Abstract
Background
The aim of the present study was to perform a systematic review and meta-analysis of cancer-specific outcomes after curative rectal cancer surgery comparing anastomotic leak (AL) with no leak.
Methods
PubMed, Medline and Embase databases were searched to identify studies comparing cancer-specific outcomes after rectal cancer surgery in patients with AL and without. A meta-analysis with a random-effects model was used to calculate pooled odds ratios (OR) and confidence intervals (CI) for each outcome measure.
Results
A total of 18 studies were included for meta-analysis, comprising a total of 18,039 patients after curative rectal resection (1764 AL, 16,275 without AL). The overall rate of AL was 9.8%. After AL and excluding 30-day mortality there was an increased risk of local recurrence (OR 1.50; CI 1.23, 1.82), worse overall survival (OR 0.69; CI 0.60–0.81), decreased disease free survival (OR 0.51; CI 0.36–0.73) and cancer specific survival (OR 0.71; CI 0.54–0.94). Distant recurrence (OR 1.10; CI 0.89–1.37) and overall recurrence (OR 1.33; CI 0.64–2.76) were not significantly different between the two groups.
Conclusions
AL may negatively impact cancer-specific outcomes after curative rectal cancer surgery and could be considered an independent negative prognostic factor.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Improvement in outcomes after rectal cancer treatment have occurred over the last three decades irrespective of tumour stage, largely attributable to advances seen in available therapies [1]. The standard treatment paradigm in a curative setting involves a multi-modal approach including neoadjuvant chemoradiation, surgery and adjuvant chemotherapy where indicated [2].
In locally advanced rectal cancer there is established benefit derived from using 5-fluorouracil (FU) based neoadjuvant chemoradiation to reduce local recurrence [3, 4], even where total mesorectal excision (TME) has been performed [5]. Adjuvant chemotherapy has been shown to improve recurrence, disease free and overall survival rates with 5-FU or Capecitabine based chemotherapy with the addition of oxaliplatin [6,7,8,9,10,11,12]. A Cochrane meta-analysis demonstrated a 25% reduction in risk of recurrence after usage of 5-FU based adjuvant regimens [13].
TME has been the standard surgical approach for treatment of rectal adenocarcinoma since 1982 [14]. This involves en bloc removal of the entire mesorectum via a meticulous dissection to avoid breaching the mesorectal plane. Initial reports following the advent of TME reported drastically reduced rates of local recurrence, as low as 4–9% compared with 32–55% in non-TME series [15].
Unfortunately after rectal resection 5–19% of patients will develop anastomotic leak (AL), with devastating impact on short term outcomes [16] with real time prediction of AL in its early stages [17, 18]. A recent national Dutch audit reported peri-operative mortality after AL to be 16.4% vs 3.1% without AL [19]. Whilst short term outcomes after AL are established, the effect of AL upon longer term oncological outcomes after rectal cancer surgery is unclear.
One meta-analysis from 2011 has reported increased local recurrence after rectal cancer surgery complicated by AL [20]. Espin et al. recently reported contrasting data from the Spanish Rectal Cancer Project and noted that the prior meta-analysis includes a number of pre-TME era studies and may not be supported by the subsequent published literature [21].
Our meta-analysis seeks to comprehensively investigate the effect of AL after rectal cancer surgery upon long term cancer-specific outcome measures.
Materials and methods
Search strategy
Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement guidelines were followed for conducting and reporting meta-analysis data [22]. Medline and Embase were searched from inception to July 2015 using the search terms: “anastomosis” OR “anastomotic” AND “leak” OR “dehiscence” OR “leakage” AND “recurrence” OR “local recurrence” OR “survival” OR “disease free survival” OR “overall survival”. The same terms were used to search PubMed. The search encompassed titles, abstracts, subject headings and registry words. Results were filtered to exclude animal and non-English language studies, with duplicates then removed.
Study selection
Search results were screened by title and abstract and relevant full text articles were obtained. Full text review was performed for eligibility of inclusion into meta-analysis independently by authors PW and HP. Discrepancies of opinion were resolved by discussion of the particular manuscript between authors.
Studies were considered for meta-analysis if they included attempted curative rectal cancer surgery with anastomosis and reported long term cancer specific outcomes for patients with and without AL. Appropriate cancer specific outcome measures chosen were rates of 5 year local recurrence (LR), distant recurrence (DR), overall recurrence (OR), disease free survival (DFS), cancer specific survival (CSS) and overall survival (OS). Studies with limited oncological follow-up (< 3 years) or inclusion of recurrent disease, palliative resections, perforated tumours and unmatched stage IV disease were excluded from analysis. Studies pre-dating the total mesorectal excision (TME) era were excluded [14]. Studies that did not explicitly report outcome measures after 30 or 90 day mortality data exclusion or where such outcomes could not be derived were removed from later analysis.
Data extraction
Data extraction was performed by authors PW and HP for each study into a Microsoft Excel spreadsheet (MS Office 2010). Relevant data included study author, date range, study design, patient numbers (total, AL, no AL, with and without 30/90 day mortality data exclusion), definition of anastomotic leak, definition of rectum, follow-up details, group patient characteristics (age, sex, neo-adjuvant therapy, diversion stoma, tumour characteristics and disease stage, r0/1 classification, positivity of circumferential resection margin (CRM), adjuvant chemotherapy), 5-year outcome measures (LR, DR, OR, DFS, CSS, OS).
Studies reporting outcomes for both colon and rectal resection were included if rectal data could be extracted separately for analysis.
Statistical analysis
Extracted data underwent statistical analysis with Rev Man 5.3, SPSS (version 20; IBM) and Comprehensive Meta Analysis (version 3.3.070). Patient group characteristics were compared using χ2 test without Yates correction and unpaired t-test for dichotomous and continuous variables respectively. A p value of < 0.05 was deemed significant. All outcome variables were dichotomous and were analysed with the Mantel–Haenszel statistical method and random effects model. This model was chosen as it does not assume homogeneity between included studies, either in terms of methodology or clinical characteristics, resulting in a more conservative analysis than a fixed effect model. Outcome measures were reported differently between studies and hence numbers of patients in each meta-analysis were variable. OR and 95% CI, forest and funnel plots were created for each outcome.
Risk of bias
Study quality was assessed using the Newcastle–Ottawa score for non-randomised studies in meta-analysis. (https://www.ohri.ca/programs/clinical_epidemiology/oxford.asp). Thresholds chosen for quality assessment were: < 5 ‘poor’, 5–6 ‘fair’ and ≥ 7 ‘good’.
Study heterogeneity was assessed by τ2 and χ2 testing with a quantitative measure of heterogeneity provided by the I2 measure. An I2 value of greater than 50% was considered to be evidence of substantial heterogeneity. Publication bias was assessed by funnel plot analysis and study distribution was inspected around the combined effect size. Egger’s test of funnel plot asymmetry was also performed for each outcome measure that included ten or more studies to ensure statistical power. Meta-analysis was repeated without outlier high risk studies as required to reduce bias.
Outcomes
Outcome measures for meta-analysis were chosen to test the null hypothesis of equivalent cancer specific outcomes with and without AL. Primary outcome measures comprised LR, DFS and OS. Secondary outcome measures were DR, OR and CSS.
Results
Search results
The search strategy identified a total of 7219 articles from Medline, Embase and PubMed databases (following English language and human filters). Title and abstract screening excluded 7064 records, with a further 106 excluded as duplicates. This left 49 full-text articles to be assessed for eligibility. Following full-text review 18 studies were included for meta-analysis. (Fig. 1; Table 1).
Study characteristics
The characteristics of the included 18 studies are summarised in Table 1. There was no overlap of study populations in the included studies. All studies comprised retrospective analysis with two matched case–control studies [28, 31].
Four studies recruited patients directly from national colorectal cancer registries in Norway [29], Spain [21], Denmark [24] and Sweden [31]. Three studies used pooled trial data [27, 37, 39], with the remainder either being prospectively collected multi or single center in origin.
Three studies were graded as ‘fair’ [23, 30, 39] according to the NOS criteria with the remaining 15 studies scoring 7 or above (‘good’ quality). The ‘fair’ quality studies did not report 30 day mortality and were therefore excluded from every meta-analysis except local recurrence.
Only 8 of 18 studies defined the rectum [21, 29, 31, 32, 36,37,38,39], which varied from 12 to 16 cm from the anal verge. Of the 18 included studies, 11 excluded 30 or 90 day mortality during reporting of outcome measures [21, 24,25,26,27,28,29, 32, 34, 36, 37] and a further three allowed adjusted outcome data to be derived [31, 35, 38]. Only one included stage IV patients and was appropriate for analysis due to case matching [28]. 15 studies defined anastomotic leak using a combination of clinical, radiological and interventional criteria.
Patient characteristics
A total 18,039 patients were included in the analysis of which 1764 suffered AL giving an overall leak rate of 9.8% (range 2.5–14.8%). There was an older population of patients and a greater male preponderance in those with AL (77% vs 71%; p < 0.0001, χ2). Significantly fewer patients in the AL group (40.8%) received a diverting stoma at the time of surgery compared with patients without AL (50.1%) (p < 0.0001, χ2). (see Table 2).
Tumour stage was reported in 11 studies and differently across included studies with 6 studies reporting according to UICC criteria [26, 28, 31, 36,37,38] and a further 6 studies using TNM classification [21, 28, 29, 31, 32, 35]. There was a significantly higher proportion of stage III patients in the leak group (p = 0.0015, χ2). However, TNM status was worse in the group without AL in terms of T (p = 0.0002, χ2) and N stage (p = 0.018, χ2). There was no disparity in the proportion of low rectal cancer cases between the group with and without AL (13% vs 12.2%; p = 0.6381, χ2).
Eight studies [21, 29, 31, 32, 34, 35, 37, 38] reported on neo-adjuvant therapy prior to surgery, and significantly fewer patients in the without AL group received such treatment (31% vs 11%, p < 0.0001, χ2). 8 of the 18 studies [21, 26, 30,31,32, 34] reported adjuvant chemotherapy use after surgery, with no studies quantitatively reported adjuvant treatment delay. Only 31.5% of patients in the AL group eventually received adjuvant chemotherapy, compared with 52% in the group without AL (p < 0.0001, χ2).
Outcome measures
Local recurrence
12 of 18 studies reported local recurrence after anastomotic leak, comprising a total of 13,610 patients with 1434 patients suffering AL [21, 23, 37,38,39]. 130 (9.1%) episodes of local recurrence were reported in the AL group, compared with 813 (6.7%) episodes in the group without AL. There was an increased risk of local recurrence in the AL group (OR 1.47; CI 1.17–1.85) which was highly significant (Z = 3.28, p = 0.001). There was minimal heterogeneity (τ2 = 0.03; χ2 13.29 df = 11 p = 0.27, I2 = 17%). Egger's test was not significant (p = 0.47, 2 tailed). However, funnel plot analysis revealed an outlier study [38] which was removed from subsequent analysis and produced a slight alteration in results that remained highly significant (OR 1.34 CI 1.09–1.65, Z = 2.77, p = 0.006). Heterogeneity was reduced even further and Egger’s test was non-significant (I2 = 0, τ2 = 0 Eggers 2 tailed p = 0.45) (Fig. 2).
11 of 18 studies either directly adjusted for 30 day mortality or allowed it to be derived, comprising a total of 11,951 patients (1329 AL vs 10,622 without AL) (see Fig. 3) [19, 22,23,24,25,26,27, 29, 34,35,36]. There were 144 (10.8%) events in the AL group and 824 (7.8%) in the without AL group. Local recurrence was significantly increased in the AL group (OR 1.50; CI 1.23, 1.82; Z = 4.06, p = 0.0001). There was minimal heterogeneity in this group (I2 = 0%, χ2 = 9.05, df = 10, p = 0.53, τ = 0.00) and funnel plot revealed no outliers (see Fig. 4). Egger's test was not significant (2-tailed p = 0.75). All studies in this meta-analysis scored 7 or above on NOS criteria.
Distant recurrence
Distant recurrence was only reported in 4 of 18 studies after exclusion of 30 day mortality (500 with AL, 3931 without) [24, 26, 27, 31]. There was no difference between the two groups (OR 1.10; CI 0.89–1.37) with minimal heterogeneity amongst the studies (τ2 = 0.00, χ2 = 3.98, df = 4, p = 0.41; I2 = 1%) (Fig. 5).
Overall recurrence
Only 5 of 18 studies reported overall recurrence following exclusion of 30 day mortality (305 with AL vs 2704 without) comprising just 18% of the total study population [28, 31, 33, 35, 38]. There was no significant difference between groups (OR 1.33; CI 0.64–2.76) and a high degree of heterogeneity was noted between studies (τ2 = 0.49, χ2 = 17.53 df = 4, p = 0.002; I2 = 77%) (Fig. 6).
Disease free survival
Six studies reported disease free survival (at 5 years) excluding 30 day mortality with 69.4% (455/655) DFS in the group with AL [26,27,28, 33, 35, 37]. There was greater survival in the group without AL (75.7%; 4095/5406), which was significant (OR 0.51; CI 0.36–0.73). Marked heterogeneity was noted within studies (τ2 = 0.1, χ2 = 12.67, df = 5, p = 0.03, I2 = 61%) but Egger’s test was not performed due to lack of power (Fig. 7).
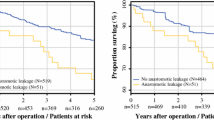
Overall survival
11 of 18 studies reported overall survival excluding 30 day mortality (722 with AL, 8535 without) [22, 24, 25, 27,28,29, 31, 32, 34, 35, 38]. 65.9% of patients with AL were alive at 5 years, compared with 75.7% without AL. There was a significant decrease in overall survival following AL (OR 0.66; CI 0.56–0.78; Z = 4.81 p < 0.00001). There was minor heterogeneity of studies (τ2 = 0.02, χ2 = 13.6, df = 10, p = 0.19, I2 = 26%) and funnel plot analysis revealed an outlier study [34] (Fig. 8).
Subsequent analysis without the outlier diminished significance only slightly (OR 0.69, CI 0.60–0.81). Egger’s test was not significant (2-tailed p = 0.28) and heterogeneity became minimal (τ2 = 0.01, I2 = 9%) (Fig. 9).
Cancer specific survival
6 of 18 studies reported cancer specific survival excluding 30 day mortality (470 with AL vs 4542 without) [21, 28, 31, 32, 36, 38]. 5 year cancer specific survival was 76.6% with AL and 82.9% without AL respectively. This proved to be significant (OR 0.71; CI 0.54–0.94; p < 0.02, Z 2.4). Heterogeneity was minimal [τ2 = 0.02, χ2 = 6.07 df = 5 (p = 0.30) I2 = 18%] with no outliers identified on funnel plot (Figs. 10, 11).
Discussion
Our meta-analysis is, to the best of our knowledge, the first to examine the full spectrum of long term cancer-specific outcomes after curative rectal cancer surgery complicated by AL. The meta-analysis was designed to limit oncological bias and followed strict inclusion and exclusion criteria with removal of studies not reporting rectal cancer surgery outcomes separately. Wide variation was noted between studies in criteria for definition of the rectum, AL and oncological outcome measures. Reporting of neoadjuvant therapy use, pathological r grade and adjuvant chemotherapy treatment was also incomplete.
In total, 18 studies with a combined patient population of 18,036 met inclusion criteria and were eligible for meta-analysis. This analysis includes published data from national colorectal cancer registries of Denmark, Norway, Spain and Sweden, and incorporates an extremely large number of patients with which to interrogate oncological outcomes after rectal cancer surgery. The principal findings are that patients who suffer AL are significantly more likely to develop LR and experience reduced DFS, CSS and OS. Furthermore, these outcomes remain significant after adjustment for exclusion of operative 30 day mortality. Our results suggest that AL increases risk of developing LR by nearly 50%, with 5 year DFS, CSS and OS reduced by 6%, 6% and 9% respectively after AL. No significant difference between groups was identified for DR, OR and CSS, but meta-analysis was limited by the small number of studies that provided data on these outcome measures.
A limitation of this meta-analysis is the heterogeneity between the two groups undergoing comparison. This can be attributed to the unmatched nature of the majority of studies in the analysis and also reflects the observation that patients who suffer AL in general display differing risk factors, patient and tumour characteristics to those who do not. In accordance with published data, patients with AL were older and more likely to be male [19]. Only two studies attempted case–control matching of patient groups with one [28] demonstrating worse outcomes after AL and no difference from the second report [31]. Both studies included relatively small patient numbers.
Tumour stage has marked prognostic implications and a difference in stage distribution between the two groups would have resulted in significant oncological impact upon outcome measures. An attempt was made to compare the composition of tumour stages between groups but unfortunately this was reported variably between studies. Limited analysis revealed a larger number of stage III patients in the group with AL, but TNM stage was more advanced in the group without AL (data from a different cohort of studies). There were too few studies with either reporting measure to perform a robust subset meta-analysis in an attempt to reduce the effect of tumour stage on outcomes.
Wang et al. in 2017 reported that AL was associated with high LR and poor survival (both overall and cancer-specific), but not with DR [40]. The exact mechanism by which AL may cause a worse oncological outcome is unknown. The presence of viable tumour cells within the bowel lumen has been established [41]. Poor outcomes have also been identified in patients with perforated tumours [42] and this supports the theory that AL allows the escape of viable tumour cells from the bowel lumen to potentially implant within the peritoneal cavity. This may explain the increased LR and reduction in DFS in patients suffering AL in our meta-analysis. The pelvis is a relatively confined area and it is feasible that AL localised to this space may only increase LR but not DR. Some studies found that peritoneal infection increased serum interleukin-6 (IL-6), vascular endothelial growth factor (VEGF), and C-reactive protein (CRP) concentrations, which are associated with poor overall and cancer-specific survival [43]. Furthermore AL causes postoperative peritoneal and pelvic infection, which may enhance proliferation, migration, and invasion capacities of cancer cells as shown in cancer cell lines in vitro [44].
This may also explain our findings of equivalent DR and OR between the two groups.
AL may prevent or delay the receipt of adjuvant chemotherapy. This may also explain poorer survival in patients with AL [45]. This study found that significantly fewer patients in the AL group received adjuvant chemotherapy than in the group without AL (31.5% vs 52%). Given the increase in morbidity and mortality with AL after rectal cancer surgery it seems logical that fewer such patients would be fit to receive adjuvant chemotherapy. Failure to receive the established survival benefit from adjuvant chemotherapy [13] may be an important factor in explaining the worse oncological outcomes after AL we have identified.
A previous meta-analysis by Mirnezami in 2011 examined oncological outcomes after colorectal cancer surgery and AL [20]. Following a rectal cancer subset analysis, an increased risk of LR after AL was reported (OR 2.05; CI 1.51–2.8) in a population of 12,202 patients (1249 AL, 10,953 without AL). This meta-analysis includes a number of pre-TME era studies [46,47,48,49] and did not exclude studies with unmatched stage IV disease [50], or report on DR, OR, DFS, CSS or OS specific to rectal cancer surgery. A recent meta-analysis performed in 2017 by Won Ha et al. studied oncologic impact of anastomotic leakage following colorectal cancer surgery [51]. The rectal cancer subset analysis showed increased local recurrence (RR 1.62, 95% CI 1.29–2.05,) and reduced OS (RR 1.45, 95% CI 1.26–1.67). AL had no significant effect on distant recurrence (RR 1.04, 95% CI 0.89–1.21). This meta-analysis subgroup also included a number of pre-TME studies and the authors had commented on variable follow up periods as being a study limitation.
Our use of more rigorous exclusion criteria and the addition of recent published studies [21, 23, 30, 33, 35, 38, 39] to the meta-analysis provides a current and precise understanding of the impact of AL on long term outcomes in a significantly larger patient population (n = 18,039). Furthermore, our results agree with the findings of the previous meta-analyses by also demonstrating a significant association between AL and the development of LR. The attenuated significance in our meta-analysis (OR 1.50; CI 1.23, 1.82) may be due to the inclusion of more recently published data.
Conclusions
Our results confirm that AL significantly worsens LR after curative rectal cancer surgery and demonstrates that this negative oncological effect extends also to all survival outcomes. The latter findings are novel to this analysis and have not been examined or reported elsewhere. The addition of tumour stage-specific outcome analysis or larger matched case–control studies in the future may allow the true effect of AL on oncological outcome to be more clearly elucidated. Patients with AL after rectal curative surgery may require special attention in terms of adjuvant therapy. AL may be an independent negative prognostic factor and adjuvant therapy should be strongly considered in these patients.
References
Rutter CM, Johnson EA, Feuer EJ et al (2013) Secular trends in colon and rectal cancer relative survival. J Natl Cancer Inst 105(23):1806–1813
Janjua Z, Moran B (2014) Rectal cancer-specialist practice, p(69) (ISBN: 978–0–7020–4965)
Folkesson J, Birgisson H, Pahlman L et al (2005) Swedish Rectal Cancer Trial: long lasting benefits from radiotherapy on survival and local recurrence rate. J Clin Oncol 23:5644–5650
Sauer R, Liersch T, Merkel S et al (2012) Preoperative versus postoperative chemoradiotherapy for locally advanced rectal cancer: results of the German CAO/ARO/AIO-94 randomized phase III trial after a median follow-up of 11 years. J Clin Oncol 30:1926–1933
van Gijn W, Marijnen CA, Nagtegaal ID et al (2011) Preoperative radiotherapy combined with total mesorectal excision for resectable rectal cancer: 12-year follow-up of the multicentre, randomised controlled TME trial. Lancet Oncol 12:575–582
Fisher B, Wolmark N, Rockette H et al (1988) Postoperative adjuvant chemotherapy or radiation therapy for rectal cancer: results from NSABP protocol R-01. J Natl Cancer Inst 80:21–29
Krook JE, Moertel CG, Gunderson LL et al (1991) Effective surgical adjuvant therapy for high-risk rectal carcinoma. N Engl J Med 324:709–715
Wolmark N, Rockette H, Fisher B et al (1993) The benefit of leucovorin-modulated fluorouracil as postoperative adjuvant therapy for primary colon cancer: results from National Surgical Adjuvant Breast and Bowel Project protocol C-03. J Clin Oncol 11:1879–1887
O’Connell MJ, Martenson JA, Wieand HS et al (1994) Improving adjuvant therapy for rectal cancer by combining protracted-infusion fluorouracil with radiation therapy after curative surgery. N Engl J Med 331:502–507
Hofheinz RD, Wenz F, Post S et al (2012) Chemoradiotherapy with capecitabine versus fluorouracil for locally advanced rectal cancer: a randomised, multicentre, non-inferiority, phase 3 trial. Lancet Oncol 13:579–588
Yothers G, O’Connell MJ, Allegra CJ et al (2011) Oxaliplatin as adjuvant therapy for colon cancer: updated results of NSABP C-07 trial, including survival and subset analyses. J Clin Oncol 29:3768–3774
André T, Boni C, Navarro M et al (2009) Improved overall survival with oxaliplatin, fluorouracil, and leucovorin as adjuvant treatment in stage II or III colon cancer in the MOSAIC trial. J Clin Oncol 27:3109–3116
Petersen SH, Harling H, Kirkeby LT et al (2012) Postoperative adjuvant chemotherapy in rectal cancer operated for cure. Cochrane Database Syst Rev 3:CD004078
Heald RJ, Husband EM, Ryall RD (1982) The mesorectum in rectal cancer surgery–the clue to pelvic recurrence? Br J Surg 69(10):613–616
Havenga K, Enker WE, Norstein J et al (1999) Improved survival and local control after total mesorectal excision or D3 lymphadenectomy in the treatment of primary rectal cancer: an international analysis of 1411 patients. Eur J Surg Oncol 25:368–374
McDermott FD, Heeney A, Kelly ME, Steele RJ, Carlson GL, Winter DC (2015) Systematic review of preoperative, intraoperative and postoperative risk factors for colorectal anastomotic leaks. Br J Surg 102(5):462–479
Arezzo A, Migliore M, Chiaro P, REAL Score Collaborators et al (2019) The REAL (REctal Anastomotic Leak) score for prediction of anastomotic leak after rectal cancer surgery. Tech Coloproctol 23:649–663. https://doi.org/10.1007/s10151-019-02028-4
Rausa E1, Zappa MA2, Kelly ME et al (2019) A standardized use of intraoperative anastomotic testing in colorectal surgery in the new millennium: Is technology taking over? A systematic review and network meta-analysis. Tech Coloproctol 23(7):625–631. https://doi.org/10.1007/s10151-019-02034-6(epub 2019 Jul 13)
Bakker S, Grossmann I, Henneman D et al (2014) Risk factors for anastomotic leakage and leak-related mortality after colonic cancer surgery in a nationwide audit. Br J Surg 101(4):424–432
Mirnezami A, Mirnezami R, Chandrakumaran K et al (2011) Increased local recurrence and reduced survival from colorectal cancer following anastomotic leak: systematic review and meta-analysis. Ann Surg 253(5):890–899 (review)
Espín E, Ciga MA, Pera M et al (2015) Oncological outcome following anastomotic leak in rectal surgery. Br J Surg 102(4):416–422
Adelsdorfer C, Delgado S, Adelsdorfer W et al (2012) Influence of anastomotic leakage in the long term results of laparoscopic treatment of curative rectal cancer. Surg Endosc Other Interv Tech 26:S276
Bertelsen CA, Andreasen AH, Jorgensen T et al (2010) Anastomotic leakage after curative anterior resection for rectal cancer: short and long-term outcome. Colorectal Dis 12:e76–81
Branagan G, Finnis D (2005) Prognosis after anastomotic leakage in colorectal surgery. Dis Colon Rectum 48(5):1021–1026
Chang SC, Lin JK, Yang SH et al (2003) Long-term outcome of anastomosis leakage after curative resection for mid and low rectal cancer. Hepatogastroenterology 50(54):1898–1902
den Dulk M, Marijnen CA, Collette L et al (2009) Multicentre analysis of oncological and survival outcomes following anastomotic leakage after rectal cancer surgery. Br J Surg 96(9):1066–1075
Eberhardt JM, Kiran RP, Lavery IC (2009) The impact of leak and intra-abdominal abscess on cancer related outcomes after resection for colorectal cancer: a case control study. Dis Colon Rectum 52(3):380–386
Eriksen MT, Wibe A, Norstein J et al (2005) Anastomotic leakage following routine mesorectal excision for rectal cancer in a national cohort of patients. Colorectal Dis 7(1):51–57
Hai-Lin K, Pan C, Hui-Ming L et al (2015) The influence of anastomotic leakage of longterm survival after resection for cancer. Eur Surg Acta Chirugica Austriaca 47(S61):1682–8631
Jorgren F, Johansson R, Damber L (2011) Anastomotic leakage after surgery for rectal cancer: a risk factor for local recurrence, distant metastasis and reduced cancer-specific survival? Colorectal Dis 13(3):272–283 (1462–8910; 1463–1318)
Jung SH, Yu CS, Choi PW et al (2008) Risk factors and oncologic impact of anastomotic leakage after rectal cancer surgery. Dis Colon Rectum 51(6):902–908
Katoh H, Yamashita K, Wang G et al (2011) Anastomotic leakage contributes to the risk for systemic recurrence in stage II colorectal cancer. J Gastrointest Surg 15(1):120–129
Kulu Y, Tarantio I, Warschkow R et al (2015) Anastomotic leakage is associated with impaired overall and disease-free survival after curative rectal cancer resection: a propensity score analysis. Ann Surg Oncol 22(6):2059–2067
Lee WS, Yun SH, Roh YN et al (2008) Risk factors and clinical outcome for anastomotic leakage after total mesorectal excision for rectal cancer. World J Surg 32(6):1124–1129
Merkel S, Wang WY, Schmidt O et al (2001) Locoregional recurrence in patients with anastomotic leakage after anterior resection for rectal carcinoma. Colorectal Dis 3(3):154–160
Ptok H, Marusch F, Meyer F et al (2007) Impact of anastomotic leakage on oncological outcome after rectal cancer resection. Br J Surg 94(12):1548–1554
Smith JD, Paty PB, Weiser MR et al (2013) Anastomotic leak following low anterior resection in stage IV rectal cancer is associated with poor survival. Ann Surg Oncol 20(8):2641–2646
Steele R, Quirke P, Grieve R et al (2012) Long term outcome after anastomotic leak and the impact of short course pre-operative radiotherapy-date from the MRC CR07 trial. Colorectal Dis 14(25):1462–8910
Wang S, Liu J, Wang S, Zhao H, Ge S, Wang W (2017) Adverse effects of anastomotic leakage on local recurrence and survival after curative anterior resection for rectal cancer: a systematic review and meta-analysis. World J Surg 41(1):277–284
Umpleby HC, Fermor B, Symes MO, Williamson RC (1984) Viability of exfoliated colorectal carcinoma cells. Br J Surg 71:659–663
Slanetz CA Jr (1984) The effect of inadvertent intraoperative perforation on survival and recurrence in colorectal cancer. Dis Colon Rectum 27:792–797
Alonso S, Pascual M, Salvans S, Mayol X, Mojal S, Gil MJ, Grande L, Pera M (2015) Postoperative intra-abdominal infection and colorectal cancer recurrence: a prospective matched cohort study of inflammatory and angiogenic responses as mechanisms involved in this association. Eur J Surg Oncol 41(2):208–214
Salvans S, Mayol X, Alonso S, Messeguer R, Pascual M, Mojal S, Grande L, Pera M (2014) Postoperative peritoneal infection enhances migration and invasion capacities of tumor cells in vitro: an insight into the association between anastomotic leak and recurrence after surgery for colorectal cancer. Ann Surg 260(5):939–943
Des Guetz G, Nicolas P, Perret GY, Morere JF, Uzzan B (2010) Does delaying adjuvant chemotherapy after curative surgery for colorectal cancer impair survival? A meta-analysis. Eur J Cancer 46(6):1049–1055
Amato A, Pescatori M, Butti A (1991) Local recurrence following abdominoperineal excision and anterior resection for rectal carcinoma. Dis Colon Rectum 34:317–332
Fujita S, Teramoto T, Watanabe M et al (1993) Anastomotic leakage after colorectal surgery: a risk factor for recurrence and poor prognosis. Jpn J Clin Oncol 23:299–302
Pakkastie TE, Luukonen PE, Jarvinen HJ (1995) Anterior resection controls cancer of the rectum as well as abdominoperineal excision. Eur J Surg 161:833–839
Bell SW, Walker KG, Rickard MJFX et al (2003) Anastomotic leakage after curative anterior resection results in a higher prevalence of local recurrence. Br J Surg 90:1261–1266
Law WL, Choi HK, Lee YM et al (2007) Anastomotic leakage is associated with poor long term outcome in patients after curative colorectal resection for malignancy. J Gastrointest Surg 11:8–15
Ha W et al (2017) Oncologic impact of anastomotic leakage following colorectal cancer surgery: a systematic review and meta-analysis. Ann Surg Oncol 24(11):3289–3299
Funding
No source of funding for declaration.
Author information
Authors and Affiliations
Contributions
AK and PWW conception and design of study, acquisition of data, analysis and interpretation of data, drafting article, final approval. VC, SZ and SK drafting article, final approval. HPP acquisition of data, analysis and interpretation of data, drafting article, final approval.
Corresponding author
Ethics declarations
Conflict of interest
The authors deny any conflict of interest.
Ethical approval
The study does not contain any human participants and does not require ethical approval.
Informed consent
For this type of study formal consent is not required.
Data sharing statement
No additional data are available.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Karim, A., Cubas, V., Zaman, S. et al. Anastomotic leak and cancer-specific outcomes after curative rectal cancer surgery: a systematic review and meta-analysis. Tech Coloproctol 24, 513–525 (2020). https://doi.org/10.1007/s10151-020-02153-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10151-020-02153-5