Abstract
Background
The activation of the nuclear factor-κB (NF-κB) signaling pathway gives rise to inflammation in the pathogenesis of lupus nephritis (LN), with A20 serving as a negative feedback regulator and ubiquitin C‑terminal hydrolase L1 (UCH-L1) acting as a downstream target protein. However, their roles in the mechanism of LN remain undetermined.
Methods
In the present study, the expression of A20 and UCH-L1, the activity of NF-κB and ubiquitin–proteasome system (UPS) were measured in MRL/lpr mice and A20 gene silenced podocytes. The severity of podocyte injury and immune complex deposits were detected by transmission electron microscopy.
Results
The in vivo experiments revealed that A20 failed to terminate the activation of NF-κB, which was accompanied by UCH-L1 overexpression, ubiquitin accumulation, and glomerular injury in LN mice. Immunosuppression therapy did improve LN progression by attenuating A20 deficiency. In vitro experiments confirmed that tumor necrosis factor-α induced NF-κB activation, which led to UCH-L1 overexpression, UPS impairment, the upregulation of desmin and the downregulation of synaptopodin in A20 gene silenced podocytes.
Conclusion
Thus, the results of the present study suggest that A20 regulates UCH-L1 expression via the NF-κB signaling pathway and A20 deficiency might play an important role in LN pathogenesis. Therefore, the A20 protein may serve as a promising therapeutic target for LN.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Lupus nephritis (LN), which is characterized by glomerulonephritis and tubulointerstitial inflammation with immune complex (IC) deposits in renal tissue, is associated with significant morbidity and mortality in patients with systemic lupus erythematosus (SLE) [1]. However, the mechanism underlying renal damage in LN has not been fully elucidated.
Phosphorylated nuclear factor-κB (p-NF-κB) dimers serve a prominent role in the onset and progression of LN [2], by translocating to the nucleus, binding to specific DNA sequences, and inducing target proteins to mediate inflammatory and immune responses [3]. Ubiquitin is expressed in eukaryotes, labeling various target proteins for proteasome degradation [4]. Our previous study demonstrated that the ubiquitin level in cerebrospinal fluid may be a promising biomarker for active neuropsychiatric SLE [5]. The glomerular deposits of ubiquitin were also reported to be increased in SLE patients and SLE-prone mice [6].
A20, a cytoplasmic protein also known as tumor necrosis factor-α (TNF-α) induced protein 3 (TNFAIP3), serves an essential role in the inhibition of inflammation, mainly through the negative regulation of the NF-κB signaling pathway triggered by the TNF and interleukin-1 (IL-1) receptors [7]. In addition, several single nucleotide polymorphisms (SNPs) in the A20 genomic locus have been reported to be associated with increased susceptibility to SLE [8]. Ubiquitin C-terminal hydrolase-L1 (UCH-L1), also known as protein gene product 9.5, is a deubiquitinating enzyme that regulates the ubiquitin–proteasome system (UPS) [9]. UCH-L1 is also a downstream target protein in the NF-κB signaling pathway and is upregulated via p-NF-κB dimers binding to the UCH-L1 promoter site [10, 11]. Little is known about the association between A20 and UCH-L1, or their roles in the pathogenesis of LN.
In the present study, the inflammatory state, A20 deficiency and the activated NF-κB -UCH-L1 pathway were investigated in the glomeruli of MRL/lpr mice and TNF-α treated A20 gene silenced podocytes. These observations elucidated that A20 deficiency may contribute to LN pathogenesis and may be a potential therapeutic target for LN.
Materials and methods
Animals
Female MRL/lpr mice (n = 50; 16 weeks old; 18–22 g), and age and weight-matched female C57BL/6 mice (n = 30) were obtained from Experimental Animal Center of Nanjing Military Region (Nanjing, China). All mice were specific pathogen-free grade. MRL/lpr mice were randomly divided into three disease control (DC) groups (10 mice per group; sacrificed at weeks 0, 8 and 16) and two prednisone treatment groups (Tx; 10 mice per group; sacrificed at weeks 8 and 16), termed as DC 0w, DC 8w, DC 16w, Tx 8w and Tx 16w, respectively. C57BL/6 mice were used as the normal control (NC) and randomly divided into three groups, sacrificed at weeks 0, 8 and 16, termed as NC 0w, NC 8w, and NC 16w, respectively. Mice in the Tx groups were given prednisone at a dosage of 0.1 mg/10 g·day−1 via intragastric administration. Mice in the NC and DC groups received equal amounts of normal saline daily. Animal protocols and procedures were approved by the Biomedical Research Ethics Committee of Xuzhou Central Hospital, College of Southeast University (Jiangsu, China).
Mouse sample collection
At the end of weeks 0, 8 and 16, urine samples were collected in metabolic cages to examine the 24 h urinary protein levels, and blood samples were obtained by eye puncture when the mice were anesthetized with isoflurane; the mice were then sacrificed via cervical dislocation. Kidneys were perfused with phosphate buffer saline prior to harvesting. Part of the kidneys was used for the isolation of glomeruli using a differential sieving method [12].
Cell culture and A20/TNFAIP3 small interference (si)-RNA interference
The conditionally thermosensitive SV40‑transfected immortalized murine podocyte cell (MPC) line, MPC5 (a gift from Dr. Zhao, Peking University First Hospital, Beijing, China) was cultured under permissive conditions [33 °C, 5% (v/v) CO2, in 10% (v/v) fetal bovine serum (10100147; Gibco; Thermo Fisher Scientific, Inc.), RPMI-1640 and 10 U/ml γ-interferon] to induce proliferation, and then under non-permissive conditions (37 °C without γ-interferon) for 10–14 days to induce differentiation. Differentiated podocytes were identified by their large arborized shape and expression of synaptopodin mRNA [13]. Differentiated podocyte cells were plated on six-well plates and cultured in antibiotic-free medium to 60–80% confluence prior to transfection. Specific siRNA (Thermo Fisher Scientific, Inc., Waltham, MA, USA) for the target gene A20/TNFAIP3 (4390771) and scrambled control (4390843) were transfected with Lipofectamine® RNAiMAX (13778150; Invitrogen; Thermo Fisher Scientific, Inc.) according to the manufacturer’s instructions. Following 24 h, the culture medium was changed, then cells were classified into: blank group (without any treatment), TNF-α group (treated with stated concentration of TNF-α, T7539, Sigma‑Aldrich, Merck KGaA, Darmstadt, Germany), siRNA-A20 group (transfected with siRNA-A20), siRNA-scramble group (transfected with siRNA-scramble), TNF-α + siRNA-A20 group (treated with TNF-α at 24 h after transfection with siRNA-A20), TNF-α + siRNA-scramble group (treated with TNF-α at 24 h after transfection with siRNA-A20), TNF-α + pyrrolidine dithiocarbamate (PDTC) group (simultaneously treated with TNF-α and PDTC), TNF-α + siRNA-A20 + PDTC group (simultaneously treated with TNF-α and PDTC after 24 h of transfection with siRNA-A20), and TNF-α + siRNA-scramble + PDTC group (simultaneously treated with TNF-α and PDTC after 24 h of transfection with siRNA-scramble).
Antibodies
The rabbit anti-UCH-L1 antibody (13179S) was purchased from Cell Signaling Technology, Inc. (Danvers, MA, USA); the mouse anti-A20/TNFAIP3 antibody (ab13597), rabbit anti-IL1β antibody (ab9722), mouse anti-ubiquitin antibody (ab7254), rabbit anti-p-NF-kB p65 (p-p65) antibody (ab86299), anti-desmin antibodies (ab8976, ab32362), rabbit anti-synaptopodin antibody (ab109560) and rabbit anti-lamin B1 antibody (ab16048) were purchased from Abcam (Cambridge, UK); the mouse anti-NF-kB p65 (T-p65) antibody (MAB3026) was from EMD Millipore (Billerica, MA, USA); and the rabbit anti-TNF-α antibody (E90277) and mouse anti-glyceraldehyde-3-phosphate dehydrogenase (GAPDH) antibody (E12-057) were obtained from EnoGene Biotech Co., Ltd. (New York, NY, USA).
Enzyme-linked immunosorbent assay (ELISA)
Serum TNF-α and IL-1β levels were determined using the BD OptEIA™ ELISA kits (mouse TNF, 560478; and mouse IL-1β, 557966; BD Biosciences, Franklin Lakes, NJ, USA). The anti-double strand (ds) DNA antibody was also analyzed using ELISA kits (3041; Chondrex, Inc., Redmond, WA, USA).
Transmission electronic microscopy (TEM)
The 3% glutaraldehyde-fixed 1-mm3 blocks of renal cortex were fixed with 1% osmic acid, dehydrated in graded ethanol, embedded in EPON, sectioned, stained with uranyl acetate and lead citrate, then observed and recorded with a TE microscope (JEM-1010; JEOL Ltd; Japan). A total of three EM images, consisting of at least one loop of the glomerular basement membrane (GBM) in each image, were selected for calculation of the effacement ratio (EFR) using image analysis software (Olympus Corporation, Tokyo, Japan). The mean EFR was used to evaluate the injury degree of the podocytes [14].
Reverse transcription-quantitative polymerase chain reaction (RT-qPCR)
The total RNA of cells was isolated using TRIzol (15596-026; Invitrogen; Thermo Fisher Scientific, Inc.). cDNA was synthesized using a transcriptor first strand cDNA synthesis kit (cat. K1622; Fermentas; Thermo Fisher Scientific, Inc.). qPCR was performed with a real-time PCR master mix (SYBR Green; QPK201; Toyobo Life Science, Osaka, Japan) and a real-time PCR system (DA7600; Daan Gene Co., Ltd; China). For quantification, target genes were normalized to GAPDH. The expression of genes was determined using the following primers: A20/TNFAIP3, forward 5′-GACGTAGGCGGAGCACATCT-3′ and reverse 5′-GAGCGAGCAGCTTGGTTTGT-3′; UCH-L1, forward 5′-GGGCCAGTGTCGGGTAGATG-3′ and reverse 5′-GCGCCATGGTTCACTGGAAA-3′; synaptopodin, forward 5′-CCACAGCGAGCTGGAACCTA-3′ and reverse 5′-CTCGAACCAGTTCCCTTCAGGA-3′; desmin, forward 5′-GGGAGCTGGAGGATCGCTTT-3′ and reverse 5′-GTCCTGGTACTCGCGCAGAT-3′; and GAPDH, forward 5′-ACAACTTTGGCATTGTGGAA-3′ and reverse 5′-GATGCAGGGATGATGTTCTG-3′. Three replicate samples were analyzed separately for each experiment.
Western blot analysis
Lysates were extracted from isolated glomeruli and treated cells. The protein concentrations of lysates were detected using Bicinchoninic Acid Protein Assay kits (P0010S; Beyotime Institute of Biotechnology, Haimen, China). Equal quantities of protein (40 μg) were separated by SDS-PAGE, transferred to PVDF membranes (EMD Millipore), blocked with 5% non-fat milk in TBST (TBS with 0.1% Tween-20, pH 7.4) at room temperature for 2 h, then incubated with the following primary antibodies: anti-UCH-L1 (1:1,000), anti-A20/TNFAIP3 (1:500), anti-desmin (1:1000), anti-synaptopodin (1:1,000), anti-ubiquitin (1:2,000), anti-TNF-α (1:1,000), anti-IL1β (1:2,000), anti-T-p65 (1:1,000) and anti-p-p65 (1:2,000) at 4 °C overnight. Membranes were washed three times and incubated with horseradish peroxidase (HRP)-conjugated secondary antibodies (1:10000) (7074 and 7076; Cell Signaling Technology, Inc.) at room temperature for 2 h. Anti-GAPDH (1:3,000) and anti-lamin B1 (1:1,000) antibodies were used as internal controls. Peroxidase-labeled bands were visualized using an enhanced chemiluminescence system (P0018A; Beyotime Institute of Biotechnology), quantified using Image J 1.48 software (National Institutes of Health, Bethesda, WA, USA) and expressed as fold changes relative to the internal controls. Three replicate samples were analyzed separately for each experiment.
Electrophoretic mobility shift assay (EMSA)
Nuclear extracts of the renal cortex were prepared with nuclear and cytoplasmic protein extraction kits (P0028; Beyotime Institute of Biotechnology). The probe for the NF-kB p65 binding sequence of the UCH-L1 promoter was biotin-labeled at 5′-OH, forward 5′- GGAGGGAGGAAGACCGACAAAT-3′, and reverse 5′- ATTTGTCGGTCTTCCTCCCTCC-3′ [10] (GenScript, Nanjing, China). The anti-NF-kB p65 antibody was incubated with the nuclear extracts. The resultant DNA–protein complexes were separated from free DNA via electrophoresis and blotted onto a positively charged nylon membrane, blocked, incubated with HRP-conjugated streptavidin and visualized using LightShift™ chemiluminescent EMSA kits (20148; Thermo Fisher Scientific, Inc.).
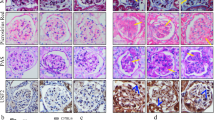
Histopathological and immunohistochemical (IHC) analyses
For microscopic examination, 2.5 μm-thick formalin-fixed and paraffin-embedded sections of renal tissues were dewaxed by xylene. The sections were washed with distilled water twice (each time for 5 min) after soaked in 100%, 95%, 80%, 70% gradient alcohol respectively for 2 min. After hydration, the sections were stained with hematoxylin and eosin (HE), and masson's trichrome (MASSON) (D006 and D026; Nanjing Jiancheng Bioengineering Institute; China). IHC stains for A20/TNFAIP3 (1:200) and UCH-L1 (1:200) at 4 °C overnight. Washed with phosphate-buffered saline (PBS) for 2 min and with addition of 50 μL of HRP-conjugated secondary antibodies (8114 and 8125; Cell Signaling Technology, Inc.) (1: 1000), the sections were incubated at 37 °C for 30 min, washed with PBS, stained with DAB, re-stained with hematoxylin for 5 min, and washed with tap water for 10 min. Then gradient alcohol dehydration and xylene transparency were performed. Renal tissue cells containing brown granulation in the endochylema or nucleus were considered as positive.
Immunofluorescence (IF) Staining and Confocal Microscopy
Kidney cryosections were fixed with 3.7% pre-cooled paraformalin for 15 min at room temperature. After blocking with 5% bovine serum albumin (BSA) for 1 h, the slides were immunostained with primary antibodies against UCH-L1 (13179S; 1:200) and desmin (ab8976, 1:100), A20/TNFAIP3 (ab135957; 1:50) and desmin (ab32362; 1:50) overnight at 4 °C. They were then washed with PBS twice, incubated with fluorescein isothiocyanate (FITC) or Alexa Fluor 647 conjugated secondary antibody (Abcam, Cambridge, UK) in the dark at room temperature for 1 h. DPAI (4,6-diamidino-2-phenylindole) was used to stain the nucleus at room temperature in the dark for 30 min. Finally, the sections were washed twice with PBS, covered with 1,4-Diazabicyclo (2.2.2) octane (DABCO, Sigma‐Aldrich Chemical Company, St Louis, MO), and observed under a confocal laser scanning microscope (Olympus, Tokyo, Japan).
Statistical analysis
Statistical analysis was performed using GraphPad Prism version 7.0 (GraphPad Software, Inc., La Jolla, CA, USA). For parametric data, statistical significance among groups was evaluated by one-way analysis of variance with Tukey’s honest significant difference post hoc test. For nonparametric data, the Kruskal–Wallis and Mann–Whitney U tests were used. Spearman’s rank correlation coefficient was employed to analyze the association between two variables, based on all data from each group, including the NC, DC, or Tx mice groups. P < 0.05 was considered to indicate a statistically significant difference.
Results
Observations of proteinuria, renal function, and the anti-dsDNA antibody titer
All mice survived the interventions and were sacrificed at the indicated times (weeks 0, 8 and 16). One mouse in the DC 16w group was excluded due to its pathological diagnosis of kidney cancer, thus, the DC 16w group contained nine mice.
Proteinuria was significantly higher in MRL/lpr mice when compared with that observed in C57BL/6 mice, and a reduction of proteinuria was observed in the Tx groups (Fig. 1a). The levels of blood urea nitrogen (BUN), serum creatine (SCr) and anti-dsDNA antibody presented similar trends among the NC, DC and Tx groups (Fig. 1b–d). There was no glomerular, interstitial or vascular injury in the renal tissue of C57BL/6 mice, while the cellular proliferation, crescentic formation, and interstitial fibrosis were observed in MRL/lpr mice, and prednisone treatment could alleviate these pathological changes (Fig. 1e). These results confirmed that the MRL/lpr mice developed kidney disease and could be used to study LN pathogenesis.
Prednisone reduces proteinuria and preserves renal function in MRL/lpr mice. The levels of a 24 h urinary protein excretion, b BUN, c SCr and d anti-dsDNA antibody were higher in the DC groups than in the NC groups and were significantly reduced following prednisone treatment. e Renal tissue was stained with hematoxylin and eosin (HE), and Masson. Original magnification, × 400; scale bar, 30 µm. NC normal control, DC disease control, Tx prednisone treatment, BUN blood urea nitrogen, SCr serum creatine, dsDNA double-stranded DNA
A20 deficiency is associated with NF-κB activation and UCH-L1 upregulation in MRL/lpr mice
In weeks 8 and 16, the serum levels of TNF-α and IL-1β were higher in the DC groups when compared with the NC groups, and were decreased significantly in the Tx groups. Western blotting revealed a similar variation tendency (Fig. 2a, b and f). P65 is a well‑known subunit of NF‑B, involved in the transcriptional regulation of multiple genes. Phosphorylation of p65 is a typical feature of NF‑B activation [3]. Western blotting detected that the expression of p-p65 increased in the DC groups in weeks 0, 8 and 16, and decreased markedly in the Tx groups (Fig. 2e and f). The upregulation of pro-inflammatory cytokines reflected the deteriorative inflammatory state, and the overexpression of p-p65 confirmed NF-κB activation in MRL/lpr mice.
A20 deficiency is associated with NF-κB activation and UCH-L1 upregulation in MRL/lpr mice. The levels of a serum TNF-α and b IL-1β were higher in the DC groups than in the NC groups and were significantly reduced following prednisone treatment. c A20 expression decreased and was accompanied by the overexpression of d UCH-L1 and e p-p65 in the DC group. f The expression of A20, UCH-L1, TNF-α, IL-1β, p-p65 and T-p65 in the glomeruli was detected by western blotting. g A close negative correlation between UCH‑L1 and A20 expression was observed. h A close positive correlation between UCH‑L1 and p-p65 expressions was observed. Under the confocal laser scanning microscopy, immunofluorescence staining revealed i A20 and j UCH-L1 expression in the glomeruli, A20 deficiency was observed in MRL/lpr mice accompanied with the overexpression of UCH-L1 and desmin, which could be corrected by prednisone treatment. *P < 0.05, **P < 0.01, ***P < 0.001 and ****P < 0.0001. UCH-L1 ubiquitin C-terminal hydrolase-L1, NC normal control, DC disease control, Tx prednisone treatment, NF-κB nuclear factor-κB, TNF-α tumor necrosis factor-α, IL-1β interleukin-1β, p- phosphorylated, T-p65 nuclear factor-kB p65
A20 expression was negatively associated with p-p65 expression (Fig. 2c and f, Fig. S2), which indicated that A20 deficiency was associated with an exacerbated inflammatory response in MRL/lpr mice. The inflammatory state was attenuated in Tx groups, with upregulation of A20 and a lower expression of TNF-α, IL-1β and p-p65 in glomeruli (Fig. 2). UCH-L1 expression was revealed to be stimulated by NF-κB activation (Fig. 3), which was in accordance with a previous study [10]. Western blotting demonstrated that UCH-L1 expression was higher in the DC groups than in the NC groups, was significantly decreased in the Tx groups (Fig. 2d and f), positively correlated with p-p65 expression (r = 0.62, P < 0.05, Fig. 2h) and negatively correlated with A20 expression in the glomeruli of MRL/lpr mice (r = − 0.58, P < 0.05, Fig. 2g).
Electrophoretic mobility shift assay analysis of UCH-L1 DNA sequence binding with NF-κB p65 subunit. DNA binding was performed with nuclear extracts of the renal cortex. The band migrated via electrophoresis more slowly following adding anti-p65 antibody (supershift, lane 11), indicating that the complexes contained p65. NC normal control, DC disease control, Tx prednisone treatment
Desmin, a podocyte injury marker, was co-immunostained with A20 and UCH-L1, respectively. In comparison with the NC group, IF assay showed the decreasing expression of A20 in MRL/lpr mice, with increasing expression of UCH-L1 and desmin. The A20 and UCH-L1 could be detected in both podocyte and other glomeruli resident cells (Fig. 2i and j). Fig. S1 also demonstrated the expression of A20 and UCH-L1 in the renal tissues of NC, DC and TX mice using IHC.
Ubiquitin accumulation and podocyte injury are associated with the upregulation of UCH-L1
Western blotting results confirmed that the polyubiquitin accumulation during the progression of LN in MRL/lpr mice was attenuated following prednisone treatment (Fig. 4a and b), and positively correlated with UCH-L1 expression (r = 0.77, P < 0.001, Fig. 4e). The expression of desmin exhibited a similar expression as polyubiquitin in MRL/lpr mice (Fig. 3a and c), and a positive correlation with UCH-L expression (r = 0.57, P < 0.05, Fig. 3f). By contrast, synaptopodin decreased significantly in normal saline-treated MRL/lpr mice and increased following prednisone treatment (Fig. 3a and d). The correlation coefficients between synaptopodin, UCH-L1 and A20 were listed in Fig. S2. The upregulation of desmin and downregulation of synaptopodin were indicative of podocyte injury.
Expression of ubiquitin, desmin and synaptopodin in MRL/lpr mice. a Western blotting against ubiquitin, desmin and synaptopodin in the glomeruli. Quantification of b ubiquitin, c desmin and d synaptopodin levels; expression was normalized against GAPDH. Close positive correlations between e UCH‑L1 and ubiquitin expressions, and f UCH‑L1 and desmin expressions. *P < 0.05, **P < 0.01, ***P < 0.001 and ****P < 0.0001. UB ubiquitin, UCH-L1 ubiquitin C-terminal hydrolase-L1, NC normal control, DC disease control, Tx prednisone treatment
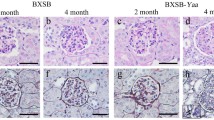
TEM images validated diffuse podocyte foot process effacement and uneven thickened GBM in MRL/lpr mice, even during the early onset of LN, without immune complex (IC) deposition. With the progression of LN, the EFR of podocyte foot processes increased, which was accompanied by IC deposits and increasing expression of UCH-L1 in the glomeruli (r = 0.69, P < 0.01, Fig. 5).
Morphology of podocyte foot process effacement in MRL/lpr mice. a Representative transmission electronic microscopy images at 16 weeks of age (week 0) revealed foot process effacement and uneven thickened GBM (white arrow head in DC 0w group), without electron-dense deposits in MRL/lpr mice, when compared with the intact foot processes and normal-appearing podocytes of the controls. By 32 weeks of age (week 16), fusion of podocyte foot processes was also more severe, with prominent electron-dense deposits (white arrow heads in DC 16w and Tx 16w groups) in the GBM in MRL/lpr mice. Original magnification, × 10,000 and × 25,000; scale bars, 2 nm in the top panel and 1 nm in the bottom panel. b Analysis of foot process EFR, calculated as the total length of foot process effacement in GBM divided by the total length of GBM, c which also presented a positive correlation between UCH‑L1 levels in MRL/lpr mice. *P < 0.05, **P < 0.01 and ****P < 0.0001. NC normal control, DC disease control, Tx prednisone treatment, GBM glomerular basement membrane, EFR effacement ratio
A20 gene silencing in MPC increases TNF-α-induced UCH-L1 overexpression, UPS impairment, and cell injury
The levels of nuclear p-p65 elevated gradually with increasing concentrations of TNF-α in the A20 gene silenced MPCs (Fig. 6a and c). Accordingly, UCH-L1 expression increased following TNF-α stimulation in the A20 gene silenced MPCs (Fig. 5b and d). Polyubiquitin accumulated in A20 gene silenced MPCs following stimulation with TNF-α, while monoubiquitin exhibited the opposite trend (Fig. 5b), which was indicative of UPS impairment. Subsequently, upregulation of desmin and downregulation of synaptopodin were observed in the A20 gene silenced MPCs (Fig. 5b, e and f). In addition, after TNF-α intervention, the NF-κB signaling pathway of podocyte was further blocked using PDTC, when comparing the TNF-α groups, TNF-α + PDTC groups exhibited downregulated expression of NF-κB p-p65, UCH-L1, ubiquitin, and desmin, as well as upregulated expression of synaptopodin in podocyte (Fig. S3).
UCH-L1 expression, UPS impairment and cell damage in response to TNF-α stimulation in A20 gene silenced MPCs. Lysates from the treated cells were analyzed by western blotting and reverse transcription-quantitative polymerase chain reaction. The levels of A20 decreased significantly in the A20 gene silenced MPCs (a and c). Stimulation of TNF-α resulted in a concentration-dependent increase in a nuclear p-p65, b and d UCH-L1, b poly UB and b, e desmin, and a decrease in b mono UB and b, f synaptopodin in the transfected MPCs via A20 siRNA. *P < 0.05, **P < 0.01, ***P < 0.001 and ****P < 0.0001. UCH-L1 ubiquitin C-terminal hydrolase-L1, UB ubiquitin, UPS ubiquitin–proteasome system, TNF-α tumor necrosis factor-α, MPCs murine podocyte cells, siRNA small interfering RNA
Discussion
The MRL/lpr strain is a well-established SLE-prone murine model [15]. MRL/lpr females are more susceptible to lupus-like syndrome, and high levels of antinuclear antibody and anti-dsDNA can be detected within 2–3 months of age. In addition, early renal involvement can be observed at ~ 4–5 months of age and mortality is nearly 100% by 9 months of age [16]. Therefore, MRL/lpr females have been used extensively to study the potential mechanisms of human LN. Compared with the lupus-prone strains, such as MRL/lpr and NZB/W F1, C57BL/6 mice rarely develop autoimmune diseases [17]. Thus C57BL/6 females were chosen as control groups in the present study. The results revealed that the levels of proteinuria, serum BUN, SCr and anti-dsDNA antibody indicated that the MRL/lpr mice developed LN at 16 weeks old. Prednisone treatment was started at the early onset of LN, which reduced proteinuria, the anti-dsDNA antibody titer, and SCr, indicating that the MRL/lpr mice could mimic human LN, which allowed for further study of LN pathogenesis.
The dysregulation of NF-κB activation serves a prominent role in the progression of LN [2, 18]. In MRL/lpr mice, serum TNF-α and IL-1β were significantly increased, which is indicative of systematic inflammation. Overexpression of p-p65 in the glomeruli suggested that NF-κB activation served an essential role in local inflammation of kidney.
As a TNF-inducible protein, A20 expression should be upregulated as well as a negative feedback regulating the NF-κB pathway triggered by TNF-α or IL-1β, via deubiquitinating activity, ubiquitin binding activity and/or E3 ligase activity [19]. A20 deficient mice spontaneously develop severe inflammation, and SNPs near or in the A20 region are associated with SLE [20, 21]. However, little is known regarding A20 expression in the renal tissue of MRL/lpr mice and its roles in LN pathogenesis. The present results suggested that A20 deficiency failed to terminate NF-κB activation in the glomeruli of MRL/lpr mice. Prednisone treatment could increase A20 expression, inhibit NF-κB activation and downregulate pro-inflammatory cytokines in the circulation and glomeruli. A20 deficiency may contribute to the inflammatory state by failing to regulate the NF-κB pathway in MRL/lpr mice.
UCH-L1 serves an important role in proteasomal protein degradation by exhibiting ubiquitin-ubiquitin ligase activity, hydrolyzing ubiquitinated proteins, and binding to and stabilizing monoubiquitin [22]. The overexpression of UCH-L1 contributes to the dysregulation of UPS, resulting in the progressive accumulation of ubiquitinated proteins and polyubiquitin [23]. NF‑B upregulates UCH‑L1 by binding to the − 300 and − 109 bp sites of the UCH‑L1 promoter [10, 24]. The present results demonstrated that UCH-L1 expression was regulated by NF-κB and negatively correlated with A20 expression in the glomeruli of MRL/lpr mice, which indicated that A20 deficiency failed to terminate NF‑B activation, resulting in UCH‑L1 overexpression. Prednisone could inhibit the NF‑B signaling pathway and decrease UCH-L1 expression by attenuating A20 deficiency in MRL/lpr mice.
The filtration barrier of the glomeruli is composed of fenestrated endothelial cells, GBM, as well as foot processes and the slit diaphragm of podocytes. Podocytes are highly differentiated epithelial cells that form part of the filtration barrier to prevent urinary protein loss [25]. The traditional paradigm of LN is regarded as a proliferative immune complex glomerulonephritis, triggered by glomerular deposits of circulating IC [26]. Effacement of foot processes is a fundamental response to podocyte injury [14]. Only a few studies have reported correlations between proteinuria and diffuse effacement of foot processes in LN without IC deposits [27, 28]. The present TEM results revealed diffuse effacement of podocyte foot processes in the DC 0w group (16 weeks old MRL/lpr mice), without IC deposits in renal tissue or evident proteinuria. These results demonstrated podocyte damage in the early onset of LN.
NF–B activation and UCH-L1 upregulation have been demonstrated to be vital in podocyte injury in IC-mediated glomerulonephritis [10, 24]; however, little is known regarding the specific substrates and biological activity of UCH-L1. To investigate the roles of A20 and UCH-L1 in the podocyte injury of LN, the present study measured the expression levels of ubiquitin, desmin, and synaptopodin in the glomeruli of MRL/lpr mice and A20 gene silenced MPCs.
UPS dysfunction, characterized by ubiquitin accumulation, could trigger persistent disease in podocytes via the accumulation of nondegraded proteins [29]. In vitro, polyubiquitin increased and monoubiquitin decreased in the cultured A20 gene silenced MPCs, which was indicative of UPS impairment. In vivo, western blotting data revealed that the levels of monoubiquitin did not differ among the disease and control groups, whereas polyubiquitin levels were higher in the DC groups than in the Tx and NC groups. This was a notable phenomenon and could be explained as follows. During the early stages of the disease (in cultured podocytes), low levels of monoubiquitin possibly reflected the increased ubiquitination processes that are required for the removal of misfolded or damaged proteins. UCH-L1 upregulation coupled with monoubiquitin downregulation suggested there may be a feedback loop to compensate for the decreased monoubiquitin levels. UCH-L1 stabilizes the monoubiquitin pool via hydrolysis of polyubiquitin chains, monoubiquitin proteins and ubiquitin precursors [23]. With the progression of LN (in MRL/lpr mice), polyubiquitin accumulated, while monoubiquitin returned to normal levels [23].
Desmin is an intermediate filament protein of the cytoskeleton that typically indicates podocyte injury [30]. By contrast, synaptopodin, an actin-associated protein in differentiated podocytes that is typically considered to be an important marker of mature podocytes, decreased markedly in injured podocytes [31]. Compared with the C57BL/6 mice, the increased expression of desmin was detected and positively correlated with UCH-L1 expression, which was in contrast to the decreased synaptopodin expression in MRL/lpr mice. In A20 gene silenced MPCs, desmin was upregulated and synaptopodin was downregulated by TNF-α, which was accompanied by UCH-L1 overexpression and polyubiquitin accumulation. These results suggested that UCH-L1 overexpression may induce podocyte damage by impairing UPS functioning in LN pathogenesis.
In the in vitro experiments, the highest concentration of TNF-α (15 ng/ml) was a relatively low concentration for the intervention of podocytes [32], and could not influence A20 expression in normal MPCs, while siRNA-scramble treated MPCs could be more susceptible to TNF-α stimulation, therefore, the increased A20 could be secondary to stated concentration of TNF-α intervention. In the same way, the increased UCH-L1 was also secondary to TNF-α intervention, that was the reason that the increased A20 was accompanied by increased UCH-L1 in the subgroup of siRNA-scramble podocyte. The different levels of NF-κB activation led to different expressions of UCH-L1, ubiquitin, desmin and synaptopodin in the normal MPCs, A20 gene silenced MPCs and siRNA-scramble treated MPCs.
Taken together, it is hypothesized that A20 deficiency fails to terminate NF-κB activation, which results in UCH-L1 overexpression and leads to podocyte injury through UCH-L1-associated UPS impairment. The signaling pathway underlying the A20 regulation of UCH-L1 expression may serve an essential role in LN pathogenesis. In addition, immunosuppression therapy may improve LN progression by attenuating A20 deficiency. In the future, the A20 protein may serve as a novel biomarker or therapeutic target in patients with LN.
Data availability
All data generated or analyzed during this study are included in this published article.
References
Tsokos GC. Systemic lupus erythematosus. N Engl J Med. 2011;365:2110–211.
Jiang T, Tian F, Zheng HT, Whitman SA, Lin YF, Zhang ZG, et al. Nrf2 suppresses lupus nephritis through inhibition of oxidative injury and the NF-kappa B-mediated inflammatory response. Kidney Int. 2014;85(2):333–43. https://doi.org/10.1038/ki.2013.343.
Ghosh S, Hayden MS. Celebrating 25 years of NF-kappa B research. Immunol Rev. 2012;246:5–13. https://doi.org/10.1111/j.1600-065X.2012.01111.x.
Hochstrasser M. Origin and function of ubiquitin-like proteins. Nature. 2009;458(7237):422–9. https://doi.org/10.1038/nature07958.
Sun L, Chen H, Hu C, Wang P, Li Y, Xie J, et al. Identify biomarkers of neuropsychiatric systemic lupus erythematosus by matrix-assisted laser desorption/ionization time-of-flight mass spectrometry combined with weak cation magnetic beads. J Rheumatol. 2011;38(3):454–61.
Elouaai F, Lule J, Benoist H, Appolinairepilipenko S, Atanassov C, Muller S, et al. Autoimmunity to histones, ubiquitin, and ubiquitinated histone H2A in NZB × NZW and MRL-LPR/LPR mice—antihistone antibodies are concentrated in glomerular eluates of lupus mice. Nephrol Dial Transpl. 1994;9(4):362–6.
Parvatiyar K, Harhaj EW. Regulation of inflammatory and antiviral signaling by A20. Microbes Infect. 2011;13(3):209–15.
Musone SL, Taylor KE, Nititham J, Chu C, Poon A, Liao W, et al. Sequencing of TNFAIP3 and association of variants with multiple autoimmune diseases. Genes Immun. 2011;12(3):176–82.
Liu Y, Wu J, Wu H, Wang T, Gan H, Zhang X, et al. UCH-L1 expression of podocytes in diseased glomeruli and in vitro. J Pathol. 2009;217:642–53.
Zhang H, Sun Y, Hu R, Luo W, Mao X, Zhao Z, et al. The regulation of the UCH-L1 gene by transcription factor NF-κB in podocytes. Cell Signal. 2013;25:1574–85.
Wang R, Zhang M, Zhou W, Ly PTT, Cai F, Song W. NF-κB signaling inhibits ubiquitin carboxyl-terminal hydrolase L1 gene expression. J Neurochem. 2011;116:1160–70.
Zhou L, Lu L-M. Isolation and culture of renal glomeruli from rats. Acta Physiol Sin. 2015;67(6):629–35.
Shankland SJ, Pippin JW, Reiser J, Mundel P. Podocytes in culture: past, present, and future. Kidney Int. 2007;72(1):26–36. https://doi.org/10.1038/sj.ki.5002291.
Tewari R, Nada R, Rayat CS, Boruah D, Dudeja P, Joshi K, et al. Correlation of proteinuria with podocyte foot process effacement in IgA nephropathy: an ultrastructural study. Ultrastruct Pathol. 2014;17(2):1–5.
Perry D, Sang A, Yin YM, Zheng YY, Morel L. Murine models of systemic lupus erythematosus. J Biomed Biotechnol. 2011. https://doi.org/10.1155/2011/271694.
Du Y, Sanam S, Kate K, Mohan C. Animal models of lupus and lupus nephritis. Curr Pharm Des. 2015;21:2320–49.
Merinoo R, Shibata T, Kossodo SD, Izui S. Differential effect of the autoimmune Yaa and Ipr genes on the acceleration of lupus-like syndrome in MRL/MpJ mice. Eur J Immunol. 1989;19:2131–7.
Kalergis AM, Iruretagoyena MI, Barrientos MJ, Lez PAG, Herrada AA, Leiva ED, et al. Modulation of nuclear factor-kB activity can influence the susceptibility to systemic lupus erythematosus. Immunol Lett. 2008;128:e306–e314314.
Lee EG, Boone DL, Chai S, Libby SL, Chien M, Lodolce JP, et al. Failure to regulate TNF-induced NF-κB and Cell death responses in A20-deficient mice. Science. 2000;289(5488):2350–4.
Graham RR, Cotsapas C, Davies L, Hackett R, Lessard CJ, Leon JM, et al. Genetic variants near TNFAIP3 on 6q23 are associated with systemic lupus erythematosus. Nat Genet. 2008;40:1059–61.
Musone SL, Taylor KE, Lu TT, Nititham J, Ferreira RC, Ortmann W, et al. Multiple polymorphisms in the TNFAIP3 region are independently associated with systemic lupus erythematosus. Nat Genet. 2008;40:1062–4.
Sakurai M, Ayukawa K, Setsuie R, Nishikawa K, Hara Y, Ohashi H, et al. Ubiquitin C-terminal hydrolase L1 regulates the morphology of neural progenitor cells and modulates their differentiation. J Cell Sci. 2006;119:162–71.
Meyer-Schwesinger C, Meyer TN, Sievert H, Hoxha E, Sachs M, Klupp E-M, et al. Ubiquitin C-terminal hydrolase-L1 activity induces polyubiquitin accumulation in podocytes and increases proteinuria in rat embranous nephropathy. Am J Pathol. 2011;178(5):2044–57.
Zhang H, Gao X, Sun Y, Hu R, Luo W, Zhao Z, et al. NF-κB upregulates ubiquitin C-terminal hydrolase 1 in diseased podocytes in glomerulonephritis. Mol Med Rep. 2015;12(2):2893–901.
Greka A, Mundel P. Cell biology and pathology of podocytes. Annu Rev Physiol. 2012;74:299–32323.
Anders H-J, Fogo AB. Immunopathology of lupus nephritis. Semin Immunopathol. 2014;36:443–59.
Kraft SW, Schwartz MM, Korbet SM, Lewis EJ. Glomerular podocytopathy in patients with systemic lupus erythematosus. J Am Soc Nephrol. 2005;16:175–9.
Trivedi S, Zeier M, Reiser J. Role of podocytes in lupus nephritis. Nephrol Dial Transplant. 2009;24:3607–12.
Beeken M, Lindenmeyer MT, Blattner SM, Radón V, Oh J, Meyer TN, et al. Alterations in the ubiquitin proteasome system in persistent but not reversible proteinuric diseases. J Am Soc Nephrol. 2014;25:2511–25.
Hoshi S, Shu Y, Yoshida F, Inagaki T, Sonoda J, Watanabe T, et al. Podocyte injury promotes progressive nephropathy in Zucker diabetic fatty rats. Lab Invest. 2002;82(1):25–35.
Li JS, Chen X, Peng L, Wei SY, Zhao SL, Diao TT, et al. Angiopoietin-Like-4, a potential target of tacrolimus, predicts earlier podocyte injury in minimal change disease. PLoS ONE. 2015. https://doi.org/10.1371/journal.pone.0137049.
Bitzan M, Babayeva S, Vasudevan A, Goodyer P, Torban E. TNF alpha pathway blockade ameliorates toxic effects of FSGS plasma on podocyte cytoskeleton and beta 3 integrin activation. Pediatr Nephrol. 2012;27(12):2217–26. https://doi.org/10.1007/s00467-012-2163-3.
Funding
The present study was supported by Grants from the National Natural Science Foundation of China (Grant no. 81600540), Natural Science Foundation of Jiangsu Province (Grant no. BK20150224), Science and Technology Foundation of Xuzhou City (Grant no. KC16SL119), Jiangsu Entrepreneurial Innovation Program, Jiangsu Six Talent Peaks Project, Jiangsu Health International (regional) Exchange Support Program, and the Xuzhou Entrepreneurial Innovation Program.
Author information
Authors and Affiliations
Contributions
LS and LZ conceived and designed the experiments. LS, LZ, YH, DZ, JW and TC performed the experiments. LS and LZ analyzed the data. YH and DZ contributed reagents/materials/analysis tools. LS wrote the paper, and LS and LZ revised the manuscript.
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare that they have no competing interests.
Ethical approval
The present study was approved by the Biomedical Research Ethics Committee of Xuzhou Central Hospital, College of Southeast University (Jiangsu, China).
Informed consent
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
About this article
Cite this article
Sun, L., Zou, LX., Han, YC. et al. Role of A20/TNFAIP3 deficiency in lupus nephritis in MRL/lpr mice. Clin Exp Nephrol 24, 107–118 (2020). https://doi.org/10.1007/s10157-019-01826-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10157-019-01826-2