Abstract
Background
The purpose was to compare survival differences between patients with external auditory canal (EAC) cancer treated according to the University of Pittsburgh modified TNM staging system and those treated in accordance with the 8th edition of the American Joint Committee on Cancer (AJCC) staging manual on the TNM staging system for cutaneous cancers of the head and neck.
Methods
We performed a retrospective, single-institution review of 60 patients with EAC cancer treated with curative intent between September 2002 and March 2018. Survival outcomes were measured on the basis of the two staging systems.
Results
The C-index values for the overall survival (OS) rate revealed that the University of Pittsburgh staging system had higher prognostic accuracy than the 8th edition of the AJCC staging system. Univariable and multivariable analysis showed that T classification according to the University of Pittsburgh staging system was an independent predictor of the OS rate (hazard ratio 5.25; 95% confidence interval 1.38–24.9; P = 0.015). Meanwhile, the AJCC staging system could not differentiate T2 from T3–4 cancers.
Conclusion
The University of Pittsburgh staging system for patients with EAC cancer is a valuable tool for use in clinical decision-making and predicting survival outcome.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
External auditory canal (EAC) cancer is rare, with a reported prevalence of 1 per 1 million population, and accounts for less than 0.2% of all tumors of the head and neck [1, 2]. Surgical resection with or without radiotherapy (RT) is widely performed as the mainstay of treatment for EAC cancers [3,4,5,6,7]. RT alone is also the treatment of choice for early-stage tumors, and definitive chemoradiotherapy (CRT) may be appropriate for cases with unresectable tumors [8, 9]. There is a consensus that the prognosis for patients with EAC cancer is good for those with early-stage, but poor for those with advanced-stage disease [1,2,3,4, 9, 10].
The tumor, node, and metastasis (TNM) classification system has utility in determining the extent of disease, providing guidance for treatment planning, and predicting the patient’s prognosis. The University of Pittsburgh staging system for EAC cancer was proposed in 1990 as a straightforward and precise system for classifying disease before treatment [11], and then modified in 2000 [2]. To date, this classification is widely applied for determining the T category for assessment of the extent of the primary tumor. The validity of this staging system has been endorsed and confirmed by several previous studies [8,9,10, 12,13,14].
Meanwhile, there has been no agreement on a staging system for EAC cancer by the American Joint Committee on Cancer (AJCC) or the Union for International Cancer Control (UICC). Over the past few decades, the AJCC/UICC TNM staging system has been revised continuously, with the latest edition implemented in January 2017 [15]. The 8th edition of the AJCC TNM staging manual develops the classification system regarding cutaneous cancer of the head and neck, in which specific anatomic locations include the skin of the lip, temple, nose, cheek, scalp and auricle as well as EAC [15]. However, tumors located on the EAC, which possesses anatomic specificity and complexity, has been reported to show a poorer prognosis than those on other anatomic sites [16, 17]. Thus, it remains controversial whether EAC cancer can be managed comprehensively as a cutaneous cancer of the head and neck.
The aim of this study was to compare survival differences between patients with EAC cancer treated according to the University of Pittsburgh modified TNM staging system and those treated in accordance with the 8th edition of the AJCC staging manual on the TNM staging system, and to investigate whether these staging systems provide appropriate guidance for treatment planning and prediction of the survival outcome.
Materials and methods
Patients
We performed a retrospective, single-institution review of consecutive patients with previously untreated squamous cell carcinoma of the EAC treated with curative intent in the Department of Otolaryngology, Head and Neck Surgery, Hokkaido University Hospital between September 2002 and March 2018. Patients with tumors arising from the parotid, auricle, concha, or periauricular skin, a history of previous head and neck RT or lost to follow-up were excluded from this analysis.
All patients were initially evaluated by a multidisciplinary team consisting of otolaryngologists, radiation oncologists and medical oncologists. They had to be cleared for treatment, and informed consent was obtained after a full explanation of the potential risks and benefits. This research adhered to the tenets of the Declaration of Helsinki and was approved by our Institutional Review Board.
Staging system
All patients underwent a thorough history-taking, physical examination, routine blood tests, including full blood count and blood biochemistry, otoscopic examination, as well as computed tomography (CT) and magnetic resonance imaging (MRI) to evaluate the locoregional lesions. Head and neck ultrasonography (US) and/or 18[F]-fluoro-2-deoxy-d-glucose-positron emission tomography/computed tomography (18FDG-PET/CT) were performed to evaluate intraparotid involvement, lymph node metastases and distant metastases as required. Based on pre-treatment clinical findings and imaging, staging was performed using the University of Pittsburgh modified TNM staging system (Table 1) [2, 18]. Restaging was performed using the 8th edition of the AJCC staging manual on TNM staging system for cutaneous cancer of the head and neck (Table 2) [15]. Survival outcomes were compared between patients with EAC cancer treated on the basis of the two staging systems.
Treatment strategy
The selection of treatment modalities for EAC cancers was managed by a multidisciplinary team and based on the extent of disease, comorbidity, performance status, patient wishes and/or the attending physician’s discretion in each case, as stated below.
Lateral temporal bone resection was selected as the initial choice of treatment for patients with tumors confined to the EAC. The extent of the disease was confirmed by intraoperative and postoperative histologic findings. If histologic examination revealed positive surgical margins or more extensive involvement than preoperative imaging suggested, postoperative RT (a total dose of 60–70 Gy at 2.0 Gy per fraction) was performed. Patients who rejected surgery or could not undergo surgery due to comorbidities, such as severe respiratory, hepatic, renal and/or cardiovascular disease, underwent RT alone (a total dose of 65–70 Gy at 2.0–2.5 Gy per fraction).
For patients with tumors extending beyond the EAC, lateral or subtotal temporal bone resection was performed. Parotidectomy was combined with resection of the primary lesions if positive intraparotid lymph node metastasis or invasion to the parotid glands was clinically detected. Neck dissection in addition to parotidectomy was performed in cases clinically positive for neck lymph node metastasis. No prophylactic neck dissection was performed. Adjuvant RT or CRT (a total dose of 60–70 Gy at 2.0 Gy per fraction) for patients with tumors extending beyond the EAC was systematically proposed after surgical resection. For locally advanced tumors with extension to the pyramidal apex, posterior cranial fossa, middle cranial fossa or internal carotid artery, definitive CRT or RT (a total dose of 65–70 Gy at 2.0–2.5 Gy per fraction) was also performed. The regimens of TPF (cisplatin, 5-fluorouracil and docetaxel), weekly intravenous administration of cisplatin and rapid superselective high-dose cisplatin infusion (RADPLAT) were selected, as previously described [9].
Follow-up
After the completion of treatment, subsequent clinical visits were scheduled every 1–3 months for the first year, every 3–6 months for the second year, and every 6 months thereafter. CT, MRI, US and/or 18FDG-PET/CT were carried out every 6–12 months for up to 5 years after treatment. Tumor recurrence was diagnosed by histopathological examination or by imaging studies when biopsy specimens were not obtained. Patients with tumor recurrence were eligible to receive 5-fluorouracil- or tegafur-based chemotherapy.
Statistical analysis
Statistical analyses were performed using JMP software (version 10.0; SAS Institute Inc.; Cary, NC, USA) and “R language” software. A Kaplan–Meier time-to-event method was used to calculate the overall survival (OS). For the calculation of OS rates, death was counted as an event, whereas the patient being alive at the latest contact, regardless of disease status, was counted as censored. The time of interest included the date of definite diagnosis, last follow-up, recurrence and death. Survival status was updated in March 2018. The predictive accuracy of the staging systems was evaluated by Harrell’s concordance index (C-index) for the OS rate, which can range from perfect concordance (1.0) to perfect discordance (0.0) [19]. Univariable analysis was conducted in relation to OS rates, and stepwise regression analysis was carried out to build an appropriate model through the selection of predictor variables. Multivariable analysis was performed using the Cox proportional hazards model. Statistical differences were analyzed using the log-rank test, with a P value of less than 0.05 considered statistically significant.
Results
Subject profiles
A total of 60 patients with EAC cancer were enrolled according to the inclusion and exclusion criteria used for this study. The study population consisted of 26 males and 34 females, ranging in age from 39 to 87, with a median age of 65 years. The follow-up period ranged from 4 to 139 months, with a median of 47 months.
Distributions of stage and treatment modality according to the University of Pittsburgh modified TNM staging system
The distributions of T and N classifications based on the University of Pittsburgh modified TNM staging system are shown in Table 3. No patients had distant metastasis. Nineteen patients (31.7%) were categorized as stage I, 11 (18.3%) as stage II, 7 (11.6%) as stage III and 23 (38.3%) as stage IV.
The distribution of treatment modality is summarized in Table 4. Surgery was performed in 15 patients with T1, 9 with T2, 5 with T3 and 2 with T4 disease. Among the T1-2 patients with pathologically positive surgical margins, 2 patients received postoperative RT and 3 were followed by CRT. Among the T3-4 patients receiving surgery, 5 patients received postoperative RT and 2 were followed by CRT. RT alone was performed in 4 patients with T1, 2 with T2 and 4 with T4. Definitive CRT was undertaken in 6 patients with T3 and 13 with T4.
Survival outcome according to the University of Pittsburgh modified TNM staging system
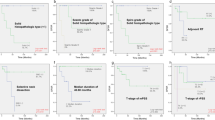
The 5-year OS rates based on the University of Pittsburgh modified TNM staging system were 94.1% for T1, 80.8% for T2, 62.5% for T3, and 46.3% for T4 (Fig. 1a). The 5-year OS rates for patients with N0 and N1 disease were 78.6 and 45.5%, respectively (Fig. 1b). The 5-year OS rates for patients with stage I, II, III and IV were 94.1, 80.8, 60.0, and 49.5%, respectively (Fig. 1c). T, N and staging classifications were correlated significantly with survival outcomes (P < 0.001, P = 0.032 and P = 0.001, respectively).
Distributions of stage and treatment modality according to the 8th edition of the AJCC staging manual on TNM staging system
The distributions of T and N classifications, and treatment modality based on the 8th edition of the AJCC staging manual on TNM staging system are shown in Tables 5 and 6, respectively. With regard to the changes in the distribution of T classification, all T2 and T3 cases according to the Pittsburgh classification shifted to T3 and T4a, respectively, according to the AJCC classification. Among the T4 cases according to the Pittsburgh classification, 2 patients (10.5%) shifted to T3 according to the AJCC classification, 8 (42.1%) to T4a and 9 (47.4%) to T4b. Nineteen (31.7%) patients were categorized as stage I, 13 (21.7%) as stage III and 28 (46.7%) as stage IV. No patients were categorized as stage II. In 18 (30.0%) of the 60 patients, the staging classification according to the AJCC system was higher than that according to the University of Pittsburgh staging system.
Survival outcome according to the 8th edition of the AJCC staging manual on TNM staging system
The 5-year OS rates regarding T, N and staging classifications based on the 8th edition of the AJCC staging manual on TNM staging system are shown in Fig. 2a-c. Although the survival rates for patients with T2 and stage II disease could not be evaluated, T, N and staging classifications were correlated significantly with survival outcomes (P < 0.001, P = 0.003 and P = 0.003, respectively).
Comparisons between the University of Pittsburgh modified TNM staging system and the 8th edition of the AJCC staging manual on TNM staging system
The C-index values based on the University of Pittsburgh modified TNM staging system were 0.774 [95% confidence interval (CI) 0.753–0.794] for T classification, 0.704 (95% CI 0.683–0.724) for N classification and 0.777 (95% CI 0.754–0.799) for staging classification, whereas those based on the 8th edition of the AJCC staging manual on TNM staging system were 0.734 (95% CI 0.713–0.754) for T classification, 0.586 (95% CI 0.561–0.613) for N classification and 0.774 (95% CI 0.752–0.795) for staging classification. Although there were no significant differences in C-index values for T and staging classifications, those for the entire cohort revealed higher prognostic accuracy for the University of Pittsburgh staging system than for the 8th edition of the AJCC staging system.
Predictive factors for outcome
Univariable analysis indicated that T, N and staging classifications based on the University of Pittsburgh modified TNM staging system and the 8th edition of the AJCC staging manual on TNM staging system, surgery, RT and surgical margins (P = 0.002, P = 0.032, P = 0.002, P = 0.014, P = 0.032, P = 0.014, P = 0.008, P = 0.002 and P = 0.010, respectively) were significant prognostic factors for EAC cancer (Table 7). Meanwhile, other clinicopathologic features, such as age, gender, smoking status and alcohol consumption, histopathological differentiation and chemotherapy were not significantly correlated with survival outcome.
Stepwise regression analysis was performed to identify potential confounders among these significant prognostic factors, and multivariable analysis using the Cox proportional hazards model showed that T classification based on the University of Pittsburgh modified TNM staging system was an independent predictor of OS rate (hazard ratio 5.25; 95% CI 1.38–24.9; P = 0.015).
Discussion
The TNM staging system is the most important tool for treatment planning in oncology and for assessing the patient’s prognosis, with a number of classification methods used to date for EAC cancer. Stell and McCormick originally proposed a system classified into 3 stages in 1985 [20]. Arriaga et al. developed a system based on 4 stages at the University of Pittsburgh in 1990 [11], and Moody et al. updated their series in 2000 [2]. Currently, the University of Pittsburgh modified TNM staging system has been accepted for the classification of EAC cancer. This analysis could confirm that T, N and staging classifications based on the University of Pittsburgh modified TNM staging system were correlated significantly with survival outcome in the univariable analysis, which is consistent with previously published literature [8, 10]. The early diagnosis and management of EAC cancer are essential in limiting primary tumor extension and achieving good survival outcomes.
It is noteworthy that T classification based on the University of Pittsburgh modified TNM staging system was demonstrated to be an independent prognostic factor in the multivariable analysis. Unlike most other forms of cancer, the majority of deaths from EAC cancer appear to result from uncontrolled locoregional recurrence rather than from distant organ metastasis [4, 9, 10, 21]. Complete resection of tumors has been reported to achieve good survival outcomes and locoregional control [3,4,5,6,7, 9]. This analysis could also confirm that pathologically margin status was an important prognostic factor for surgical treatment, and the extent of resection must be carefully determined according to T classification. Bone condition in the osseous EAC; i.e., whether it presents as minor erosion or destruction of the full thickness, is a valuable finding for predicting whether surgical treatment can be accomplished at low risk of pathologically positive margins and recurrence [9]. The University of Pittsburgh modified TNM staging system, which distinguishes between T2 and T3 based on the status of bony EAC, is a clinically valuable method for making decision regarding treatment modality for patients with EAC cancer.
The AJCC/UICC TNM classification has been recognized as most well-established malignant tumor staging system worldwide. The external ear, which consists of the “auricle” and the “EAC”, has been included as a specific anatomic location in the 8th edition of the AJCC staging manual on TNM staging system for cutaneous cancer of the head and neck [15]. The AJCC staging system has been widely applied for cancer of the “auricle”. However, it remains unknown whether cancer of the “EAC” can be evaluated using this system. EAC cancers arise from the skin of the auditory canal, whereas the majority of head and neck cancers occur in the mucosa of the nasal cavity, paranasal sinus, oral cavity, pharynx or larynx. Thus, EAC cancers seem to be classifiable, both biologically and histopathologically, as cutaneous cancers. Meanwhile, there is an anatomical difference between the skin of the EAC and other parts of the head and neck including the auricle. The EAC is surrounded by the temporal bone in which major vessels, cranial nerves, and intracranial structures are located [4, 9]. The surgical procedure for EAC cancers has significant morbidity and mortality, resulting in poor prognosis compared with cutaneous cancers at other anatomic sites including the auricle [16, 17].
In this study, the application of the AJCC TNM staging manual for cutaneous cancers of the head and neck resulted in a marked reduction in the distribution of T2 patients. This classification system distinguishes between T1 and T2 by the size of the tumor with 2 cm as the boundary, and T2 and T3 by presence or absence of bone erosion. The length of the canal is approximately 2.5 cm along its posterosuperior aspect and 3.0 cm along its anteroinferiorly aspect, with an average diameter of 0.8 cm [22]. The skin of the osseous EAC is lacking a subcutaneous layer and adnexal structures, such as numerous hair follicles, sebaceous glands and ceruminous glands, and is much thinner than that at other sites, with a thickness of less than 0.2 mm [22]. The thinness of the skin readily allows bone erosion associated with tumor invasion before lesions extend more than 2 cm horizontally in the axial direction of the EAC. Thus, the majority of patients with T2 lesions according to the Pittsburgh classification, for whom a good prognosis can be achieved by complete resection of the tumors with pathologically negative margins, shift to T3 according to the AJCC classification, resulting in some overestimation. Furthermore, both T1 and T2 lesions according to the AJCC classification are confined to the EAC with intact bone, implying that this classification may not be a valuable factor for planning treatment modalities.
The AJCC TNM classification for cutaneous cancers of the head and neck distinguishes between T3 and T4 by presence or absence of gross bone destruction and between T4a and T4b by presence or absence of skull base invasion and/or skull base foramen involvement. As a result, all patients with T3 according to the Pittsburgh classification shifted to T4a according to the AJCC classification, and the majority of patients with T4 according to the Pittsburgh classification were separated into T4a and T4b based on the AJCC classification. Since the selection of treatment modality for advanced-stage EAC cancer has been reported to depend on whether tumors spread beyond the temporal bone [9], the criteria used in the AJCC classification seem to provide useful guidance for treatment and prognosis. However, the prognosis of patients with bone destruction of the fallopian canal has been recognized as poor, even if tumor does not extend past the temporal bone [2, 23]. The AJCC TNM staging system has categorized patients with perineural invasion as T3, leading to concerns that EAC cancers with facial paralysis may be underestimated.
Due to the retrospective nature of this study, the presence of bias caused by loss of subjects to follow-up, the selection criteria for patients and treatment protocols cannot be completely ruled out. In particular, as the treatment modalities for EAC cancers were conducted based on the University of Pittsburg staging system, restaging using the 8th edition of the AJCC staging system could lead to inconsistent treatment results. However, the rarity of EAC cancer makes it difficult to perform well-designed analysis at a single institution. The retrospective chart review is an important method for gathering clinical data on outcomes, aiding clinical decision-making, as well as generating hypotheses. The staging system and survival outcome for patients with EAC cancer should be validated in further trials.
Conclusion
This analysis demonstrated that the University of Pittsburgh modified TNM staging system had better survival discrimination than did the 8th edition of the AJCC staging system, suggesting that the University of Pittsburgh modified TNM staging system is a useful classification method for patients with EAC cancer for determining the extent of disease, providing a basis for decisions on treatment planning, and predicting prognosis. In particular, the criteria for distinguishing between T2 and T3 by the presence of bone erosion or destruction might be a valuable aid in the selection of appropriate treatment and prognostic prediction. Meanwhile, the AJCC staging system did not seem to differentiate T2 from T3–4 cancers, and many patients with EAC cancer might be classified as a more advanced-stage than that based on the University of Pittsburgh staging system. Although the criteria for advanced-stage disease based on the AJCC staging system might provide useful guidance for treatment planning and prognosis, it is necessary to understand that EAC cancer possesses anatomical features distinct from those of other cutaneous cancers of the head and neck, including those of the auricle, and to provide the clinical data for future revisions of the AJCC staging system.
References
Barrs DM (2001) Temporal bone carcinoma. Otolaryngol Clin N Am 34:1197–1218
Moody SA, Hirsch BE, Myers EN (2000) Squamous cell carcinoma of the external auditory canal: an evaluation of a staging system. Am J Otol 21:582–588
Zhang T, Li W, Dai C et al (2013) Evidenced-based surgical management of T1 or T2 temporal bone malignancies. Laryngoscope 123:244–248
Nakagawa T, Kumamoto Y, Natori Y et al (2006) Squamous cell carcinoma of the external auditory canal and middle ear: an operation combined with preoperative chemoradiotherapy and a free surgical margin. Otol Neurotol 27:242–249
Pfreundner L, Schwager K, Willner J et al (1999) Carcinoma of the external auditory canal and middle ear. Int J Radiat Oncol Biol Phys 44:777–788
Gacek RR, Goodman M (1977) Management of malignancy of the temporal bone. Laryngoscope 87(10 Pt 1):1622–1634
Ihler F, Koopmann M, Weiss BG et al (2015) Surgical margins and oncologic results after carcinoma of the external auditory canal. Laryngoscope 125:2107–2112
Takenaka Y, Cho H, Nakahara S et al (2015) Chemoradiation therapy for squamous cell carcinoma of the external auditory canal: a meta-analysis. Head Neck 37:1073–1080
Morita S, Homma A, Nakamaru Y et al (2016) The outcomes of surgery and chemoradiotherapy for temporal bone cancer. Otol Neurotol 37:1174–1182
Yin M, Ishikawa K, Honda K et al (2006) Analysis of 95 cases of squamous cell carcinoma of the external and middle ear. Auris Nasus Larynx 33:251–257
Arriaga M, Curtin H, Takahashi H et al (1990) Staging proposal for external auditory meatus carcinoma based on preoperative clinical examination and computed tomography findings. Ann Otol Rhinol Laryngol 99:714–721
Nyrop M, Grontved A (2002) Cancer of the external auditory canal. Arch Otolaryngol Head Neck Surg 128:834–837
Gillespie MB, Francis HW, Chee N et al (2001) Squamous cell carcinoma of the temporal bone: a radiographic–pathologic correlation. Arch Otolaryngol Head Neck Surg 127:803–807
Higgins TS, Antonio SA (2010) The role of facial palsy in staging squamous cell carcinoma of the temporal bone and external auditory canal: a comparative survival analysis. Otol Neurotol 31:1473–1479
Amin MB, Edge SB, Greene FL et al (2017) AJCC cancer staging manual, 8th edn. Springer, New York
Brantsch KD, Meisner C, Schönfisch B et al (2008) Analysis of risk factors determining prognosis of cutaneous squamous-cell carcinoma: a prospective study. Lancet Oncol 9:713–720
Brougham ND, Dennett ER, Cameron R et al (2012) The incidence of metastasis from cutaneous squamous cell carcinoma and the impact of its risk factors. J Surg Oncol 106:811–815
Hirsch BE (2002) Staging system revision. Arch Otolaryngol Head Neck Surg 128:93–94
Harrell FE Jr, Lee KL, Mark DB (1996) Multivariable prognostic models: issues in developing models, evaluating assumptions and adequacy, and measuring and reducing errors. Stat Med 15:361–387
Stell PM, McCormick MS (1985) Carcinoma of the external auditory meatus and middle ear. Prognostic factors and a suggested staging system. J Laryngol Otol 99:847–850
Schmults CD, Karia PS, Carter JB et al (2013) Factors predictive of recurrence and death from cutaneous squamous cell carcinoma: a 10-year, single-institution cohort study. JAMA Dermatol 149:541–547
Alvord LS, Farmer BL (1997) Anatomy and orientation of the human external ear. J Am Acad Audiol 8:383–390
Ito M, Hatano M, Yoshizaki T (2009) Prognostic factors for squamous cell carcinoma of the temporal bone: extensive bone involvement or extensive soft tissue involvement? Acta Otolaryngol 129:1313–1319
Acknowledgements
We have no financial support to acknowledge.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflicts of interest to declare.
About this article
Cite this article
Morita, S., Mizumachi, T., Nakamaru, Y. et al. Comparison of the University of Pittsburgh staging system and the eighth edition of the American Joint Committee on Cancer TNM classification for the prognostic evaluation of external auditory canal cancer. Int J Clin Oncol 23, 1029–1037 (2018). https://doi.org/10.1007/s10147-018-1314-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10147-018-1314-3