Abstract
Background
Partial nephrectomy (PNx) can be associated with macrocirculatory and microcirculatory alterations, ultimately leading to acute kidney injury (AKI). Measuring kidney tissue oxygenation (μHbO2) and microcirculation during open PNx might be feasible to early detect these alterations and prevent postoperative AKI.
Methods
μHbO2 and microcirculation were measured in 45 patients undergoing PNx by reflectance spectrophotometry and laser Doppler flowmetry (O2C™, Lea, Germany), related to ischemia time and tumour size. Pre- and postoperative creatinine levels were determined.
Results
μHbO2 was lower after reperfusion than before clamping (72 vs. 75%), while microcirculation and regional haemoglobin did not differ. Ischemia time was 15.7 min on average. μHbO2 was higher without ischemia (80 vs. 70%, p = 0.109) and in T1a- than T1b-tumours, independent of ischemia time and reperfusion. The renal collecting system (RCS) was opened in 19/45 patients with μHbO2 of 68% after reperfusion compared to 74% with intact RCS. Postoperative complications occurred in 6/45 patients (13%). μHbO2 was 68% before clamping vs. 75% without complications. Serum creatinine of patients with T1b was higher compared to T1a (103 vs. 87 µmol/L). Patients with larger tumours had higher postoperative creatinine levels (173 vs. 124 µmol/L; p = 0.052).
Conclusion
We showed for the first time that the method is feasible to monitor renal tissue oxygenation at the level of microcirculation non-invasively and reproducibly during PNx. Tumour size seems to have a decisive influence on oxygenation and postoperative renal function. Our results imply that postoperative complications may be predicted by low intraoperative renal oxygenation and microcirculatory flow measurements.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The era of radical nephrectomy as the main treatment for renal cell carcinoma (RCC) belongs to the past. In the past 20 years, organ preservation by nephron-sparing surgery has become increasingly important. And partial nephrectomy has become firmly established in current guidelines [1, 2] as the standard curative treatment option for T1a- and T1b-renal cell carcinoma [2]. Complication, survival and recurrence rates of partial nephrectomy compared to radical nephrectomy have been intensively investigated and seem to show a clear benefit for partial nephrectomy in most patients [3, 4].
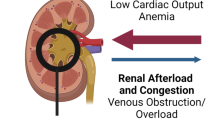
The focus of perioperative hemodynamic monitoring during surgery for RCC is based on macrocirculatory variables such as mean arterial blood pressure (MAP). However, the microcirculation is often dissociated from systemic hemodynamics so that microvascular perfusion cannot be predicted by any of the systemic variables. The microcirculation is, however, a central part of cardiovascular function consisting of blood vessels with a diameter of < 150 µm. The microcirculation delivers oxygen to the cells and maintains tissue oxygenation (μHbO2). Thus, it has a central relevance for organ function.
Partial nephrectomy is often performed with clamping of the renal vessels interrupting the microcirculation. Meanwhile, monitoring tissue oxygenation and the microcirculation has been recognized as an early indicator for the presence of impaired organ perfusion and allows a much earlier intervention to improve the hemodynamic management and, therefore, the outcome [5]. Currently, there is no established technique for routine microcirculatory monitoring and there is still a need to optimize this [6]. A recent development for the measurement of microcirculation and μHbO2 is the O2C device (Oxygen to see©, LEA Medical technology GmbH, Giessen), which was used in this study. In a previous study, we have shown that the intraoperative measurements of microcirculation and μHbO2 of the transplanted kidney with this device could predict early postoperative graft function [7].
In this study, μHbO2 and microcirculation of the kidney were measured intraoperatively during partial nephrectomy for renal tumours to investigate the effects of different surgical variables, especially ischemia time, tumour size and complexity of the surgical procedure, as well as to determine the effects on postoperative kidney function and potential complications. That is, the main focus of the study was to evaluate an intraoperative monitoring method for its practical feasibility and its prognostic ability to predict postoperative kidney function in partial nephrectomy.
Methods
Ethical committee approval was obtained from the institutional review board (number A01/2007). Informed consent was obtained from all patients prior to surgery. Renal microcirculation and oxygenation was measured during surgery of 45 consecutive patients who underwent a partial nephrectomy in the Dept. of Urology at Rostock University Hospital.
Experimental procedure: surgical technique and intraoperative measurement
Partial nephrectomy was performed in cold ischemia; the kidney was cooled with ice water and ice packs while the renal artery was temporarily occluded with a bulldog clamp. The tumour was excised in toto with a safety margin of normal renal parenchyma.
The following relevant variables were recorded: tumour size, ischemia time, complexity of renal surgery and histopathology.
Measurement of kidney oxygenation and microcirculatory blood flow
μHbO2 was measured by white light reflectance spectrophotometry and microcirculatory kidney perfusion by laser Doppler flowmetry (820 nm) (O2C™, Lea, Germany). This device combines both optical techniques in one optical fibre without interference due to different wavelengths used. In this study, we used a flat probe with a measurement depth of 4–6 mm for the kidney surface (Figs. 1, 2) and a microlight-guide (measurement depth 0.2 mm) for the reference measurement of the buccal mucosa. Briefly, the tissue is illuminated by the probe with visible light (500–630 nm) and the backscattered light is analyzed by the spectrophotometer at a rate of 100 Hz giving the μHbO2 values (Fig. 3). The values are averaged and displayed every 2 s.
Measurements were performed at three time points (ToM—time of measurement): immediately before clamping the renal vessels after exposing the kidney (ToM 1), 5 min (ToM 2) and 30 min after release of the vascular clamping and reperfusion of the kidney (ToM 3). Each measurement was performed on the surface of the kidney at three pre-defined sites: the upper pole of the kidney, the lower pole and the convexity opposite to the renal hilum. Each area was measured for 10 s and the values obtained at each measurement point were averaged for each kidney. As the reference, a second probe was placed intraorally to measure microcirculation and μHbO2 at the buccal mucosa. As a clinical parameter of kidney function serum creatinine was used. The preoperative creatinine levels were determined regularly 1 day before surgery, the postoperative controls mostly within the first 6 postoperative days.
Statistical data analyses
Data were analyzed using a standard software package (SPSS 15.0, SPSS Inc., Chicago, USA). Normal data distribution was tested using Kolmogorow–Smirnow-test. With normal distribution, data are presented as means ± SD and further analysis was performed with Student’s t test or ANOVA. Otherwise, data are presented as medians ± range and analysis was performed by Mann–Whitney-U test and Wilcoxon-test. Correlation analysis was performed according to Pearson (normal data distribution) or Spearman. A multivariate analysis was performed according to the equation: y = (ßixi) + ξ + α. A p value < 0.05 was considered statistically significant.
Results
Measurements were performed on 45 patients, 76% of whom had a RCC. Patients and tumour characteristics are shown in Table 1.
Microcirculation and tissue oxygenation
There were no significant differences between the mean values of the measured variables of microcirculatory blood flow and kidney oxygenation before and after clamping the renal vessels. μHbO2 tended to be lower 5 min after reperfusion than before clamping (72 vs. 75%), while the variables of microcirculatory blood flow and regional haemoglobin level did not differ.
30 min after release of the renal vessels and the start of reperfusion (ToM 3), the mean values of μHbO2, flow and velocity were higher than after 5 min (ToM 2).
After 30 min of reperfusion, μHbO2 had recovered slightly. The initial values before cross-clamping were almost reached again (Fig. 3). However, there was a significant increase of microcirculatory blood flow by 15% (t test, p 0.026) in terms of reactive hyperemia. In summary, μHbO2 initially decreased slightly as a result of vascular clamping and immediately after the start of reperfusion (ToM2) but then recovered during the reperfusion phase (ToM3) back to baseline levels (Fig. 3).
Surgical factors
Opening of the renal collecting system
The renal collecting system was opened in 19/45 patients during the surgical procedure. After reperfusion (ToM 2), the measured μHbO2 was on average 68% in the patients with previously opened collecting system compared to 74% in patients with intact collecting system, however, this difference was not significant (t test, p = 0.124). However, at ToM 3 μHbO2 was approximately equal in both groups again.
Influence of ischemia time
The surgical procedure was carried out without clamping of the renal vessels in seven patients. For the 38 patients with intraoperative renal ischemia, average ischemia time was 15.7 min (range 0–40). Patients without clamping tended to have a higher μHbO2 than patients with ischemia (80 vs. 70%, p = 0.109). However, there was no significant difference between the groups (Table 2).
Influence of tumour size
The measured values of μHbO2 tended to be higher in T1a-(< 4 cm) than in T1b-tumours (4–7 cm) at all times, independent of ischemia time and reperfusion. However, a significant correlation between tumor size and μHbO2 was not seen (Table 3).
Postoperative course
Incidence of postoperative complications
Postoperative complications occurred in 6/45 patients (13%). In 2 patients a renal abscess was diagnosed, in one patient a retroperitoneal abscess. A postoperative urine fistula or urinoma occurred in two cases and a soft tissue emphysema in another patient. Revision surgery was performed in two patients for the treatment of complications, in two other patients a percutaneous abscess drainage was necessary. Eventually, two of the patients with complications given above underwent nephrectomy. No patient required hemodialysis.
In the group of the patients who experienced complications, the average of μHbO2 before clamping of the renal vessels at ToM 1 was 68% compared to 75% in the group without postoperative complications (p = 0.194). However, this finding was not statistically significant. (Table 4).
Relationship with renal function
Serum creatinine levels of patients with T1b tended to be higher pre- and postoperatively than those in patients with T1a-tumours. The mean preoperative creatinine level was 103 µmol/L in patients with T1b and 87 µmol/L in those with T1a (p = 0.x). Postoperatively, a similar increase in serum creatinine was seen in both groups. However, postoperative creatinine levels tended to be higher in patients with larger tumours (173 vs. 124 µmol/L; p = 0.052), and were also increased more markedly when complications occured, but this was not significantly different (p = 0.268) (Table 5).
Multivariate analysis
A complex model for the representation of the relationship between each variable and outcome parameters has been established by means of a multivariate analysis (Table 6). A mild non-significant influence on the intraoperative measurement of microcirculation and μHbO2 was noted by gender, hematocrit and tumour size. A negative influence (negative ß value) was found for hematocrit, i.e. kidney oxygenation decreased with increasing hematocrit values. There was no relationship between μHbO2 and MAP (Table 6).
Discussion
In this study, we have shown that renal tumour size seems to have a decisive influence on μHbO2 and function. For T1a-tumours, better μHbO2 levels were seen and serum creatinine levels were preoperatively distinctly lower than in patients with T1b-tumours. Furthermore, our findings suggest a correlation of μHbO2 with postoperative complications; these patients tended to have lower μHbO2 before renal surgery.
The monitoring of the microcirculation and μHbO2 increasingly gains clinical relevance since disturbances at the level of the microcirculation are an important cornerstone of pathophysiological processes. Thus, the early detection of such disturbances becomes possible by measurements of microcirculation which are a prerequisite for timely and adequate treatment interventions [8, 9].
The two methods of measurement with the O2C ©-device have already been successfully used in previous studies [10,11,12]. A particularly important advantage of the O2C ©-device is its non-invasiveness. The tissue assessed is not traumatized by the measuring probes because they are placed on the measured area without applying any pressure.
The O2C ©-probes measure the tissue to a depth of approximately 8 mm [13]. Thus, in the present study especially the microcirculation of the renal cortex is measured which is approximately up to 10 mm wide [14]. Thus, the measurement assesses mainly the renal tissue most affected by ischemia as shown by electron microscopy in an animal study [15]. As expected, our data show a slight decrease in μHbO2 immediately after the start of reperfusion (ToM 2), which was not statistically significant, in our interpretation probably due to the short duration of ischemia (16 min on average). In the measurements 30 min after the start of reperfusion, the pre-clamping baseline values were almost reached again, suggesting that there was a rapid recovery of renal tissue and no irreversible ischemic damage.
We also found a slight decrease of the microcirculatory flow after the relatively short ischemia time at ToM 2 which, however, was reversed at ToM 3. This might be interpreted as reactive hyperemia after previous ischemia.
As expected, μHbO2 did not at any time correlate with the MAP (Table 6). This is most likely an expression of the preserved autoregulation of renal blood flow and glomerular filtration rate (GFR), the so-called Bayliss effect [16, 17]. In contrast, as we have shown in a previous study with renal transplantation, μHbO2 of the (denervated) kidney depended on MAP, which was attributed to loss of renal autoregulation [7].
The tumour size in our patient population was on average 2.7 cm, probably too small to cause compressive effects on the microcirculation and oxygenation of the remaining renal parenchyma and thus on the autoregulation of renal blood flow. With T1a-tumours, we found higher levels of μHbO2 of normal renal tissue than with T1b-tumours at all measurement times independent of ischemia or reperfusion. One possible explanation could be that the tissue of kidneys with large tumours is somehow influenced preoperatively by the tumour, its vascularization and angiogenesis. Thus, μHbO2 of the normal renal parenchyma of tumour-bearing kidneys was already impaired at the level of microcirculation before clamping the renal vessels. Moreover, the more complicated and extended resection of larger tumours also may result in a significant injury to the remaining renal parenchyma. In previous studies, it has been shown by Doppler sonography that RCC have a marked neovascularization [18]. The tumour size also correlated with renal function. A temporary increase in serum creatinine is generally seen after renal surgery but we observed a clear difference between groups with different tumour size. Patients with T1b-tumours had higher creatinine levels compared to those with T1a-tumours both pre- and postoperatively. This suggests that larger tumours already reduce renal function in advance. Other studies have also reported this correlation and have hypothesized that the tumour can damage normal renal parenchyma by invasive growth with displacement/compression of healthy parenchyma directly. Moreover, a primarily limited renal function and the outpouring of growth factors could promote tumour growth which in itself triggers an inflammatory response which further impairs renal function. The fact that marginal chronic renal failure increases the risk of urogenital malignancy generally may support this hypothesis [19].
Concerning ischemia time, we saw a trend that the group without clamping of the renal vessels had slightly higher values of μHbO2 at ToM 2 and ToM 3. In recent studies, it has been reported that both in robotic and laparoscopic partial nephrectomy (without any renal ischemia) compared to open partial nephrectomy less postoperative impairment of renal function was seen (GFR − 1.8 vs − 14.9%) although the overall surgical time was on average longer (256 vs. 212 min) [20]. The reported complication rate was also significantly lower in the absence of renal ischemia (10 vs. 20%) [21]. However, there were no significant differences when the clamping time of the open partial nephrectomy group was under 30 min [21]. According to data from a multicenter study, partial nephrectomy with a maximum of warm ischemia of 20 min and of cold ischemia under 35 min is considered safe [22]. It seems important to note that opening the renal collecting system during surgery had a negative influence on tissue oxygenation. This fact can be seen as an indicator of the complexity of the procedure. This also corresponds with the fact that the collecting system is often opened in kidneys with a centrally located or very large tumour. Thus, there is an increased risk of postoperative complications [23].
Clamping time and thus the duration of ischemia also corresponded with tumour size and thereby the complexity of the procedure. This in turn leads to a decrease in perfusion and oxygenation of the renal tissue. The different preoperative oxygenation values suggest on the one hand that an adequate μHbO2 protects the kidney from postoperative complications. On the other hand, an already damaged kidney which can be recognized by lower preoperative μHbO2 has a higher risk of postoperative complications [24].
A limitation of our study is the relatively small number of patients. A post hoc sample size calculation based on our findings revealed that 612 patients would be necessary to show an effect size of 10% and 2467 patients to indicate a 5% difference in tissue oxygenation and renal function. Another point of criticism concerns the intraoperative measurements. The probe was held for about 10–20 s by the surgeon to the defined renal regions until stable values were recorded. To avoid environment-related disturbances, motion artifacts have to be excluded and the surgical lights were turned away during the measurements. An automatic ambient light correction on the device must be performed and the probe must be positioned steadily and without any pressure. In our study, the O2C ©-device was therefore re-calibrated before each measurement. Furthermore, we restricted the handling of the measuring probes to two experienced surgeons to minimize user-related artifacts. Naturally, it was impossible to perform long-term postoperative measurements.
Conclusions
In summary, our results suggest that tumour size seems to have a decisive influence on kidney oxygenation and postoperative renal function. There were better oxygenation values for smaller tumours and lower preoperative creatinine levels than in patients with larger tumours. Our results indeed suggest a correlation of renal oxygenation and postoperative renal complications in the sense that a worse renal oxygenation prior to resection is associated with a higher risk of postoperative complications.
In conclusion, we showed for the first time that monitoring tissue oxygenation non-invasively at the level of the microcirculation is feasible and reproducible during partial nephrectomy.
References
Ljungberg B. Nephron-sparing surgery—strategies for partial nephrectomy in renal cell carcinoma. Scand J Surg. 2004;93(2):126–31.
Ljungberg B, Bensalah K, Canfield S, et al. EAU guidelines on renal cell carcinoma: 2014 update. Eur Urol. 2015;67(5):913–24.
Van Poppel H, Da Pozzo L, Albrecht W, et al. A prospective, randomised EORTC intergroup phase 3 study comparing the oncologic outcome of elective nephron-sparing surgery and radical nephrectomy for low-stage renal cell carcinoma. Eur Urol. 2011;59(4):543–52.
Hansen J, Sun M, Bianchi M, et al. Assessment of cancer control outcomes in patients with high-risk renal cell carcinoma treated with partial nephrectomy. Urology. 2012;80(2):347–53.
Christ F, Bauer A, Brügger D. Different optical methods for clinical monitoring of the microcirculation. Eur Surg Res. 2002;34(1–2):145–51.
Dantzker DR. Monitoring tissue oxygenation: the quest continues. Chest. 2001;120:701–2.
Scheeren TW, Martin K, Maruschke M, Hakenberg OW. Prognostic value of intraoperative renal tissue oxygenation measurement on early renal transplant function. Transpl Int. 2011;24(7):687–96.
Spronk PE, Zandstra DF, Ince C. Bench-to-bedside review: sepsis is a disease of the microcirculation. Crit Care. 2004;8(No 6):462–8.
Bauer A, Bruegger D, Christ F. Microcirculatory monitoring of sepsis. Anaesthesist. 2005;54:1163–75.
Beckert S, Witte MB, Königsrainer A, Coerper S. The impact of the micro-lightguide O2C for the quantification of tissue ischemia in diabetic foot ulcers. Diabetes Care. 2004;27(No 12):2863–7.
Laduner R, Feilitzsch M, Steurer W, et al. The impact of a micro-lightguide spectrophotometer on the intraoperative assessment of hepatic microcirculation: a pilot study. Microvasc Res. 2009;77:387–8.
Sakr Y, Gath V, Oishi J, Klinzing S, Simon TP, Reinhart K, Marx G. Characterization of buccal microvascular response in patients with septic shock. Eur J Anaesthesiol. 2010;27(4):388–94.
Medizintechnik LEA. O2C (oxygen to see). http://www.lea.de/, http://www.lea.de/deu/fro2chd.htm-Informations-CD.
Moll KJ, Moll M. Kurzlehrbuch Anatomie. 17th ed. München: Urban & Fischer Verlag; 2002. p. 530ff.
Yin M, Currin RT, Peng XX, et al. Different patterns of renal cell killing after warm and cold ischemia. Ren Fail. 2002;24(2):147–63.
Voets T, Nilius B. TRPCs, GPCRs and the Bayliss effect. EMBO J. 2009;28(1):4–5.
Loutzenhiser R, Griffin K, Williamson G, Bidani A. Renal autoregulation: new perspectives regarding the protective and regulatory roles of the underlying mechanisms. Am J Physiol Regul Integr Comp Physiol. 2006;290(5):R1153–R1167.
Rosenbaum C, Wach S, Kunath F, Wullich B, Scholbach T, Engehausen DG. Dynamic tissue perfusion measurement: a new tool for characterizing renal perfusion in renal cell carcinoma patients. Urol Int. 2013;90(1):87–94.
Donin NM, Suh LK, Barlow L, et al. Tumour diameter and decreased preoperative estimated glomerular filtration rate are independently correlated in patients with renal cell carcinoma. BJU Int. 2001;109:379–83.
Borofsky MS, Gill IS, Hemal AK, et al. Near-infrared fluorescence imaging to faciliate super-selective arterial clamping during zero-ischaemia robotic partial nephrectomy. BJU Int. 2013;111(4):604–10.
George AK, Herati AS, Srinivasan AK, et al. Perioperative outcomes of off-clamp vs. complete hilar control laparoscopic partial nephrectomy. BJU Int. 2013;111(4PtB):E235–E41.
Becker F, Van Poppel H, Hakenberg OW, et al: Assessing the impact of ischemia time during partial nephrectomy. Eur Urol. 2009;56:625–35. (© 2009 European Association of Urology. Published by Elsevier B.V.).
Ghavamian R, Zincke H. Partial nephrectomy treatment and management. Medscape reference© 2001 WebMD, LLC. http://emedicine.medscape.com/article/446317 (2001).
Schmaderer C, Lutz J, Stangl M, Heemann U. Ischämie-/Reperfusionsschaden nach Nierentransplantation. In: TransplantLinc, Heft 10. © Pabst Science Publishers; 2005. p. 15–25.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest, including financial interests or relationships.
Ethical approval
All procedures performed in this study involving human participants were in accordance with the ethical standards of the institutional research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. The study was approved by the Medical Ethical Committee of the University of Rostock (A57/2007).
Informed consent
Informed consent was obtained from all individual participants included in the study.
About this article
Cite this article
Maruschke, M., Hagel, K., Hakenberg, O. et al. Prognostic value of intraoperative measurements of renal tissue oxygenation and microcirculation on renal function in partial nephrectomy. Clin Exp Nephrol 22, 735–742 (2018). https://doi.org/10.1007/s10157-017-1506-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10157-017-1506-6