Abstract
Whether surgical revascularization can prevent recurrent hemorrhage in hemorrhagic moyamoya disease (HMD) patients remains a matter of debate. This study mainly aims at the comparison of treatment effect between surgical revascularization and conservative treatment of adult HMD patients. We retrospectively enrolled 322 adult HMD patients, including 133 in revascularization group and 189 in conservative group. The revascularization group included patients who underwent combined (n = 97) or indirect revascularization alone (n = 36). Ninety-two and forty-one patients underwent unilateral and bilateral revascularization respectively. The modified Rankin scale (mRS) was used to assess the functional status. The comparison was made based on initial treatment paradigm among two categories: (1) revascularization vs. conservative, (2) unilateral vs. bilateral revascularization. The rebleeding rate was significantly lower in revascularization group than that in conservative group (14.3% vs. 27.0%, P = 0.007). As for the functional outcomes, the average mRS was significantly better in revascularization group (1.7 ± 1.5) than that in conservative group (2.8 ± 1.9) (P < 0.001). The death rate in revascularization group was 8.3% (11/133), comparing to 20.1% (38/189) in conservative group (P = 0.004). While comparing between unilateral and bilateral revascularization within the revascularization group, the result demonstrated lower annual rebleeding rate in bilateral group (0.5%/side-year) than that in unilateral group (3.3%/side-year) (P = 0.001). This study proved the better treatment efficacy of surgical revascularization than that of conservative treatment in HMD patients, regarding both in rebleeding rate and mortality rate. Furthermore, bilateral revascularization seems more effective in preventing rebleeding than unilateral revascularization.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Moyamoya disease (MMD) is a unique cerebrovascular disease characterized by the progressive occlusion of the distal internal carotid artery (ICA), proximal middle and anterior cerebral arteries (MCA and ACA), with the resulting hazy network of basal collaterals [25]. Ischemic and hemorrhagic symptoms are the most common in children and adults with MMD, respectively [11]. Cerebral ischemia and transient ischemic attack are common in North American and European patients. In contrast, Asian patients are more likely to suffer intracranial hemorrhage as the initial symptom [10, 14]. In fact, rebleeding is the leading cause of death in hemorrhagic moyamoya disease (HMD), the frequency of rebleeding ranges between 16 and 66%, and the mortality caused by intracranial hemorrhage in HMD patients ranges between 6.8 and 28.6%, as reported in previous studies [6, 18, 28, 30]. At present, the surgical revascularization is the main treatment for MMD, but the presence of the regional racial difference and the paucity of long-term follow-up studies in HMD, the pathogenesis associated with rebleeding in HMD patients, and the efficacy of surgical revascularization procedure are still on debate [6, 18, 28, 30]. Recent studies have shown that surgical revascularization can resolve hemodynamic impairment and reduce the risk of subsequent hemorrhagic stroke [1, 5, 18, 30]. In a cohort of MMD patients containing both ischemic and hemorrhagic types, Taichi et al. showed that double revascularization may not prevent rebleeding in HMD patients, but can only prevent further ischemic attacks in ischemic MMD patients [6]. However, some scholars believed that the effect of revascularization for preventing rebleeding in MMD is much greater than that for preventing ischemia [7]. Furthermore, there is no evidence of the effect of surgical revascularization on the prevention of contralateral rebleeding, and whether bilateral revascularization is necessary in HMD patients [15]. According to these doubts, the comparison was made based on initial treatment paradigm among two categories: (1) revascularization vs. conservative, (2) unilateral vs. bilateral revascularization. So, we focused on investigating the clinical features of adult HMD, and comparing between revascularization group and conservative groups and between unilateral and bilateral revascularization within the revascularization group, further guiding the treatment strategy for reducing the rebleeding in HMD.
Materials and methods
Study population and radiological characteristics
We reviewed 322 nonselective and consecutive adult HMD patients admitted to our hospital from May 2015 to June 2019. The inclusion criteria were as follows: (1) All patients initially presented with intracranial hemorrhage, which was confirmed by brain computed tomographic (CT) scan. (2) The diagnosis of MMD was based on digital subtraction angiography (DSA) or computerized tomographic angiography (CTA). (3) Aged ≥ 18 years. Patients with ischemic symptoms as the initial presentation, pseudo-MMD, and moyamoya syndrome caused by other systemic diseases (such as neurofibromatosis, sickle cell disease, history of irradiation, or hyperthyroidism) were excluded. The patterns of hemorrhage included intraparenchymal hemorrhage (IPH), intraventricular hemorrhage (IVH), IPH with IVH, and subarachnoid hemorrhage (SAH). The side of hemorrhage was categorized into left, right, and bilateral. SAH was categorized into bilateral group. The modified Rankin scale (mRS; 0–6, the score of 6 was defined as death) was used to assess clinical status at presentation and functional outcomes.
Data collection
Clinical characteristics data of the HMD patients at admission was collected, including age, sex, initial clinical manifestations, and the mRS of bleeding. We also collected data of risk factors including hypertension (systolic blood pressure > 140 mmHg or diastolic blood pressure > 90 mmHg, or use of antihypertensive medication), smoking, alcohol use, and aneurysms.
Therapy and surgical technique
Treatment modalities included surgical revascularization and conservative management. Surgical treatments for MMD were usually divided into three categories: direct, indirect, and combined revascularization [29]. Direct revascularization used a microsurgical end-to-side anastomosis of superficial temporal artery (STA) to identical cortical branches of the middle cerebral artery (MCA), that is, the so-called STA-MCA revascularization. Indirect revascularization involved the placement of vascularized tissue supplied by the external carotid artery (such as dura or temporalis muscle) in direct contact with the brain, leading to the ingrowth of new blood vessels to the underlying cerebral cortex. We mainly perform the following two types of surgery: (1) The adopted method of indirect revascularization in this study was encephalo-dura-myo-synangiosis (EDMS), which has been widely performed in other medical centers [8]. (2) Combined revascularization was a combination of STA-MCA bypass and EDMS. Postoperative DSA or CTA were used to evaluate the patency of STA-MCA anastomosis.
The surgical strategies were mainly as follows. First, surgical revascularization was not performed in the acute phase of intracranial bleeding. Second, the bleeding hemisphere was the preferred side for revascularization. Third, bilateral revascularization was recommended for the HMD patients with bilateral abnormal collaterals or bilateral presentation, even though there was no intracranial hemorrhage in the contralateral hemisphere. Fourth, combined revascularization was the preferred procedures. Indirect revascularization was applied when the donor or recipient artery was too small or fragile to perform with STA-MCA bypass.
Conservative treatment included ventricular drainages or only hematoma evacuations without EDMS, in the acute phase, and ventriculoperitoneal shunt in the chronic phase following hemorrhage, The conservative strategy was jointly determined by surgeons and patients’ family members.
Follow-up and end points
Cross-sectional follow-up data was consisted of the management condition of risk factors for stroke, survival condition, recurrent bleeding events, and mRS evaluated by two experienced neurosurgeons. In addition to the follow-up in out-patient department, all patients were contacted via telephone to update their clinical and performance status on time. All revascularization patients were required to undergo DSA 6 months postoperatively. Poor functional outcome referred to mRS ≥ 3.0.
The primary endpoint was rebleeding. The secondary endpoint was death resulted from HMD, including lethal hemorrhagic stroke, cerebral infarction, and other fatal events. When performing survival analysis, two conditions were defined as censoring events. First, patients were alive at the end of the follow-up period but lost to follow-up. Second, patient died from other disease.
Statistical analysis
Statistical analysis was carried out by using SPSS (Windows version 25.0, IBM). The categorical variables were presented as counts (with percentages). The continuous variables were presented as the means ± standard deviations (SD). The average annual rebleeding rate was calculated by dividing the number of recurrent hemorrhage events from the initial episode by patient years. All data were subjected to Kolmogorov–Smirnov test to determine compliance with normal distribution. The chi-square test or Fisher exact test was used to analyze categorical variables. The continuous variables were analyzed using a t-test or nonparametric test. The cumulative risk of rebleeding and survival curves was estimated by the Kaplan–Meier product-limit method. Moreover, determining whether Kaplan–Meier transition curves differed among subgroups by log-rank test.
Result
Clinical characteristics
Baseline presentation and characteristics of the patient cohort are presented in Table 1 and Table 2 among two categories: (1) revascularization vs. conservative, (2) unilateral vs. bilateral revascularization within revascularization group. Table 3 and Table 4 summarize the long-term rebleeding rates according to the above groups. A consecutive series of 606 patients with bilateral or unilateral MMD was diagnosed, and 335 patients (55.3%) presented with intracranial bleeding. The 4 pediatric HMD patients were excluded and 9 patients were lost of contact during follow-up. Finally, 322 patients were enrolled in this study (Fig. 1). Of the 322 HMD patients, 187 were women and 135 were men (F/M ratio, 1.385:1). The average age was 48.2 ± 10.9 years at the first bleeding. The most common initial symptom was sudden headache (62.7%), vomiting (49.6%), and unconsciousness (35.9%). The typical CT images are shown in Fig. 2, including IPH, IVH, IPH with IVH, and SAH. In our results, IVH and IPH were the most frequent presentations, accounting for 32.0% and 25.2%, respectively. Notably, 15 cases in revascularization group suffered from intracranial bleeding two times before surgical revascularization was adopted. According to Suzuki’s classification, the stages III and IV were the most common types in the DSA of HMD patients, accounting for 62.7% of 102 HMD patients. As for accompanying diseases, 14.6% of patients had aneurysm, and 32.9% had hypertension.
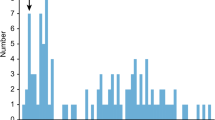
Eighty-five of 322 patients (26.4%) which included 35 men and 50 women experienced rebleeding attacks following initial hemorrhagic attack during a median follow-up period of 42 months (range 0.10–240.0). Same as the first bleeding, IVH (35.3%) was also the most common recurrent hemorrhagic type, followed by IPH (29.4%). Interestingly, with average follow-up period of 86.7 months, there was a decreasing trend in the number of rebleeding events after the first hemorrhage, the highest number of patients suffered rebleeding after the first hemorrhage within 2 years (38 patients, 44.7%), followed by in 7 to 9 years (13 patients, 15.3%), in 2 to 4 years (12 patients, 14.1%), and only 9 rebleeding episodes (10.6%) in 12 to 18 years (Fig. 3).
Revascularization vs. conservative treatment
In this study, 133 patients underwent surgical revascularization, and 189 patients underwent conservative treatment. In the revascularization group, 97 patients underwent combined revascularization, and 36 patients who’s the donor or recipient artery was too small or fragile that were only treated with EDMS. To verify that the follow-up time of the revascularization group was sufficient, we compared the follow-up time of rebleeding in conservative group (52.3 months) and no rebleeding in revascularization group (47.1 months) (P > 0.05). There was no statistical difference in other baseline characteristics, too. The clinical outcomes in conservative group and revascularization group are described in Table 5. In revascularization group, 19 of 133 patients (14.3%) suffered from rebleeding after surgical revascularization. In addition, referring to the first hemorrhagic hemisphere, 8 patients (6.0%) suffered rebleeding in the contralateral hemisphere, and 11 patients (8.3%) in the same hemisphere. In conservative group, 51 of 189 patients (27.0%) suffered cerebral rebleeding after the initial treatment, among which 20 patients (10.6%) in the contralateral hemisphere and 31 patients (16.4%) in the same hemisphere. Such results demonstrated that revascularization was significantly effective in reducing the probability of rebleeding on the operated side but not on the contralateral side (P = 0.033 and P = 0.152, respectively).
In contralateral hemisphere patients, who underwent conservative group had average 54.9 months from first bleeding to rebleeding, 36.3 months in revascularization group. In ipsilateral hemisphere patients, who underwent conservative group had average 67.5 months from first bleeding to rebleeding, 31.6 months in revascularization group. So, either operated or contralateral side, surgical revascularization could not prolong the time from first bleeding to rebleeding (P = 0.360 and P = 0.438, respectively). In addition, 8 patients (6.0%) suffer from hydrocephalus in the revascularization group versus 24 in the conservative group (12.7%) (P = 0.048), and 11 deaths (8.3%) in the revascularization group versus 38 in the conservative group (20.1%) (P = 0.004).
As for the functional outcomes, the average mRS was significantly better in revascularization group (1.7 ± 1.5) than that in conservative group (2.8 ± 1.9) (P < 0.001). The proportion of patients with mRS < 3 (83.5%) in revascularization group was also significantly more than that in the conservative group (52.9%) (P < 0.001).
Unilateral vs. bilateral revascularization
Given that the effectiveness of revascularization has been proved, we stepped forward to consider the choice of bilateral or unilateral revascularization. In revascularization group, bilateral revascularization was performed in 42 patients and unilateral revascularization in 91 patients. The average interval from last surgical revascularization to the rebleeding was 32.1 ± 15.8 months in bilateral group and 29.3 ± 15.1 months in unilateral group (P = 0.402). There was no statistical difference in the baseline characteristics. The clinical outcomes in unilateral revascularization group and bilateral revascularization group are described in Table 6.
In order to reveal the difference of the treatment effect between unilateral and bilateral revascularization group, we define the rebleeding on the operative side following surgical revascularization as positive event, no matter rebleeding or not on the hemisphere contralateral to the operative side. In the unilateral group, 11 of 91 sides (12.1%) suffered from positive events and 2 of 84 sides (2.4%) suffered from positive events in the bilateral group (P = 0.034). It is important to note that case 29 suffered from bilateral IVH after the second revascularization, and other seven bilateral-revascularization patients suffered from rebleeding between the bilateral revascularization in the contralateral side of the first revascularization side.
In addition, there was no significant difference in the functional outcomes, the average mRS was 1.8 ± 1.6 in bilateral group and 1.4 ± 1.3 in unilateral group (P = 0.099), and the proportion of patients with mRS < 3 was 84.6% in bilateral group and 90.5% in unilateral group (P = 0.358). According to this study, we suggest that the premier choice is the bilateral revascularization for patients with HMD.
Annual rebleeding rates in each category
The long-term rebleeding rates and Kaplan–Meier rebleeding-free curves had difference in the revascularization and conservative groups, as well as in the unilateral and bilateral revascularization groups.
(1) The annual rebleeding rate (ARR) (ipsilateral rebleeding) in revascularization and non-revascularization group was 2.0% and 3.8%/person-year, respectively. The P value was 0.111, using the log-rank test (risk hazard ratio 0.531, 95% confidence interval 0.277–1.019; Fig. 4a). (2) ARR (contralateral rebleeding) in revascularization and non-revascularization group was 1.5% and 2.5%/person-year, respectively. The P value was 0.261, using the log-rank test (risk hazard ratio 0.568, 95% confidence interval 0.258–1.252; Fig. 4b). (3) ARR (postoperative rebleeding) in bilateral revascularization and unilateral revascularization group was 0.5% and 3.3%/side-year, respectively. The P value was 0.001, using the log-rank test (risk hazard ratio 0.258, 95% confidence interval 0.057–1.164; Fig. 4c). Such result further proved the superiority of bilateral revascularization to unilateral revascularization.
Follow-up image findings
Due to the limitations of the medical conditions and the patient compliance, DSA studies were only performed in a few patients postoperatively, but MR angiography or CTA was performed in many patients several years after discharge. Postoperative DSA follow-ups were obtained in 61 patients (postoperative 0.5–2 years). According to the criteria proposed by Matsushima and Inaba [16], of 73 hemispheres, well-developed revascularization (grades A and B) was observed in 60 hemispheres (82.2%) and poor-developed revascularization (grade C) in 13 hemispheres (17.8%). Figure 5 illustrates a bilateral revascularization patient with well-developed revascularization. In addition, moyamoya vessels were regressed in 36 hemispheres (49.3%).
a, b Digital subtraction angiography (DSA) of a 25-year-old man with HMD. c, d DSA 9 months after left combined revascularization shows that the left MCA was supplied by the STA. e, f DSA 9 months after subsequent right combined revascularization shows that the right MCA was supplied by the STA. The arrows represent the anastomotic sites
Discussion
HMD is a common type of cerebrovascular disease with high rates of disability, mortality, and high risk of rebleeding [30]. In our cohort, patients with HMD were more frequent than those with ischemic type, accounting for 55.8% of all MMD patients, higher than reports from North America and Europe [10, 14]. It primarily affected adult females, with a female to male ratio of 1.385:1.0. The above-described epidemic characteristics of HMD were similar to other reports in China or Japan [9, 21]. Based on radiologic characteristic, IVH was the most frequent presentations, accounting for 32.0% of all cases in this cohort, the underlying mechanism may be attributed to the rupture of periventricular anastomosis from abnormally dilated branches of AChA-PCoA after long-standing hemodynamic stress [19]. Rebleeding is the leading cause of death in HMD. In this study, 85 patients (26.4% of all HMD patients) suffered from rebleeding events during follow-up, among which twenty patients (23.5%) died directly from rebleeding. The frequency of rebleeding is within the range (16–66%) of previous studies [12, 13, 28]. Furthermore, our result demonstrated that the rebleeding rate can be decreased significantly after surgical revascularization (14.29% in revascularization group vs. 26.98% in conservative group). Notably, the sample size (322 HMD cases) in this study is the largest among the reports regarding HMD until now. In addition, with average follow-up period of 86.7 months, most of these patients (38 patients, 44.7%) suffered from rebleeding within 2 years, and this result illustrated that HMD is prone to rebleeding within the short term following first hemorrhagic attack. Five revascularization patients suffered from rebleeding 10 years later after initial bleeding. So, it is essential for long-term follow-up of HMD patients, despite underwent revascularization.
The treatment modalities of MMD included surgical revascularization and conservative management. Actually, STA-MCA bypass is generally employed as the standard surgical treatment for ischemic MMD based on the guideline recommendation [20, 23]. Regarding HMD, it has been a controversy whether surgical revascularization could reduce the risk of rebleeding. Previous studies have shown that revascularization does not exhibit better outcome than conservative treatment for HMD [4, 7]. But most other scholars disagree this viewpoint [1, 5, 15]. Particularly, the recent JAM trial provided the best evidence that direct revascularization could reduce the risk for rebleeding in adult patients with HMD; the 80 patients were enrolled and randomized to non-surgical and surgical group who underwent bypass in this prospective study [17]. The result showed that the annual risk of rebleeding was 2.7% in surgical group and was significantly lower than that in non-revascularization group (7.6%/year, P = 0.042). In addition, Zhao et al. suggested that revascularization can improve regional blood flow and have greater efficacy at preventing rebleeding than conservative treatment [15]. Revascularization could also improve HMD patients’ performance status and the functional outcomes [1]. Our results were consistent with the current widely accepted viewpoints.
In this study, the rebleeding rate was significantly lower in revascularization group than that in conservative group (14.29% vs. 26.98%, P = 0.007). Further explore annual rebleeding rate, ipsilateral rebleeding ARR in revascularization and non-revascularization group was 2.02%/person-year and 3.79%/person-year (P = 0.111). Contralateral rebleeding ARR in revascularization and non-revascularization group was 1.47%/person-year and 2.45%/person-year (P = 0.261). These results indicated that revascularization surgery for HMD patients is effective, although further evaluation with long-term follow-up is necessary to validate this strategy. However, conservative treatments do not improve hemodynamic disorders and existing malformed vessels, like improvement in anterior choroidal artery (AChA)-posterior communicating artery (PCoA) extension [8]. So, the results of conservative treatment obtained in follow-up basically fit with the natural course of HMD.
Based on the pathological characteristic of bilateral vascular abnormality in HMD, the necessity of bilateral revascularization in HMD patient needs to be further verified. Our result showed that the postoperative rebleeding ARR in bilateral revascularization group was significantly lower than that of the unilateral revascularization group (0.46%/side-year vs. 3.34%/side-year, P = 0.001). Such result demonstrated that HMD patients may evidently benefit from bilateral revascularization regarding long-term rebleeding rate. However, we have to bear in mind the retrospective nature of this study. To further elucidate the necessity of bilateral revascularization in HMD group, it is necessary to conduct a prospective controlled study which only enrolls HMD patients with bilateral vascular pathology and history of single-side hemorrhage, and then compares the rebleeding rate of the hemisphere contralateral to the primary bleeding side between unilateral and bilateral revascularization group.
In fact, the pathogenesis of recurrent hemorrhage in HMD remains unclear. The fragile collateral vessels, concomitant microaneurysms, abnormal dilation and branch extension of AChA-PCoA, and cerebral microbleeds may be responsible [10, 12, 19, 26]. In this study, 47 patients (14.6%) had intracranial aneurysms, nearly half of them suffered from rebleeding. The study had shown that because of structural dysfunction of moyamoya vessels and hemodynamic disorders, MMD patients maybe more likely to have intracranial aneurysms [22]. But Ni et al. believed that after revascularization, especially for MMD patients with unilateral surgery while the aneurysm was contralateral, the surgery reduced the pressure of the aneurysmal vessel, and prolonged decompression might cause the aneurysm to disappear [18]. In addition, the inadequate collateral revascularization and the abnormal dilation and branch extension of AChA-PCoA have been recognized as an independent risk factor for rebleeding in HMD [3]. In a prospective study, the operated hemispheres showed a higher rate of improvement in AChA-PCoA extension than non-operated hemispheres [8]. Therefore, bilateral revascularization may be more effective in improving the abnormal vessels bilaterally and further preventing bleeding. All of these might be correlated with the reduced rate of rebleeding in revascularization group.
Besides rebleeding, the performance status and functional outcomes of patients are also of concern. In this study, revascularization could significantly improve functional outcome, and the average mRS was significantly better in revascularization group (1.7 ± 1.5) than that in conservative group (2.8 ± 1.9) (P < 0.001). But there was no significant difference between bilateral and unilateral revascularization, the average mRS was 1.4 ± 1.3 in bilateral group and 1.8 ± 1.6 in unilateral group (P = 0.099). As demonstrated in a recent study of functional outcomes in HMD, a total of 104 HMD patients were included with mean mRS of 1.3 at baseline, after underwent STA-MCA bypass or indirect revascularization, their mean mRS improved to 1.1 [1]. In addition, they indicated that the patients’ initial mRS was positively associated with mRS at the final follow-up (P < 0.001) and STA-MCA direct bypass was associated with better performance status (P = 0.033) in this study. Therefore, we may need to include more revascularization patients or a longer follow-up period, to verify superiority of STA-MCA bypass between different surgical techniques for preventing rebleeding and improving functional outcomes.
Interestingly, the surgical revascularization significantly reduced the occurrence rate of hydrocephalus compared to conservative group. It is now generally accepted that the significant mass effect caused by parenchymal hemorrhage or blood in the ventricular system is the major causes of hydrocephalus [2, 24, 27]. According to this study, after surgical revascularization, the rate of rebleeding was 14.3%, compared to 27.0% of the rebleeding rate in the conservative group. So, the reduced rate of hydrocephalous in revascularization group may result from the reduced rebleeding rate.
Limitations
Several limitations of the study must be noted. First, 9 patients were lost to follow-up in this study. The loss to follow-up rate could have affected the results. Second, because of the retrospective and non-random nature of this study, selection biases might have assigned patients with different features and known or unknown risks to the revascularization versus the conservative groups. Third, revascularization group including indirect and combined revascularization, which is more effective in preventing bleeding, remains to be proved. These biases may have an impact on the validity of conclusions. Further multicenter prospective studies that have a low rate of loss of follow-up may resolve these limitations.
Conclusions
This study proved the better treatment efficacy of surgical revascularization than that of conservative treatment in HMD patients, regarding both in rebleeding rate and mortality rate. Furthermore, bilateral revascularization seems more effective in preventing rebleeding than unilateral revascularization. Both bilateral revascularization and unilateral revascularization could significantly improve functional outcome.
Availability of data and material
The data that support the findings of this study are available from the corresponding author upon reasonable request.
Code availability
Not applicable.
References
Abhinav K, Furtado SV, Nielsen TH, Iyer A, Gooderham PA, Teo M, Lee J, Han SS, Steinberg GK (2020) Functional outcomes after revascularization procedures in patients with hemorrhagic moyamoya disease. Neurosurgery 86(2):257–265. https://doi.org/10.1093/neuros/nyz074
Diringer MN, Edwards DF, Zazulia AR (1998) Hydrocephalus: a previously unrecognized predictor of poor outcome from supratentorial intracerebral hemorrhage. Stroke 29(7):1352–1357. https://doi.org/10.1161/01.str.29.7.13523
Funaki T, Takahashi JC, Houkin K, Kuroda S, Takeuchi S, Fujimura M, Tomata Y, Miyamoto S (2018) Angiographic features of hemorrhagic moyamoya disease with high recurrence risk: a supplementary analysis of the Japan Adult Moyamoya Trial. J Neurosurg 128(3):777–784. https://doi.org/10.3171/2016.11.Jns161650
Ge P, Zhang Q, Ye X, Liu X, Deng X, Li H, Wang R, Zhang Y, Zhang D, Zhao J (2017) Long-term outcome after conservative treatment and direct bypass surgery of moyamoya disease at late Suzuki stage. World Neurosurg 103:283–290. https://doi.org/10.1016/j.wneu.2017.03.101
Ge P, Zhang Q, Ye X, Liu X, Deng X, Wang J, Wang R, Zhang Y, Zhang D, Zhao J (2020) Postoperative collateral formation after indirect bypass for hemorrhagic moyamoya disease. BMC Neurol 20(1):28. https://doi.org/10.1186/s12883-020-1612-z
Ishiguro T, Okada Y, Ishikawa T, Yamaguchi K, Kawashima A, Kawamata T (2019) Efficacy of superficial temporal artery-middle cerebral artery double bypass in patients with hemorrhagic moyamoya disease: surgical effects for operated hemispheric sides. Neurosurg Rev 42(2):559–568. https://doi.org/10.1007/s10143-018-01059-z
Jang DK, Lee KS, Rha HK, Huh PW, Yang JH, Park IS, Ahn JG, Sung JH, Han YM (2017) Bypass surgery versus medical treatment for symptomatic moyamoya disease in adults. J Neurosurg 127(3):492–502. https://doi.org/10.3171/2016.8.Jns152875
Jiang H, Ni W, Xu B, Lei Y, Tian Y, Xu F, Gu Y, Mao Y (2014) Outcome in adult patients with hemorrhagic moyamoya disease after combined extracranial-intracranial bypass. J Neurosurg 121(5):1048–1055. https://doi.org/10.3171/2014.7.Jns132434
Kang S, Liu X, Zhang D, Wang R, Zhang Y, Zhang Q, Yang W, Zhao JZ (2019) Natural course of moyamoya disease in patients with prior hemorrhagic stroke. Stroke 50(5):1060–1066. https://doi.org/10.1161/strokeaha.118.022771
Khan NI, Saherwala AA, Chen M, Salehian S, Salahuddin H, Welch BG, Pinho MC, Shang T (2019) Prevalence of and risk factors for cerebral microbleeds in moyamoya disease and syndrome in the American population. Cerebrovascular diseases extra 9(3):139–147. https://doi.org/10.1159/000504530
Kim JS (2016) Moyamoya disease: epidemiology, clinical features, and diagnosis. J Stroke 18(1):2–11. https://doi.org/10.5853/jos.2015.01627
Kim KM, Kim JE, Cho WS, Kang HS, Son YJ, Han MH, Oh CW (2017) Natural history and risk factor of recurrent hemorrhage in hemorrhagic adult moyamoya disease. Neurosurgery 81(2):289–296. https://doi.org/10.1093/neuros/nyw179
Kobayashi E, Saeki N, Oishi H, Hirai S, Yamaura A (2000) Long-term natural history of hemorrhagic moyamoya disease in 42 patients. J Neurosurg 93(6):976–980. https://doi.org/10.3171/jns.2000.93.6.0976
Kraemer M, Heienbrok W, Berlit P (2008) Moyamoya disease in Europeans. Stroke 39(12):3193–3200. https://doi.org/10.1161/strokeaha.107.513408
Liu X, Zhang D, Shuo W, Zhao Y, Wang R, Zhao J (2013) Long term outcome after conservative and surgical treatment of haemorrhagic moyamoya disease. J Neurol Neurosurg Psychiatry 84(3):258–265. https://doi.org/10.1136/jnnp-2012-302236
Matsushima Y, Inaba Y (1984) Moyamoya disease in children and its surgical treatment. Introduction of a new surgical procedure and its follow-up angiograms. Childs Brain 11(3): 155–170. https://doi.org/10.1159/000120172
Miyamoto S, Yoshimoto T, Hashimoto N, Okada Y, Tsuji I, Tominaga T, Nakagawara J, Takahashi JC (2014) Effects of extracranial-intracranial bypass for patients with hemorrhagic moyamoya disease: results of the Japan Adult Moyamoya Trial. Stroke 45(5):1415–1421. https://doi.org/10.1161/strokeaha.113.004386
Ni W, Jiang H, Xu B, Lei Y, Yang H, Su J, Gu Y, Mao Y (2018) Treatment of aneurysms in patients with moyamoya disease: a 10-year single-center experience. J Neurosurg 128(6):1813–1822. https://doi.org/10.3171/2017.3.Jns162290
Qin Y, Ogawa T, Fujii S, Shinohara Y, Kitao S, Miyoshi F, Takasugi M, Watanabe T, Kaminou T (2015) High incidence of asymptomatic cerebral microbleeds in patients with hemorrhagic onset-type moyamoya disease: a phase-sensitive MRI study and meta-analysis. Acta Radiol 56(3):329–338. https://doi.org/10.1177/0284185114524198
Research Committee on the Pathology and Treatment of Spontaneous Occlusion of the Circle of Willis; Health Labour Sciences Research Grant for Research on Measures for Infractable Diseases (2012) Guidelines for diagnosis and treatment of moyamoya disease (spontaneous occlusion of the circle of Willis). Neurol Med Chir (Tokyo) 52(5):245–266. https://doi.org/10.2176/nmc.52.245
Sato Y, Kazumata K, Nakatani E, Houkin K, Kanatani Y (2019) Characteristics of moyamoya disease based on national registry data in Japan. Stroke 50(8):1973–1980. https://doi.org/10.1161/strokeaha.119.024689
Sencer S, Poyanli A, Kiriş T, Sencer A, Minareci O (2000) Recent experience with moyamoya disease in Turkey. Eur Radiol 10(4):569–572. https://doi.org/10.1007/s003300050962
Shang S, Zhou D, Ya J, Li S, Yang Q, Ding Y, Ji X, Meng R (2020) Progress in moyamoya disease. Neurosurg Rev 43(2):371–382. https://doi.org/10.1007/s10143-018-0994-5
Staykov D, Volbers B, Wagner I, Huttner HB, Doerfler A, Schwab S, Bardutzky J (2011) Prognostic significance of third ventricle blood volume in intracerebral haemorrhage with severe ventricular involvement. J Neurol Neurosurg Psychiatry 82(11):1260–1263. https://doi.org/10.1136/jnnp.2010.234542
Suzuki J, Takaku A (1969) Cerebrovascular “moyamoya” disease. Disease showing abnormal net-like vessels in base of brain. Arch Neurol 20(3): 288–299. https://doi.org/10.1001/archneur.1969.00480090076012
Yamada H, Saga I, Kojima A, Horiguchi T (2019) Short-term spontaneous resolution of ruptured peripheral aneurysm in moyamoya disease. World Neurosurg 126:247–251. https://doi.org/10.1016/j.wneu.2019.02.193
Yang WS, Shen YQ, Zhang XD, Zhao LB, Wei X, Xiong X, Xie XF, Li R, Deng L, Li XH, Lv XN, Lv FJ, Li Q, Xie P (2021) Hydrocephalus growth: definition, prevalence, association with poor outcome in acute intracerebral hemorrhage. Neurocrit Care 35(1):62–71. https://doi.org/10.1007/s12028-020-01140-w
Yoshida Y, Yoshimoto T, Shirane R, Sakurai Y (1999) Clinical course, surgical management, and long-term outcome of moyamoya patients with rebleeding after an episode of intracerebral hemorrhage: an extensive follow-Up study. Stroke 30(11):2272–2276. https://doi.org/10.1161/01.str.30.11.2272
Zhang H, Zheng L, Feng L (2019) Epidemiology, diagnosis and treatment of moyamoya disease. Exp Ther Med 17(3):1977–1984. https://doi.org/10.3892/etm.2019.7198
Zhang M, Tang J, Liu N, Xue Y, Ren X, Fu J (2020) Postoperative functional outcomes and prognostic factors in two types of adult moyamoya diseases. J Stroke Cerebrovasc Dis 29(8):104846. https://doi.org/10.1016/j.jstrokecerebrovasdis.2020.104846
Funding
This work was supported by the Fundamental Research Funds for the Central Universities (WK9110000133), the Public Welfare Technology Application Research Linkage Project of Anhui Province in China (No. 1704f0804015), and the Key Research and Development Program Projects of Anhui Province in China (No. 1804h08020250).
Author information
Authors and Affiliations
Contributions
Conception and design: SJ Yu, N Zhang, CY Xia. Acquisition of data: J Liu, CW Li, S Qian, Y Xu. Analysis and interpretation of data: SJ Yu, N Zhang, CY Xia. Drafting the article: SJ Yu, N Zhang. Critically revising the article: N Zhang, CY Xia. Reviewed submitted version of manuscript: all authors. Approved the final version of the manuscript: all authors. Statistical analysis: SJ Yu. Administrative/technical/material support: N Zhang, T Yang, N Li, MH Zeng, DX Li, CY Xia. Study supervision: CY Xia.
Corresponding author
Ethics declarations
Ethics approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Consent to participate
Informed consent was obtained from all individual participants included in the study.
Consent for publication
Not applicable.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Yu, S., Zhang, N., Liu, J. et al. Surgical revascularization vs. conservative treatment for adult hemorrhagic moyamoya disease: analysis of rebleeding in 322 consecutive patients. Neurosurg Rev 45, 1709–1720 (2022). https://doi.org/10.1007/s10143-021-01689-w
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10143-021-01689-w