Abstract
Background
Sarcopenia impacts perioperative outcomes and prognosis in various carcinomas. We aimed to investigate whether sarcopenia at the time of chemotherapy induction in patients with urothelial carcinoma is associated with prognosis.
Methods
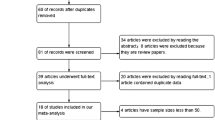
We evaluated patients treated with chemotherapy for urothelial carcinoma between April 2013 and February 2018 at our institution and affiliated centers. Skeletal muscle mass (total psoas muscle, paraspinal muscle, and total skeletal muscle areas) were used to calculate the total psoas muscle index, paraspinal muscle index, and skeletal muscle index. All participants were grouped as per cutoff points set at the median value for each sex. Overall survival was evaluated using Cox regression analysis.
Results
Of the 240 patients, 171 were men and 69 were women; mean age during chemotherapy was 71 years (range: 43–88); and 36, 56, and 148 patients were at stages II, III, and IV, respectively. Paraspinal muscle index was most associated with the prognosis; groups with lower paraspinal muscle index were defined as sarcopenic (men: ≤ 20.9 cm2/m2, women: ≤ 16.8 cm2/m2). The overall survival was significantly longer in the non-sarcopenia group including all stages (p = 0.001), and in stage III (p = 0.048) and IV (p = 0.005) patients. There was no significant difference among stage II patients (p = 0.648). After propensity score matching, survival was still significantly longer in the non-sarcopenia group (p = 0.004).
Conclusions
Paraspinal muscle index measurements obtained during chemotherapy induction for urothelial carcinoma were independent prognostic factors. The absence of sarcopenia may lead to long-term survival in patients undergoing chemotherapy for urothelial carcinoma.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Approximately, 20,000 new cases of urothelial carcinoma (UC) are diagnosed, and 7000 deaths attributed to UC occur annually in Japan [1]. Systemic chemotherapy is the standard treatment for advanced UC and involves administration of gemcitabine and cisplatin (GC) or a combination of methotrexate, vinblastine, doxorubicin, and cisplatin (MVAC), with GC being preferred because of its lower toxicity [2].
In general, locally advanced bladder cancer is also treated with neoadjuvant chemotherapy (NAC) to shrink the tumor, followed by radical cystectomy depending on the tumor size, cancer stage, and response to NAC [3]. The 2021 European Urological Association guidelines make a strong recommendation to “Offer post-operative systemic platinum-based chemotherapy to patients with muscle-invasive UTUC [4].”
However, most UC patients are older adults, and physiological changes associated with aging affect pharmacokinetics and drug sensitivity. In older adults, there is a large variation among individual patients, and it is desirable to examine the life expectancy before starting chemotherapy, and then consider whether drug therapy or dose adjustment is necessary; however, there is no clear indicator [5].
Recent geriatrics reports show that sarcopenia is associated with a worse prognosis and outcome in various diseases. The concept of sarcopenia was proposed by Rosenberg, who described the phenomenon as “age-related decrease in muscle mass” [6].
On average, it is estimated that 5–13% of older adults aged 60–70 years are affected by sarcopenia. The numbers increase to 11–50% for those aged ≥ 80 years [7].
Sarcopenia is considered to have a prognostic impact in oncology, and there has been a recent surge in reports of sarcopenia being associated with poor prognosis and outcomes in urology. Although, many studies report on the relationship between sarcopenia and surgical outcomes and survival for localized bladder cancer, few have discussed the overall survival (OS) of patients treated with systemic chemotherapy for advanced UC.
We have previously reported that sarcopenia at the time of chemotherapy induction is a prognostic factor [8], but in this study, we used multiple indices in a multicenter setting.
Materials and methods
Patients
We retrospectively reviewed 240 patients with UC who received first-line chemotherapy (GC or GCa) at our institution and affiliated facilities between April 2013 and February 2018. Most UC patients received gemcitabine 1000 mg/m2 on days 1, 8, and 15 plus cisplatin 70 mg/m2 on day 2. On the other hand, cisplatin-unfit patients [with estimated glomerular filtration rate < 60 mL/min and Eastern Cooperative Oncology Group performance status (ECOG-PS) ≥ 2] received gemcitabine 1000 mg/m2 on days 1, 8, and 15 plus carboplatin with an area under the curve of 5, according to the Calvert formula, on day 2.
Variables evaluated included age at first chemotherapy session, sex, ECOG-PS, T stage, N stage, M stage, diabetes status, smoking habits, body mass index (BMI), body surface area (BSA), pre-treatment blood biochemical data (Hgb, PLT, albumin, CRP, eGFR), and platinum drug type.
This study was approved by the Ethics Committee of Tottori University of Medicine (Approval No. 18A038).
Image analysis
All patients underwent computed tomography (CT) before chemotherapy to evaluate for sarcopenia. The cross-sectional area of the skeletal muscle at the level of the third lumbar vertebra (L3) was evaluated using the OsiriX DICOM viewer. Three parameters of skeletal muscle mass were assessed: total psoas area (TPA) (Fig. 1a); paraspinal muscle area (PSMA) including total psoas, quadratus lumborum, erector spinae, and multifidus (Fig. 1b); and skeletal muscle area (SMA) including the paraspinal, transverse abdominis, external and internal oblique abdominis, and rectus abdominis (Fig. 1c). To assess sarcopenia, these muscle areas were normalized by the square of height to calculate the total psoas muscle index (TPI) (cm2/m2), paraspinal muscle index (PSMI) (cm2/m2), and skeletal muscle index (SMI) (cm2/m2). For each index, the median value for each sex was set as the cutoff point. For SMI, patients were classified as sarcopenic according to sex-specific international consensus reference values [9].
Three muscle areas measured in the axial image of a computed tomography scan at L3 were normalized with square of the height and defined as a total psoas muscle index, b paraspinal muscle index, and c skeletal muscle index, respectively. a The cross-sectional area at L3 of the total psoas muscle (bilateral psoas muscle). b The cross-sectional area at L3 of the paraspinal muscle (including total psoas, quadratus lumborum, erector spinae, and multifidus muscle). c The cross-sectional area at L3 of the skeletal muscle (including paraspinal muscle, transversus abdominus, external and internal obliques, and rectus abdominus)
Statistics
The background and pre-treatment factors of patients and their OS were analyzed. Univariate and multivariate analyses were performed, and odds ratios were analyzed using logistic regression models. Survival curves were constructed using Kaplan–Meier analysis, and the log-rank test and Cox regression model were used for comparison between the two groups.
Thereafter, propensity score matching analyses were performed to reduce confounding bias. Propensity score matching analysis is a popular approach that uses the propensity score calculated by a logistic regression model to form matched sets with similar distributions [10]. The caliper width was set to the standard deviation of the propensity score, multiplied by 0.2. Age, sex, tumor location, T stage, N stage, M stage, surgery, and ECOG-PS were entered as covariates in the corresponding 1:1 propensity score matching model. For all tests, p values < 0.05, were considered statistically significant. Statistical analysis was conducted using SPSS Statistics software (version 24.0; SPSS Inc.).
Results
Patients
The patient characteristics before chemotherapy is shown in Table 1.
Of the 240 patients, 171 were men and 69 were women, with a mean age of 71 years (range: 43–88 years). Thirty-six patients were stage II for neoadjuvant chemotherapy, 56 were stage III for neoadjuvant or adjuvant chemotherapy, and 148 were stage IV. A total of 78 patients had tumors in the upper urinary tract, 139 in the lower urinary tract, and 22 in both. The median cutoffs of TPA were ≤ 4.35 and ≤ 2.7 cm2/m2, of PSMI were ≤ 20.9 and ≤ 16.8 cm2/m2, and of SMI were ≤ 39.3 and ≤ 30.8 cm2/m2 for men and women, respectively. Patients were also evaluated according to the international consensus reference values for men and women (men: SMI < 55 cm2/m2; women: SMI < 39 cm2/m2) [9].
Overall survival before propensity score matching
Figure 2 shows the Kaplan–Meier curve comparing the OS of the higher and lower groups of TPA, PSMI, and SMI. Setting the international standard of SMI as the cutoff, 14 patients were in the non-sarcopenia group and 226 patients were in the sarcopenia group, with no significant difference in OS (no figure, p = 0.176). Because the index mostly associated with OS was the PSMI, we adopted the median cutoffs of PSMI (men: PSMI ≤ 20.9 cm2/m2; women: PSMI ≤ 16.8 cm2/m2) as a criterion for sarcopenia. The total mean number of cycles of chemotherapy in patients with and without sarcopenia was, respectively, 4.16 and 3.63 (p = 701) for stage II, 4.00 and 3.65 (p = 0.717) for stage III, and 3.25 and 3.97 (p = 0.138) for stage IV. The log-rank test revealed that the OS of all patients in the non-sarcopenia group was significantly longer than that of those in the sarcopenia group (p = 0.001). Furthermore, the OS was not significantly different among stage II patients between the sarcopenia and non-sarcopenia groups (p = 0.648); however, stage III and IV patients in the non-sarcopenia group had significantly longer OS than those in the sarcopenia group (p = 0.048 and p = 0.005, respectively) (Fig. 2e–h).
Kaplan–Meier curves of overall survival divided into a lower group and a higher group as per the cutoff values for total psoas muscle area a–d, paraspinal muscle index e–h and skeletal muscle index i–l: a, e, i All stages, b, f, j stage II, c, g, k stage III, and d, h, l stage IV. All p values were extracted from log-rank tests
Sarcopenia was significantly associated with lower OS in multivariate analysis using the Cox regression model [hazard ratio (HR) of death = 1.948, 95% confidence interval (CI): 1.193–3.179, p = 0.008]. M stage, CRP level, and albumin level at the time of chemotherapy induction were also independent prognostic factors (Table 2).
Propensity score adjustment for patient characteristics
To further examine the accuracy of the analysis results, propensity score matching was performed between the two groups, with the corresponding clinicopathological characteristics (age, sex, tumor site, T stage, N stage, M stage, surgery, and ECOG-PS) as covariates. The matching ratio was set at 1:1, and 194 patients (97 with sarcopenia and 97 without sarcopenia) were matched. The right side of Table 1 shows the clinicopathological characteristics of the two groups after propensity score adjustment, showing that there was no significant difference between the two groups for all confounding factors (p > 0.05).
Overall survival following propensity score matching
After propensity score matching, in all stages, the OS was significantly longer in the non-sarcopenia group (p = 0.004). By stage, there was no significant difference in stage II patients (p = 0.684); however, stage III and IV patients in the non-sarcopenia group had significantly longer OS (p = 0.045 and p = 0.039, respectively). The Kaplan–Meier curve after propensity score matching is shown in Fig. 3.
Furthermore, sarcopenia was significantly associated with OS in the multivariate Cox proportional hazards model after propensity score matching (HR of death = 1.728, 95% CI: 1.014–2.946, p = 0.044; Table 3). M stage, Hgb, and CRP levels at the time of chemotherapy induction were other independent predictors of OS.
Discussion
In 1989, Rosenberg et al. proposed the term “sarcopenia” (Greek: “sarx” or flesh + “penia” or loss) to describe the age-related decrease of muscle mass [6]. Sarcopenia is considered as important as frailty in the field of geriatrics because it directly affects the quality of life and prognosis of older adults [11]. According to the clinical definition by the European Working Group on Sarcopenia in Older People (EWGSOP): (1) loss of muscle strength indicates possible sarcopenia, (2) loss of both muscle strength and skeletal muscle mass indicates confirmed sarcopenia), and (3) sarcopenia accompanied by (1) and (2), and loss of physical activity is considered severe. In addition, sarcopenia caused by aging is defined as primary sarcopenia, while that caused by other factors is defined as secondary sarcopenia [12]. In patients with cancer, the inflammatory cytokines released by cancer cells result in a hyper inflammatory state, which can lead to consumptive sarcopenia. In addition, pain and fatigue caused by cancer can indirectly cause sarcopenia via decreased activity (disuse syndrome). In advanced cancers with cachexia, muscle mass also decreases due to decreased protein synthesis [9]. In this study, there was a tendency for muscle mass to decrease as the cancer stage increased; however, the difference was not significant (data not shown). Thus, patients with carcinoma can easily develop secondary sarcopenia as cancer progresses.
The parameters of sarcopenia are muscle mass and function. The measurable parameters are considered to be muscle mass, muscle strength, and physical ability, and it is important to repeat measurements from the same individual over the long term using the same measurement method to check for changes [13]. Although, muscle strength and physical ability are difficult to assess retrospectively, there are several ways to assess muscle mass. EWGSOP recommends CT, magnetic resonance imaging (MRI), dual-energy X-ray absorptiometry (DXA), and bioelectrical impedance analysis (BIA). CT and MRI are used in general clinical practice and are considered the gold standard for measuring muscle mass in research, and many studies have measured the area of muscle mass at the level of L3. It is also easy to obtain in retrospective studies, as CT and MRI are performed for staging purposes in cancer cases [9]. Theoretically, the most reliable image-based evaluation method should be to perform CT/MRI of the whole body and measure all muscle mass, but this is not practical because of cost and radiation exposure [14].
In this study, we retrospectively analyzed the CT images obtained before the introduction of chemotherapy. Three parameters of skeletal muscle mass were calculated: TPI (cm2/m2), PSMI (cm2/m2), and SMI (cm2/m2), and the median of each was used as the cutoff. For SMI, patients were classified as sarcopenic according to sex-specific international consensus reference values [9]. Although, TPI is easily measured and several reports in the field of urology consider it a prognostic indicator, there is no international standard to define sarcopenia [9, 15]. Although there are few reports of PSMI use in oncology, it was reported to be associated with the risk of back pain in orthopedics and with survival after liver transplantation in gastrointestinal surgery [16,17,18]. SMI is currently the most widely used index of sarcopenia in oncology, with numerous reports and international standards for cutoff values [9, 12, 15]. However, in this study, 224 patients (93.3%) were defined as having sarcopenia based on international consensus reference values, which is a significant different from previous reports on the prevalence of sarcopenia. This may be due to the difference in body size between Asians and the cohort of 2115 cancer patients treated at a cancer treatment center serving northern Alberta, Canada, which is the source of the international consensus [19]. In our cohort, sarcopenia, evaluated using the median SMI and PMSI, was significantly associated with mortality. Since PMSI is simpler than SMI and is more associated with mortality, we adopted PSMI as a criterion for sarcopenia and conducted various studies.
The importance of sarcopenia in geriatrics has been recognized since early times, and it has recently been reported that sarcopenia is associated with poor prognosis and outcomes in various diseases [15]. The number of reported sarcopenia studies in oncology has increased remarkably since the beginning of the 2010s. Sarcopenia studies in oncology can be categorized into several types. The first is a study to investigate the impact of primary sarcopenia on cancer prognosis and treatment efficacy, especially in cases of early stage cancer. The second is a study to evaluate the impact of secondary sarcopenia caused by therapeutic interventions for cancer (surgery, chemotherapy, etc.) on treatment outcomes and prognosis. The third study evaluated the impact of sarcopenia on the prognosis of patients with advanced cancer.
In the field of urology, studies on the relationship between sarcopenia and prognosis before total cystectomy or total nephroureterectomy are the most common, corresponding to the first above [20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36]. Several studies have evaluated changes in muscle mass before and after total cystectomy and NAC, which corresponds to the second point above [37,38,39,40]. Several studies have evaluated the impact of sarcopenia in advanced or metastatic urothelial carcinoma, which falls within the scope of the third category of studies mentioned above [14, 16, 41,42,43].
In this report, we examined the prognostic impact of sarcopenia on 92 patients who received perioperative chemotherapy at stage III or lower and 148 patients who received induction chemotherapy at stage IV, as assessed by PSMI values, and it was a study that corresponds to the first and third categories of studies stated above. It is the largest reported stage IV case to date, and there are few reports that use PSMI to assess sarcopenia in urological oncology. In our study, the presence of sarcopenia at the time of chemotherapy induction was associated with a poor prognosis overall (all stages). When evaluated by stage, sarcopenia was associated with poor prognosis in stages III and IV but the association was not significant in stage II. Sarcopenia remained an independent prognostic factor after propensity score matching to remove confounders. One of the reported reasons for this finding is that sarcopenia is associated with chemotherapy toxicity, leading to dose reductions, dose delays, or even chemotherapy discontinuation [44, 45]. Therefore, patients with sarcopenia may not fully benefit from chemotherapy. In addition, patients with sarcopenia are susceptible to infections [46]. Sarcopenia itself may be a factor in the poor prognosis of cancer patients through these mechanisms.
As mentioned above, evidence of sarcopenia as a prognostic factor in bladder cancer has been accumulating. Since PSMI is relatively easy to measure, sarcopenia screening can be performed routinely in clinical practice.
Our study has some limitations. First, this was a retrospective study. Second, we used PSMI determined using pre therapy CT to define sarcopenia. Currently, there is no optimal evaluation method for sarcopenia, and a clear definition of sarcopenia has not been established. Therefore, future studies may be needed to accurately define sarcopenia. Despite these limitations, we were able to draw some useful conclusions from our data.
In conclusion, there have been few reports in the field of oncology that have evaluated the prognosis of patients with sarcopenia using PSMI as an index, but this study showed that PSMI is useful as a marker for predicting the prognosis of patients with UC treated with chemotherapy. Despite this study’s retrospective design and the need for further validation of its findings in a larger prospective cohort, our findings are evidence that the absence of sarcopenia increases the possibility of long-term survival in patients who are administered chemotherapy for UC.
References
Hori M, Matsuda T, Shibata A et al (2015) Cancer incidence and incidence rates in Japan in 2009: a study of 32 population-based cancer registries for the Monitoring of Cancer Incidence in Japan (MCIJ) project. Jpn J Clin Oncol 45(9):884–891. https://doi.org/10.1093/jjco/hyv088
von der Maase H, Sengelov L, Roberts JT et al (2005) Long-term survival results of a randomized trial comparing gemcitabine plus cisplatin, with methotrexate, vinblastine, doxorubicin, plus cisplatin in patients with bladder cancer. J Clin Oncol 23(21):4602–4608. https://doi.org/10.1200/JCO.2005.07.757
DeGeorge KC, Holt HR, Hodges SC (2017) Bladder cancer: diagnosis and treatment. Am Fam Physician 96(8):507–514
Leow JJ, Chong YL, Chang SL et al (2021) Neoadjuvant and adjuvant chemotherapy for upper tract urothelial carcinoma: a 2020 systematic review and meta-analysis, and future perspectives on systemic therapy. Eur Urol 79(5):635–654. https://doi.org/10.1016/j.eururo.2020.07.003
Imamura CK (2015) Dose optimization of anticancer drugs in the elderly. Gan To Kagaku Ryoho 42(1):21–25
Rosenberg IH (1997) Sarcopenia: origins and clinical relevance. J Nutr 127(5 Suppl):990S-991S. https://doi.org/10.1093/jn/127.5.990S
von Haehling S, Morley JE, Anker SD (2010) An overview of sarcopenia: facts and numbers on prevalence and clinical impact. J Cachexia Sarcopenia Muscle 1(2):129–133. https://doi.org/10.1007/s13539-010-0014-2
Yumioka T, Honda M, Nishikawa R et al (2020) Sarcopenia as a significant predictive factor of neutropenia and overall survival in urothelial carcinoma patients underwent gemcitabine and cisplatin or carboplatin. Int J Clin Oncol 25(1):158–164. https://doi.org/10.1007/s10147-019-01544-5
Fearon K, Strasser F, Anker SD et al (2011) Definition and classification of cancer cachexia: an international consensus. Lancet Oncol 12(5):489–495. https://doi.org/10.1016/S1470-2045(10)70218-7
Austin PC (2011) Optimal caliper widths for propensity-score matching when estimating differences in means and differences in proportions in observational studies. Pharm Stat 10(2):150–161. https://doi.org/10.1002/pst.433
Inouye SK, Studenski S, Tinetti ME et al (2007) Geriatric syndromes: clinical, research, and policy implications of a core geriatric concept. J Am Geriatr Soc 55(5):780–791. https://doi.org/10.1111/j.1532-5415.2007.01156.x
Cruz-Jentoft AJ, Baeyens JP, Bauer JM et al (2010) Sarcopenia: European consensus on definition and diagnosis: report of the European Working Group on Sarcopenia in Older People. Age Ageing 39(4):412–423. https://doi.org/10.1093/ageing/afq034
Lukaski H (1997) Sarcopenia: assessment of muscle mass. J Nutr 127(5 Suppl):994S-997S. https://doi.org/10.1093/jn/127.5.994S
Taguchi S, Akamatsu N, Nakagawa T et al (2016) Sarcopenia evaluated using the skeletal muscle index is a significant prognostic factor for metastatic urothelial carcinoma. Clin Genitourin Cancer 14(3):237–243. https://doi.org/10.1016/j.clgc.2015.07.015
Prado CM, Purcell SA, Alish C et al (2018) Implications of low muscle mass across the continuum of care: a narrative review. Ann Med 50(8):675–693. https://doi.org/10.1080/07853890.2018.1511918
Abe H, Takei K, Uematsu T et al (2018) Significance of sarcopenia as a prognostic factor for metastatic urothelial carcinoma patients treated with systemic chemotherapy. Int J Clin Oncol 23(2):338–346. https://doi.org/10.1007/s10147-017-1207-x
Fortin M, Battié MC (2012) Quantitative paraspinal muscle measurements: inter-software reliability and agreement using OsiriX and ImageJ. Phys Ther 92(6):853–864. https://doi.org/10.2522/ptj.20110380
Pinto Dos Santos D, Kloeckner R, Koch S et al (2020) Sarcopenia as prognostic factor for survival after orthotopic liver transplantation. Eur J Gastroenterol Hepatol 32(5):626–634. https://doi.org/10.1097/MEG.0000000000001552
Prado CM, Lieffers JR, McCargar LJ et al (2008) Prevalence and clinical implications of sarcopenic obesity in patients with solid tumours of the respiratory and gastrointestinal tracts: a population-based study. Lancet Oncol 9(7):629–635. https://doi.org/10.1016/S1470-2045(08)70153-0
Psutka SP, Carrasco A, Schmit GD et al (2014) Sarcopenia in patients with bladder cancer undergoing radical cystectomy: impact on cancer-specific and all-cause mortality. Cancer 120(18):2910–2918. https://doi.org/10.1002/cncr.28798
Smith AB, Deal AM, Yu H et al (2014) Sarcopenia as a predictor of complications and survival following radical cystectomy. J Urol 191(6):1714–1720. https://doi.org/10.1016/j.juro.2013.12.047
Wan F, Zhu Y, Gu C et al (2014) Lower skeletal muscle index and early complications in patients undergoing radical cystectomy for bladder cancer. World J Surg Oncol 12:14. https://doi.org/10.1186/1477-7819-12-14
Psutka SP, Boorjian SA, Moynagh MR et al (2015) Mortality after radical cystectomy: impact of obesity versus adiposity after adjusting for skeletal muscle wasting. J Urol 193(5):1507–1513. https://doi.org/10.1016/j.juro.2014.11.088
Hirasawa Y, Nakashima J, Yunaiyama D et al (2016) Sarcopenia as a novel preoperative prognostic predictor for survival in patients with bladder cancer undergoing radical cystectomy. Ann Surg Oncol 23(Suppl 5):1048–1054. https://doi.org/10.1245/s10434-016-5606-4
Miyake M, Morizawa Y, Hori S et al (2017) Clinical impact of postoperative loss in psoas major muscle and nutrition index after radical cystectomy for patients with urothelial carcinoma of the bladder. BMC Cancer 17(1):237. https://doi.org/10.1186/s12885-017-3231-7
Miyake M, Morizawa Y, Hori S et al (2017) Integrative assessment of pretreatment inflammation-, nutrition-, and muscle-based prognostic markers in patients with muscle-invasive bladder cancer undergoing radical cystectomy. Oncology 93(4):259–269. https://doi.org/10.1159/000477405
Saitoh-Maeda Y, Kawahara T, Miyoshi Y et al (2017) A low psoas muscle volume correlates with a longer hospitalization after radical cystectomy. BMC Urol 17(1):87. https://doi.org/10.1186/s12894-017-0279-2
Mayr R, Gierth M, Zeman F et al (2018) Sarcopenia as a comorbidity-independent predictor of survival following radical cystectomy for bladder cancer. J Cachexia Sarcopenia Muscle 9(3):505–513. https://doi.org/10.1002/jcsm.12279
Ha YS, Kim SW, Kwon TG et al (2019) Decrease in skeletal muscle index 1 year after radical cystectomy as a prognostic indicator in patients with urothelial bladder cancer. Int Braz J Urol 45(4):686–694. https://doi.org/10.1590/S1677-5538.IBJU.2018.0530
Ritch CR, Cookson MS, Clark PE et al (2019) Perioperative oral nutrition supplementation reduces prevalence of sarcopenia following radical cystectomy: results of a prospective randomized controlled trial. J Urol 201(3):470–477. https://doi.org/10.1016/j.juro.2018.10.010
Fukushima H, Nakanishi Y, Kataoka M et al (2016) Prognostic significance of sarcopenia in upper tract urothelial carcinoma patients treated with radical nephroureterectomy. Cancer Med 5(9):2213–2220. https://doi.org/10.1002/cam4.795
Ishihara H, Kondo T, Omae K et al (2017) Sarcopenia predicts survival outcomes among patients with urothelial carcinoma of the upper urinary tract undergoing radical nephroureterectomy: a retrospective multi-institution study. Int J Clin Oncol 22(1):136–144. https://doi.org/10.1007/s10147-016-1021-x
Kocher NJ, Jafri S, Balabhadra S et al (2018) Is sarcopenia and sarcopenic obesity associated with clinical and pathological outcomes in patients undergoing radical nephroureterectomy? Urol Oncol 36(4):156.e117-156.e122. https://doi.org/10.1016/j.urolonc.2017.12.004
Anno T, Kikuchi E, Fukumoto K et al (2018) Preoperative sarcopenia status is associated with lymphovascular invasion in upper tract urothelial carcinoma patients treated with radical nephroureterectomy. Can Urol Assoc J 12(3):E132–E136. https://doi.org/10.5489/cuaj.4786
Tsutsumi S, Kawahara T, Teranishi JI et al (2018) A low psoas muscle volume predicts longer hospitalization and cancer recurrence in upper urinary tract urothelial carcinoma. Mol Clin Oncol 8(2):320–322. https://doi.org/10.3892/mco.2017.1537
Itami Y, Miyake M, Tatsumi Y et al (2019) Preoperative predictive factors focused on inflammation-, nutrition-, and muscle-status in patients with upper urinary tract urothelial carcinoma undergoing nephroureterectomy. Int J Clin Oncol 24(5):533–545. https://doi.org/10.1007/s10147-018-01381-y
Mari A, D’Andrea D, Kimura S et al (2018) Sarcopenia as a predictive factor for response to upfront cisplatin-based chemotherapy in patients with muscle-invasive urothelial bladder cancer. Urol Int 101(2):197–200. https://doi.org/10.1159/000489013
Rimar KJ, Glaser AP, Kundu S et al (2018) Changes in lean muscle mass associated with neoadjuvant platinum-based chemotherapy in patients with muscle invasive bladder cancer. Bladder Cancer 4(4):411–418. https://doi.org/10.3233/BLC-180188
Zargar H, Almassi N, Kovac E et al (2017) Change in psoas muscle volume as a predictor of outcomes in patients treated with chemotherapy and radical cystectomy for muscle-invasive bladder cancer. Bladder Cancer 3(1):57–63. https://doi.org/10.3233/BLC-160080
Lyon TD, Frank I, Takahashi N et al (2019) Sarcopenia and response to neoadjuvant chemotherapy for muscle-invasive bladder cancer. Clin Genitourin Cancer 17(3):216-222.e215. https://doi.org/10.1016/j.clgc.2019.03.007
Fukushima H, Yokoyama M, Nakanishi Y et al (2015) Sarcopenia as a prognostic biomarker of advanced urothelial carcinoma. PLoS One 10(1):e0115895. https://doi.org/10.1371/journal.pone.0115895
Kasahara R, Kawahara T, Ohtake S et al (2017) A low psoas muscle index before treatment can predict a poorer prognosis in advanced bladder cancer patients who receive gemcitabine and nedaplatin therapy. Biomed Res Int 2017:7981549. https://doi.org/10.1155/2017/7981549
Fukushima H, Kataoka M, Nakanishi Y et al (2018) Posttherapeutic skeletal muscle mass recovery predicts favorable prognosis in patients with advanced urothelial carcinoma receiving first-line platinum-based chemotherapy. Urol Oncol 36(4):156.e159-156.e116. https://doi.org/10.1016/j.urolonc.2017.09.016
Antoun S, Baracos VE, Birdsell L et al (2010) Low body mass index and sarcopenia associated with dose-limiting toxicity of sorafenib in patients with renal cell carcinoma. Ann Oncol 21(8):1594–1598. https://doi.org/10.1093/annonc/mdp605
Prado CM, Baracos VE, McCargar LJ et al (2007) Body composition as an independent determinant of 5-fluorouracil-based chemotherapy toxicity. Clin Cancer Res 13(11):3264–3268. https://doi.org/10.1158/1078-0432.CCR-06-3067
Cosquéric G, Sebag A, Ducolombier C et al (2006) Sarcopenia is predictive of nosocomial infection in care of the elderly. Br J Nutr 96(5):895–901. https://doi.org/10.1017/bjn20061943
Acknowledgements
The Authors would like to thank the doctors of satellite hospitals for their contribution in data collection.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
The need for informed consent was waived because of the retrospective nature of the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
About this article
Cite this article
Shimizu, R., Honda, M., Teraoka, S. et al. Sarcopenia is associated with survival in patients with urothelial carcinoma treated with systemic chemotherapy. Int J Clin Oncol 27, 175–183 (2022). https://doi.org/10.1007/s10147-021-02032-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10147-021-02032-5