Abstract
The surgical management of hydrocephalus in patients with posterior fossa lesions (PFL) is critical for optimal patient outcome(s). Accordingly, it is prudent to identify patients in need of aggressive surgical intervention (i.e., ventriculoperitoneal [VP] shunting). To analyze prevalence of, and risk factors associated with, the development of post-operative hydrocephalus in both pediatrics and adults. A retrospective institutional analysis and review of patient records in those who had undergone PFL surgery was performed. In so doing, the authors identified patients that went on to develop post-operative hydrocephalus. The study included pediatric and adult patients treated between 2009 and 2017. Fifteen of 40 pediatric (37.5%) and 18 of 262 adult (6.9%) patients developed hydrocephalus after PFL surgery. The most common tumor entity in pediatrics was medulloblastoma (34%), astrocytoma (24.4%), and pilocytic astrocytoma (22%), whereas in adults, metastasis (29.5%), meningioma (22%), and acoustic neuroma (17.8%) were most common. Young age ≤ 2 years, medulloblastoma (OR 13.9), and brain stem compression (OR 5.4) were confirmed as independent predictors for hydrocephalus in pediatrics and pilocytic astrocytoma (OR 15.4) and pre-operative hydrocephalus (OR 3.6) in adults, respectively. All patients received VP shunts for hydrocephalus management and the mean follow-up was 29.5 months in pediatrics vs 19.2 months in adults. Overall complication rates related to VP shunts were 33.3% in pediatrics and 16.7% in adults, respectively. Shunt dependency and associated complications in pediatrics were noted to be higher than in adults. Given the identification of predictors for hydrocephalus, it is authors’ contention that certain patients with those predictors may ultimately benefit from an alternative treatment regimen (e.g., pre-operative interventions) prior to PFT surgery.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Hydrocephalus is one of the major complications associated with surgery for lesions located within the posterior fossa [1, 2, 5, 16]. Interestingly, there continue to be discussions within the neurosurgical community with regard to the optimal timing and treatment modality for hydrocephalus [1, 2, 5, 11, 16, 19, 20, 22, 24, 26].
Given such discordance of an optimal strategy for hydrocephalus management (e.g., pre- or post-operative shunting; perioperative implantation of external ventricular drainage; endoscopic third ventriculostomies), it is important to identify cohorts of patients who are at risk for the development of hydrocephalus prior to lesion resection. Previous studies have demonstrated that the rate of post-resection hydrocephalus (i.e., for tumors of the posterior fossa) ranges from 10 to 40% of pediatric patients [4, 8, 16]. These studies identified young age, medulloblastoma, papilledema, and grade of hydrocephalus as key risk factors [10, 16, 21]. Alternatives to ventriculoperitoneal (VP) shunting such as prophylactic endoscopic third ventriculostomies (ETV) have been reported resulting in a reduction of tumor-related occlusive hydrocephalus in up to 90% of cases [3]. The effectiveness of ETV prior to posterior fossa lesions (PFL) surgery was described in adults as well as pediatric patients resulting in a significant reduction of shunt dependency [17]. However, major complications (e.g., injury of basilar artery) have been described in patients undergoing ETV [7].
In stark contrast to pediatrics, data in adult patients remains scarce. To the best of our knowledge, there has been one study describing 85 shunts among 287 consecutive patients undergoing posterior fossa surgery without any risk factor analyses [26]. Accordingly, we sought to examine a large institutional database containing both pediatric and adult patients who underwent removal of a posterior fossa tumor. Our ultimate aim was to investigate the prevalence and risk factors associated with the development of post-operative hydrocephalus. In so doing, we sought to identify patients at risk for shunt placement in an effort to fully inform neurosurgical plans prior to posterior fossa tumor surgery.
Methods
This study was approved by the author’s Institutional Review Board (IRB) and Committee on Ethics. No informed consent of patient was required for this study. Briefly, we retrospectively analyzed the institutional database for posterior fossa brain lesion patients who underwent resection between the years 2009 and 2017 for the subsequent development of hydrocephalus. The last documented clinical and/or radiological encounter was used for all downstream analyses. All patients with PFL, who underwent surgical treatment, were included in the study. Patients with pre-operative shunt implantation or conservative treatment were excluded in order to build a homogenous cohort.
As per the abovementioned, the following parameters were retrieved from the database: basic characteristics (age, sex); histopathology of tumor; volume/location/side of the lesion; perilesional edema; pre-operative hydrocephalus and cerebrospinal fluid (CSF) capping; patient position during surgery; rate of pre-/peri- and post-operative implementation of external ventricular drains (EVD), extent of resection divided into complete, subtotal (> 90% lesion mass reduction), biopsy; post-operative hydrocephalus; interval to VP shunt implantation and complications at follow-up.
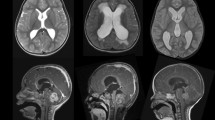
Patients with acute symptomatic hydrocephalus received pre-operative EVD. Prior to PFL surgery, all cases were presented in our conference and interdisciplinary decision for prophylactic perioperative EVD was made depending on the MRI result, preference of surgeon, and recently published novel grading system for the necessity of CSF drainage [27]. A pre-operative magnetic resonance imaging (MRI) scan was used for the analysis of hydrocephalus. Evans’ ratio > 0.3 with associated clinical manifestations and/or a CSF fistula, which could not surgically be managed despite one or more revisions with associated clinical symptoms like headache and vomiting, was ultimately defined as hydrocephalus. At follow-up, if patients developed clinical symptoms, additional MRI or CT scan was performed to rule out a late hydrocephalus. Perilesional edema was classified into 3 categories: perifocal, unilateral, and bilateral. Perifocal edema was defined as edema, which disseminated < 5 mm from the tumor. Edema which had disseminated > 5 mm from the tumor without crossing the midline was defined as unilateral while edema crossing midline was defined as bilateral edema. As previously reported, ABC/2 was used for the estimation of tumor volume [28]. Per our institutional standard(s), all patients underwent post-operative imaging within 72 h of surgery [15]. The modality was dependent on the clinical indication (i.e., computed tomography [CT] vs MRI).
All patients with post-operative hydrocephalus and/or acute symptomatic hydrocephalus which necessitated permanent CSF drainage underwent implantation of a VP shunt; patients were followed for up to 5 years. As noted, the aims of the study were to analyze the prevalence of hydrocephalus requiring intervention in both pediatric and adult patients, and predictors of hydrocephalus. This was accomplished by dividing all patients into 2 groups (post-operative hydrocephalus and no hydrocephalus). Of note, we excluded 3 patients (n = 3), who underwent pre-operative VP shunt implantation in order to define homogenous cohorts. By doing so, all variables were dichotomized and analyzed. Finally, we evaluated interval, etiology, and complications associated with VP shunt implantation at discharge as well as at follow-up.
Statistical analysis
For the purposes of data analyses, patients were dichotomized by the median of the any interrogated parameters (e.g., age, volume). For parametric analyses, Student’s t test was used. Binary parameters were analyzed via the chi-square test. Multivariate analyses were performed using a binary logistic regression model; this incorporated a backward, stepwise exclusion to identify independent predictors of post-operative hydrocephalus. All statistical tests were 2-tailed. Further, odds ratio (OR) and confidence interval with 95% (Cl 95%) were calculated. In case of an empty cell value, the OR was not calculated. A p value < 0.05 was deemed to be statistically significant. All calculations were performed via IBM SPSS Statistics© (version 24, IBM Corp., Armonk, NY, USA).
Results
Our study included 40 pediatric and 262 adult patients. Of these, 15 pediatric (37.5%) and 18 adult (6.9%) patients went on to develop hydrocephalus after resection of a posterior fossa lesion (Table 1).
Overall characteristics of posterior fossa lesions in pediatric and adult patients
In pediatric patients, the most frequent lesion entity within the posterior fossa was medulloblastoma (14 patients; 34%), followed by astrocytoma (10 patients; 24.4%) and pilocytic astrocytoma (9 patients; 22%). Brain stem tumors with unclear histopathology were classified into the category “others.” In contrast, metastasis (77 patients; 29.5%) was the most frequent tumor entity in adult patients followed by meningioma (58 patients; 22%) and acoustic neuroma (46 patients; 17.8%). With regard to adult metastases, lung carcinoma (33 patients; 43.5%) was the most common followed by breast cancer (18 patients; 23.1%) and gastrointestinal tumors (17 patients; 21.8%) (Fig. 1).
The median age of pediatric patients was 12 years (IQR 7–14); 19 of 40 patients (47.5%) were female. Regarding lesion location, 31 patients (77.5%) presented with midline lesions. The most frequent anatomic location was within the fourth ventricle (27 patients; 67.5%) followed by cerebellum (24 patients; 60%); importantly, some patients presented with multi-focal disease. Pediatric patients had significant larger median lesion volume compared with adult patients (i.e., 22 cm3 vs 12 cm3 of adult) (IQR 13.5–31.2) which was also reflected in the higher rate of resultant hydrocephalus (55% vs 38.3% of adults) and CSF capping (72.5% vs 53.4% of adults). Pre- and perioperative EVD were placed in 34 patients (85%). There was no necessity of EVD placement post-operatively. Complete resection was obtained in 23 patients (57.5%) while a subtotal resection of tumor was obtained in 16 patients (40%) and a biopsy was performed in 1 patient (2.5%) (Table 1).
Regarding adult patients, the median age was 55 years (IQR 41–64) and 158 of 262 patients were female (60.3%). As compared with pediatric patients, the most frequent anatomic location of these posterior fossa lesions was within the cerebellum (49.2%). Other highly prevalent locations included the cerebellopontine angle (CPA) (29.9%); tumors were typically unilateral in location (82.6%). Radiologically, perilesional edema occurred more often in adult then pediatric patients (61.4% vs. 46.3%). One hundred eighty-six patients (71%) received pre- and perioperative EVD; among them, 3 patients (1.1%) had acute symptomatic hydrocephalus. One patient (0.3%) without initial EVD received EVD post-operatively due to hydrocephalus. In 175 patients (66.8%), complete resection of lesion was achieved, while a subtotal resection was achieved in 85 patients (32.4%) and a biopsy was performed in 2 patients (0.8%) (Table 2).
Risk factors associated with the development of post-operative hydrocephalus
Univariate analysis demonstrated that risk factors for post-operative hydrocephalus in pediatric patients were young age (i.e., ≤ 2 years) (OR was not calculated due to empty cell value, p = 0.02), medulloblastoma (OR 6.0, p = 0.01), particularly lesions localized within the fourth ventricle (OR 6.5, p = 0.02), brain stem compression (OR 4.9, p = 0.02), and CSF capping (OR 9.3, p = 0.02). Interestingly, histopathology indicative of astrocytoma (OR 0.1, p = 0.003) was a negative predictor for the development of hydrocephalus (Table 3).
Multivariate analysis, young age (i.e., ≤ 2 years) (OR was not calculated due to empty cell value, p = 0.001), medulloblastoma (OR 13.9, p = 0.007), and brain stem compression (OR 5.4, p = 0.03) were confirmed as independent parameters associated with the development of post-operative hydrocephalus (Nagelkerke R2 = 0.621). Pre-operative hydrocephalus or CSF capping was not associated with hydrocephalus (Table 3).
Regarding adult patients, pilocytic astrocytoma (OR 15.1, p = 0.001; OR 15.4, p = 0.01) and pre-operative hydrocephalus (OR 3.5, p = 0.01) were significant risk factors for the development of post-operative hydrocephalus in the univariate as well as in the multivariate analysis (Table 4).
As per the above, we note that pediatric patients had different parameters (age ≤ 2 years, medulloblastoma, brain stem compression) that were independently associated with the development of hydrocephalus as compared with adults (pilocytic astrocytoma, pre-operative hydrocephalus).
Management of hydrocephalus
As per our institutional standard, all pediatric and adult patients underwent the implementation of VP shunts for the surgical management of hydrocephalus. In pediatric patients, the mean interval from posterior fossa lesion surgery until VP shunt implantation was 17.9 ± 16.7 days, whereas in adult patients, the interval was 69.7 ± 109.9 days. In other patients, the leading etiology for shunt was communicating hydrocephalus (pediatric 66.7% vs. adult 50%) followed by CSF fistulas (pediatric 26.8% vs. adult 50%). The overall complication rate was 33.3% in pediatric patients; 2 patients (13.3%) had infections, 3 patients (20%) had shunt malfunctions at a mean follow-up of 29.5 months. In adult patients, the overall complication rates were lower at 16.7%; 2 patients developed infection and 1 patient dysfunction at a mean follow-up of 19.2 months (Table 5).
Discussion
Herein, we attempted to determine the prevalence of post-operative hydrocephalus in pediatric and adult patients secondary to the resection of a posterior fossa lesion and in so doing identify associated risk factors. The data obtained from our retrospective institutional cohort ultimately revealed a ~ 5-fold higher occurrence of post-operative hydrocephalus in pediatric patients as compared with adults; given such an elevated risk, it may be prudent to consider advantages associated with pre-operative shunting within pediatric populations. In line with such thinking, rapid clinical improvement, lower in-hospital morbidity/mortality, decreased exposure to anesthesia, and less technically challenging surgeries have all been highlighted as potential benefits of such an approach [1, 11, 16]. It is also important to note that VP shunt placement has been linked to several complications (e.g., infection, dysfunction, and dislocation) [16]. Critically severe—albeit rare—complications of VP shunting (e.g., tentorial herniation, hemorrhage, and metastasis along shunt catheters) have also been reported [9, 12, 13, 16]. On the other hand, occlusive hydrocephalus might be spontaneously treated after PFL surgery, which implies rather to a conservative management. Thus, many clinicians still prefer EVD or pre-/perioperative ETV as alternative treatment regimens in patients at high risk for post-operative development of hydrocephalus [19, 20] [26, 27].
Previously, Riva-Cambrin et al. developed the Canadian Pre-operative Prediction Rule for Hydrocephalus (CPPRH) in pediatric patients upon diagnosis of posterior fossa tumor in an effort to identify those at high risk of developing hydrocephalus [21]. Five components (age less than 2 years, presence of papilledema, hydrocephalus on pre-operative imaging, estimated tumor diagnosis like medulloblastoma, ependymoma, brain stem glioma, and cerebral metastasis) comprised a scoring system that ranges between 0 and 10 points with higher scores correlating with a higher risk for persistent hydrocephalus [21]. In the modified version, the presence of papilledema was replaced by radiological evidence of transependymal flow [10].
Beyond clinical characteristics, molecular subtype may also have an influence on the development of hydrocephalus within pediatric cohorts. Interestingly, Schneider et al. examined molecular subtypes of medulloblastoma in 130 pediatric patients and found that up to 43% of those subtype 4 developed persistent hydrocephalus whereas those within the wingless (WNT) subgroup were not affected [16, 23].
In contrast to pediatrics, the exploration of hydrocephalus risk factors and clinical management in adults with posterior fossa lesions remains underexplored and is therefore less clear. Herein, two predictors associated with the development of hydrocephalus after resection of a posterior fossa lesion were identified, i.e., pilocytic astrocytoma and pre-operative hydrocephalus. Given the small number of patients within our cohort diagnosed with pilocytic astrocytoma, the prevailing mechanisms remain elusive but a possible pathophysiologic explanation may be related to the slow growth of the tumor [6]. Such growth kinetics may lead to the development of chronic hydrocephalus (i.e., a decrease in parenchymal compliance) resulting in rigidity of ventricular walls thereby requiring surgical management irrespective of resection outcome(s).
As per our institutional standard, the management of hydrocephalus was via VP shunt placement. Despite this, we acknowledge that ETV has gained popularity as first-line therapy to treat, as well as prevent, post-operative hydrocephalus [3]. The success rate of ETVs ranges between 71% and over 90% in a longitudinal analysis up to over 9 years, whereas the overall complication rate of ETV was shown to be 9% in a recent meta-analysis [14, 18, 25]. As such, it does have lower complication rates then have been associated with VP shunts, yet it must be acknowledge that severe complications (e.g., intratumoral hemorrhage, upward herniation, and death) have been reported in ~ 1% of examined cohorts [16]. Given such data, pre-resection ETVs remain controversial. We do note that post-resection ETVs have however been shown to be effective in cases of EVD weaning failure as an alternative to shunt placement [18, 25].
Limitations of the study
While the study was retrospective in nature (i.e., with acknowledgement on the potential for both bias and/or confounding), we feel that this is outweighed by the inclusion of large number of consecutively treated pediatric and adult patients with an extensive period of surgical follow-up.
Conclusions
As per the abovementioned, the predictors identified may be useful tool for the stratification of low- and/or high-risk patients, who may benefit from the prophylactic management of hydrocephalus. By verifying those predictors and integrating them into a clinical prediction score, such distinctions might also help to facilitate the conversations with patients/families given their risk of hydrocephalus after a posterior fossa lesion resection. Moreover, these predictors could be used for further studies concerning alternative neurosurgical management regarding hydrocephalus.
References
Abraham J, Chandy J (1963) Ventriculo-atrial shunt in the management of posterior-fossa tumours: preliminary report. J Neurosurg 20:252–253. https://doi.org/10.3171/jns.1963.20.3.0252
Albright L, Reigel DH (1977) Management of hydrocephalus secondary to posterior fossa tumors. J Neurosurg 46:52–55. https://doi.org/10.3171/jns.1977.46.1.0052
Beuriat P-A, Puget S, Cinalli G, Blauwblomme T, Beccaria K, Zerah M, Sainte-Rose C (2017) Hydrocephalus treatment in children: long-term outcome in 975 consecutive patients. J Neurosurg Pediatr 20:10–18. https://doi.org/10.3171/2017.2.PEDS16491
Bognár L, Borgulya G, Benke P, Madarassy G (2003) Analysis of CSF shunting procedure requirement in children with posterior fossa tumors. Childs Nerv Syst 19:332–336. https://doi.org/10.1007/s00381-003-0745-x
Böhm B, Mohadjer MHR (1978) Preoperative continuous measurements of ventricular pressure in hydrocephalus occlusus with tumors of the posterior fossa: the value of ventriculoauricular shunt. Adv Neurosurg 5:194–198
Bornhorst M, Frappaz D, Packer RJ (2016) Pilocytic astrocytomas. Handb Clin Neurol 134:329–344. https://doi.org/10.1016/B978-0-12-802997-8.00020-7
Bouras T, Sgouros S (2011) Complications of endoscopic third ventriculostomy. J Neurosurg Pediatr 7:643–649. https://doi.org/10.3171/2011.4.PEDS10503
Culley DJ, Berger MS, Shaw D, Geyer R (1994) An analysis of factors determining the need for ventriculoperitoneal shunts after posterior fossa tumor surgery in children. Neurosurgery 34:402–7-8
Epstein F, Murali R (1978) Pediatric posterior fossa tumors: hazards of the “preoperative” shunt. Neurosurgery 3:348–350
Foreman P, McClugage S, Naftel R, Griessenauer CJ, Ditty BJ, Agee BS, Riva-Cambrin J, Wellons J (2013) Validation and modification of a predictive model of postresection hydrocephalus in pediatric patients with posterior fossa tumors. J Neurosurg Pediatr 12:220–226. https://doi.org/10.3171/2013.5.PEDS1371
Hekmatpanah J (1989) Cerebellar tumors in children and their management. Semin Neurol 9:225–230. https://doi.org/10.1055/s-2008-1041329
Hoffman HJ, Hendrick EB, Humphreys RP (1976) Metastasis via ventriculoperitoneal shunt in patients with medulloblastoma. J Neurosurg 44:562–566. https://doi.org/10.3171/jns.1976.44.5.0562
Kessler LA, Dugan P, Concannon JP (1975) Systemic metastases of medulloblastoma promoted by shunting. Surg Neurol 3:147–152
Lam S, Harris DA, Lin Y, Rocque BG, Ham S, Pan I-W (2016) Outcomes of endoscopic third ventriculostomy in adults. J Clin Neurosci 31:166–171. https://doi.org/10.1016/j.jocn.2016.03.004
Lescher S, Schniewindt S, Jurcoane A, Senft C, Hattingen E (2014) Time window for postoperative reactive enhancement after resection of brain tumors: less than 72 hours. Neurosurg Focus 37:E3. https://doi.org/10.3171/2014.9.FOCUS14479
Lin C-T, Riva-Cambrin JK (2015) Management of posterior fossa tumors and hydrocephalus in children: a review. Childs Nerv Syst 31:1781–1789. https://doi.org/10.1007/s00381-015-2781-8
Marx S, El Damaty A, Manwaring J, El Refaee E, Fleck S, Fritsch M, Gaab MR, Schroeder HWS, Baldauf J (2018) Endoscopic third ventriculostomy before posterior fossa tumor surgery in adult patients. J Neurol Surg A Cent Eur Neurosurg 79:123–129. https://doi.org/10.1055/s-0037-1608786
Morelli D, Pirotte B, Lubansu A, Detemmerman D, Aeby A, Fricx C, Berré J, David P, Brotchi J (2005) Persistent hydrocephalus after early surgical management of posterior fossa tumors in children: is routine preoperative endoscopic third ventriculostomy justified? J Neurosurg 103:247–252. https://doi.org/10.3171/ped.2005.103.3.0247
Papo I, Caruselli G, Luongo A (1982) External ventricular drainage in the management of posterior fossa tumors in children and adolescents. Neurosurgery 10:13–15
Rappaport ZH, Shalit MN (1989) Perioperative external ventricular drainage in obstructive hydrocephalus secondary to infratentorial brain tumours. Acta Neurochir 96:118–121. https://doi.org/10.1007/BF01456169
Riva-Cambrin J, Detsky AS, Lamberti-Pasculli M, Sargent MA, Armstrong D, Moineddin R, Cochrane DD, Drake JM (2009) Predicting postresection hydrocephalus in pediatric patients with posterior fossa tumors. J Neurosurg Pediatr 3:378–385. https://doi.org/10.3171/2009.1.PEDS08298
Schmid UD, Seiler RW (1986) Management of obstructive hydrocephalus secondary to posterior fossa tumors by steroids and subcutaneous ventricular catheter reservoir. J Neurosurg 65:649–653. https://doi.org/10.3171/jns.1986.65.5.0649
Schneider C, Ramaswamy V, Kulkarni AV, Rutka JT, Remke M, Tabori U, Hawkins C, Bouffet E, Taylor MD (2015) Clinical implications of medulloblastoma subgroups: incidence of CSF diversion surgery. J Neurosurg Pediatr 15:236–242. https://doi.org/10.3171/2014.9.PEDS14280
Shalit MN, Ben Ari Y, Eynan N (1979) The management of obstructive hydrocephalus by the use of external continuous ventricular drainage. Acta Neurochir 47:161–172. https://doi.org/10.1007/BF01406401
Tamburrini G, Pettorini BL, Massimi L, Caldarelli M, Di Rocco C (2008) Endoscopic third ventriculostomy: the best option in the treatment of persistent hydrocephalus after posterior cranial fossa tumour removal? Childs Nerv Syst 24:1405–1412. https://doi.org/10.1007/s00381-008-0699-0
Taylor WA, Todd NV, Leighton SE (1992) CSF drainage in patients with posterior fossa tumours. Acta Neurochir 117:1–6. https://doi.org/10.1007/BF01400627
Won S-Y, Gessler F, Dubinski D, Eibach M, Behmanesh B, Herrmann E, Seifert V, Konczalla J, Tritt S, Senft C (2019) A novel grading system for the prediction of the need for cerebrospinal fluid drainage following posterior fossa tumor surgery. J Neurosurg 1–10. doi: https://doi.org/10.3171/2018.8.JNS181005
Yu Y-L, Lee M-S, Juan C-J, Hueng D-Y (2013) Calculating the tumor volume of acoustic neuromas: comparison of ABC/2 formula with planimetry method. Clin Neurol Neurosurg 115:1371–1374. https://doi.org/10.1016/j.clineuro.2012.12.029
Acknowledgments
We thank Marina Heibel and Anne Sicking for their excellent technical support.
Author information
Authors and Affiliations
Contributions
Sae-Yeon Won—study concept and design, acquisition of data, analysis and interpretation of data
Daniel Dubinski—study design, acquisition of data
Bedjan Behmanesh—acquisition of data, interpretation of data
Joshua D. Bernstock—interpretation of data, critical revision of manuscript for intellectual content
Volker Seifert—critical revision of manuscript for intellectual content, study supervision
Juergen Konczalla—study design, analysis and interpretation of data, critical revision of manuscript for intellectual content, study supervision
Stephanie Tritt—study design, analysis and interpretation of data, critical revision of manuscript for intellectual content, study supervision
Christian Senft—study design, analysis and interpretation of data, critical revision of manuscript for intellectual content
Florian Gessler—study design, analysis and interpretation of data, critical revision of manuscript for intellectual content
Corresponding author
Ethics declarations
Conflict of interest
Dr. Bernstock has positions/equity in both CITC Ltd. and Avidea Technologies.
Ethical approval
This study was approved by the author’s Institutional Review Board (IRB) and Committee on Ethics (EK213/15). No informed consent of patient was required for this study.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Won, SY., Dubinski, D., Behmanesh, B. et al. Management of hydrocephalus after resection of posterior fossa lesions in pediatric and adult patients—predictors for development of hydrocephalus. Neurosurg Rev 43, 1143–1150 (2020). https://doi.org/10.1007/s10143-019-01139-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10143-019-01139-8