Abstract
Background
Enzalutamide is effective against castration-resistant prostate cancer (CRPC). However, it is unclear which patients would benefit more from enzalutamide treatment. Here, we analyzed patients who received enzalutamide as first-line therapy for CRPC and evaluated the factors that predict treatment response and prognosis.
Methods
We retrospectively analyzed 101 patients treated with enzalutamide for CRPC at our institution. As primary endpoints we regarded the prostate-specific antigen (PSA) response rate and PSA–progression-free survival (PSA–PFS) from the start of enzalutamide treatment. Laboratory and imaging data were analyzed to predict treatment efficacy.
Results
PSA reductions of ≥ 50% and ≥ 90% were observed in 78 (77%) and 47 (47%) patients, respectively, compared with the baseline. During the follow-up period, 67 (66%) patients showed PSA progression, with a median PSA–PFS of 11 months. Moreover, 31 patients (31%) died, with a median overall survival of 64 months. On multivariate analysis, lymph node metastases at the start of enzalutamide treatment [odds ratio (OR) 0.0575, 95% confidence interval (CI) 0.0105–0.316, p = 0.0010] and time to CRPC (OR 0.177, 95% CI 0.0428–0.731, p = 0.0167] were associated with ≥ 90% PSA response. Lymph node metastases (hazard ratio [HR] 3.00, 95% CI 1.48–6.09, p = 0.0023) and time to CRPC (HR 1.84, 95% CI 1.02–3.30, p = 0.0419) were also predictors of PSA–PFS on a multivariate model.
Conclusions
Time to CRPC and lymph node metastasis were predictors of the PSA response rate and PSA–PFS.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Prostate cancer has been the most frequently diagnosed cancer in the United States in 2022 and the second deadliest cancer among men [1]. Of the newly diagnosed prostate cancers, 80% are localized, while the remaining 20% are advanced or metastatic [2]. Metastatic prostate cancers are treated with hormonal therapy, but almost all patients eventually progress to castration-resistant prostate cancer (CRPC) with a poor prognosis after a median of 18–24 months of hormonal therapy [3, 4]. Therefore, the 5-year overall survival rate for advanced and metastatic prostate cancer is very low at 26–30% [5]. The COU-AA-302 and PREVAIL studies demonstrated the usefulness of the androgen receptor-axis-target (ARAT) for chemo-naïve metastatic CRPC [6, 7].
In the COU-AA-302 study cohort, the presence of lymph node metastases and the number of bone metastases at the start of abiraterone acetate treatment were reported to significantly reduce radiographic progression-free survival (rPFS) in patients with metastatic CRPC [8]. Chikamatsu et al. reported that the risk classification by the CHAARTED criteria [9] at the time of CRPC diagnosis could predict prognosis after the start of its treatment [10]. However, Hatakeyama et al. reported that the CHAARTED classification at the initial diagnosis of hormone-sensitive prostate cancer (HSPC) was not associated with prognosis after the progression of CRPC [11]. Thus, there are reports predicting prognosis based on metastatic status after progression to CRPC, rather than at diagnosis. However, there are few reports predicting prognosis or treatment efficacy after the initiation of enzalutamide administration. In this study, using real-world data from Japan, we analyzed the factors influencing the outcome of enzalutamide as a first-line therapy for CRPC, focusing on imaging findings at the time of initial diagnosis and at the start of enzalutamide treatment.
Materials and methods
Study cohort
Docetaxel- and ARAT-naïve patients who received enzalutamide for CRPC at the Osaka University Hospital between 2014 and 2022 were included in the study. Patients were also included if they received docetaxel for HSPC or treated with vintage hormone therapy, steroids, or tegafur/uracil. Patients for whom sufficient clinical data could not be obtained were excluded. Ultimately, 101 patients met the study eligibility criteria (Fig. 1).
Endpoints
Since the post-hoc analysis of the PREVAIL trial reported that the prostate-specific antigen (PSA) response rate correlated with overall survival (OS), radiographic progression-free survival (rPFS), and quality of life [12], we defined the PSA response rate and PSA–progression-free survival (PSA–PFS) from the start of enzalutamide treatment as the co-primary endpoints of the study. The secondary endpoint was OS.
Clinical variables
Patients’ age, Gleason score, PSA nadir during the initial treatment for HSPC, time to CRPC, imaging results at the initial diagnosis and at the start of enzalutamide treatment, PSA levels, hemoglobin (Hb), lactate dehydrogenase (LDH), alkaline phosphatase (ALP), and testosterone at the start of enzalutamide administration were obtained from their charts. CRPC was defined as PSA progression despite androgen deprivation therapy (ADT) and serum testosterone level of < 50 ng/dL. The imaging evaluation method followed the recommendations of the prostate cancer working group 3 (PCWG3) [13]. The evaluation method for lymph node metastasis was also in accordance with the recommendations of PCWG3, with lymph nodes larger than 15 mm in the short diameter being considered positive, and lymph nodes 10–15 mm in the short diameter being judged clinically. Patients who were positive for lymph node metastasis at the time of diagnosis but whose lymph nodes had shrunk to 5 mm or less at the start of enzalutamide treatment were defined as “no lymph node metastasis at the start of enzalutamide treatment.” High-volume tumors were defined as having four or more bone metastases (at least one of which was vertebral or extrapelvic) or one or more visceral metastases, according to the criteria of the CHAATED trial [9]. Other cases were defined as low-volume tumors. PSA–PFS was defined as PSA progression (≥ 25% and ≥ 2 ng/mL increase from the nadir point) or time to last follow-up according to PCWG3 recommendations. The PSA response was defined as ≥ 90% PSA reduction from the baseline according to previous reports [7, 14].
Ethical considerations
This study was conducted with the approval of the Institutional Review Board of the Osaka University Hospital (ethical review number: 13397-20). All patients provided informed consent for their data to be used for the analysis and included in the publication.
Statistical analysis
Survival curves were generated using the Kaplan–Meier method and the log-rank test. The association between clinical variables and PSA–PFS and OS was evaluated using the Cox proportional hazards model. The relationship between clinical variables and PSA response was assessed using logistic regression analysis. All of the statistically significant variables in the univariate analysis were included in the multivariate analysis. Statistical significance was set at p < 0.05. All data were analyzed using JMP Pro version (SAS Institute Inc., Cary, NC).
Results
Patient characteristics
The clinical characteristics of the 101 patients included in the study are shown in Table 1. The median patients’ age was 74 years [interquartile range (IQR) 69–81] and the median time to CRPC was 17.5 (IQR 9.0–35.5) months. The median PSA nadir during the initial treatment for HSPC was 0.29 ng/mL (IQR 0.035–1.21). Overall, 42 (42%) patients achieved PSA nadir < 0.2 ng/mL during the initial treatment for HSPC. The median observation period was 19 (IQR 12–41) months, and the median duration of enzalutamide treatment was 11 (IQR 5–22) months. Just before the introduction of enzalutamide treatment, 21 (21%) patients had metastases in the lymph nodes, 65 (64%) in the bones, 11 (11%) in the internal organs, and 48 (48%) bore high-volume tumors. Overall, 77 (76%) patients had distant metastases at the start of enzalutamide treatment. Of the 21 patients who had lymph node metastases at the start of enzalutamide, 11 cases developed new lymph node metastases. Median Hb, LDH, ALP, PSA, and testosterone at the start of enzalutamide administration were 12.6 (IQR 11.4–13.5), 203 (IQR 175–239), 270 (IQR 209–419), 18.9 (IQR 7.9–61.6), and 0.14 (IQR 0.07–0.22), respectively.
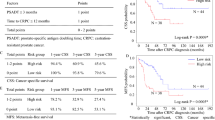
Univariate and multivariate analysis of PSA response rate
A waterfall plot of the maximum PSA response rate is shown in Fig. 2A. PSA reductions of ≥ 50% and ≥ 90% were observed in 78 (77%) and 47 (47%) patients, respectively, compared to the baseline. The associations between clinical variables and PSA response rates of ≥ 90% are shown in Table 2. In univariate analysis, PSA nadir ≥ 0.2 ng/mL during the initial treatment for HSPC [odds ratio (OR) 0.337, 95% confidence interval (CI) 0.143–0.797, p = 0.013], shorter time to CRPC (OR 0.197, 95%CI 0.0819–0.475, p = 0.0003) and the presence of lymph node metastases at the start of enzalutamide (OR 0.0783, 95% CI 0.017–0.361, p = 0.0011) were significantly associated with PSA response. In multivariate analysis, a shorter time to CRPC (OR 0.177, 95% CI 0.0428–0.731, p = 0.0167) and the presence of lymph node metastases at the start of enzalutamide treatment (OR 0.0575, 95%CI 0.0105–0.316, p = 0.0010) were independently and significantly associated with PSA response. In 77 patients with metastatic CRPC (mCRPC), shorter time to CRPC (OR 0.228, 95%CI 0.084–0.617, p = 0.0036) and the presence of lymph node metastases at the start of enzalutamide (OR 0.103, 95% CI 0.021–0.501, p = 0.0049) were significantly associated with PSA response in univariate analysis.
Univariate and multivariate analysis of PSA–PFS
The Kaplan–Meier curve for PSA–PFS is shown in Fig. 2B. Sixty-seven (66%) patients had PSA progression during the observation period, with a median PSA–PFS of 11 (IQR 8–13) months. The results of the univariate analysis of the association between clinical variables and PSA–PFS are shown in Table 3. The presence of lymph node metastases at the start of enzalutamide treatment (HR 3.20, 95% CI 1.74–5.86, p = 0.0002), shorter time to CRPC (HR 2.05, 95% CI 1.23–3.43, p = 0.0058), high-volume tumor at the start of enzalutamide treatment (HR 2.06, 95% CI 1.21–3.49, p = 0.0075), lower age (HR 1.65, 95% CI 1.01–2.69, p = 0.0439), higher ALP level (HR 1.87, 95% CI 1.06–3.32, p = 0.0315), and higher PSA levels (HR 2.68, 95% CI 1.62–4.45, p = 0.0001) were significantly associated with shorter PSA–PFS. However, none of the clinical variables at initial diagnosis correlated with a shorter PSA–PFS. In multivariate analysis, the presence of lymph node metastases at the start of enzalutamide treatment (HR 3.00, 95% CI 1.48–6.09, p = 0.0023) and time to CRPC (HR 1.84, 95% CI 1.02–3.30, p = 0.0419) were significant predictors (Table 3). The presence of lymph node metastases (HR 3.46, 95% CI 1.70–7.07, p = 0.0006) and time to CRPC (HR 2.17, 95% CI 1.21–3.91, p = 0.0096) were also significant predictors of PSA–PFS in the 77 patients with mCRPC in univariate analysis.
Univariate and multivariate analysis of OS
During the observation period, 30 patients continued to receive enzalutamide, and 71 ended enzalutamide treatment. Posterior sequential treatments after the end of enzalutamide treatment are shown in Supplementary Table 1. Among 71 patients who ended enzalutamide treatment, 35 (49%) patients were treated with docetaxel and 14 (20%) with abiraterone acetate. The Kaplan–Meier curve for OS is shown in Fig. 2C. Thirty-one (31%) patients died during the observation period, with a median OS of 64 months (IQR 38–84) months. The associations between the clinical variables and OS are shown in Table 4. In univariate analysis, shorter time to CRPC (HR 2.75, 95% CI 1.27–5.93, p = 0.0101), the presence of high-volume tumors at the start of enzalutamide treatment (HR 2.89, 95% CI 1.31–6.39, p = 0.0087), higher ALP levels (HR 3.08, 95%CI 1.32–7.20, p = 0.0095), and higher PSA levels (HR 2.51, 95% CI 1.18–5.30, p = 0.0162) were significantly associated with shorter OS. In multivariate analysis, no factors significantly shortened OS, but a shorter time to CRPC (HR 2.18, 95% CI 0.945–5.04, p = 0.0677) tended to lead to a shorter OS. Clinical parameters at diagnosis did not correlate with any of the endpoints.
Discussion
The results of this study showed that the presence of lymph node metastases at the start of enzalutamide treatment and a shorter time to CRPC were significant factors that decreased the PSA response rate and shortened PSA–PFS. There were no significant factors that shortened OS, but a shorter time to CRPC tended to shorten OS.
In particular, lymph node metastases at the start of enzalutamide treatment had the highest HR for PSA–PFS. The presence of lymph node metastases at the start of abiraterone acetate treatment has been reported to significantly reduce rPFS in patients with metastatic CRPC [8], and when combined with the results of this study, the presence of lymph node metastases at the start of ARAT may predict resistance to therapy. In contrast, in a meta-analysis evaluating OS in patients treated with docetaxel for CRPC, classified by metastatic sites, lymph node metastasis did not affect the prognosis [15]. The presence of lymph node metastases may have different implications for docetaxel and ARAT.
In patients with metastatic HSPC (mHSPC) treated with ADT, it has been reported that patients with only lymph node metastases had significantly longer OS and time to CRPC compared to patients with bone plus/minus lymph node metastases [16]. On the other hand, several recent reports have shown that the presence of lymph node metastases shortens the time to CRPC and OS in mHSPC patients [17,18,19]. The impact of the presence of lymph node metastases on the efficacy and prognosis of ADT is controversial. To date, it also remains unclear whether the presence of lymph node metastases is associated with the efficacy of ARAT in patients with mHSPC.
Chikamatsu et al. reported that a high-volume tumor at diagnosis of CRPC is a prognostic factor predicting PFS and OS after the initiation of treatment with ARAT or docetaxel [10], while Hatakeyama et al. reported that risk classification by the CHAARTED criteria at the initial presentation of HSPC was not associated with OS after progression to CRPC [11]. In our study, the presence of high-volume tumors at the start of enzalutamide treatment was also a significant factor for the shortened PSA–PFS in univariate analysis. In contrast, the presence of lymph node metastases or high-volume tumors at diagnosis did not correlate with PSA response, PSA–PFS, or OS. Thus, imaging findings after progression to CRPC are more accurate predictors of response to ARAT than the findings at initial diagnosis.
A shorter time to CRPC was associated with a significantly shorter PSA–PFS and lower PSA response. A shorter time to CRPC also tended to shorten OS, although not significantly, and was associated with all endpoints. Time to CRPC has long been described as an important prognostic factor for OS in patients with CRPC [20, 21]. Loriot et al. also reported that a time to CRPC of less than 12 months correlated with PFS and PSA response rates for ARAT [22]. A polymorphism in the androgen metabolism pathway, which has been reported to correlate significantly with the time to CRPC [23, 24], may confer resistance to ARAT. Time to CRPC did not correlate with prognosis in patients who received docetaxel in a subgroup analysis of the TAX327 trial [25], although some reports indicated that it was correlated with OS and PFS [26, 27]. Recently, Shigeta et al. reported that in patients with less than 16 months to CRPC, the longer time to docetaxel initiation was significantly associated with shorter cancer-specific survival and recommended earlier docetaxel administration for patients with shorter ADT efficacy [27].
Five laboratory parameters were analyzed in this study: Hb, LDH, ALP, PSA, and testosterone levels. Higher LDH and ALP levels were reported to be poor prognostic factors in patients with CRPC receiving abiraterone acetate in the COU-AA-301 cohort [28], and lower Hb levels were reported to shorten OS and PFS in CRPC patients receiving enzalutamide [29]. Hb and ALP levels were also reported to be poor prognostic factors for CRPC patients who received docetaxel in the TAX327 trial [30]. Templeton et al. also reported Hb, LDH, and ALP levels as poor prognostic factors for CRPC patients who received docetaxel [31]. Thus, Hb, LDH, and ALP are accepted as poor prognostic factors for CRPC. Although a high testosterone level was reported as a prognostic factor for patients with CRPC who received ARAT [32, 33], it was not a prognostic factor in the present study.
The limitations of this study are that it was a retrospective study and was conducted at a single institution with a small number of patients. Lymph node metastases at the start of enzalutamide treatment correlated with PSA response and PSA–PFS, but not with OS. This suggests that patients with lymph node metastases may not respond to enzalutamide treatment but may respond to subsequent therapies, such as docetaxel.
This study demonstrated that the time to CRPC and the presence of lymph node metastases at the start of enzalutamide treatment correlated with the enzalutamide treatment response. Therefore, it will be of great help in determining treatment strategies for patients with chemo- and ARAT-naïve CRPC.
Conclusions
A shorter time to CRPC and the presence of lymph node metastases at the start of enzalutamide were predictors of response to enzalutamide treatment in terms of both ≥ 90% PSA reduction and PSA–PFS.
Data availability
Raw data were generated at Osaka University. Derived data supporting the results of this study are available upon request from the corresponding author, KH.
References
Siegel RL, Miller KD, Fuchs HE et al (2022) Cancer statistics, 2022. CA Cancer J Clin 72:7–33
Li J, Siegel DA, King JB (2018) Stage-specific incidence rates and trends of prostate cancer by age, race, and ethnicity, United States, 2004–2014. Ann Epidemiol 28:328–330
Ritch C, Cookson M (2018) Recent trends in the management of advanced prostate cancer. F1000 Fac Rev 1513(7):F1000Res
Taylor BS, Schultz N, Hieronymus H et al (2010) Integrative genomic profiling of human prostate cancer. Cancer Cell 18:11–22
Steele CB, Li J, Huang B et al (2017) Prostate cancer survival in the United States by race and stage (2001–2009): findings from the CONCORD-2 study. Cancer 123(Suppl 24):5160–5177
Ryan CJ, Smith MR, de Bono JS et al (2013) Abiraterone in metastatic prostate cancer without previous chemotherapy. N Engl J Med 368:138–148
Beer TM, Armstrong AJ, Rathkopf DE et al (2014) Enzalutamide in metastatic prostate cancer before chemotherapy. N Engl J Med 371:424–433
Ryan CJ, Kheoh T, Li J et al (2017) Prognostic index model for progression-free survival in chemotherapy-naïve metastatic castration-resistant prostate cancer treated with abiraterone acetate plus prednisone. Clin Genitourin Cancer S1558–7673(17):30211–30212
Sweeney CJ, Chen YH, Carducci M et al (2015) Chemohormonal therapy in metastatic hormone-sensitive prostate cancer. N Engl J Med 373:737–746
Chikamatsu S, Shiota M, Yamada S et al (2022) Prognostic significance of risk stratification in CHAARTED and LATITUDE studies among Japanese men with castration-resistant prostate cancer. Prostate Int 10:7–13
Hatakeyama S, Narita S, Takahashi M et al (2020) Association of tumor burden with the eligibility of upfront intensification therapy in metastatic castration-sensitive prostate cancer: a multicenter retrospective study. Int J Urol 27:610–617
Armstrong AJ, Lin P, Higano CS et al (2019) Prognostic association of prostate-specific antigen decline with clinical outcomes in men with metastatic castration-resistant prostate cancer treated with enzalutamide in a randomized clinical trial. Eur Urol Oncol 2:677–684
Scher HI, Morris MJ, Stadler WM et al (2016) Trial design and objectives for castration-resistant prostate cancer: updated recommendations from the prostate cancer clinical trials working group 3. J Clin Oncol 34:1402–1418
Scher HI, Fizazi K, Saad F et al (2012) Increased survival with enzalutamide in prostate cancer after chemotherapy. N Engl J Med 367:1187–1197
Halabi S, Kelly WK, Ma H et al (2016) Meta-analysis evaluating the impact of site of metastasis on overall survival in men with castration-resistant prostate cancer. J Clin Oncol 34:1652–1659
Francini E, Gray KP, Xie W et al (2018) Time of metastatic disease presentation and volume of disease are prognostic for metastatic hormone sensitive prostate cancer (mHSPC). Prostate 78:889–895
Cho S, Kang SG, Tae BS et al (2012) Influence of nonregional lymph node metastasis as a prognostic factor in metastatic prostate cancer patients. Korean J Urol 53:673–679
Ali A, Hoyle A, Mistry H et al (2019) Importance of non-regional lymph nodes in assigning risk in primary metastatic prostate cancer. BJU Int 123:65–73
Narita S, Hatakeyama S, Takahashi M et al (2020) Clinical outcomes and prognostic factors in patients with newly diagnosed metastatic prostate cancer initially treated with androgen deprivation therapy: a retrospective multicenter study in Japan. Int J Clin Oncol 25:912–920
Bournakis E, Efstathiou E, Varkaris A et al (2011) Time to castration resistance is an independent predictor of castration-resistant prostate cancer survival. Anticancer Res 31:1475–1482
Frees S, Akamatsu S, Bidnur S et al (2018) The impact of time to metastasis on overall survival in patients with prostate cancer. World J Urol 36:1039–1046
Loriot Y, Eymard JC, Patrikidou A et al (2015) Prior long response to androgen deprivation predicts response to next-generation androgen receptor axis targeted drugs in castration resistant prostate cancer. Eur J Cancer 51:1946–1952
Ross RW, Oh WK, Xie W et al (2008) Inherited variation in the androgen pathway is associated with the efficacy of androgen-deprivation therapy in men with prostate cancer. J Clin Oncol 26:842–847
Yang M, Xie W, Mostaghel E et al (2011) SLCO2B1 and SLCO1B3 may determine time to progression for patients receiving androgen deprivation therapy for prostate cancer. J Clin Oncol 29:2565–2573
van Soest RJ, Templeton AJ, Vera-Badillo FE et al (2015) Neutrophil-to-lymphocyte ratio as a prognostic biomarker for men with metastatic castration-resistant prostate cancer receiving first-line chemotherapy: data from two randomized phase III trials. Ann Oncol 26:743–749
Shimabukuro T, Sakano S, Matsuda K et al (2013) Can docetaxel therapy improve overall survival from primary therapy compared with androgen-deprivation therapy alone in Japanese patients with castration-resistant prostate cancer? A multi-institutional cooperative study. Int J Clin Oncol 18:62–67
Shigeta K, Kosaka T, Hongo H et al (2019) Castration-resistant prostate cancer patients who had poor response on first androgen deprivation therapy would obtain certain clinical benefit from early docetaxel administration. Int J Clin Oncol 24:546–553
Chi KN, Kheoh T, Ryan CJ et al (2016) A prognostic index model for predicting overall survival in patients with metastatic castration-resistant prostate cancer treated with abiraterone acetate after docetaxel. Ann Oncol 27:454–460
Miyazawa Y, Sekine Y, Arai S et al (2021) A prospective study of the relationship between clinical outcomes after enzalutamide and serum androgen levels measured via liquid chromatography-tandem mass spectrometry in patients with castration-resistant prostate cancer. Eur Urol Open Sci 29:59–67
Tannock IF, de Wit R, Berry WR et al (2004) Docetaxel plus prednisone or mitoxantrone plus prednisone for advanced prostate cancer. N Engl J Med 351:1502–1512
Templeton AJ, Pezaro C, Omlin A et al (2014) Simple prognostic score for metastatic castration-resistant prostate cancer with incorporation of neutrophil-to-lymphocyte ratio. Cancer 120:3346–3352
Shiota M, Kashiwagi E, Murakami T et al (2019) Serum testosterone level as possible predictive marker in androgen receptor axis-targeting agents and taxane chemotherapies for castration-resistant prostate cancer. Urol Oncol 37:180.e19-180.e24
Sakamoto S, Maimaiti M, Xu M et al (2019) Higher serum testosterone levels associated with favorable prognosis in enzalutamide- and abiraterone-treated castration-resistant prostate cancer. J Clin Med 8:489
Acknowledgements
We would like to thank Editage (http://www.editage.com) for English language editing.
Funding
This work was supported by the Japan Society for the Promotion of Science KAKENHI [Grant number 22K09447].
Author information
Authors and Affiliations
Contributions
TO and KH contributed to the study conception and design. Material preparation and data collection and analysis were performed by TO, KH, YO, AY, TU, GY, ET, YI, YY, TK, AK, KF, and NN. Data analysis was performed by TO. The first draft of the manuscript was written by TO, and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
KH and NN have the following potential conflict of interest to report: receipt of Grants/research supports: Astellas Global.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
About this article
Cite this article
Oka, T., Hatano, K., Okuda, Y. et al. The presence of lymph node metastases and time to castration resistance predict the therapeutic effect of enzalutamide for castration-resistant prostate cancer. Int J Clin Oncol 28, 427–435 (2023). https://doi.org/10.1007/s10147-022-02288-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10147-022-02288-5