normal or slightly elevated levels of serum Cr. The following histopathological findings were characteristic in our patient: PAS-positive hemispherical/spherical lesions along glomerular capillary walls, positive staining for immunoglobulins (IgM dominant) at varying intensities along glomerular capillary walls, and variably electron-dense material in the hemispherical/spherical lesions in dilated glomerular capillaries. Double contours of glomerular basement membranes, mesangiolysis, and partial effacement of podocyte foot processes were also commonly observed. Immunohistochemical studies showed positive staining for immunoglobulins and negative staining for CD61-positive platelets in glomerular capillary hemispherical/spherical lesions. These histopathological findings are consistent with those in the recently described Bmab-associated glomerular microangiopathy [9, 10]. Additionally, our study along with a very recent case report [17] showed that hemispherical/spherical positive staining for immunoglobulins (IgM dominant or “full house” staining) is a characteristic pattern of this glomerulopathy on immunofluorescence microscopy. Furthermore, positive staining for C4d along glomerular capillary walls was commonly observed in our study. Glomerular C4d deposition can be detected in the majority of cases of Bmab-associated glomerular microangiopathy [9, 10], as a result of endothelial injury [23].
Pfister et al. [9] proposed a hypothetical sequence of the evolution of segmental hyalinosis from glomerular capillary microaneurysms in anti-VEGF therapy-induced glomerular microangiopathy, which may explain the clinicopathological characteristics of this glomerular microangiopathy. Initially, anti-VEGF agents induce a loss of fenestration of glomerular endothelial cells and degenerative changes of these cells with detachment from glomerular basement membranes. During this process, a microaneurysm forms, and this is progressively filled with material probably of plasma insudations, including immunoglobulins and complements, which solidify to segmental hyalinoses as the process advances. Although podocytes are well preserved at the beginning of insult, they develop partial effacement of the podocyte foot processes as a consequence of persistent proteinuria during the course of the disease. Person et al. [10] also suggested that Bmab-associated hyaline occlusive glomerular microangiopathy likely arises from endothelial leakage followed by subendothelial accumulation of plasma proteins, based on the results of comparative proteomics analysis of glomerular proteins from patients with Bmab-associated glomerular microangiopathy, acute glomerular TMA, and cryoglobulinemic membranoproliferative glomerulonephritis. The mechanistic processes of Bmab-associated hyaline occlusive lesions may be similar to those of the so-called fibrin cap in diabetic nephropathy. Fibrin cap lesions are caused by insudation and accumulation of plasma proteins between the glomerular epithelia and basement membranes within microaneurysms, which are usually found surrounding the expanded nodules during disease progression [24].
Our 9 study patients with VEGF-VEGFR2 inhibitor-associated hyaline occlusive glomerular microangiopathy developed moderate to heavy proteinuria (NS in 5 patients) with normal or slightly elevated levels of serum Cr. After withdrawal of VEGF-VEGFR2 inhibitors, proteinuria improved without any specific treatment in all cases, except for Case #9 with diabetic kidney disease. In contrast to decreased or undetectable glomerular VEGF expression in patients with glomerular TMA following anti-VEGF therapy [7, 25], our immunohistochemical analysis revealed that VEGF was positively stained at varying intensities in podocytes in all patients, indicating preserved VEGF production by podocytes. In the previous cohort studies of Bmab-associated glomerular microangiopathy [9, 10], glomerular VEGF expression was not examined. Morimoto et al. [17] presented a single case of NS due to this glomerular microangiopathy, whereby VEGF expression was markedly reduced in glomeruli. This patient did not achieve type 1 partial remission or complete remission of NS at 28 months after Bmab withdrawal. Therefore, the VEGF-VEGFR2 inhibitor-associated glomerular microangiopathy in our cases and that of Morimoto et al. [17] suggest that preserved VEGF production by podocytes may have a cellular protective effect against nephrotoxicity of VEGF-VEGFR2 inhibitors to facilitate early recovery. This may be supported by the following observations in mice: cultured podocytes have a functional autocrine VEGF system that promotes cell survival through VEGFR2 by regulating slit diaphragm proteins [26], and podocyte-derived VEGF regulates the structure and function of the adjacent glomerular endothelial cells through a paracrine VEGF-VEGFR2 signaling loop [27].
The reason why only a subset of patients receiving VEGF-VEGFR2 inhibitors develop glomerular TMA or hyaline occlusive glomerular microangiopathy remains unclear. The cause of the different main histopathological types among the reported cohorts [6,7,8,9,10] also remains obscure. Glomerular TMA was the main histopathological type in the European cohorts of den Deurwaarder et al. [6], Vigneau et al. [7], and Izzedine et al. [8], whereas hyaline occlusive glomerular microangiopathy was the main histopathological type in the recently reported European cohorts of Pfister et al [9] and Person et al. [10] as well as in our Japanese cohort. Thus, different genetic backgrounds are unlikely to be the source of such differences. In the previously reported European cohorts [6,7,8,9,10], the cumulative dose of Bmab was not described. It is therefore difficult to elucidate the relationship between the drug dosage and histopathological type. In recent years, the use of VEGF-VEGFR2 inhibitors has become widespread, and the number of cancer patients with treatment-associated renal diseases is increasing. It is possible that different indications of renal biopsy for these cancer patients may be one of the causes of the different incidences of VEGF-VEGFR2 inhibitor-associated glomerular microangiopathy among institutes. A recent Japanese single-institution analysis identified systolic blood pressure, concomitant use of calcium channel blockers, and the number of cycles of chemotherapy with VEGF-VEGFR2 inhibitors as significant predictors of the development of proteinuria in cancer patients treated with Bmab, RAM, and AFB [28]. A recent database analysis of the Japanese Adverse Drugs Event Report also showed that VEGF-VEGFR2 inhibitors were the major causative drugs in patients with NS due to antineoplastic drugs [29]. Thus, further studies of VEGF-VEGFR2 inhibitor-associated renal diseases are important in the field of onconephrology [30, 31].
In conclusion, the recently described new form of hyaline occlusive glomerular microangiopathy is the main histopathological type in our Japanese cancer patients treated with VEGF-VEGFR2 inhibitors. Nephrologists should be aware of this form in these inhibitor-treated cancer patients with proteinuria and relatively preserved renal function. This form can be diagnosed by light and immunofluorescence microscopies and may be reversible after early drug discontinuation.
References
Neufeld G, Cohen T, Gengrinovitch S, Poltorak AZ. Vascular endothelial growth factor (VEGF) and its receptors. FASEB J. 1999;13:9–22.
Ferrara N. Role of vascular endothelial growth factor in regulation of physiological angiogenesis. Am J Physiol Cell Physiol. 2001;280:C1358-1366.
Estrada CC, Maldonado A, Mallipattu SK. Therapeutic inhibition of VFGF signaling a d associated nephrotoxicities. J Am Soc Nephrol. 2019;30:187–200.
Wu S, Kim C, Baer L, Zhu X. Bevacizumab increases risk for severe proteinuria in cancer patients. J Am Soc Nephrol. 2010;21:1381–9.
Eremina V, Jefferson JA, Kowalewska J, Hochster H, Haas M, Weisstuch J, et al. VEGF inhibition and renal thrombotic microangiopathy. N Engl J Ned. 2008;358:1129–36.
den Deurwaarder ESG, Desar IME, Steenbergen EJ, Mulders PF, Wetzels JFM, van Herpen CML. Kidney injury during VEGF inhibitor therapy. Neth J Med. 2012;70:267–71.
Vigneau C, Lorcy N, Dolley-Hitze T, Jouan F, Arlot-Bonnemains Y, Laguerre B, et al. All anti-vascular endothelial growth factor drugs can induce ‘pre-eclampsia-like syndrome’: a RARe study. Nephrol Dial Transplant. 2014;29:325–32.
Izzedine H, Escudier B, Lhomme C, Pautier P, Rouvier P, Gueutin V, et al. Kidney diseases associated with anti-vascular endothelial growth f actor (VEGF): an 8-year observational study at a single center. Medicine (Baltimore). 2014;93:333–9.
Pfister F, Amann K, Daniel C, Klewer M, Büttner A, Büttner-Herold M. Characteristic morphological changes in anti-VEGF therapy-induced glomerular microangiopathy. Histopathology. 2018;73:990–1001.
Person F, Rinschen MM, Brix SR, Wulf S, Noriega MLM, Fehrle W, et al. Bevacizumab-associated glomerular microangiopathy. Mod Pathol. 2019;32:684–700.
Ozawa M, Komatsuda A, Ohtani H, Nara M, Sato R, Togashi M, et al. Long-term prognosis of AL and AA renal amyloidosis: a Japanese single-center experience. Clin Exp Nephrol. 2017;21:212–27.
Saito A, Komatsuda A, Saito M, Kaga H, Abe F, Sawamura M, et al. Clinicopathological features and outcomes of diabetic kidney disease with extracapillary hyper cellularity: a Japanese single-center experience. Clin Exp Nephrol. 2020;24:509–17.
Nasr SH, Fidler ME, Said SM. Paraffin immunofluorescence: a valuable ancillary technique in renal pathology. Kidney Int Rep. 2018;3:1260–6.
Müller-Deile J, Schiffer M. Renal involvement in preeclampsia: similarities to VEGF ablation therapy. J Pregnancy. 2011;2011:176973.
Yahata M, Nakaya I, Sakuma T, Sato H, Aoki S, Soma J. Immunoglobulin A nephropathy with massive paramesangial deposits caused by anti-vascular endothelial growth factor therapy for metastatic rectal cancer: a case report and review of the literature. BMC Res Notes. 2013;6:450.
Tomita M, Ochiai M, Shu S, Yamauchi Y, Shihara H, Ogata A, et al. A case of thrombotic microangiopathy with glomerular subendothelial IgA deposition due to bevacizumab. Nihon Jinzo Gakkai Shi. 2014;56:612–7 (in Japanese with English abstract).
Morimoto M, Arai T, Matsuura M, Ono Y. Bevacizumab-associated glomerular microangiopathy that occurred after postoperative chemotherapy for ovarian cancer. CEN Case Rep. 2021;10:6–11.
Abdel-Rahman O, ElHalawani H. Proteinuria in patients with solid tumors treated with ramucirumab: a systematic review and meta-analysis. Chemotherapy. 2014;60:325–33.
Hanna RM, Tran NT, Patel SS, Hou J, Jhaveri KD, Parikh R, et al. Thrombotic microangiopathy and acute kidney injury induced after intravitreal injection of vascular endothelial growth factor inhibitors VEGF blockade-related TMA after intravitreal use. Front Med (Lausanne). 2020;7:579603.
Yamada R, Okawa T, Matsuo K, Suzuki M, Mori N, Mori K. Renal-limited thrombotic microangiopathy after switching from bevacizumab to ramucirumab: a case report. BMC Nephrol. 2019;20:14.
Fujii T, Kawasoe K, Tonooka A, Ohta A, Nitta K. Nephrotic syndrome associated with ramucirumab therapy: a single-center case series and literature review. Medicine (Baltimore). 2019;98:e16236.
Hasegawa M, Uehara A, Suzuki T, Sekine R, Yazawa M, Ichikawa D, et al. Nintedanib-induced glomerular microangiopathy: a case report. CEN Case Rep. 2020;9:295–300.
Cohen D, Colvin RB, Daha MR, Drachenberg CB, Haas M, Nickeleit V, et al. Pros and cons for C4d as a biomarker. Kidney Int. 2012;81:628–39.
Alsaad KO, Herzenberg AM. Distinguishing diabetic nephropathy from other causes of glomerulosclerosis: an update. J Clin Pathol. 2007;60:18–26.
Izzedine H, Mangier M, Ory V, Zhang SY, Sendeyo K, Bouachi K, et al. Expression patterns of RelA and c-mip are associated with different glomerular diseases following anti-VEGF therapy. Kidney Int. 2013;85:457–70.
Guan F, Villegas G, Teichman J, Mundel P, Tufro A. Autocrine VEGF-A system in podocytes regulated podocin and its interaction with CD2AP. Am J Physiol Renal Physiol. 2006;291:F422–8.
Sison K, Eremina V, Baelde H, Min W, Hirashima M, Fantus IG, et al. Glomerular structure and function require paracrine, not Autocrine, VEGF–VEGFR-2 signaling. J Am Soc Nephrol. 2010;21:1691–701.
Kanbayashi Y, Ishikawa T, Tabuchi Y, Sakaguchi K, Ouchi Y, Otsuji E, et al. Predictive factors for the development of proteinuria in cancer patients treated with bevacizumab, ramucirumab, and aflibercept: a single-institution retrospective analysis. Sci Rep. 2020;10:2011.
Okada K, Usui K, Kikuchi D, Takahashi M, Watanabe Y. The risk of nephrotic syndrome with non-VEGF inhibitory antineoplastic drugs; from viewpoint of the adverse event reports in Japan. Clin Exp Nephrol. 2021;25:97–8.
Kitai Y, Matsubara T, Yanagita M. Onco-nephrology: current concepts and future perspectives. Jpn J Clin Oncol. 2015;45:617–28.
Rosner MH, Jhaveri KD, McMahon BA, Perazella MA. Onconephrology: the intersections between the kidney and cancer. CA Cancer J Clin. 2021;71:47–77.
Acknowledgements
The authors thank all the doctors at our affiliated hospitals for the referral of the patients. This study was supported in part by private donations from Dr. Ken Satoh, Satoh Naika Clinic, Sakata, Japan, and Dr. Masaru Togashi, Akita Renal, Collagen and Rheumatic Disease Clinic, Akita, Japan.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Dr. Naoto Takahashi has received grants and personal fees from Novartis Pharmaceuticals, grants and personal fees from Pfizer, grants and personal fees from Otsuka Pharmaceutical, grants from Kyowa Kirin, grants from Astellas Pharma, grants from Chugai Pharmaceutical, grants from Asahi Kasei Pharma, grants from Ono Pharmaceutical, and grants from Eisai Pharmaceuticals, outside of the submitted work. The remaining authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee at which the studies were conducted (IRB approval number 1026), and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
About this article
Cite this article
Ozawa, M., Ohtani, H., Komatsuda, A. et al. VEGF-VEGFR2 inhibitor-associated hyaline occlusive glomerular microangiopathy: a Japanese single-center experience. Clin Exp Nephrol 25, 1193–1202 (2021). https://doi.org/10.1007/s10157-021-02090-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10157-021-02090-z