Abstract
Background
The aim of the present study was to compare sacral nerve stimulation (SNS) for constipation (SNS-C) with SNS for idiopathic faecal incontinence (SNS-IFI) regarding explantation rate, additional visits, and improvement of patient satisfaction 5 years after implantation.
Methods
From our prospective database (launched in 2009), we extracted all SNS-C patients 5 years post-implantation, and the SNS-IFI patients implanted just before and just after each SNS-C patient. We retrospectively evaluated the explantation rate, number of additional visits, and patient satisfaction using a visual analogue scale (VAS). We hypothesized that compared with those in the SNS-IFI group: (1) the explantation rate would be higher in SNS-C patients, (2) the number of additional visits would be higher in SNS-C patients, and (3) in patients with an active implant at 5 years, the improvement in VAS would be the same.
Results
We included 40 SNS-C patients and 80 SNS-IFI patients. In the SNS-C group 7/40 (17.5%), patients were explanted, compared to 10/80 (12.5%) patients in the SNS-IFI group (p = 0.56). The mean number of additional visits in the SNS-C group was 3.5 (95% CI 2.8–4.1)) and 3.0 (95% CI 2.6–3.6)) in the SNS-IFI group (p = 0.38). Additional visits due to loss of efficacy were significantly higher in the SNS-C patients (p = 0.03). The reduction in VAS score (delta VAS) at 5 years was 37.1 (95% CI 20.9–53.3) in the SNS-C group, and 46.0 (95% CI 37.9–54.0) in the SNS-IFI group (p = 0.27).
Conclusions
No significant difference was found regarding explantation rate, number of additional visits, or improvement of VAS at 5 years after SNS implantation between SNS-C patients and SNS-IFI patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Constipation is a common disorder in the adult Western population and has a very negative impact on quality of life [1, 2]. Constipation can be categorized into slow-transit constipation, obstructed defaecation syndrome (ODS) with normal transit, or a combination of both [3,4,5]. Conservative therapy is the first-line treatment [5] and surgery is only indicated in highly selected and motivated patients not responding sufficiently to conservative therapy [1, 6].
Sacral nerve stimulation (SNS) was introduced for the treatment of faecal incontinence (FI) in 1995 by Matzel et al. [7]. The exact mechanism of action of SNS is unclear. However, it is generally accepted that afferent neuromodulation appears to have a central role [8, 9]. Over the last 25 years, SNS has become an accepted treatment for FI. The short- and mid-term success of SNS in patients with FI has been demonstrated in several studies [10,11,12,13]. Recently, studies with long-term follow-up have shown a lasting effect [13,14,15,16].
In 2001, SNS was introduced in Europe for the treatment of constipation, since early cohort studies reported high success rates [17,18,19,20]. However, the role of SNS in constipation has been questioned, as several studies including two prospectively randomized studies suggested that the effects of SNS were poor and non-lasting [5, 6, 13, 20,21,22]. Currently, no predictors have been found that can identify the constipated patients who would be most likely to benefit from SNS. However, it has been speculated that constipated patients with combined rectal hyposensitivity may have a high response rate to SNS therapy [23].
The aims of this study were to compare postoperative events (explantation rate, number of additional visits) and patient satisfaction at 5 years post-SNS implantation for patients permanently implanted with SNS for the indication constipation (SNS-C) with those permanently implanted with SNS in the same period for the indication idiopathic faecal incontinence (IFI) (SNS-IFI). Furthermore, the correlation between rectal sensitivity to distension preimplantation and VAS at 5-year follow-up was explored for patients treated with SNS for the indication of slow transit constipation.
Materials and methods
In May 2009, the SNS prospective database (SNSPD) was launched to collect detailed pre-, intra- and postoperative information in all patients undergoing SNS for bowel dysfunction. Since its introduction, it has been in use at Aarhus University Hospital, Denmark, and all patients with a permanent implantation are followed according to database criteria. The details of the database and its content have been previously published [24].
The database includes indications for SNS, explantation, additional visits, patient satisfaction by using a visual analogue scale (VAS), Wexner incontinence score, Wexner constipation score (CCCS) [25], the Altomare ODS scoring system [26] and preimplantation rectal sensitivity to distension for patients diagnosed with slow transit constipation [27]. In September 2019, the data for the present study were extracted from the SNSPD for all SNS-C patients if they had at least 5 years of follow-up. The data for SNS-IFI patients, implanted just before and after each SNS-C patient, were also extracted to be used as a control group.
Constipation was defined as ≤ 2 bowel evacuations per week on average and/or straining to evacuate during ≥ 25% of attempts to evacuate and/or sensation of incomplete evacuation after defecation in ≥ 25% of occasions [17]. We subdivided constipation into slow-transit constipation (with or without ODS) and ODS with normal transit time.
Faecal incontinence was classified as IFI if there was no history of anorectal surgery, diabetes, spinal cord injury, neurological disorder or thyroid dysfunction, We included patients with minor external anal sphincter defects on ultrasonography if they had no history of a sphincter repair.
Before investigation at the pelvic floor clinic, all patients had clinical evaluation including endoscopy to exclude cancer, inflammatory bowel disease or other relevant diseases and conditions before treatment. All patients considered suitable for SNS were offered a 3-week peripheral nerve evaluation (PNE) test stimulation if conservative therapy had failed. Patients with constipation were offered permanent implantation if at least a 50% improvement in the number of bowel movements, straining or incomplete evacuations per week was obtained, and patients with IFI were permanently implanted if at least a 50% reduction in the number of incontinence episodes per week was observed. After permanent implantation, patients had a planned follow-up after 1, 3, 6, and 12 months and then yearly. Explantation was defined as the removal of the permanent lead, pacemaker or both [28].
All contacts between the planned follow-ups were recorded as additional visits. These visits were labelled according to the reason for the additional visit (loss/lack of efficacy, pain, infection, lead/ implantable pulse generators (IPG) migration or erosion, technical device problem and other).
For both SNS-C patients and SNS-IFI patients, patient satisfaction was measured by the impact of the symptoms on daily life using a visual analogue scale (VAS) (score; 0 no impact, 100 maximum impact). Improvement in patient satisfaction was measured as the delta values between preimplantation and 5-year follow-up for each patient with active SNS.
For patients with an active pacemaker, the difference between baseline and 5-year follow-up was calculated. In the SNS-C, the functional outcome was evaluated using the CCCS, Altomare ODS score, and the SNS-IFI was evaluated using the Wexner incontinence score. In case of missing data, the last recorded data were carried forward.
Based on the currently limited literature, we hypothesized that after 5 years of follow-up:
-
1.
The explanation rate would be higher among the SNS-C patients, than among the SNS-IFI patients.
-
2.
The number of additional visits would be higher among the SNS-C patients, than among the SNS-IFI patients.
-
3.
In patients with active SNS at 5 years, the improvement in patient satisfaction would be similar between the SNS-C patients and SNS-IFI patients.
Statistical analysis
A power calculation was performed based on the primary hypothesis (explantation rate). According to a previous publication from the SNSPD, the explantation rate for patients treated with SNS for faecal incontinence was 5% after median 22.9 (range 1.1–51.9) months of follow-up [23]. We hypothesized that the explantation rate in the constipated group would be at least 20%. Based on these assumptions and a 5% significance level (one sided), the study would have a power of 82%.
Data are presented as the median and range. Whenever possible, patients served as their own controls using the paired t test, otherwise an unpaired t test was used. Statistical comparisons between groups were performed using the Mann–Whitney U test or the two-tailed Fisher’s exact test as appropriate. p values ≤ 0.05 were considered statistically significant. All statistics were performed with Stata version 10.1. Stata Corporation, College Station, TX, USA.
Results
Baseline demographics
In total, 40 SNS-C patients with at least 5 years of follow-up were compared with 80 SNS-IFI patients. There were no significant differences in sex or preimplantation VAS satisfaction score by indication. Patients in the SNS-C group were significantly younger than those in the SNS-IFI group (median age 50 [IQR 43–61] years versus 63.5 [IQR 52.5–74.5] years; p = 0.001) (Table 1).
Comparisons of 5-year outcomes between SNS-C and SNS-FI
Explantation rate
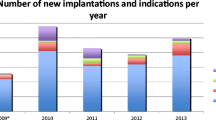
After 5 years of follow-up, seven (17.5% (95% CI 7.3–32.89)) patients in the SNS-C and ten (12.5% (95% CI 6.2–21.8)) patients in the SNS-FI were explanted (p = 0.56). Figure 1 illustrates the number of patients with an active implant over time. The indications for explantation were not significantly different between the SNS-C and SNS-IFI patients (Table 2).
Additional visits
The mean number of additional visits during the first 5 years of follow-up was 3.5 (95% CI 2.8–4.1) in the SNS-C group and 3.0 (95% CI 2.6–3.6) in the SNS-IFI group (p = 0.38). Additional visits due to loss of efficacy were more common (p = 0.03) in the SNS-C patients (Table 3).
Improvement in VAS score
At 5 years, the delta value was 37.1 (95% CI 20.9–53.3) in the SNS-C patients and 46.0 (95% CI 37.9–54.0) in the SNS-IFI patients (p = 0.269). The delta values at follow-up from 1 month to 5 years are shown in Table 4.
Symptom improvement by indication
For the SNS-C patients implanted for slow-transit constipation with an active implant at 5 years, the CCCS was significantly reduced from 16 (range 9–23) at baseline to 12 (range 4–20) at the 5-year follow-up (p = < 0.001). In the ODS patients with an active implant, there was a statistically significant reduction in the Altomare ODS score from 17 (range 11–21) at baseline to 11.5 (range 2–19) at the 5-year follow-up (p = 0.017). For the SNS-IFI patients with an active implant at 5 years, the Wexner incontinence score was significantly reduced from 14.9 (range 7–20) at baseline to 9.4 (range 1–18) at the 5-year follow-up (p = < 0.001).
Rectal sensitivity at baseline and correlation to VAS during follow-up
In SNS-C patients with slow-transit constipation, a regression analysis was performed to determine whether rectal distension volume (first sensation, desire to defaecate and maximum tolerable volume) could be correlated to delta VAS at the 5-year follow-up. There were no significant associations between first sensation, desire to defaecate, maximum tolerable volume and VAS improvements (p = 0.58, 0.65, 0.31) (data not shown).
Discussion
In this single-centre retrospective study, we compared postoperative events in patients treated with SNS for constipation or IFI at 5-year follow-up. We found no significant difference regarding explantation rates, the need for additional visits or patient satisfaction between the two groups.
In 2001, Ganio et al. introduced SNS as a treatment option for chronic constipation in patients who had failed conservative therapy. Several studies with a relatively small number of patients have confirmed the efficacy of SNS in the treatment of constipation [10,11,12,13]. Recently, two randomized studies, both crossover double-blinded sham controlled, did not document any efficacy of SNS therapy for constipation [6, 29].
In this study, all SNS-C patients were extracted from our prospectively maintained SNS database. To strengthen the power of the comparison, we included double the number of SNS-IFI patients as a control group by extracting patients implanted just before and after each SNS-C patient. Using this method, any change over time, such as the programming method or implantation technique, would not influence the comparison.
As previous reports have shown, the long-lasting efficacy of SNS therapy for constipation is approximately 30% [22]. We hypothesized that the explantation rates would be at least 20% in the SNS-C group and 5% in the SNS-IFI group. However, in the current series, the explantation rates were not significantly different between SNS-C patients (17.5% (95% CI 7.3–32.89)) and SNS-IFI patients (12.5% (95% CI 6.2–21.8)) (p = 0.56). Our explantation rates are comparable to those of other reports [30]. Although we observed a higher explantation rate in the SNS-C group, the difference was non-significant. This could be due to a type-II error, owing to the limited number of patients treated with SNS for constipation in our department.
Similarly, we hypothesized that the number of additional visits would be higher in the SNS-C group. In our material, the total number of additional visits was not significantly different between the SNS-C and SNS-IFI patients (p = 0.38), but additional visits due to loss of efficacy were significantly more common among the SNS-C patients. The initial effect of the stimulation with subsequent loss of efficacy could indicate a placebo effect, as previously reported [20].
At 5-year follow-up, we found no significant difference (p = 0.269) in the VAS scores for patient satisfaction between the SNS-C and SNS-IFI patients. At all follow-ups, the improvement in the VAS score compared to the preimplantation level was lower in the SNS-C group than in the SNS-FI group. The difference was statistically significant in the follow-up period from 6 to 36 months (p = 0.048, 0.022, 0.030, 0.008). One explanation for this difference could be that the explantation rate in the SNS-C group is lower until the 36-month follow-up (Fig. 1). Furthermore, an increased number of reprogramming sessions were needed in the SNS-C group (Table 3), indicating that it is more difficult to identify the optimal stimulation setting or to recognize a placebo effect in this group of patients.
The SNS-C patients were significantly younger than the SNS-IFI patients, and it could be speculated that this age difference explains the increased number of additional visits due to loss of efficacy, as young patients may be more persistent in attempting to achieve an optimal treatment response.
We have previously reported that as an evaluation tool, the VAS, is valid for patients with faecal incontinence treated with SNS, and a reduced score correlates with a reduction in the number of incontinence episodes [31]. Patient-reported outcome measures (PROMs) are important both at the initial evaluation and during follow-up of initiated therapy in patients with functional disorders. Two PROMs for constipation have recently been developed [32, 33], and in the future they may be useful for the evaluation of the impact of constipation on quality of life.
The limitations of this study include its retrospective design, but all evaluations of functional outcomes were collected prospectively and high data quality has been documented [24]. We only implanted a limited number of patients for the indication constipation which increases the risk of a type-II error. Furthermore, all evaluation methods used for functional outcome were based on symptom scores. For patients with slow-transit constipation, a radiological evaluation with colonic transit time during follow-up could have strengthened our results.
A recent double-blinded randomized crossover study found a strong and persistent placebo effect of SNS [20]. However, in our data we found that selected patients treated with SNS therapy for constipation could expect symptom improvements that were long lasting and comparable to those of patients treated with SNS for idiopathic faecal incontinence. Other long-term reports have documented that the use of SNS for constipation is effective at least for a subgroup of patients [22, 34]. It has been speculated that patients with constipation and rectal hyposensitivity may have a high response rate to SNS therapy [23]. In our material, we could not document any relation between rectal sensitivity to distension at baseline and VAS improvement during follow-up.
Currently, a large randomized study comparing personalized conservative treatment and SNS for constipation is ongoing in Holland [35]. This study will hopefully provide further insight into the best treatment for constipation and clarify the role of SNS therapy in the treatment of constipation.
Conclusions
The role of SNS in treating constipation needs further evaluation. We found that the use of SNS for constipation was effective in selected patients. Patient satisfaction as evaluated by a VAS score and the CCCS improved at the 5-year follow-up. Explantation rates and the need for additional visits are comparable to to those of patients treated with SNS for idiopathic faecal incontinence. Further studies are needed to establish the role of SNS in constipation.
References
Holzer B et al (2008) Sacral nerve stimulation in patients with severe constipation. Dis Colon Rectum 51:524
Everhart JE, Ruhl CE (2009) Burden of digestive diseases in the United States Part II: lower gastrointestinal diseases. Gastroenterology 136:741–754
Thomas GP, Dudding TC, Rahbour G, Nicholls RJ, Vaizey CJ (2013) Sacral nerve stimulation for constipation. Br J Surg 100:174
Ratto C et al (2015) Long-term results following sacral nerve stimulation for chronic constipation. Color Dis 17(4):320–328
Schiano di Visconte M, Pasquali A, Cipolat Mis T, Brusciano L, Docimo L, Bellio G (2019) Sacral nerve stimulation in slow-transit constipation: effectiveness at 5-year follow-up. Int J Colorectal Dis 34:1529
Zerbib F et al (2017) Randomized clinical trial of sacral nerve stimulation for refractory constipation. Br J Surg 104(3):205–213
Matzel KE, Stadelmaie U, Gall FP, Hohenfellner M (1995) Electrical stimulation of sacral spinal nerves for treatment of faecal incontinence. Lancet 346:1124
Gourcerol G, Vitton V, Leroi AM, Michot F, Abysique A, Bouvier M (2011) How sacral nerve stimulation works in patients with faecal incontinence. Colorectal Dis 13(8):e203–e211
Sheldon R, Kiff ES, Clarke A, Harris ML, Hamdy S (2005) Sacral nerve stimulation reduces corticoanal excitability in patients with faecal incontinence. Br J Surg 92:1423
Hotouras A et al (2013) Outcome of sacral nerve stimulation for fecal incontinence in patients refractory to percutaneous tibial nerve stimulation. Dis Colon Rectum 56:915–920
Tjandra JJ, Chan MKY, Yeh CH, Murray-Green C (2008) Sacral nerve stimulation is more effective than optimal medical therapy for severe fecal incontinence: a randomized, controlled study. Dis Colon Rectum 51:494–502
Wexner SD et al (2010) Sacral nerve stimulation for fecal incontinence: results of a 120-patient prospective multicenter study. Ann Surg 251(3):441–449
Widmann B et al (2019) Success and complication rates after sacral neuromodulation for fecal incontinence and constipation: a single-center follow-up study. J Neurogastroenterol Motil 25(1):159–170
Hollingshead JRF, Dudding TC, Vaizey CJ (2011) Sacral nerve stimulation for faecal incontinence: results from a single centre over a 10-year period. Color Dis 13:1030–1034
Mellgren A et al (2011) Long-term efficacy and safety of sacral nerve stimulation for fecal incontinence. Dis Colon Rectum 54:1065–1075
Altomare DF, Ratto C, Ganio E, Lolli P, Masin A, Villani RD (2009) Long-term outcome of sacral nerve stimulation for fecal incontinence. Dis Colon Rectum 52:11–17
Kamm MA et al (2010) Sacral nerve stimulation for intractable constipation. Gut 59:333–340
Sharma A, Liu B, Waudby P, Duthie GS (2011) Sacral neuromodulation for the management of severe constipation: development of a constipation treatment protocol. Int J Colorectal Dis 26:1583–1587
Govaert B, Maeda Y, Alberga J, Buntzen S, Laurberg S, Baeten CG (2012) Medium-term outcome of sacral nerve modulation for constipation. Dis Colon Rectum 55:26–31
Yiannakou Y et al (2019) A randomized double-blinded sham-controlled cross-over trial of tined-lead sacral nerve stimulation testing for chronic constipation. Eur J Gastroenterol Hepatol 31(6):653–660
Patton V, Stewart P, Lubowski DZ, Cook IJ, Dinning PG (2016) Sacral nerve stimulation fails to offer long-term benefit in patients with slow-transit constipation. Dis Colon Rectum 59(9):878–885
Gortazar de las Casas S et al (2019) Sacral nerve stimulation for constipation: long-term outcomes. Tech Coloproctol 23(6):559–564
Knowles CH et al (2012) Prospective randomized double-blind study of temporary sacral nerve stimulation in patients with rectal evacuatory dysfunction and rectal hyposensitivity. Ann Surg 255:643–649
Duelund-Jakobsen J, Lehur PA, Lundby L, Wyart V, Laurberg S, Buntzen S (2016) Sacral nerve stimulation for faecal incontinence—efficacy confirmed from a two-centre prospectively maintained database. Int J Colorectal Dis 31:421–428
Agachan F, Chen T, Pfeifer J, Reissman P, Wexner SD (1996) A constipation scoring system to simplify evaluation and management of constipated patients. Dis Colon Rectum 39:681–685
Altomare DF, Spazzafumo L, Rinaldi M, Dodi G, Ghiselli R, Piloni V (2008) Set-up and statistical validation of a new scoring system for obstructed defaecation syndrome. Color Dis 10(1):84–88
Krogh K, Rhyhammer AM, Lundby L, Gregersen H, Laurberg S (2001) Comparison of methods used for measurement of rectal compliance. Dis Colon Rectum 44:199–206
Maeda Y, Matzel K, Lundby L, Buntzen S, Laurberg S (2011) Postoperative issues of sacral nerve stimulation for fecal incontinence and constipation: a systematic literature review and treatment guideline. Dis Colon Rectum 54(11):1443–1460
Dinning PG et al (2015) Treatment efficacy of sacral nerve stimulation in slow transit constipation: a two-phase, double-blind randomized controlled crossover study. Am J Gastroenterol 110(5):733–740
Bielefeldt K (2016) Adverse events of sacral neuromodulation for fecal incontinence reported to the federal drug administration. World J Gastrointest Pharmacol Ther 7(2):294–305
Duelund-Jakobsen J, van Wunnik B, Buntzen S, Lundby L, Baeten C, Laurberg S (2012) Functional results and patient satisfaction with sacral nerve stimulation for idiopathic faecal incontinence. Color Dis 14:753–759
Marquis P, De La Loge C, Dubois D, McDermott A, Chassany O (2005) Development and validation of the patient assessment of constipation quality of life questionnaire. Scand J Gastroenterol 40(5):540–551
Frank L, Kleinman L, Farup C, Taylor L, Miner P (1999) Psychometric validation of a constipation symptom assessment questionnaire. Scand J Gastroenterol 34:870–877
Maeda Y et al (2017) Long-term outcome of sacral neuromodulation for chronic refractory constipation. Tech Coloproctol 21(4):277–286
Heemskerk SCM et al (2018) Sacral neuromodulation versus personalized conservative treatment in patients with idiopathic slow-transit constipation: study protocol of the No.2-trial, a multicenter open-label randomized controlled trial and cost-effectiveness analysis. Int J Colorectal Dis 33(4):493–501
Acknowledgements
LL, SL and JDJ have received honorarium from Medtronic as speakers at meetings and/or as members of the medical advisory board. Medtronic sponsored the construction and yearly maintenance services of the database from which the data is extracted. The study design, analysis, and reporting have been conducted without the influence of Medtronic.
Funding
This study was conducted as a part of routine clinical work and no funding was received. Medtronic sponsored the construction and yearly maintenance services of the database from which the data were extracted. The study design, analysis, and reporting were conducted without the influence of Medtronic. The corresponding author had full access to all data in the study and had final responsibility for the decision to submit for publication.
Author information
Authors and Affiliations
Contributions
SL and JDJ were responsible for the study concept and design. LL and JDJ acquired and monitored the data. JH and JDJ did the statistical analysis and JH and JDJ drafted the manuscript and analysed and interpreted the data. All authors revised the manuscript for important intellectual content. JDJ was the principal investigator.
Corresponding author
Ethics declarations
Conflict of interest
The authors have nothing to disclose.
Ethical approval
No ethical approval was needed according to Danish law.
Informed consent
All patients were informed of the database content.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Hidaka, J., Lundby, L., Laurberg, S. et al. Comparison of long-term outcome of sacral nerve stimulation for constipation and faecal incontinence with focus on explantation rate, additional visits, and patient satisfaction. Tech Coloproctol 24, 1189–1195 (2020). https://doi.org/10.1007/s10151-020-02328-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10151-020-02328-0