Abstract
Background
Our aim was to evaluate whether it is safe to use a totally implantable venous access device (TIVAD) on the day of implantation.
Methods
We investigated data from 1315 cancer patients divided into two groups according to the time interval between TIVAD placement and the first use of the TIVAD to adminster chemotherapy: patients whose devices were used during the first 24 h after placement were enrolled into group 1 and patients whose devices were first used more than 24 h after device placement were enrolled into group 2.
Results
Early complications were all related to device insertion and occurred before chemotherapy administration. Infection and venous thrombosis were the most frequent complications during the first 6 months after TIVAD insertion in both groups. However, the frequency of late complications was statistically the same for the two groups.
Conclusions
The early use of TIVADs appears safe. Usage of the catheter for chemotherapy administration during the first 24 h after insertion has no effect on the rate of complications.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Safe venous access is an important consideration during the administration of chemotherapy, parenteral nutrition support, and intravenous fluids, and in the transfusion of blood and blood products to cancer patients [1]. The totally implantable venous access device (TIVAD), which is placed subcutaneously, is one of the best approaches to resolving the problems associated with other venous access techniques.
TIVADs are used increasingly in oncology practices to protect patients from the venous toxicities of antineoplastic agents, to prevent complications due to the extravasation of chemotherapeutics, to reduce infection risk, and to allow patients to perform activities of daily living more easily [2]. While there are many advantages of TIVADs, there are also several acute complications associated with the insertion and usage of devices, such as arterial puncture, hemothorax, pneumothorax, and late complications (including infection and thrombosis of the catheter or the vein) [1, 3–6].
Data on the appropriate interval between the implantation of a TIVAD and the first time that it is used are rather scarce in the literature. An interval of at least 24 h between the placement of the TIVAD and the first use of it is usually advised, but an interval of 4 h between placement of the TIVAD and the first use of it has also been reported to be safe [7, 8]. In another study, ensuring an interval of at least 8 days between the insertion of the TIVAD and the first use of it was found to significantly reduce complications [9].
Our aim was to evaluate any possible early and late complications associated with a short (≤24 h) or a long (>24 h) time interval between the insertion of the TIVAD and the first time it is used for administering chemotherapeutic agents to patients. In addition, we tried to identify the optimal time interval before first use for these devices.
Patients and methods
This was an observational nonrandomized study. Prospectively collected data from 1315 consecutive patients whose TIVADs were inserted at the Surgical Oncology Unit of the Istanbul University Institute of Oncology between January 2007 and October 2010 were evaluated retrospectively. All patients who were referred to the authors for TIVAD insertion during the study period were analyzed. The protocol was approved by the Ethics Committee of the Institute of Oncology Istanbul University. All patients were diagnosed with cancer. The age, gender, type of tumor, features of device insertion, time interval between the insertion of TIVAD and the first use of the device, and complications encountered during the first 6 months after device insertion were recorded. Seventy patients who died, 41 patients who were lost to follow-up, and 75 patients for whom the time interval between the insertion of TIVAD and the first use of it could not be established were not included in the analyses.
Study design
Patients were divided into two groups according to the time interval between TIVAD placement and the first use of the device to administer chemotherapy: patients whose devices were used during the first 24 h after device placement were enrolled into group 1 (≤24 h) and patients whose devices were first used more than 24 h after device placement were enrolled into group 2 (>24 h). The aim of the study was to compare these two groups in terms of the characteristics of TIVAD use and observed complications (such as healing problems, infections, thrombosis, and occlusion of the catheter after insertion).
Surgical technique
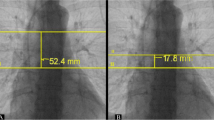
All of the TIVADs were introduced during a daytime, ambulatory setting. A single type of port system (Celsite ST 301, B. Braun, Melsungen, Germany) was used. In the operating room, the patient was placed in a 5–10° Trendelenburg position and the skin of the neck, chest, and shoulders was prepared in the customary sterile manner. Skin was shaved immediately before surgery. Electrocardiogram and heart rate monitoring as well as pulse oximetry were performed. Local anesthesia was given subcutaneously using 15–20 mL of 2 % prilocaine hydrochloride (Citanest, AstraZeneca, Istanbul, Turkey). All TIVADs were inserted via the subclavian vein puncture method. The Seldinger technique was used to access the vein with dilators and peel away sheaths for the insertion. Two incisions were usually necessary: one small incision at the exit site of the wire from the skin, and a second (larger) incision for placing the implantable access device. A subcutaneous tunnel was made to pass the catheter from one incision to the other. Ports were placed in a tight subcutaneous chamber over the right pectoralis fascia, 2 cm under the clavicle, without holding sutures. The implanted port was positioned, tested, and heparinized (5000 IU of heparin sodium in 100 mL of isotonic saline). Surgical wounds were closed with 3/0 interrupted sutures. At the end, a thoracic radiograph was performed to assess early complications, including arterial positioning, catheter malposition, pneumothorax, hemothorax, and arrhythmias. An attempt was made to place the catheter tip in the superior vena cava–right atrium junction to prevent arrhythmias. Patients received 1 g cefazolin by intravenous bolus injection before the incision. Cefazolin was chosen because of its half-life and known activity against Staphylococcus aureus and Staphylococcus epidermidis, the most common agents isolated from infected TIVAD incisions in our previous work [3]. All patients were checked to assess early surgical site complications such as hematoma and surgical wound dehiscence within 24–48 h. TIVADs were flushed either monthly or after every chemotherapy cycle with heparinized saline solution until removal. Patients did not routinely receive oral anticoagulants or heparin to prevent thrombosis.
Definitions
Complications related to the presence of the TIVAD that occurred during the first 6 months after device placement were recorded. The complications were classified as “early” and “late.” Early complications were defined as those which occurred peroperatively during the first 24 h after device placement and were related to device placement. Early complications included arterial puncture, catheter malposition, pneumothorax, hemothorax, port hematoma, and arrhythmia. Late complications were defined as complications that developed more than 24 h and during the first 6 months after device insertion. Port infections, venous thrombosis (Doppler ultrasound diagnosis in symptomatic cases), wound dehiscence, port erosion, catheter occlusion, and malfunctioning (allowing perfusion but not aspiration or total catheter obstruction) are examples of potential late complications. The wound infections were classified as either superficial surgical site infections (SSIs) or deep SSIs according to the 1999 Guideline for Prevention of Surgical Site Infection of the Centers for Disease Control and Prevention [12]. Superficial SSIs were limited to skin and subcutaneous tissue, whereas deep SSIs involved areas deeper than the subcutaneous tissue. Pocket infections were considered deep SSIs. Information about systemic infections and device-related bacteremia was also given.
Statistical analysis
Differences between the categorical data of the two groups were analyzed using chi-squared analysis or Fisher’s exact test as deemed appropriate. Comparisons of median age and median duration of surgery with days from surgery to chemotherapy were analyzed using Student’s t test or the Mann–Whitney U test, as appropriate. A p value of <0.05 was considered statistically significant. Analyses were performed by means of a computerized statistics package (SPSS® v16.0 for Windows®, SPSS Inc., Chicago, IL, USA).
Results
Patient characteristics
Patient characteristics are listed in Table 1. All patients had solid tumors. The median age, duration of surgery, and the frequencies of gender and tumor types were found to be similar in the two groups. The groups also had matching ASA scores, body mass indices, and frequencies of diabetes mellitus and steroid use. The median time to first TIVAD use was the fourth day (range 2–33 days) after insertion in group 2. The most common tumor type in both groups was colorectal cancer (group 1: 56.3 %, group 2: 56.5 %). Features relating to port insertion, including the use of antibiotic prophylaxis, were also statistically similar for the two groups (Table 2). In group 1, 37.9 % of patients were given antibiotic prophylaxis, whereas 35.2 % of patients in group 2 received antibiotic prophylaxis (p = 0.34).
Early complications
The early complications encountered are listed in Table 3. All of the early complications were related to device insertion and occurred before chemotherapy administration. Eight of the 10 (2 patients in group 1, 6 patients in group 2) patients that experienced a pneumothorax were treated with chest tube placement. The pneumothorax improved spontaneously in the other 2 patients. All cases of hemothorax (1 patient in group 1) and hematoma (1 patient in group 1, 2 patients in group 2) resolved without any medical intervention.
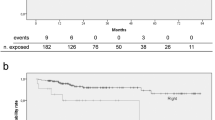
Late complications
The late complications observed in both groups are provided in Table 3. Infection and venous thrombosis were the most frequent complications that developed during the first 6 months after chemotherapy administration via TIVAD in both groups. The frequency of late complications did not differ statistically significantly between the two groups. The infection rate was higher in group 2 than in group 1 (p = 0.08), and the frequency of venous thrombosis was found to be higher in group 1 than in group 2 (p = 0.07), but the differences between the two groups did not reach statistically significant levels. All infections were superficial surgical site infections (SSIs). Only in 2 patients did the SSI progress to a deep SSI. The TIVAD was removed due to signs of systemic infection in one of those patients with a deep SSI. Peripheral cultures and blood cultures were obtained from the patient. No infectious agent was identified via blood cultures. In 8 patients, purulent drainage developed, and samples from those drainages were analyzed for bacterial cultures. The infections were drained. S. aureus was detected in the bacterial culture media of 3 patients and S. epidermidis grew in the culture media from 2 patients. Antibiotic treatment was given according to the results of the culture antibiograms of those 5 patients, whereas 3 patients were treated with empirical antibiotics. Other SSIs that did not show any infectious agent growth in culture media were also treated with empirical antibiotics.
In the 14 patients who developed venous thromboses, low molecular weight heparin was started and the TIVADs were continued with because the devices continued to function properly. In 6 patients, the skin of the surgical site became thinner due to grade 3–4 weight loss, and the TIVAD moved out of the skin [the Common Toxicity Criteria (version 3.0) was used to grade weight loss: grade 3 is a weight loss of >20 % and grade 4 is a life-threatening weight loss but is not specifically defined]. The catheter was removed in 10 patients due to skin dehiscence with TIVAD damage (6 patients), occlusion of the catheter (3 patients), and infection (1 patient). In patients with occlusion of the catheter, injection and aspiration was impossible. Urokinase and/or tissue plasminogen activators were not used in these patients. The catheter tip position was correctly placed in 12 (86 %) patients who experienced venous thromboses. However, in some cases with occluded catheters, the tip was not in the correct place: the catheter tip was located in the internal jugular vein in 2 patients and in the left subclavian vein in 1 patient. The characteristics of the patients who experienced complications were not statistically different from those of who did not experience complications (Table 4). Among the patients who experienced complications, no difference was observed between the patients in whom the TIVAD was used for the first time 2–4 days after insertion and the patients in whom the TIVAD was used for the first time more than 4 days after insertion. The complication rates were 5 % (29 of 538 patients), 6 % (17 of 303 patients), and 5 % (13 of 288 patients) for the patients in whom the TIVAD was first used 0–1 days (≤24 h), 2–4 days, and >4 days after insertion, respectively (p = 0.89).
Discussion
We evaluated whether the early use of a TIVAD for chemotherapy administration was safe or not. We found that, in terms of rates of early and late complications, patients for whom there was a short (≤24 h) time interval between the insertion and the first use of a TIVAD did not statistically significantly differ from patients for whom this interval was longer (>24 h). This finding indicates that the immediate use of a TIVAD route after its insertion is safe.
Port catheters have been a safe and easily performed venous access method and a commonly used way of parenterally administering chemotherapy in oncology practices since they were first developed in 1982 [10, 11]. In the literature, due to their increasing use in cancer patients, there are many reports of studies investigating the effects of port catheters on patient quality of life and possible early or late complications of port catheter use [1, 3–5, 7].
Early initial use of port catheters is preferred for cytotoxic drug administration in some centers, whereas many other centers recommend waiting for a period of time before performing drug infusions via a TIVAD. In fact, the appropriate time interval before the first use of a TIVAD is not clear, and few studies have evaluated whether early use causes more complications or late use prevents early complications [7]. Özdemir et al. [8] studied 180 patients and reported that the early use of a port catheter (1–4 h after insertion) was as safe in terms of early and late complications as late use. On the other hand, Narducci et al. [9] reported that the interval between the insertion and the first use of a TIVAD was the factor that was most strongly predictive of complications. The morbidity rate was found to be 24.4 % when this interval was 0–3 days, 17 % when it was 4–7 days, and 12.1 % when it exceeded 7 days (p < 0.01). They suggested that an interval of at least 8 days between placement of the TIVAD and the first use of the device may be necessary to reduce complications.
The frequencies of hemothorax, pneumothorax, pain, infection, bleeding, great vessel injury, arrythmia, arterial puncture, and thrombosis after port catheter insertion are reported to be 4–35 % depending on the type of complication [12, 13]. Compared to results from previous studies available in the literature, the frequency of complications observed in this study was low (Table 2). The most serious complication, pneumothorax, developed in 4 patients (0.2 %) in group 1 and 6 patients (1 %) in group 2; such rates are similar to those reported previously in the literature [5, 7]. These complications were all related to the TIVAD insertion procedure employed before chemotherapy administration was started. During the 24 h following the placement of each device, no complications occurred. There was no death due to acute complications.
Infection is the most important complication directly related to the presence of a port catheter. The frequency of infection varies from 0.6 to 27 % according to the type of catheter used, the site of catheter insertion, and the performance status of the patients [14]. Our results were not significantly different from those reported in the literature [1, 4, 7]. The infection rates were 1.1 % in group 1 and 2.5 % in group 2. Port-related infections play an important role in the mortality and morbidity of the patients. If the infection cannot be treated with appropriate antibiotics, removal of the port catheter should be considered. In our study, port infections did not result in the death of any of the patients. The port catheter was removed in 1 patient with a deep SSI due to signs of systemic infection. Other patients who experienced infection did not require port removal.
Catheter occlusion may occur as an early or late complication. However, the frequency of port catheter occlusion increases with the duration of port use [15, 16]. Thrombosis is the most important cause of port catheter occlusion [16–18]. Frequent port catheter care, including the infusion of anticoagulants such as heparin solution through catheter lumina, has been suggested as a possible approach to preventing occlusion; however, normal saline has recently been shown to be noninferior to heparin for preventing catheter malfunction problems. In patients with catheter malfunctions, a thrombolytic agent (tPA or urokinase) may be effective [15]. We did not use any thrombolytic agents in patients with catheter occlusion. Oral warfarin or subcutaneous low molecular weight heparin has not been recommended for the prevention of catheter occlusion in routine practice, and is only useful for preventing venous thrombosis. Catheter disconnection and catheter rupture are two other potential complications related to the use of catheters, but these were not observed in either of our patient groups.
In conclusion, the use of port catheters is an important method of obtaining safe venous access in cancer patients. The duration between the insertion and the first use of the catheter for chemotherapy administration has no effect on the rate of complications.
References
Vescia S, Baumgärtner AK, Jacobs VR et al (2008) Management of venous port systems in oncology: a review of current evidence. Ann Oncol 19:9–15
Di Carlo I, Pulvirenti E, Mannino M (2010) Increased use of percutaneous technique for totally implantable venous access devices. Is it real progress? A 27-year comprehensive review on early complications. Ann Surg Oncol 17:1649–1656
Karanlik H, Kurul S (2009) Modification of approach for totally implantable venous access device decreases rate of complications. J Surg Oncol 100:279–283
Teichgräber UK, Gebauer B, Benter T et al (2004) Long-term central venous lines and their complications. RöFo: Fortschritte auf dem Gebiete der Röntgenstrahlen und der. Nuklearmedizin 176:944
Yildizeli B, Lacin T, Batirel HF et al (2004) Complications and management of long-term central venous access catheters and ports. J Vasc Access 5:174–178
Dal Molin A, Rasero L, Guerretta L et al (2011) The late complications of totally implantable central venous access ports: the results from an Italian multicenter prospective observation study. Eur J Oncol Nurs 15:377–381
Biffi R, De Braud F, Orsi F et al (1998) Totally implantable central venous access ports for long-term chemotherapy. A prospective study analyzing complications and costs of 333 devices with a minimum follow-up of 180 days. Ann Oncol 9:767–773
Özdemir NY, Abalı H, Öksüzoğlu B et al (2009) It appears to be safe to start chemotherapy on the day of implantation through subcutaneous venous port catheters in inpatient setting. Support Care Cancer 17:399–403
Narducci F, Jean-Laurent M, Boulanger L et al (2011) Totally implantable venous access port systems and risk factors for complications: a one-year prospective study in a cancer centre. Eur J Surg Oncol 37:913–918
Biffi R, De Braud F, Orsi F et al (2001) A randomized, prospective trial of central venous ports connected to standard open-ended or Groshong catheters in adult oncology patients. Cancer 92:1204–1212
Torramade JR, Cienfuegos JA, Hernandez JL et al (1993) The complications of central venous access systems: a study of 218 patients. Eur J Surg 159:323–327
Mangram AJ, Horan TC, Pearson ML et al (1999) Guideline for prevention of surgical site infection. Am J Infect Control 27:97–134
Vardy J, Engelhardt K, Cox K et al (2004) Long-term outcome of radiological-guided insertion of implanted central venous access port devices (CVAPD) for the delivery of chemotherapy in cancer patients: institutional experience and review of the literature. Br J Cancer 91:1045–1049
Niederhuber JE, Ensminger W, Gyves JW et al (1982) Totally implanted venous and arterial access system to replace external catheters in cancer treatment. Surgery 92:706–712
Odabas H, Ozdemir NY, Ziraman I et al (2014) Effect of port-care frequency on venous port catheter-related complications in cancer patients. Int J Clin Oncol 19:761–766
Karanlik H, Kurul S, Saip P et al (2011) The role of antibiotic prophylaxis in totally implantable venous access device placement: results of a single-center prospective randomized trial. Am J Surg 202:10–15
Caers J, Fontaine C, Vinh-Hung V et al (2005) Catheter tip position as a risk factor for thrombosis associated with the use of subcutaneous infusion ports. Support Care Cancer 13:325–331
Jordan K, Behlendorf T, Surov A et al (2008) Venous access ports: frequency and management of complications in oncology patients. Onkologie 31:404–410
Conflict of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
About this article
Cite this article
Karanlik, H., Odabas, H., Yildirim, I. et al. Is there any effect of first-day usage of a totally implantable venous access device on complications?. Int J Clin Oncol 20, 1057–1062 (2015). https://doi.org/10.1007/s10147-015-0830-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10147-015-0830-7