Abstract
The scarce antifungal arsenal, changes in the susceptibility profile of fungal agents, and lack of adherence to treatment have contributed to the increase of cases of dermatomycoses. In this context, new antimicrobial substances have gained importance. Chalcones are precursors of the flavonoid family that have multiple biological activities, have high tolerability by humans, and easy synthesis. In this study, we evaluated the in vitro antifungal activity, alone and in combination with conventional antifungal drugs, of the VS02–4′ethyl chalcone-derived compound against dermatophytes and Candida spp. Susceptibility testing was carried out by broth microdilution. Experiments for determination of the target of the compound on the fungal cell, time-kill kinetics, and toxicity tests in Galleria mellonella model were also performed. Combinatory effects were evaluated by the checkerboard method. Results showed high activity of the compound VS02–4′ethyl against dermatophytes (MIC of 7.81–31.25 μg/ml). The compound targeted the cell membrane, and the time-kill test showed the compound continues to exert gradual activity after 5 days on dermatophytes, but no significant activity on Candida. Low toxicity was observed at 250 mg/kg. Excellent results were observed in the combinatory test, where VS02–4′ethyl showed synergistic interactions with itraconazole, fluconazole, terbinafine, and griseofulvin, against all isolates tested. Although further investigation is needed, these results revealed the great potential of chalcone-derived compounds against fungal infections for which treatments are long and laborious.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Dermatomycoses affect 20–25% of the world population (Baghi et al. 2016; Zhan and Liu 2017; Appelt et al. 2021). They are caused by fungi that can invade the stratum corneum the skin, the intrafollicular keratinized portion of the hair, or nail plate (Corralo et al. 2014). The main etiological agents are dermatophyte fungi, especially Trichophyton rubrum, T. mentagrophytes, Epidermophyton floccosum, and Microsporum canis; and Candida spp. (Monod and Méhul 2019; Sylla et al. 2019). The scarce antifungal arsenal and change in the susceptibility profile of the etiological agents have contributed to the perpetuation of these mycoses in the population. Furthermore, patients often fail to adhere to long-term treatments (Gupta and Stec 2019; Lindsø Andersen et al. 2020; Gupta et al. 2021).
In the search of new antimicrobial molecules, plant metabolites are being increasingly studied due to their beneficial biological properties (Dos Santos Ramos et al. 2016). In this context, chalcones, precursors of the flavonoid family, have great potential for exploration. They can interact with multiple biological targets, have high tolerability by humans, and the synthesis of its derivatives is simple (León-González et al. 2015). It has been reported many chemotherapeutic activities, including anticancer (Letafat et al. 2013; Ketabforoosh et al. 2014), antibacterial (Nowakowska 2007; Mahapatra et al. 2015; Marques et al. 2020), antiviral (Duran et al. 2021; Mothana et al. 2022; Valipour 2022; Nematollahi et al. 2023), antiparasitic (González et al. 2020; Nematollahi et al. 2023), and antifungal (Wang et al. 2016; Marques et al. 2020; Mirzaei et al. 2020; Gładkowski et al. 2023).
Currently, the main challenge in treating infectious diseases is the development of drug-resistant microorganisms. This resistance can emerge due to mutations, genetic changes, and phenotypic modifications. As a result, treatments that were once effective may no longer work, leading to unsuccessful disease management, a higher risk of transmission, and increased mortality rates. Therefore, developing new antimicrobial drugs is essential (Dhingra et al. 2020). Researchers are increasingly focusing on chalcones due to their proven antimicrobial properties against viruses, bacteria, fungi, and protozoa (Nematollahi et al. 2023).
Combining natural compounds, particularly chalcones, with antimicrobial drugs holds significant promise for improving the treatment of infectious diseases. By combining chalcones with existing antimicrobial drugs, it is possible to enhance the efficacy of treatments, especially in cases of resistance (Pereira et al. 2022; Chai et al. 2023). This synergy between traditional medicines and natural compounds, such as chalcones, carvacrol, gallic acid, epigallocatechin gallate, and essential oils, has already been reported in studies, reinforcing not only the expansion of the spectrum of antimicrobial activity but also opening the door to more effective therapeutic strategies for combating infectious diseases (Ayaz et al. 2019; Hellewell and Bhakta 2020; Brescini et al. 2021; Dos Santos et al. 2023; Sun et al. 2023).
In this study, we report the activity of a chalcone-derived compound, including determination of the target on the fungal cell, time-kill and toxicity analyses, and synergistic activity with conventional antifungals, against dermatophytes and Candida spp.
Material and methods
Fungal isolates
The list of clinical isolates and reference strains used in this study is in Table 1. In accordance with the Brazilian regulation, the isolates are registered in the SisGen (National System for the Management of Genetic Heritage and Associated Traditional Knowledge) – protocol number A2B1006.
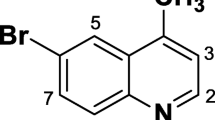
Synthesis of the compound
The chalcone-derived compound was provided by the Laboratory of Antibiotics and Chemotherapy (LAQ) at the São Paulo State University (Unesp), Campus São José do Rio Preto, Brazil. It was synthesized by Claisen–Schmidt aldol condensation reaction (Dos Santos et al. 2017, 2019). The components (aminoacetophenones and aldehydes) were dissolved in ethanol, and sodium hydroxide in ethanol was added as catalyst solution. The reaction product was kept under stirring for 2–6 h at RT and then poured into ice and filtered or extracted with ethyl acetate. The organic phases were combined and washed with aqueous NaHSO solution and dried over MgSO4. Filtration occurred under reduced pressure. After chromatographic separation and purification, the chalcone compounds were obtained in a yield of around 40%. Characterization of compounds included determination of melting points, structure, and spectral analyses. The compound used in this study was the VS02–4′ethyl, where an ethyl group was inserted at the fourth carbon position of the first aromatic ring (Fig. 1). For the in vitro assays, the compound was solubilized in 10% DMSO (LabSynth®).
Antifungal susceptibility testing
The susceptibility profiles of the fungal isolates against the VS02–4′ethyl chalcone compound and conventional antifungal drugs (itraconazole, fluconazole, terbinafine, griseofulvin—[Sigma-Aldrich®]) were determined by broth microdilution, according to protocols M38-3rd ed (CLSI 2017) and M27-3rd ed (CLSI 2008) of the Clinical Laboratory Standard Institute.
In 96-wells plates, the VS02–4′ethyl was serially diluted in RPMI–1640 medium (Rosen Park Media Institute—Sigma-Aldrich®). For dermatophytes, final testing concentrations ranged from 250 to 0.48 µg/ml. For yeast, the concentrations ranged from 1000 to 1.95 µg/ml. Similarly, the antifungals were diluted to reach the following concentrations: 256–0.5 µg/ml, for fluconazole; 8–0.015 µg/ml, for terbinafine; and 16–0.03 µg/ml, for itraconazole and griseofulvin. Griseofulvin was only tested against dermatophytes.
Dermatophytes were cultured in Potato-dextrose agar (Oxoid ®) for 7 days, at 35 °C, and yeast in Sabouraud-dextrose agar (SDA, Oxoid ®) for 24 h, at 37 °C. The inocula were prepared in 0.9% sterile saline solution to reach final concentrations of 0.4 to 5 × 104 CFU/ml, for dermatophytes, and 0.5 to 2.5 × 103 CFU/ml, for yeast.
After inoculation, the plates were incubated at 35 °C and visual readings were carried out after 120 h, for dermatophytes, and 48 h, for yeast. Minimum inhibitory concentrations (MIC) were determined as the lowest concentration capable of inhibiting 80% of fungal growth, for fluconazole and itraconazole, and 100% of fungal growth, for griseofulvin, terbinafine, and the VS02–4′ethyl compound.
Minimum fungicidal concentrations (MFC) were determined by subculturing an aliquot from each well into agar plates, and it was considered as the lowest concentration capable of inhibiting fungal growth in the culture medium.
Sterility, growth, and solvent controls were added to each test. Tests were performed in triplicate.
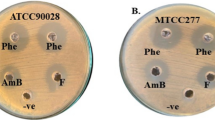
Sorbitol and ergosterol assays
In addition to the compound susceptibility testing, experiments were performed with two different supplemented RPMI–1640 to determine where the VS02–4′ethyl will target on the fungal cell. The first supplement to the RPMI–1640 medium was 0.8 M sorbitol (Sigma-Aldrich®) (De Castro et al. 2015). Sorbitol acts as an osmoprotector that allows cells to grow in the presence of an inhibitor of a fungal cell wall synthesis (Svetaz et al. 2007). Consequently, increases in MIC values indicates that the compound targets the cell wall. The other supplement was the ergosterol (Sigma-Aldrich®) at 400 μg/ml (De Castro et al. 2015). If the compound activity is due to ergosterol binding, providing exogenous ergosterol would prevent binding to ergosterol of the fungal membrane, what would increase MIC values (Escalante et al. 2008).
The fungal isolates TRCBS, TMATCC, MCATCC, EF6069, CGATCC, and CAUCBS were selected for these assays. Values of MIC were compared with and without sorbitol and ergosterol supplementation.
As controls, these isolates were tested against caspofungin (Sigma-Aldrich®) and amphotericin B (Sigma-Aldrich®) (at final concentration of 16 to 0.03 µg/ml) with RPMI–1640 without and with supplementation with sorbitol and ergosterol, respectively. Sterility, growth, and solvent controls were added to each test. Tests were performed in triplicate.
Time-kill analysis
Time-kill analysis were carried out according to Klepser et al. (1998). The isolates used in this experiment were TRCBS, TMATCC, MCATCC, EF6069, CGATCC, and CAUCBS. Fungal inocula were prepared as previously described and diluted 1:1 with VS02–4′ethyl. For dermatophytes, two concentrations of the compound were tested, 500 μg/ml and 62.5 μg/ml. For Candida spp., the concentration of the compound was 4000 μg/ml. Controls included 10% DMSO solution, without the compound.
At predetermined times (initial moment—0 h, 8 h, 24 h, 48 h, and 120 h), an aliquot of 30 μl was inoculated on SDA plates with a Drigalski spatula. After 120 h, for dermatophytes, and 48 h, for yeasts, at 35 °C, the colonies were counted, and the results adjusted to Log10 CFU/ml.
Toxicity analysis
The toxicity of the VS02–4′ethyl compound was determined by an experimental model of Galleria mellonella larvae, according to Ignasiak and Maxwell (2017). The G. mellonella in vitro model has the advantage of the fact that this insect immune system is functionally and structurally similar to the innate immune system of mammals, along with the low cost of the technique and the fast of insect reproduction (Browne et al. 2013; Ignasiak and Maxwell 2017). The compound was tested at the following concentrations: 125 μg/ml, 250 μg/ml, 500 μg/ml, 1000 μg/ml, and 2000 μg/ml). For each experiment, five groups of five larvae at the sixth stage of development (250 ± 25 mg) were inoculated with compound. Five microliters were injected into the last right proleg of the larvae using a 10 μl Hamilton model 7000.5KH micro syringe. As controls, it was used untouched larvae (naïve), larvae inoculated with 99.9% ethanol (mortality control), sterile water (negative toxicity control), and 60% DMSO.
The larvae were incubated at 37 °C, deprived of food and direct lighting. Larvae survival assessments were carried out every 24 h for 5 days and pre-pupal formations were removed daily to delay their metamorphosis. Survival analysis was performed using the log-rank (Mantel-Cox) test. GraphPad Prism® software version 9.3.0 for Windows (San Diego, California, USA) was used for statistical analysis.
Checkerboard assay
The combinatorial effect between the chalcone-derived compound and conventional antifungal drugs was evaluated using the checkerboard method (CLSI 2008; Lemes et al. 2023).
In 96-wells plates, the VS02–4′ethyl was combined with each antifungal. In the assays against dermatophytes, the chalcone-derived compound concentration ranged from 125 to 0.12 μg/ml, and, for Candida spp., ranged from 1000 to 0.97 μg/ml. The antifungal drugs varied from 128 to 0.5 μg/ml, for fluconazole; 16 to 0.03, for itraconazole; 64 to 0.007 μg/ml, for terbinafine; and 4 to 0.06 μg/ml, for griseofulvin. Griseofulvin was only tested against dermatophytes.
The isolates TRCBS, TR7984, CGATCC, and CAUCBS were used in this assay. The inocula were prepared as previously described. Inoculation, incubation, and readings were also performed as previously described.
To evaluate the interaction between the compound and the drugs, the fractional inhibitory concentration (FIC) index was calculated, following the classification by Kumar et al. (2012), where FIC ≤ 0.5 means synergistic interaction; 0.5 < FIC ≤ 1 means additive action; 1 < FIC ≤ 2 means indifferent interaction; and FIC > 2 means antagonistic interaction.
Results
Antifungal activity of VS02–4′ethyl
The chalcone-derived compound showed high activity against dermatophytes, with MIC ranging from 7.81 to 31.25 μg/ml, and geometric mean (GM) of 14.74 μg/ml. For Candida spp., MIC values ranged from 500 to 1000 μg/ml and GM of 840.90 μg/ml. Regarding MFC, values varied between 31.25 and > 250 μg/ml, for dermatophytes, and 1000 and > 1000 μg/ml, for Candida spp. (Table 2).
Regarding the antifungal drugs, terbinafine showed the most potent activity against dermatophytes (Table 2), followed by itraconazole and griseofulvin. Fluconazole showed the least activity. Against Candida isolates, only itraconazole exhibited high activity. Detailed results are shown in Table 2.
Sorbitol and ergosterol assays
Comparing of the experiments with and without supplementation, it was observed that the presence of sorbitol did not alter the MIC values. However, the presence of exogenous ergosterol in the tests caused the MIC values to increase up to 8 times (from 31.25 to 250 μg/ml) (Table 3). That indicates that the VS02–4′ethyl targets the cell membrane of fungi.
Time-kill analysis
Data obtained in the time-kill experiments can be seen on Fig. 2. For dermatophytes, results show that the compound caused a mean of 1.12-log reduction of viability, at 500 µg/ml, and 0.92-log reduction, at 62.5 µg/ml, after 5 days. The figure shows that the decrease was gradual over time, until the end of the analysis. Contrarily, the analyses evidenced that the compound does not have high activity against the Candida isolates tested, since no reduction could be observed after 5 days, even at a higher concentration of the compound (4.000 µg/ml) (Fig. 2).
Toxicity analysis
The tests with VS02–4′ethyl concentration of 125 and 250 mg/kg showed low toxicity, with survival rates of 60% of the G. mellonella larvae, after 5 days. At 500 mg/kg, 40% of the larvae survived after 5 days. Concentrations of 1000 and 2000 mg/kg of VS02–4′ethyl killed all larvae after three and 4 days, respectively (Fig. 3).
Checkerboard assay
When combined, all tests showed MIC reduction of the antifungal drugs and the VS02–4′ethyl compound. Values of FICI index varied from 0.1 to 0.5, all in the range of synergistic combinatory effect (Table 4).
Discussion
In this study, we report the antifungal activity of the chalcone-derived compound VS02–4′ethyl against the main etiological agents of dermatomycoses. Chalcones are among the main secondary metabolites of edible plants. Most chalcones are polyhydroxylated aromatic compounds and bioprecursors of open-chain flavonoids and isoflavonoids (Rudrapal et al. 2021). They can be obtained from natural or synthetic sources, which can form different derivative compounds from their main structure (Mirzaei et al. 2020). Modification of the structure of chalcones enhances their biological activity, reduces toxicity, and increases their pharmacological effects (Nawaz et al. 2023).
Some of the well-known natural chalcone containing drugs are Butein (anticancer and anti-inflammation), Xanthohumol (antibacterial and anti-HIV agent), Isoliquiritigenin (anti-cancer, chemoprotective, anti-inflammatory and antioxidant), Cardamonin (ATP diphosphohydrolase), licochalcone (anti-inflammatory, anti-cancer), Metochalcone (choleretic agent), and Sofalcone (anti-ulcer agent) (Narwal et al. 2024). Due to the presence of phenolic groups and their property of scavenging radicals, plant extracts rich in chalcones have been extensively studied in the search for new therapeutic compounds (Ouyang et al. 2021).
Regarding their antimicrobial activity, it has been reported that chalcones and other flavonoids are lipophilic, which may lead to disruption of the cell membrane and leakage of nucleic acids (Thebti et al. 2023), which corroborates the data obtained in the ergosterol experiment of this study. Additionally, the activity of a chalcone-derived compounds may result from the downregulation of genes encoding virulence factors, such as isocitrate lyase, citrate synthase and malate synthase (Cantelli et al. 2017), efflux pumps (Komoto et al. 2015; Nematollahi et al. 2023), and inhibition of fatty acid synthesis (Nematollahi et al. 2023). However, chalcones may act differently depending on the fungal species or genera (Lahtchev et al. 2008; Mellado et al. 2020; Morão et al. 2020).
The VS02–4′ethyl compound showed higher activity against dermatophytes when compared to Candida isolates, with MIC ranging from 7.81 to 31.25 μg/ml for filamentous fungi, versus MIC values ranged from 500 to 1000 μg/ml for yeast (Table 2). A previous study showed that yeast’s intracellular glutathione and cysteine molecules act as defense barriers against chalcones (Lahtchev et al. 2008). These proteins are related to vitality, cellular development, and pathogenesis (Wangsanut and Pongpom 2022). In a metabolomic study by Ciesielska et al. (2021), the authors report that, during keratin degradation by dermatophytes, cysteine levels increased but glutathione molecules were not detected in the experiment. This glutathione deficiency may help elucidate why the VS02–4′ethyl presented higher activity against dermatophytes.
It is crucial the discovery and development of new treatments for dermatomycoses because of their great incidence worldwide. Moreover, treatment failure and antifungal resistance are being increasingly reported (Gupta and Venkataraman 2022). Antifungal resistance is often related to mutations that modifies the target of the drug or regulation of efflux pumps (Ksiezopolska and Gabaldón 2018) and can be associated to long term use. A 2-year study demonstrated that excessive use of fluconazole promoted resistance in Candida species, with approximately 98% of the C. albicans isolates, 93% of C. parapsilosis, 91% of C. tropicalis, and 68% of C. glabrata resistant to fluconazole (Beardsley et al. 2018). Candida auris, although is not a common agent of superficial mycoses, colonizes the skin and it was included in this study due to the high incidence of resistance to multiple classes of antifungals and growing concern about outbreaks (Spivak and Hanson 2018).
Regarding dermatophytes, it is estimated that 19% of infections are caused by azole-resistant strains (Ghannoum 2016). Although resistance to azoles is more likely, resistance to terbinafine has also been reported in Microsporum spp. and Trichophyton spp., and is associated with mutations in genes encoding the enzyme squalene epoxidase (Lindsø Andersen et al. 2020; Gupta et al. 2021). Failures in treatment may still be associated with insufficient dose and duration regimes, in addition to low patient adherence (Gupta and Venkataraman 2022).
In this study, we highlight the antifungal activity of the VS02–4′ethyl chalcone-derived compound in association with the conventional antifungal drugs (Table 4). Synergistic interaction occurred in all experiments (FIC values less than or equal to 0.5), causing a significant decrease of MIC values for both antifungal, with reductions of up to five-fold in MIC value, and the compound itself, with reductions of up to ten-fold. This may be incredibly beneficial, especially against C. glabrata and C. auris, which presented elevated MIC values for the compound and the antifungals alone.
The best performance of the compound was observed against the C. glabrata strain in synergistic action with itraconazole. Individually, the MIC value of the compound was 1000 µg/mL, while that of itraconazole was 16 µg/mL. However, when combined, there was a significant reduction in the MIC values to 0.97 and 2 µg/mL, respectively. Considering the high resistance rates of C. glabrata to itraconazole and other azoles (Kaan et al. 2021; Frías-De-León et al. 2021; Dunaiski et al. 2024), these results indicate a potent synergistic interaction of the compound VS02–4′ethyl, which enhances the action of itraconazole, providing a promising approach for the treatment of resistant infections.
Synergistic interactions can improve drug pharmacokinetics, slow down their metabolism and elimination by the body, and decrease toxicity effects (Ahmad et al. 2017). Different possible mechanisms for synergy activities have already been proposed: one compound may act alone and the second bind to the target, facilitating the binding of the first compound; two compounds may reach different locations or biological pathways and exert a collective effect; or two compounds can act on the same biological pathway at two different stages, increasing activity (Ahmad et al. 2017; Spitzer et al. 2017).
Synergistic interactions between chalcone-derived compounds and fluconazole have already been reported. Ahmad et al. (2017) investigation indicated that the chalcone–fluconazole interaction reversed fluconazole resistance causing a downregulation of the ERG11 gene, which is important in the ergosterol biosynthesis pathway and is crucial for fluconazole resistance. Nonetheless, this may not be the only mode of action, since the VS02–4′ethyl also showed synergy with griseofulvin, which acts in the process of fungal mitosis by interacting with microtubules, disrupting the mitotic spindle (Yesudian et al. 2021). Unfortunately, most data available on the interaction of antifungal drugs and chalcone-derived compounds reference fluconazole.
In conclusion, the main finding of this study was the highly synergistic activity of VS02–4′ethyl chalcone-derived compound with conventional antifungal drugs against dermatophytes and Candida spp. The VS02–4′ethyl in concentration equal to or less than 250 mg/kg showed low toxicity, study report that some chalcones can be toxic at high concentrations, leading to cytotoxicity, genotoxicity, and other harmful effects. However, chalcones are generally considered safe at lower doses (Jesus et al. 2022). Further investigations are needed to elucidate the mode of action and the synergistic interaction of the VS02–4′ethyl with the different classes of antifungals. In addition, further studies should reveal the best administration route and the in vivo effects of the compound. Nevertheless, these results revealed the great potential of chalcone-derived compounds against fungal infections for which treatments are long and laborious.
Data availability
No datasets were generated or analysed during the current study.
References
Ahmad A, Wani MY, Patel M, Sobral AJFN, Duse AG, Aqlan FM, Al-Bogami AS (2017) Synergistic antifungal effect of cyclized chalcone derivatives and fluconazole against Candida albicans. Medchemcomm 8:2195–2207. https://doi.org/10.1039/c7md00440k
Appelt L, Nenoff P, Uhrlaß S, Krüger C, Kühn P, Eichhorn K, Buder S, Beissert S, Abraham S, Aschoff R, Bauer A (2021) Terbinafin-resistente Dermatophytosen und Onychomykose durch Trichophyton rubrum [Terbinafine-resistant dermatophytoses and onychomycosis due to Trichophyton rubrum]. Hautarzt 72:868–877. https://doi.org/10.1007/s00105-021-04879-1
Ayaz M, Ullah F, Sadiq A, Ullah F, Ovais M, Ahmed J, Devkota HP (2019) Synergistic interactions of phytochemicals with antimicrobial agents: potential strategy to counteract drug resistance. Interactions 308:294–303. https://doi.org/10.1016/j.cbi.2019.05.050
Baghi N, Shokohi T, Badali H, Makimura K, Rezaei-Matehkolaei A, Abdollahi M, Didehdar M, Haghani I, Abastabar M (2016) In vitro activity of new azoles luliconazole and lanoconazole compared with ten other antifungal drugs against clinical dermatophyte isolates. Med Mycol 54(7):757–763. https://doi.org/10.1093/mmy/myw016
Beardsley J, Halliday CL, Chen SC, Sorrell TC (2018). Responding to the emergence of antifungal drug resistance: perspectives from the bench and the bedside. Future Microbiol 13(10). https://doi.org/10.2217/fmb-2018-0059
Brescini L, Fioriti S, Morroni G, Barchiesi F (2021) Antifungal combinations in dermatophytes. J Fungi 7(9):727. https://doi.org/10.3390/jof7090727. (Basel)
Browne N, Heelan M, Kavanagh K (2013) An analysis of the structural and functional similarities of insect hemocytes and mammalian phagocytes. Virulence 4(7):597–603. https://doi.org/10.4161/viru.25906
Cantelli BAM, Bitencourt TA, Komoto TT, Beleboni RO, Marins M, Fachin AL (2017) Caffeic acid and licochalcone A interfere with the glyoxylate cycle of Trichophyton rubrum. Biomed Pharmacother 16:1389–1394. https://doi.org/10.1016/j.biopha.2017.11.051
Chai N, Sun A, Zhu X, Li Y, Wang R, Zhang Y, Mao Z (2023) Antifungal evaluation of quinoline-chalcone derivatives combined with FLC against drug-resistant Candida albicans. Bioorg Med Chem Lett 86:129242. https://doi.org/10.1016/j.bmcl.2023.129242
Ciesielska A, Kawa A, Kanarek K, Soboń A, Szewczyk R (2021). Metabolomic analysis of Trichophyton rubrum and Microsporum canis during keratin degradation. Sci Rep 11(3959). https://doi.org/10.1038/s41598-021-83632-z
CLSI (2008) Reference Method for Broth Dilution Antifungal Susceptibility Testing of Yeasts, 3rd edn CLSI standard M27-3rd. Clin Lab Stand Inst, Wayne, PA
CLSI (2017) Reference method for broth dilution antifungal susceptibility testing of filamentous fungi, 3rd edn. CLSI standard M38-3rd. Clin Lab Stand Inst, Wayne, PA
Corralo DS, Heras-Alonso ME, Acebes LO (2014) Infecciones cutáneas. Medicine 11(47):2755–2763. https://doi.org/10.1016/S0304-5412(14)70694-8
De Castro RD, de Souza TM, Bezerra LM, Ferreira GL, Costa EM, Cavalcanti AL (2015) Antifungal activity and mode of action of thymol and its synergism with nystatin against Candida species involved with infections in the oral cavity: an in vitro study. BMC Complement Altern Med 15(417). https://doi.org/10.1186/s12906-015-0947-2
Dhingra S, Rahman NAA, Peile E, Rahman M, Sartelli M, Hassali MA, Islam T, Islam S, Haque M (2020) Microbial resistance movements: an overview of global public health threats posed by antimicrobial resistance, and how best to counter. Front Public Health 8:535668. https://doi.org/10.3389/fpubh.2020.535668
Dos Santos MB, Pinhanelli VC, Garcia MAR, Silva G, Baek SJ, França SC, Fachin AL, Marins M, Regasini LO (2017) Antiproliferative and pro-apoptotic activities of 2′- and 4′-aminochalcones against tumor canine cells. Eur J Med Chem 29(138):884–889. https://doi.org/10.1016/j.ejmech.2017.06.049
Dos Santos MB, Bertholin Anselmo D, de Oliveira JG, Jardim-Perassi BV, Alves Monteiro D, Silva G, Gomes E, Lucia Fachin A, Marins M, de Campos Zuccari DAP, Octavio Regasini L (2019) Antiproliferative activity and p53 upregulation effects of chalcones on human breast cancer cells. J Enzyme Inhib Med Chem 34(1):1093–1099. https://doi.org/10.1080/14756366.2019.1615485
Dos Santos ATL, de Araújo-Neto JB, Costa da Silva MM, Paulino da Silva ME, Carneiro JNP, Fonseca VJA, Coutinho HDM, Bandeira PN, Dos Santos HS, da Silva Mendes FR, Sales DL, Morais-Braga MFB (2023) Synthesis of chalcones and their antimicrobial and drug potentiating activities. Microb Pathog 180:106129. https://doi.org/10.1016/j.micpath.2023.106129
Dos Santos Ramos MA, de Toledo LG, Calixto GM, Bonifácio BV, de Freitas Araújo MG, Dos Santos LC, de Almeida MT, Chorilli M, Bauab TM (2016) Syngonanthus nitens Bong. (Rhul.)-loaded nanostructured system for vulvovaginal candidiasis treatment. Int J Mol Sci 17(8):1368. https://doi.org/10.3390/ijms17081368
Dunaiski CM, Kock MM, Chan WY, Ismail A, Peters RPH (2024) Molecular epidemiology and antimicrobial resistance of vaginal Candida glabrata isolates in Namibia. Med Mycol 62(2):myae009. https://doi.org/10.1093/mmy/myae009
Duran N, Polat MF, Aktas DA, Alagoz MA, Ay E, Cimen F, Tek E, Anil B, Burmaoglu S, Algul O (2021) New chalcone derivatives as effective against SARS-CoV-2 agent. Int J Clin Pract 75(12):e14846. https://doi.org/10.1111/ijcp.14846
Escalante A, Gattuso M, Pérez P, Zacchino S (2008) Evidence for the mechanism of action of the antifungal phytolaccoside B isolated from Phytolacca tetramera Hauman. J Nat Prod 71(10):1720–1725. https://doi.org/10.1021/np070660i
Frías-De-León MG, Hernández-Castro R, Conde-Cuevas E, García-Coronel IH, Vázquez-Aceituno VA, Soriano-Ursúa MA, Farfán-García ED, Ocharán-Hernández E, Rodríguez-Cerdeira C, Arenas R, Robledo-Cayetano M, Ramírez-Lozada T, Meza-Meneses P, Pinto-Almazán R, Martínez-Herrera E (2021) Candida glabrata antifungal resistance and virulence factors, a perfect pathogenic combination. Pharmaceutics 13:1529. https://doi.org/10.3390/pharmaceutics13101529
Ghannoum M (2016) Azole resistance in dermatophytes: prevalence and mechanism of action. J Am Podiatr Med Assoc 106(1):79–86. https://doi.org/10.7547/14-109
Gładkowski W, Siepka M, Żarowska B, Białońska A, Gawdzik B, Urbaniak M, Wawrzeńczyk C (2023) Chalcone-derived lactones: synthesis, whole-cell biotransformation, and evaluation of their antibacterial and antifungal activity. Molecules 28(9):3800. https://doi.org/10.3390/molecules28093800
Gupta AK, Stec N (2019) Recent advances in therapies for onychomycosis and its management. F1000Res 8(F1000 Faculty Rev):968. https://doi.org/10.12688/f1000research.18646.1
Gupta AK, Venkataraman M (2022) Antifungal resistance in superficial mycoses. J Dermatolog Treat 33(4):1888–1895. https://doi.org/10.1080/09546634.2021.1942421
Gupta AK, Renaud HJ, Quinlan EM, Shear NH, Piguet V (2021) The growing problem of antifungal resistance in onychomycosis and other superficial mycoses. Am J Clin Dermatol 22:149–157. https://doi.org/10.1007/s40257-020-00580-6
Hellewell L, Bhakta S (2020) Chalcones, stilbenes and ketones have anti-infective properties via inhibition of bacterial drug-efflux and consequential synergism with antimicrobial agents. Access Microbiol 2(4):acmi000105. https://doi.org/10.1099/acmi.0.000105
Ignasiak K, Maxwell A (2017) Galleria mellonella (greater wax moth) larvae as a model for antibiotic susceptibility testing and acute toxicity trials. BMC Res Notes 10(428). https://doi.org/10.1186/s13104-017-2757-8
Jesus A, Durães F, Szemerédi N, Freitas-Silva J, da Costa PM, Pinto E, Pinto M, Spengler G, Sousa E, Cidade H (2022) BDDE-inspired chalcone derivatives to fight bacterial and fungal infections. Mar Drugs 20(5):315. https://doi.org/10.3390/md20050315
Kaan Ö, Koç AN, Atalay MA, Mutlu Sarigüzel F (2021) Molecular epidemiology, antifungal susceptibility and virulence factors of Candida glabrata complex strains in Kayseri/Turkey. Microb Pathog 154:104870. https://doi.org/10.1016/j.micpath.2021.104870
Ketabforoosh SH, Kheirollahi A, Safavi M, Esmati N, Ardestani SK, Emami S, Firoozpour L, Shafiee A, Foroumadi A (2014) Synthesis and anti-cancer activity evaluation of new dimethoxylated chalcone and flavanone analogs. Arch Pharm 347(11):853–860. https://doi.org/10.1002/ardp.201400215. (Weinheim)
Klepser ME, Ernst EJ, Lewis RE, Ernst ME, Pfaller MA (1998) Influence of test conditions on antifungal time-kill curve results: proposal for standardized methods. Antimicrob Agents Chemother 42(5). https://doi.org/10.1128/AAC.42.5.1207
Komoto TT, Bitencourt TA, Silva G, Beleboni RO, Marins M, Fachin AL (2015) Gene expression response of Trichophyton rubrum during coculture on keratinocytes exposed to antifungal agents. Evid Based Complement Alternat Med 2015:180535. https://doi.org/10.1155/2015/180535
Ksiezopolska E, Gabaldón T (2018) Evolutionary emergence of drug resistance in Candida opportunistic pathogens. Genes 9(9):461. https://doi.org/10.3390/genes9090461. (Basel)
Kumar SN, Siji JV, Nambisan B, Mohandas C (2012) Activity and synergistic interactions of stilbenes and antibiotic combinations against bacteria in vitro. World J Microbiol Biotechnol 28(11):3143–3150. https://doi.org/10.1007/s11274-012-1124-0
Lahtchev KL, Batovska DI, Parushev SP, Ubiyvovk VM, Sibirny AA (2008) Antifungal activity of chalcones: a mechanistic study using various yeast strains. Eur J Med Chem 43(10):2220–2228. https://doi.org/10.1016/j.ejmech.2007.12.027
Lemes TH, Nascentes JAS, Regasini LO, Siqueira JPZ, Maschio-Lima T, Pattini VC, Ribeiro MD, de Almeida BG, de Almeida MTG (2023) Combinatorial effect of fluconazole, itraconazole, and terbinafine with different culture extracts of Candida parapsilosis and Trichophyton spp. against Trichophyton rubrum. Int Microbiol https://doi.org/10.1007/s10123-023-00438-x
León-González AJ, Acero N, Muñoz-Mingarro D, Navarro I, Martín-Cordero C (2015) Chalcones as promising lead compounds on cancer therapy. Curr Med Chem 22(30):3407–3425. https://doi.org/10.2174/0929867322666150729114829
Letafat B, Shakeri R, Emami S, Noushini S, Mohammadhosseini N, Shirkavand N, Kabudanian Ardestani S, Safavi M, Samadizadeh M, Letafat A, Sha Ee A, Foroumadi A (2013) Synthesis and in vitro cytotoxic activity of novel chalcone-like agents. Iran J Basic Med Sci 16(11):1155–1162
Lindsø Andersen P, Jemec GB, Saunte DML (2020) Treatment adherence and psychosocial impact of tinea capitis in families: qualitative pilot study. Dermatol Ther 33(4):e13570. https://doi.org/10.1111/dth.13570
Mahapatra DK, Bharti SK, Asati V (2015) Chalcone scaffolds as anti-infective agents: structural and molecular target perspectives. Eur J Med Chem 101:496–524. https://doi.org/10.1016/j.ejmech.2015.06.052
Marques BC, Santos MB, Anselmo DB, Monteiro DA, Gomes E, Saiki MFC, Rahal P, Rosalen PL, Sardi JCO, Regasini LO (2020) Methoxychalcones: effect of methoxyl group on the antifungal, antibacterial and antiproliferative activities. Med Chem 16(7):881–891. https://doi.org/10.2174/1573406415666190724145158
Mellado M, Espinoza L, Madrid A, Mella J, Chávez-Weisser E, Diaz K, Cuellar M (2020) Design, synthesis, antifungal activity, and structure-activity relationship studies of chalcones and hybrid dihydrochromane-chalcones. Mol Divers 24:603–615. https://doi.org/10.1007/s11030-019-09967-y
Mirzaei H, Abastabar M, Emami S (2020) Indole-derived chalcones as anti-dermatophyte agents: in vitro evaluation and in silico study. Comput Biol Chem 84:107189. https://doi.org/10.1016/j.compbiolchem.2019.107189
Monod M, Méhul B (2019). Recent findings in onychomycosis and their application for appropriate treatment. J Fungi 5(1). https://doi.org/10.3390/jof5010020. (Basel)
Morão LG, Lorenzoni ASG, Chakraborty P, Ayusso GM, Cavalca LB, Santos MB, Marques BC, Dilarri G, Zamuner C, Regasini LO, Ferreira H, Scheffers DJ (2020) Investigating the modes of action of the antimicrobial chalcones BC1 and T9A. Molecules 25(20):4596. https://doi.org/10.3390/molecules25204596
Mothana RA, Arbab AH, ElGamal AA, Parvez MK, Al-Dosari MS (2022) Isolation and characterization of two chalcone derivatives with anti-hepatitis B virus activity from the endemic Socotraen Dracaena cinnabari (dragon’s blood tree). Molecules 27(3):952. https://doi.org/10.3390/molecules27030952
Narwal S, Devi B, Dhanda T, Kumar S, Tahlan S (2024) Exploring chalcone derivatives: synthesis and their therapeutic potential. J Mol Struct 1303:37554. https://doi.org/10.1016/j.molstruc.2024.137554
Nawaz T, Tajammal A, Qurashi AW (2023) Chalcones as broad-spectrum antimicrobial agents: a comprehensive review and analysis of their antimicrobial activities. ChemistrySelect 8(45):e202302798. https://doi.org/10.1002/slct.202302798
Nematollahi MH, Mehrabani M, Hozhabri Y, Mirtajaddini M, Iravani S (2023) Antiviral and antimicrobial applications of chalcones and their derivatives: from nature to greener synthesis. Heliyon 9(10):e20428. https://doi.org/10.1016/j.heliyon.2023.e20428
Nowakowska Z (2007) A review of anti-infective and anti-inflammatory chalcones. Eur J Med Chem 42(2):125–137. https://doi.org/10.1016/j.ejmech.2006.09.019
Ouyang Y, Li J, Chen X, Fu X, Sun S, Wu Q (2021) Chalcone derivatives: role in anticancer therapy. Biomolecules 11(6):894. https://doi.org/10.3390/biom11060894
Pereira D, Durães F, Szemerédi N, Freitas-da-Silva J, Pinto E, Martins-da-Costa P, Pinto M, Correia-da-Silva M, Spengler G, Sousa E, Cidade H (2022) New chalcone-triazole hybrids with promising antimicrobial activity in multidrug resistance strains. Int J Mol Sci 23(22):14291. https://doi.org/10.3390/ijms232214291
Spitzer M, Robbins N, Wright GD (2017) Combinatorial strategies for combating invasive fungal infections. Virulence 8(2):169–185. https://doi.org/10.1080/21505594.2016.1196300
Spivak ES, Hanson KE (2018) Candida auris: an emerging fungal pathogen. J Clin Microbiol 56(2):e01588. https://doi.org/10.1128/JCM.01588-17
Sun A, Chai N, Zhu X, Li Y, Wang R, Zhang Y, Mao Z (2023) Optimization and antifungal activity of quinoline derivatives linked to chalcone moiety combined with FLC against Candida albicans. Eur J Med Chem 260:115782. https://doi.org/10.1016/j.ejmech.2023.115782
Sylla K, Tine RCK, Sow D, Lelo S, Dia M, Traoré S, Faye B, Dieng T (2019) Epidemiological and mycological aspects of onychomycosis in Dakar (Senegal). J Fungi 5(2):35. https://doi.org/10.3390/jof5020035. (Basel)
Thebti A, Meddeb A, Ben Salem I, Bakary C, Ayari S, Rezgui F, Essafi-Benkhadir K, Boudabous A, Ouzari H-I (2023) Antimicrobial activities and mode of flavonoid actions. Antibiotics 12(2):225. https://doi.org/10.3390/antibiotics12020225
Valipour M (2022) Recruitment of chalcone’s potential in drug discovery of anti-SARS-CoV-2 agents. Phytother Res 36(12):4477–4490. https://doi.org/10.1002/ptr.7651
Wang YH, Dong HH, Zhao F, Wang J, Yan F, Jiang YY, Jin YS (2016) The synthesis and synergistic antifungal effects of chalcones against drug resistant Candida albicans. Bioorg Med Chem Lett 26(13):3098–3102. https://doi.org/10.1016/j.bmcl.2016.05.013
Wangsanut T, Pongpom M (2022) The role of the glutathione system in stress adaptation, morphogenesis and virulence of pathogenic fungi. Int J Mol Sci 23(18):10645. https://doi.org/10.3390/ijms231810645
Yesudian R, Yesudian PD, Yesudian P (2021) Oral treatment of ringworm with griseofulvin. Clin Exp Dermatol 46(5):993–994. https://doi.org/10.1111/ced.14415
Zhan P, Liu W (2017) The changing face of dermatophytic infections worldwide. Mycopathologia 182:77–86. https://doi.org/10.1007/s11046-016-0082-8
González LA, Upegui YA, Rivas L, Echeverri F, Escobar G, Robledo SM, Quiñones W (2020) Effect of substituents in the A and B rings of chalcones on antiparasite activity. Arch Pharm (Weinheim) 353(12):2000157. https://doi.org/10.1002/ardp.202000157
Svetaz L, Agüero MB, Alvarez S, Luna L, Feresin G, Derita M, Tapia A, Zacchino S (2007) Antifungal activity of Zuccagnia punctata Cav.: evidence for the mechanism of action. Planta Med 73(10):1074–80. https://doi.org/10.1055/s-2007-981561
Rudrapal M, Khan J, Dukhyil AAB, Alarousy RMII, Attah EI, Sharma T, Khairnar SJ, Bendale AR (2021) Chalcone Scaffolds, Bioprecursors of Flavonoids: Chemistry, Bioactivities, and Pharmacokinetics. Molecules 26(23):7177. https://doi.org/10.3390/molecules26237177
Acknowledgements
Authors would like to thank the Laboratory of Microbiology of the São José do Rio Preto School of Medicine (FAMERP) and the Laboratory of Antibiotics and Chemotherapeutics of the São Paulo State University (Unesp), Institute of Biosciences, Humanities and Exact Sciences, São José do Rio Preto, Brazil.
Funding
This study was financed in part by the Coordenação de Aperfeiçoamento de Pessoal de Nível Superior – Brasil (CAPES) – Finance Code 001.
Author information
Authors and Affiliations
Contributions
TML and MTGA the study conception and design. PTC and LOR helped synthesize the compound. TML and BGA performed the literature search and data analysis. TML, THL and MDRM performed the material preparation and data collection. GRC and MRVZK carried out the toxicity test. TML and JPZS wrote the first draft of the manuscript. All authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval
Not applied, that no ethical approval is required.
Competing interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Maschio-Lima, T., Lemes, T.H., Marques, M.D.R. et al. Synergistic activity between conventional antifungals and chalcone-derived compound against dermatophyte fungi and Candida spp.. Int Microbiol (2024). https://doi.org/10.1007/s10123-024-00541-7
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1007/s10123-024-00541-7