Abstract
When early lateral spread response (LSR) loss before decompression in HFS surgery happens, the value of intraoperative monitoring of LSR for locating neurovascular conflicts and confirming adequate decompression was considered to be reduced. This study aimed to identify preoperative parameters predicting early LSR loss and figure out the impact of early LSR loss on prognosis. Hemifacial spasm (HFS) patients who received microvascular decompression (MVD) under intraoperative electrophysiological monitoring during the period of March 2013–January 2021 were reviewed retrospectively. The patients were divided into two groups according to the disappearance of their LSR before or after decompression. Preoperative clinical and radiological predictors for early LSR loss were evaluated using logistic regression. The relationship between early LSR loss and surgical outcomes was statistically analyzed. A total of 523 patients were included in the study, and the disappearance of their LSR before decompression occurred in 129 patients. In the multivariate analysis, three independent factors predicting early LSR loss were identified: (1) smaller vessel compression; (2) milder nerve deviation; (3) lower posterior fossa crowdedness index (PFCI, calculated as hindbrain volume (HBV)/the posterior fossa volume (PFV) using 3D Slicer software). The median follow-up time was about five years, and no significant differences in the spasm relief and complication rates were found between the 2 groups. Smaller responsible vessels, milder nerve deviation, and more spacious posterior cranial fossa are associated with early LSR loss. However, early LSR loss seems to have no significant adverse effect on MVD outcomes in skilled hands.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Hemifacial spasm (HFS) is a neurological disorder typically characterized by the chronic, paroxysmal, and involuntary twitching of the muscles innervated by the ipsilateral seventh cranial nerve [1]. Microvascular decompression (MVD) has been widely accepted as the gold-standard surgical procedure for HFS based on its etiology. This treatment provides relief from spasms in over 90% of HFS patients [2]. Lateral spread responses (LSR), a typical electrophysiological feature of HFS, can be monitored during surgery [3]. Specifically, LSR is attributed to the electrical transmission of impulses between the different facial nerve branches [4]. Ideally, LSR will be lost immediately, when responsible vessels are separated from the root exit zone (REZ) of the facial nerve. However, early LSR loss prior to decompression in HFS surgery often occurs and still cannot be prevented.
Routinely, intraoperative electrophysiological monitoring is adopted to optimize surgical outcomes of HFS surgery. When early LSR loss occurs, surgeons will face the challenge of having to depend on their experience to complete the operation without electrophysiological guidance. To date, few studies have focused on this phenomenon and its clinical implications. Therefore, the goals of this study were to explore the causes of early LSR loss in HFS surgery and evaluate the clinical outcomes of early LSR loss versus LSR loss after decompression.
Materials and methods
Patient populations
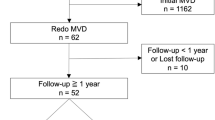
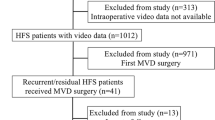
Between March 2013 and January 2021, 523 patients underwent MVD for primary HFS in the Department of Neurosurgery at Wuhan Union Hospital and Zhongnan Hospital of Wuhan University. All procedures were performed by a single neurosurgeon (Professor Xiong). He initially learned MVD from the China-Japan Friendship Hospital with a huge volume of MVD operations in China. Before this study period, he has performed nearly 300 MVD operations and is very proficient in this procedure. The primary HFS was diagnosed according to its typical clinical manifestations and neuroimaging findings. The inclusion criteria were typical HFS symptoms, LSR loss before or after decompression, and a minimum of 2 years of follow-up. The exclusion criteria were as follows: (1) incomplete clinical data; (2) LSR absence during the whole monitoring; (3) maintenance of LSR after decompression; (4) other hyperkinetic facial movement disorders such as tics or dystonia; (5) secondary HFS due to tumors, cyst, and Chiari malformation, etc.; (6) Botulinum toxin injection treatment within one year before MVD; (4) a history of craniotomy or gamma-knife surgery.
Imaging evaluation
All subjects were examined by a 3T MRI scanner (Magnetom Trio; Siemens AG, Erlangen, Germany) with a standard head coil prior to MVD. High-resolution MRI was performed with three-dimensional sampling perfection with application-optimized contrasts using different flip angle evolutions (SPACE) sequence. The parameters used for SPACE imaging were as follows: repetition time, 1000 ms; echo time, 135 ms; flip angle, 120°; number of excitations, 2; matrix, 384 × 384; field of vision, 20.0 × 20.0 cm; and slices of 0.5 mm without gap. The study was approved by the institutional ethics review board (No.2020-S897), and the need for written informed consent was waived given its retrospective design.
When recognizing the vascular contacts with the facial nerve, we recorded the responsible vessels and the nerve segments contacted. The responsible vessels were classified into three types according to size: (1) large vessels: vertebrobasilar artery; (2) medium vessels: the main trunk of the anterior inferior cerebellar artery (AICA), posterior inferior cerebellar artery (PICA), and AICA PICA common trunk (APC); (3) small vessels: branches of AICA, PICA or APC. According to the anatomic marks visualized by MRI, the nerve segments contacted are classed into “brain stem,” “root entry/exit zone (REZ)” or “cisternal portion (CP).” The brain stem region is defined as the nerve segments from emerging from the brain stem within the pontomedullary sulcus to separating from the pons at the root detachment point (RDP). The REZ is the segment from the RDP to 4 mm distal to the whole transition zone (TZ) where the central glial myelin is transformed into peripheral Schwann cell myelin. The cisternal portion (CP) is known as the segment from the TZ to the porus acoustics. The severity of neurovascular compression was graded into three groups: (1) mild: neurovascular contact without facial nerve indentation; (2) moderate: facial nerve indentation without deviation from its route; (3) severe: facial nerve deviation [5].
The boundaries of the posterior fossa were from the clivus to the occipital bone and from the foramen magnum occipitalis to the tentorium cerebelli. The pons, the cerebellum, and the medulla oblongata contained in the posterior fossa, including the fourth ventricle, were defined as the hindbrain brain. Measurements were sampled on 40 slices with a total range of 20 mm, and the midpoint of the volume slab was centered over the pontomedullary sulcus. The 3D-Slicer software (3.6.3 version; www.slicer.org.) was used to measure the posterior fossa volume (PFV) and hindbrain volume (HBV). Figure 1 is an example of axial, sagittal, and coronal slices through the measurement area. Measurements were calculated twice with a four-week interval and then averaged. All works were performed by an experienced radiologist blinded to the clinical information. The posterior fossa crowdedness index (PFCI) is calculated as the ratio of HBV to PFV.
The segmented posterior fossa CSF space is represented by yellow areas in the axial (A), sagittal (B), and coronal (C) slices. Measurements were performed on 40 slices with a total range of 20 mm (from the superior line to the inferior line, with the middle line centered over the pontomedullary sulcus, C)
Surgery
All surgeries were performed via a suboccipital retrosigmoid approach in the lateral decubitus position. With cerebrospinal fluid drainage and arachnoid dissection, neurovascular conflicts at the facial nerve root were checked via the operating microscope. The possible offending vessels were satisfactorily decompressed by padding Teflon felts. After confirming no further compressions, the dura and incision were closed.
Intraoperative monitoring
During surgery, facial electromyogram and brainstem auditory evoked potentials were monitored continuously through needle electrodes inserted in the orbicularis oris, orbicularis oculi, and mentalis muscles. A 300-μsec pulse wave with a stimulation intensity of 5–30 mA was used. The LSRs appeared in the mentalis and orbicularis oris muscles when we stimulated the zygomatic branch and in the orbicularis oculi and frontalis muscles during the buccal branch stimulation. We made 9 checks to detect when the LSR disappeared: (1) after anesthesia, (2) before dural opening, (3) immediately after dural opening, (4) at cerebrospinal fluid (CSF) drainage, (5) before decompression, (6) during dissection, (7) after decompression, (8) before dural closure, and (9) after dural closure. The patients were divided into 2 groups based on whether the LSR disappeared before (1–6) or after (7–9) decompression.
Outcome evaluation
Follow-up information is collected through clinic visits or phone interviews at various intervals. If the patient remains free of HFS symptoms, the time to the next follow-up will increase. The spasm severity was quantified using the Cohen evaluation scale, namely 0, no spasm; 1, increased blink or slight facial muscle tremor due to external stimulation; 2, slight spontaneous facial muscles vibrate without dysfunction. 3: obvious facial spasm with slight dysfunction; 4: severe facial spasm and dysfunction (unable to read, drive, etc.). If patients had no facial spasm (Cohen score = 0), they were defined as cured. All remaining patients were defined as having HFS remaining.
Statistical analysis
Groups were compared using Chi-square and Fisher’s exact test for categorical variables. The continuous variables distribution was checked using the Shapiro–Wilk test. Student’s t-test was used to evaluate variables that follows a normal distribution, for others the Mann–Whitney U test was performed. Univariate logistic regression analysis was used to identify the factors correlated with an early LSR loss. Factors associated with a p-value < 0.20 in the univariate analysis were considered for further analysis and introduced in a multivariate logistic model using a stepwise procedure, calculating the odds ratio (OR). A Cohen’s kappa coefficient for the severity of the facial nerve compression is calculated to determine the strength of agreement between the operative and imaging findings. All tests were performed using SPSS version 23(IBM Corp., Armonk, New York, USA). A two-sided 5% level was considered statistically significant.
Results
Demographic characteristics
A total of 523 patients were included in the study. Patients’ characteristics are presented in Table 1. Our population represents the actual population of HFS patients, with the left-side symptoms slightly accounting for the majority (58%). The mean age was 51 0.5 years, and the most common spasm severity was the Cohen evaluation scale 3. The patients with severe compression or distortion of the trigeminal nerve detected with imaging account for 14.3% of the total patients, the kappa coefficient of agreement for the severity of the facial nerve compression was 0.64, indicating fair to good agreement between the operative and imaging findings. The 523 patients were divided into A group (LSR loss before decompression, n = 129) and B group (LSR loss after decompression, n = 394).
Early LSR loss
Table 1 shows the proportion of early LSR loss related to different variable categories. In the univariate analysis, we found 6 variables related to early LSR loss of a 0.2-significance level: Mean duration of symptom, Cohen score, Predominant offending vessel, Severity of nerve deviation, No. of compression sites, PFCI.
These 6 factors were entered into a multivariate analysis (logistic model). At the end of the stepwise selection process, the following 3 factors were retained in the final model: medium vessels (OR 2.29, 95% CI 1.36–4.17) or small vessels (OR 5.36, 95% CI 2.93–11.65) vs large vessels, moderate neurovascular compression (OR 0.59, 95% CI 0.34–0.96) or severe neurovascular compression (OR 0.41, 95% CI 0.22–0.83) vs mild neurovascular compression, and PFCI (OR 3.13, 95% CI 1.23–6.45) (Table 2).
Correlation between MVD results and early LSR loss
In the 1-week examination following MVD, complete spasm relief rates in groups A and B were 86.0% (n = 111) and 89.6% (n = 353), respectively (Table 2). The latest follow-up examination showed HFS-free in 120 patients (93.0%) in group A and 375 (95.2%) patients in group B. There were no statistically significant differences in the surgical efficacy at one week after MVD (p = 0.27) and the long-term follow-up (p = 0.35) (Table 3).
Among all the patients, the major complications were hearing impairment in 13 patients (0.2%), delayed facial paralysis in 15 patients (0.3%), hoarseness in 8 patients (0.2%), tinnitus in 4 patients (0.1%), diplopia in 6 patients (0.1%), dizziness/vertigo in 13 patients (0.2%), and cerebellar hematoma in 4 patients (0.1%). No deaths occurred in either group. Notably, except for the two patients with hearing impairment and one patient with diplopia, all patients have gradually recovered from complications. There were no significant differences in the postoperative complications between the A and B groups (Table 4).
Discussion
At present, MVD is considered to be the most effective treatment for HFS. However, its cure and complication rates in HFS patients differ broadly in the published literature and may be due to some neglected responsible vessels [6]. Therefore, intraoperative identifying the specifically responsible vessels and decompressing adequately is vital.
Some scholars believe that LSR may be the result of pulse compression at the facial nerve root [7], while others believe that LSR may be associated with the cross-transmission of the reverse activity in the facial nucleus [4]. Recently, Møller et al. suggested that LSR were caused by facial motor nucleus hyperactivity [8]. Although the mechanism of the LSR is still not fully understood, intraoperative LSR monitoring serves as a tool to guide responsible vessel identification.
The incidence of early LSR loss reported in various studies ranged from 6.8% to 34% [9]. When early LSR loss occurs, the guiding value of intraoperative LSR monitoring is impaired. Looking at this from another perspective, Mooij et al. deemed that early LSR loss without reappearance was an indirect confirmation for sufficient decompression [10]. To date, few studies have focused on the mechanism underlying early LSR [11,12,13]. This study is the first to investigate independent predictors of early LSR loss using multivariate analysis.
A possible mechanism of early LSR loss is that the compression force exerted by the responsible vessels is relatively small. The neurovascular relationships are easily affected by subtle environmental changes, such as cerebrospinal fluid drainage, arachnoid membrane dissection, and cerebellar retraction. This can explain the differential compositions regarding responsible vessels between both groups in our study. The vertebrobasilar arteries are usually large and rigid, and they can even be deeply embedded in the brainstem tissue. Compared with some smaller responsible vessels, decompression involving the vertebrobasilar arteries is more challenging due to their stability. Those environmental changes before decompression are unlikely to cause enough anatomical shifts of the vertebrobasilar arteries around the facial nerve root and achieve the effect of decompression in advance. The converse is equally true: when small branches of AICA or PICA act as responsible vessels, more opportunities for early decompression result in more occurrences of early LSR loss.
Nerve deviation severity was also found to be associated with the occurrences of early LSR loss in our study, and slight neurovascular compression was a predictive factor. This was consistent with the results of previous studies. Jiang et al. reported that the neurovascular compression degree was not serious without indentation in patients with early LSR loss [11]. Looking at it another way, severe neurovascular compression and consequent nerve indentation and displacement also reflect the stronger compression force exerted by the responsible vessels.
In our study, we evaluated the posterior fossa crowdedness through the ratio of HBV and PFV to avoid the impact of individual differences among participants, as these differences could reduce the observable effect of proposed measurement tools, or cause them to have no observable effect at all. The PFCI accurately reflects the effective posterior cranial fossa CSF space, where neurovascular compression occurs. Posterior fossa overcrowding can bring about a closer neurovascular relationship, which increases the structural stability of neurovascular compression before decompression, and thus leading to a lower incidence of early LSR loss.
Kim et al. demonstrated that an early LSR loss was correlated with worse outcomes [14]. Considering the decompression guiding meaning of intraoperative LSR monitoring, this finding seems reasonable. Interestingly, in our study, no statistically significant difference was found in the postoperative and long-term cure rates between the 2 groups. Here we tried to explain the conflicting findings. Under these circumstances of the early LSR loss, the operator’s experience is important to perform adequate decompression. For surgeons who are in the rising period of the learning curve of MVD, intraoperative neuromonitoring helps identify the offending vessels and confirm facial nerve decompression after padding Teflon felts. Therefore, an early LSR loss may bring adverse effects. However, as surgeons gained more and more experience, all forms of possible neurovascular compression and their corresponding handling methods become familiar, when the learning curve reached a flat period. Even the guiding significance of intraoperative LSR monitoring was deliberately weakened. When the intraoperative decompression and electrophysiological cues were inconsistent, the skilled operator may trust his own experience more and decide whether to finish the operation. It should be emphasized that all the operations in our study were performed by the same surgeon who had rich experience previously. In most cases, the offending vessels can be determined only by experience. When offending vessels is uncertain, the REZ was checked thoroughly, and all possible responsible vessels were separated from the facial nerve root. The increased operations to deal with all possible responsible vessels are gentle in skilled hands, which is unlikely to result in more postoperative complications. This may be the reason for the lack of difference in surgical results between the 2 groups.
Although our study is the first to determine independent predictors of early LSR loss using multivariate analysis. It has several limitations. First, this study was retrospectively performed and limited the available data. Second, all surgeries were performed by a skilled surgical team at a single center, which may be contributed to the lack of difference in clinical results between the two groups. To reduce the bias and demonstrate the clinical significance of early LSR loss more clearly, future studies should use data collected from our surgical team at different time periods or other surgical teams with different professional levels, using unique LSR monitoring protocols. Third, because a study group with persistent LSR after decompression was not enrolled, a direct comparison of the outcomes between LSR persistence and LSR loss after decompression was not possible. However, the primary objective was to determine preoperative parameters predicting early LSR loss and the present study we designed addressed this objective.
Conclusion
Our present results show that patients with early LSR loss have smaller responsible vessels, slighter nerve deviation severity, and less crowded posterior fossa. These factors reflect the unstable neurovascular anatomical relationships, which are easily influenced by subtle environmental changes before decompression, such as cerebrospinal fluid drainage, arachnoid membrane dissection, and cerebellar retraction. Although intraoperative LSR monitoring has guiding implications for HFS, MVD with early LSR loss does not show less efficacy than MVD without early LSR loss when the operation is performed by a skilled and experienced surgeon.
Data availability
The data used to support the findings of this study are available from the corresponding author upon request.
References
Rosenstengel C, Matthes M, Baldauf J et al (2012) Hemifacial spasm: conservative and surgical treatment options. Dtsch Arztebl Int 109:667–673
Hughes MA, Branstetter BF, Taylor CT et al (2015) MRI findings in patients with a history of failed prior microvascular decompression for hemifacial spasm: how to image and where to look. AJNR Am J Neuroradiol 36:768–773
Nielsen VK (1984) Pathophysiology of hemifacial spasm: II. Lateral spread of the supraorbital nerve reflex. Neurology 34:427–431
Kameyama S, Masuda H, Shirozu H et al (2016) Ephaptic transmission is the origin of the abnormal muscle response seen in hemifacial spasm. Clin Neurophysiol 127:2240–2245
Campos-Benitez M, Kaufmann AM (2008) Neurovascular compression findings in hemifacial spasm. J Neurosurg 109:416–420
Xia YF, Zhou WP, Zhang Y et al (2022) How to improve the effect of microvascular decompression for hemifacial spasm: a retrospective study of 32 cases with unsuccessful first time MVD. J Neurol Surg A Cent Eur Neurosurg 83:338–343
Kim P, Fukushima T (1984) Observations on synkinesis in patients with hemifacial spasm. Effect of microvascular decompression and etiological considerations. J Neurosurg 60:821–827
Moller AR (1987) Hemifacial spasm: ephaptic transmission or hyperexcitability of the facial motor nucleus? Exp Neurol 98:110–119
Chan RW, Chiang YH, Chen YY et al (2021) Predicting early loss of lateral spread response before decompression in hemifacial spasm surgery. Life (Basel) 12:40
Mooij JJ, Mustafa MK, van Weerden TW (2001) Hemifacial spasm: intraoperative electromyographic monitoring as a guide for microvascular decompression. Neurosurgery 49:1365–1370 (discussion 1370-1361)
Jiang C, Xu W, Dai Y et al (2017) Early permanent disappearance of abnormal muscle response during microvascular decompression for hemifacial spasm: a retrospective clinical study. Neurosurg Rev 40:479–484
Haines SJ, Torres F (1991) Intraoperative monitoring of the facial nerve during decompressive surgery for hemifacial spasm. J Neurosurg 74:254–257
Hirono S, Yamakami I, Sato M et al (2014) Continuous intraoperative monitoring of abnormal muscle response in microvascular decompression for hemifacial spasm; a real-time navigator for complete relief. Neurosurg Rev 37:311–319 (discussion 319-320)
Kim CH, Kong DS, Lee JA et al (2010) The potential value of the disappearance of the lateral spread response during microvascular decompression for predicting the clinical outcome of hemifacial spasms: a prospective study. Neurosurgery 67:1581–1588
Funding
Scientific Research Fund of Wuhan Health Commission, Grant ID: WX21D68.
Author information
Authors and Affiliations
Contributions
(I) Conception and design: Songshan Chai, Ji Wu; (II) Administrative support: Jiabin Zhou, Nanxiang Xiong; (III) Provision of study materials or patients: Yuankun Cai, Jingwei Zhao; (IV) Collection and assembly of data: Zhimin Mei, Yixuan Zhou, Yihao Wang; (V) Data analysis and interpretation: Hao Xu, Jiabin Zhou; (VI) Manuscript writing: Songshan Chai, Ji Wu; (VII) Final approval of manuscript: All authors.
Corresponding authors
Ethics declarations
Ethics approval
The study received full approval from the ethics committee of Tongji Medical College, Huazhong University of Science and Technology and informed consent was waived due to the retrospective nature of the study.
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Chai, S., Wu, J., Cai, Y. et al. Early lateral spread response loss during microvascular decompression for hemifacial spasm: its preoperative predictive factors and impact on surgical outcomes. Neurosurg Rev 46, 174 (2023). https://doi.org/10.1007/s10143-023-02083-4
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1007/s10143-023-02083-4