Abstract
Background
Adiponectin, a peptide hormone secreted from adipocytes, exerts anti-diabetic, anti-atherogenic, and anti-inflammatory properties. We aimed to determine the relationship between serum adiponectin levels and albuminuria, and evaluate determinant factors for serum adiponectin in patients with chronic kidney disease (CKD).
Methods
In total, 1442 CKD patients were included and divided into three groups according to their albumin-to-creatinine ratios: patients with normoalbuminuria (N = 228), microalbuminuria (N = 444), and macroalbuminuria (N = 761). Serum adiponectin was specifically assayed with a commercially available enzyme-linked immunosorbent assay kit.
Results
Serum adiponectin was significantly higher in patients with macroalbuminuria than in those without macroalbuminuria (9.7 ± 6.0, 12.4 ± 9.0, and 14.9 ± 11.0 μg/mL in patients with normoalbuminuria, microalbuminuria, and macroalbuminuria, respectively). Univariate linear regression analysis showed that the serum adiponectin concentrations were correlated with age, the albumin-to-creatinine ratio, total cholesterol, low-density lipoprotein cholesterol, and high-density lipoprotein cholesterol, whereas they were negatively correlated with body mass index, the estimated glomerular filtration rate, and serum albumin and triglyceride levels. The stepwise regression multiple analysis showed that sex; the estimated glomerular filtration rate; body mass index; total cholesterol, high-density lipoprotein cholesterol, and triglyceride levels; and logarithm of the albumin-to-creatinine ratio were independently associated with the logarithm of serum adiponectin levels (r = 0.55, p < 0.001).
Conclusion
Serum adiponectin concentrations are higher in patients with increasing albuminuria, and these levels are associated with renal insufficiency and lipid profiles.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Obesity is associated with metabolic syndrome, which is characterized by hyperinsulinemia, insulin resistance, diabetes mellitus (DM), hypertriglycemia, and decreased high-density lipoprotein (HDL) cholesterol levels. In addition, obesity is recognized as a major risk factor for chronic kidney disease (CKD) progression to end-stage renal disease [1]. Adiponectin is a 30 kDa collagen-like protein secreted from adipocytes. Interestingly, plasma concentrations are inversely correlated with the amount of body fat in obesity [2].
Experimental evidence showed the direct role of renoprotective effects such as the anti-inflammatory and anti-fibrotic effects of adiponectin [3, 4]. However, human studies investigating the relationship between serum adiponectin and albuminuria have shown conflicting results [5]. In addition, serum adiponectin levels are an inverse predictor of cardiovascular outcomes [6]. Most research about adiponectin has been conducted on a relatively small population and limited number of patients with DM or obesity. Moreover, some medications affecting serum adiponectin and albuminuria such as renin–angiotensin system blockers or thiazolidinedione were not considered.
We aimed to determine the relationship between serum adiponectin levels and albuminuria in DM and non-DM patients, and evaluate determinant factors for serum adiponectin in patients with CKD.
Patients and methods
Study subjects
The design of the KoreaN Cohort Study for Outcome in Patients With Chronic Kidney Disease (KNOW-CKD) study has been described in detail in a previous study (NCT01630486) [7]. KNOW-CKD is a patient-based, multicenter cohort study comprised nine clinical centers of major university-affiliated hospitals of South Korea. The KNOW-CKD enrolled ethnic Korean patients with CKD who ranged in age between 20 and 75 years. Specific causes of CKD were defined and classified into four sub-cohorts: glomerulonephritis, diabetic nephropathy, hypertensive nephropathy, and polycystic kidney disease. Patients with other causes were categorized as unclassified. Serum and urine samples were subsequently collected on a regular basis according to the standardized protocol. All data, including clinical information, laboratory results, and outcomes, were entered into a web-based, electronic, case-reporting form.
A baseline survey was administered from February 2011 through May 2015 in an ongoing prospective cohort study in collaboration with a multicenter cohort study. In total, 1529 patients were included in this analysis, and we excluded 87 patients with missing data of serum adiponectin and creatinine. Ultimately, 1442 participants were included in the final analysis. These subjects were classified into three groups according to their urine albumin-to-creatinine ratio (UACR): patients with normoalbuminuria (UACR <30 mg/g; N = 228), microalbuminuria (30 mg/g ≤UACR <300 mg/g; N = 444), and macroalbuminuria (UACR ≥300 mg/g; N = 761). CKD was defined by a calculated value of the estimated glomerular filtration rate (eGFR), which was calculated using the Chronic Kidney Disease Epidemiology Collaboration formula [8].
Clinical data and laboratory analyses
Clinical data, including detailed demographic information and baseline laboratory results, were extracted from the electronic data management system (PhactaX, Seoul, Korea). The adiponectin level was measured using an enzyme-linked immunosorbent assay (Adipogen, Seoul, Korea). Adiponectin is secreted into the bloodstream as three oligomeric complexes, including a trimer [low molecular weight (LMW)], hexamer (middle molecular weight), and multimer [high molecular weight (HMW)] comprised at least 18 monomers that possess distinct biological activities. Adiponectin does not circulate in biological fluids as monomers or dimers [9]. The Adiponectin (human) ELISA Kit, which we used, was a total adiponectin kit that detected the sum of values of low-, middle-, and high-molecular-weight adiponectin. The intra- and interassay coefficients of variation were 3.3 and 7.4 %, respectively.
Statistical analysis
Continuous variables with normal distributions are presented as mean ± SD and were compared using one-way analysis of variance. Pearson’s Chi-square test was used to evaluate differences between categorical variables. Simple linear regression analysis was used to examine the relationship between serum adiponectin and various parameters and the relationship between eGFR; body mass index (BMI); systolic blood pressure; diastolic blood pressure; UACR; and fasting blood glucose, serum albumin, total cholesterol, triglyceride, low-density lipoprotein (LDL) cholesterol, and HDL cholesterol levels. Multiple stepwise regression analysis was used to determine the contribution of various factors to serum adiponectin levels. All statistical tests were performed using the Statistical Package for Social Sciences software, version 18.0 (IBM Corp., Armonk, NY). P values <0.05 were considered significant.
Results
Baseline characteristics
In total, 1442 patients (mean age: 53.6 ± 12.3 years; men, 61.6 %) were included in this study. Table 1 summarizes the baseline general characteristics, including 324 with diabetic nephropathy, 309 with hypertensive nephropathy, 455 with glomerulonephropathy, and 246 with autosomal dominant polycystic kidney disease. Table 2 presents the demographics and clinical features according to the albuminuria categories. At baseline, 15.8 % (N = 228) of patients had normoalbuminuria, 30.7 % (N = 444) had microalbuminuria, and 52.7 % (N = 761) had macroalbuminuria. With increasing albuminuria, patients had a higher BMI; systolic blood pressure; and fasting blood glucose, triglyceride, and adiponectin levels, whereas they had lower levels of serum albumin and HDL cholesterol. Increasing albuminuria was associated with a higher prevalence of DM, and use of angiotensin-converting enzyme inhibitors (ACEIs) or angiotensin II receptor blockers (ARBs). LDL cholesterol and total cholesterol levels were higher in patients as albuminuria increased. There were no differences in sex and age among the groups. As expected, eGFR decreased with increasing albuminuria. Mean eGFRs were 72 ± 30, 53 ± 28, and 44 ± 28 mL/min/1.73 m2 in patients with normoalbuminuria, microalbuminuria, and macroalbuminuria, respectively.
Levels of serum adiponectin according to the CKD stage
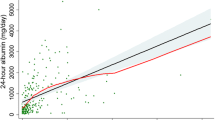
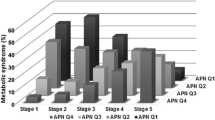
Patients were divided into five eGFR groups corresponding to strata used to define the CKD stages: GFR ≥90; 60 ≤ GFR < 90; 30 ≤ GFR < 60; 15 ≤ GFR < 30; and GFR <15 mL/min/1.73 m2 [10]. Figure 1 shows the serum adiponectin levels according to the CKD stages. There was no difference in the adiponectin concentration among CKD stages 1, 2, and 3, but the serum adiponectin concentration in patients with CKD stage 4 was higher than those in patients with CKD stages 1–3. The serum adiponectin concentrations were higher in patients with CKD stage 5 than in those with CKD stages 1–4 (Fig. 2).
Levels of serum adiponectin according to albuminuria
We compared a group of patients with macroalbuminuria with groups of patients with normoalbuminuria and microalbuminuria. The serum adiponectin level was significantly higher in patients with macroalbuminuria than in those without microalbuminuria (9.7 ± 6.0, 12.4 ± 9.0, and 14.9 ± 11.0 μg/mL in patients with normoalbuminuria, microalbuminuria, and macroalbuminuria, respectively).
Association between the serum adiponectin level and clinical parameters
The serum adiponectin level correlated with age; UACR; and total cholesterol, triglyceride, LDL cholesterol, and HDL cholesterol levels, whereas BMI, eGFR, and the serum albumin level correlated inversely with this protein (Table 3). In stepwise multiple regression analysis, sex; eGFR; BMI; the total cholesterol, HDL cholesterol, and triglyceride levels; and the logarithm of UACR were independent predictors of the logarithm of serum adiponectin (Table 4). However, age, DM, the LDL cholesterol levels, ACEIs or ARBs, statins, thiazolidinedione, the fasting blood glucose level, and systolic blood pressure were not determinants. Additional analysis was performed in DM patients and non-DM patients. Similarly, in both DM and non-DM patients, sex; eGFR; total cholesterol, HDL cholesterol, and triglyceride levels; and the logarithm of UACR were common determinants. In non-DM patient, BMI and the fasting blood glucose level were included with independent predictors of the logarithm of serum adiponectin.
Discussion
In the present study, the serum adiponectin level was much higher in patients with macroalbuminuria than in patients with normoalbuminuria or microalbuminuria. Albuminuria and the HDL cholesterol level were positively correlated with serum adiponectin, whereas serum albumin, BMI, and eGFR were inversely correlated with this protein. In stepwise multiple regression analysis, the logarithm of UACR; sex; eGFR; BMI; and total cholesterol, HDL cholesterol, and triglyceride levels were independent predictors of the logarithm of serum adiponectin. This result strongly suggests that renal proteinuria is compensated by a substantial increase in adiponectin synthesis in CKD patients with high levels of albuminuria.
Adiponectin is a peptide hormone secreted from adipocytes that has insulin-sensitizing, anti-artherogenic, and anti-inflammatory properties [11, 12]. It was reported that serum adiponectin is inversely related to eGFR [6, 13]. Adiponectin circulates as various isoforms and polymers [14–16], and its monomers (28 kDa) and dimers can cross the normal glomerular filtration barrier and is cleared by the kidney. It seems that a higher-molecular-weight adiponectin is not secreted in urine, thus a high-molecular-weight adiponectin can be a marker of adiponectin production independent of eGFR.
Adiponectin receptors (AdipoR) 1 and 2 are found in the kidney and are located in the intrarenal arterioles, endothelium, podocytes, mesangial cells of the glomerulus, and proximal tubular cells [17, 18]. AdipoR 1 can activate the AMP-activated protein kinase (AMPK) pathway that inhibits high-glucose-induced protein synthesis and reactive oxygen species protein. Sharma et al. reported that adiponectin knockout (Ad−/−) mice exhibited increased albuminuria and podocyte effacement compared with wild-type mice. In addition, Ad−/− mice treated with adiponectin exhibited normalization of albuminuria with increased glomerular AMPK activation [19]. Furthermore, rats with adenine-induced chronic renal failure had increased renal expression of AdipoR 1 and 2, and its receptors were positively correlated with serum and urinary adiponectin levels [20]. These findings indicate that renal injury may cause a compensatory up-regulation of AdipoR 1 and 2 in the kidneys to reduce further renal injury.
In most clinical human study settings, serum adiponectin level was elevated with increasing albuminuria [21, 22]. Because studies demonstrating the beneficial effects of adiponectin regarding the reduction in albuminuria were performed exclusively in animal experiments [19, 23, 24], it is necessary to cautiously interpret the relevance between human and rodent studies. The underlying mechanism is unknown, but a plausible explanation for increasing serum adiponectin in patients with macroalbuminuria or nephropathy is a beneficial compensatory mechanism that has a protective role of adiponectin against the development of albuminuria. Considering the anti-inflammatory and anti-atherosclerotic properties of adiponectin, it is postulated that increased adiponectin levels serve to protect patients at high risk of cardiovascular disease against the harmful actions of pro-inflammatory and atherosclerotic agents, as recently suggested [25].
Albuminuria is associated with DM and obesity, and increasing albuminuria constitutes an adverse cardiovascular risk factor [2, 26, 27]. Albuminuria is associated with increased renal endothelial permeability and endothelial dysfunction [28]. Adiponectin is also related to endothelial dysfunction, as it binds to the major collagen components of the intima of blood vessels and accumulates in the vascular wall when the endothelial barrier is damaged [29]. Thus, serum adiponectin may be an early and novel biomarker for cardiovascular risk together with albuminuria.
In the present study, the logarithm of serum adiponectin was determined by sex (women had a higher serum adiponectin); eGFR; BMI; total cholesterol, HDL cholesterol, and triglyceride levels; and the logarithm of UACR. Christous et al. demonstrated that serum HDL cholesterol induces adiponectin production and a positive relationship between the levels of HDL cholesterol and serum adiponectin [30]. Although the underlying mechanism was not clear, serum HDL cholesterol showed effects against albuminuria in an observational study, and it was supposed that HDL cholesterol may have a role in increased adiponectin. Women have higher circulating serum adiponectin concentrations than men [31]. As shown recently, the sex difference in adiponectin develops during puberty, and it is negatively associated with serum levels of androgen, which is believed to suppress adiponectin synthesis [32]. It has been reported that age was also related to serum adiponectin [31], but our data did not show age as a determinant factor for adiponectin. This may be explained by the fact that age was preserved in a healthy population, whereas it was absent in patients with albuminuria.
Because the signal transduction of AdipoR seems to involve activation of AMPK and p38 mitogen-activated protein kinase and peroxisome proliferator-activated receptor-α [33], we assumed that a statin or thiazolidinedione may be a determinant for serum adiponectin, but our analysis showed that they were not related factor. This may be because the number of patients taking thiazolidinedione among DM patients was only 20, which was relatively small.
This study has several limitations. Lo et al. [34] concluded that the ratio between high-molecular-weight adiponectin and low-molecular-weight adiponectin may be an important biomarker of high cardiovascular risk. We measured the total serum adiponectin so the ratio could not be determined. Second, because it was a cross-sectional analysis of baseline data of a cohort study, we could not determine the association between serum adiponectin and cardiovascular events or mortality. Third, although we adjusted for multiple confounding factors, it is possible that some unmeasured confounders remained.
In conclusion, the relationship between serum adiponectin and albuminuria was significant in patients with CKD, independent of eGFR. Furthermore, serum adiponectin was associated with renal insufficiency and lipid profiles. Adiponectin may be key in understanding the pathophysiological roles of association among obesity and CKD, and albuminuria.
References
Vivante A, Golan E, Tzur D, Leiba A, Tirosh A, Skorecki K, et al. Body mass index in 1.2 million adolescents and risk for end-stage renal disease. Arch Intern Med. 2012;172:1644–50.
Diez JJ, Iglesias P. The role of the novel adipocyte-derived hormone adiponectin in human disease. Eur J Endocrinol. 2003;148:293–300.
Nakamaki S, Satoh H, Kudoh A, Hayashi Y, Hirai H, Watanabe T. Adiponectin reduces proteinuria in streptozotocin-induced diabetic Wistar rats. Exp Biol Med (Maywood). 2011;236:614–20.
Ohashi K, Iwatani H, Kihara S, Nakagawa Y, Komura N, Fujita K, et al. Exacerbation of albuminuria and renal fibrosis in subtotal renal ablation model of adiponectin-knockout mice. Arterioscler Thromb Vasc Biol. 2007;27:1910–7.
Christou GA, Kiortsis DN. The role of adiponectin in renal physiology and development of albuminuria. J Endocrinol. 2014;221:R49–61.
Zoccali C, Mallamaci F, Tripepi G, Benedetto FA, Cutrupi S, Parlongo S, et al. Adiponectin, metabolic risk factors, and cardiovascular events among patients with end-stage renal disease. J Am Soc Nephrol. 2002;13:134–41.
Oh KH, Park SK, Park HC, Chin HJ, Chae DW, Choi KH, et al. KNOW-CKD (KoreaN cohort study for Outcome in patients With Chronic Kidney Disease): design and methods. BMC Nephrol. 2014;15:80.
Levey AS, Stevens LA, Schmid CH, Zhang YL, Castro AF 3rd, Feldman HI, et al. A new equation to estimate glomerular filtration rate. Ann Intern Med. 2009;150:604–12.
Magkos F, Sidossis LS. Recent advances in the measurement of adiponectin isoform distribution. Curr Opin Clin Nutr Metab Care. 2007;10:571–5.
National Kidney Foundation. K/DOQI clinical practice guidelines for chronic kidney disease: evaluation, classification, and stratification. Am J Kidney Dis. 2002;39:S1–266.
Gil-Campos M, Canete RR, Gil A. Adiponectin, the missing link in insulin resistance and obesity. Clin Nutr. 2004;23:963–74.
Stefan N, Stumvoll M. Adiponectin—its role in metabolism and beyond. Horm Metab Res. 2002;34:469–74.
Fujita H, Morii T, Koshimura J, Ishikawa M, Kato M, Miura T, et al. Possible relationship between adiponectin and renal tubular injury in diabetic nephropathy. Endocr J. 2006;53:745–52.
Pajvani UB, Du X, Combs TP, Berg AH, Rajala MW, Schulthess T, et al. Structure-function studies of the adipocyte-secreted hormone Acrp30/adiponectin. Implications for metabolic regulation and bioactivity. J Biol Chem. 2003;278:9073–85.
Waki H, Yamauchi T, Kamon J, Ito Y, Uchida S, Kita S, et al. Impaired multimerization of human adiponectin mutants associated with diabetes. Molecular structure and multimer formation of adiponectin. J Biol Chem. 2003;278:40352–63.
von Eynatten M, Liu D, Hock C, Oikonomou D, Baumann M, Allolio B, et al. Urinary adiponectin excretion: a novel marker for vascular damage in type 2 diabetes. Diabetes. 2009;58:2093–9.
Cammisotto PG, Bendayan M. Adiponectin stimulates phosphorylation of AMP-activated protein kinase alpha in renal glomeruli. J Mol Histol. 2008;39:579–84.
Perri A, Vizza D, Lofaro D, Gigliotti P, Leone F, Brunelli E, et al. Adiponectin is expressed and secreted by renal tubular epithelial cells. J Nephrol. 2013;26:1049–54.
Sharma K, Ramachandrarao S, Qiu G, Usui HK, Zhu Y, Dunn SR, et al. Adiponectin regulates albuminuria and podocyte function in mice. J Clin Investig. 2008;118:1645–56.
Yu Y, Bao BJ, Fan YP, Shi L, Li SQ. Changes of adiponectin and its receptors in rats following chronic renal failure. Ren Fail. 2014;36:92–7.
Koshimura J, Fujita H, Narita T, Shimotomai T, Hosoba M, Yoshioka N, et al. Urinary adiponectin excretion is increased in patients with overt diabetic nephropathy. Biochem Biophys Res Commun. 2004;316:165–9.
Jorsal A, Petersen EH, Tarnow L, Hess G, Zdunek D, Frystyk J, et al. Urinary adiponectin excretion rises with increasing albuminuria in type 1 diabetes. J Diabetes Complicat. 2013;27:604–8.
Guo X, Zhou G, Guo M, Cheung AK, Huang Y, Beddhu S. Adiponectin retards the progression of diabetic nephropathy in db/db mice by counteracting angiotensin II. Physiol Rep. 2014;2:e00230.
Rutkowski JM, Wang ZV, Park AS, Zhang J, Zhang D, Hu MC, et al. Adiponectin promotes functional recovery after podocyte ablation. J Am Soc Nephrol. 2013;24:268–82.
Rabin KR, Kamari Y, Avni I, Grossman E, Sharabi Y. Adiponectin: linking the metabolic syndrome to its cardiovascular consequences. Expert Rev Cardiovasc Ther. 2005;3:465–71.
Hashikawa-Hobara N, Chan NY, Levi R. Histamine 3 receptor activation reduces the expression of neuronal angiotensin II type 1 receptors in the heart. J Pharmacol Exp Ther. 2012;340:185–91.
Gerstein HC, Mann JF, Yi Q, Zinman B, Dinneen SF, Hoogwerf B, et al. Albuminuria and risk of cardiovascular events, death, and heart failure in diabetic and nondiabetic individuals. JAMA. 2001;286:421–6.
Stehouwer CD, Nauta JJ, Zeldenrust GC, Hackeng WH, Donker AJ, den Ottolander GJ. Urinary albumin excretion, cardiovascular disease, and endothelial dysfunction in non-insulin-dependent diabetes mellitus. Lancet. 1992;340:319–23.
Nishigaki Y, Fujiuchi S, Fujita Y, Yamazaki Y, Sato M, Yamamoto Y, et al. Increased serum level of vascular endothelial growth factor in Mycobacterium avium complex infection. Respirology. 2006;11:407–13.
Christou GA, Tellis KC, Elisaf MC, Tselepis AD, Kiortsis DN. High density lipoprotein is positively correlated with the changes in circulating total adiponectin and high molecular weight adiponectin during dietary and fenofibrate treatment. Hormones (Athens). 2012;11:178–88.
Obata Y, Yamada Y, Takahi Y, Baden MY, Saisho K, Tamba S, et al. Relationship between serum adiponectin levels and age in healthy subjects and patients with type 2 diabetes. Clin Endocrinol (Oxf). 2013;79:204–10.
Laughlin GA, Barrett-Connor E, May S. Sex-specific determinants of serum adiponectin in older adults: the role of endogenous sex hormones. Int J Obes (Lond). 2007;31:457–65.
Kadowaki T, Yamauchi T, Kubota N, Hara K, Ueki K, Tobe K. Adiponectin and adiponectin receptors in insulin resistance, diabetes, and the metabolic syndrome. J Clin Investig. 2006;116:1784–92.
Lo MM, Salisbury S, Scherer PE, Furth SL, Warady BA, Mitsnefes MM. Serum adiponectin complexes and cardiovascular risk in children with chronic kidney disease. Pediatr Nephrol. 2011;26:2009–17.
Acknowledgments
This research was supported by grants 2011E3300300, 2012E3301100 and 2013E3301600 from Research of Korea Centers for Disease Control and Prevention, and by Basic Science Research Program through the National Research Foundation of Korea (NRF) funded by the Ministry of Science, ICT and future Planning (2013R1A2A2A01067611).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have declared that no conflict of interest exists.
About this article
Cite this article
Kim, H.Y., Bae, E.H., Ma, S.K. et al. Association of serum adiponectin level with albuminuria in chronic kidney disease patients. Clin Exp Nephrol 20, 443–449 (2016). https://doi.org/10.1007/s10157-015-1173-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10157-015-1173-4