Abstract
To evaluate the clinical efficacy of carbon dioxide laser in the treatment of female stress urinary incontinence and analyze the influencing factors. A total of 46 patients with stress urinary incontinence treated in the Affiliated Hospital of Nantong University from March 2021 to August 2022 were included through strict inclusion criteria and exclusion criteria. All patients were treated with transvaginal carbon dioxide laser therapy, and Patient Global Impression of Change (PGI-C) was used to evaluate patients’ subjective satisfaction after treatment. The efficacy was evaluated by patient’s subjective assessment of leakage, IngelmanSundberg scale, 1-h urine pad test, and international consultation on incontinence questionnaire short form (ICI-Q-SF) before and after treatment, and the adverse reactions after treatment were recorded. The treatment effect was divided into “significant effect group” and “no significant effect group” by subjective satisfaction and post-treatment-related scale evaluation. After laser treatment, patients’ subjective symptom improved, the volume of 1-h urine pad test was reduced, and the ICI-Q-SF score was decreased, and the differences were statistically significant (P < 0.05). There was no significant difference in IngelmanSundberg scale before and after treatment (P = 1.00). Multivariate logistic regression analysis showed that pad test volume was significantly correlated with treatment effect (P = 0.007). Transvaginal carbon dioxide laser is a safe and effective method for the treatment of mild to moderate stress urinary incontinence in females. The less severe the urinary leakage, the better the treatment effect.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Between 23 and 45% of the global female population over the age of 20 years have varying degrees of urinary incontinence, of which approximately 7% have significant clinical incontinence symptoms, and stress urinary incontinence (SUI) accounts for 50% of all incontinence rates [1, 2]. Regarding the treatment of SUI, according to NICE guidelines, although conservative treatment including pelvic floor muscle training, electrical stimulation, or biofeedback is preferred [3]; most patients fail to achieve satisfactory improvement due to low compliance. Surgical treatment has irreplaceable advantages in terms of its efficacy, but it has the risk of complications such as intraoperative bleeding, nerve injury, exposure to sling material, chronic pain, and voiding dysfunction [4, 5], which has led clinical investigators to explore new treatment modalities.
In recent years, vaginal carbon dioxide laser treatment for SUI has been hotly researched, and the author searched current studies at home and abroad, which are still in the stage of a small sample, single-center retrospective studies, and, although generally effective, the treatment results are uneven, and there is also a lack of research on the factors affecting the treatment outcome. In this study, we report the treatment effect of carbon dioxide laser treatment for SUI in our hospital and conduct a logistic analysis on the factors that may affect the efficacy.
Data and methods
Case data
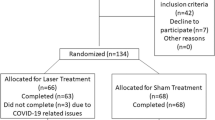
Patients who visited the pelvic floor outpatient of Nantong University Hospital from March 2021 to August 2022 for urinary leakage in the presence of increased abdominal pressure were collected. All patients had a detailed history, gynecological examination, urine routine, 3D pelvic floor ultrasound, 1-h urine pad test, and filled-out international consultation on incontinence questionnaire short form (ICI-Q-SF) score [6]. If the diagnosis of SUI was still unclear according to the above situation, urodynamic tests were performed to exclude other types of urinary incontinence. Finally, 46 patients with SUI were retrospectively selected according to the following inclusion criteria and exclusion criteria, and their age, relevant observations before and after treatment, and urethral rotation angle (URA) suggested by 3D ultrasound of the pelvic floor were recorded.
Inclusion criteria: (1) met the diagnostic criteria for SUI according to the 17-year Chinese Medical Association consensus [7]; (2) fully informed and informed consent to the treatment modality and voluntary choice of vaginal laser treatment.
Exclusion criteria: (1) urinary ultrasound suggestive of organic changes, or residual urine greater than 50 ml; (2) combined urinary tract infection; (3) combined pelvic organ prolapse of degree II or above; (4) after pelvic floor reconstruction surgery; (5) during pregnancy; (6) patients with intravaginal exposure of the tail filament of the birth control ring.
Participant mean age was 40.59 ± 10.83 years, mean body mass index was 23.73 ± 2.81, 26.09% was postmenopausal, 75% had a history of vaginal delivery.
Apparatus and surgical operation
The CO2 laser treatment machine was used, the laser mode was fractional mode, the energy density was selected as 80–110 mJ/px, and the power was selected as medium high, which was adjusted according to the age, and the elasticity of vaginal mucosa, folds, and secretions in combination with the assessment of vaginal health [8, 9]. The laser moves gradually from the proximal end of the vagina to the distal end. Every time the laser beam is emitted, the handpiece was rotated by the 45° to the next marking on the angular scale until the full circle was made. Then, the handpiece exits 1 cm outward until the entire length of the vagina is completed. When reaching the position of the vaginal opening, if the patient has obvious burning pain, the treatment parameter can be appropriately reduced to 60–80 mJ/px.
Course of treatment and precautions
A total of 2–3 treatments were given [10,11,12], each at an interval of 1 month, and if the patient did not show any improvement after 2 treatments, the third treatment was not continued. The efficacy of the treatment was evaluated afterward and followed up for any concomitant symptoms such as vaginal bleeding, abnormal discharge, painful intercourse, and discomfort in urination. Sexual intercourse and bathing were prohibited for 1 week after the operation. All operations were performed by the same doctor.
Observation indexes
Patients’ satisfaction after treatment
The Patient Global Impression of Change (PGI-C) [13] was used. There are seven options in the questionnaire, with a total score of 7. The response range is from 1 point, “significantly improved,” to 7 points, “significantly worse than before treatment.”
Patient’s subjective assessment of leakage
It was divided into none (no leakage), mild (very little leakage, a few drops), moderate (wetting underwear but not outer pants), and severe (wetting outer pants).
The IngelmanSundberg scale [14] was used
Mild: leakage when coughing or sneezing, no urine pad was needed;
Moderate: leakage when walking, running and jumping, and other daily activities, a urine pad was needed;
Severe: leakage when the light activity or changing position in lying position.
1-h urine pad test before and after treatment
This is an objective classification of SUI [7], which has been given in numerous papers and will not be repeated here.
ICI-Q-SF before and after treatment
ICI-Q-SF was used to evaluate the frequency of urinary incontinence and the impact degree of urine leakage on the quality of life of patients.
Assessment of efficacy
According to the comprehensive judgment of whether the symptoms improved; whether the number and quantity of urine leakage are reduced; whether the subjective score of clinical symptoms is downgraded; whether the volume of urine leakage by urine pad test decreased compared with that before treatment; and whether the ICI-Q-SF score decreased [11, 15, 16], it was classified as follows:
Cured: complete disappearance of clinical symptoms and negative urine pad test
Effective: significant improvement in subjective symptoms or significant reduction of leakage, which shows PGI-C ≤ 2 points [17]; subjective grade reduction in clinical symptoms; ≥ 50% reduction in leakage in 1-h urine pad test compared with that before treatment [6]; reduction in postoperative ICI-Q-SF score with a difference of ≥ 4 points.
Slightly effective: PGI-C ≥ 3 points; slight improvement in symptoms; no or barely degraded incontinence score.
Ineffective: no change in symptoms; no downgrading of incontinence scores.
Analysis of influencing factors
Cured and effective were classified as “significant effect group,” slightly effective and ineffective were classified as “no significant effect group,” and finally 30 patients with SUI were classified as “significant effect group,” and 16 patients with SUI were classified as “no significant effect group.” The treatment effect was used as the dependent variable, and the 1-h urine pad test leakage, age, and URA [18] were used as independent variables for multi-factor logistic regression analysis.
Statistical processing
SPSS 23.0 statistical software was used for data analysis, and the measurement data were expressed as (x ± s). First, check that the difference between the two groups before and after treatment has no obvious abnormal value, and the Shapiro-Wilk test was used to test whether the difference approximately obeyed a normal distribution, and the paired sample t-test was used to compare the differences between groups. Hierarchical data were examined for differences in composition ratio distributions using the chi-square test, and the Wilcoxon signed-rank test was used to see if there were differences in overall effects. The Box-Tidwell method was used to test for linearity between continuous independent variables and logit transformed values of the dependent variable, followed by dichotomous logistic regression analysis. p < 0.05 was considered a statistically significant difference.
Results
Analysis of efficacy before and after treatment
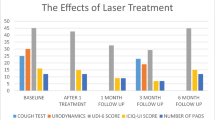
Urine pad test results
The mean level of the urine pad test was 8.34 ± 6.41 g before treatment and 6.63 ± 6.74 g after treatment, and the difference between before and after treatment was 1.72 ± 0.91 g, 95% CI of the difference: 1.45–1.98. The mean level of urine pad before treatment was higher than the mean level after treatment, and the difference was statistically significant (t = 12.812, P < 0.001), as shown in Table 1.
Results of ICI-Q-SF scores
The mean level of ICI-Q-SF scores of the study subjects was 9.63 ± 3.71 points before treatment and 6.33 ± 4.53 points after treatment, with a difference of 3.30 ± 3.21 points before and after treatment, 95% CI of the difference: 2.35–4.26. The degree of impact of urinary leakage on patients’ quality of life before treatment was higher than the mean level after treatment. The difference was statistically significant (t = 6.981, P < 0.001), as shown in Table 1.
The distribution of level of patient’s subjective assessment and IngelmanSundberg score before and after treatment is shown in Table 1. The statistical results of patient’s subjective assessment showed that Z = − 5.437, P < 0.001, indicating that the treatment was helpful to improve the patient’s subjective symptoms; however, IngelmanSundberg graduation results showed that Z = 0.00, P = 1.00, and the difference was not statistically significant.
Safety evaluation
Among all patients, 1 case that had sexual intercourse within 1 week after the operation was reported temporary symptoms of vaginitis, when inspected 10 days after surgery, and improved after drug treatment. The remaining patients had no special complications such as vaginal bleeding and painful intercourse, and none of them showed any aggravation of urinary incontinence.
Multi-factor logistic regression analysis
Of the three independent variables included in the model, the 1-h urine pad test volume change was statistically significant (OR = 0.385, P = 0.007). Its risk of treatment effectiveness decreased 0.615 times for each unit increase. The age and URA were not statistically different, as in Table 2.
Discussion
Mechanisms of SUI and principles of laser treatment
Three theories of SUI occurrence, including the pressure transmission theory, the “hammock” theory, and the holistic theory, have been extensively described in the previous literature and will not be repeated here. However, no matter what theory, it is believed that the weakness and defect of pelvic floor supporting structure are an important anatomical mechanism of SUI [19, 20]. When the support of the bladder neck and periurethral tissues is weakened, abdominal pressure increases; urethral resistance is insufficient to counteract intravesical pressure, and subluxation of the bladder neck and increased urethral mobility can be observed by three-dimensional ultrasound [21, 22]. Studies have shown an increase in the number of superficial and intermediate cells in the vaginal mucosa after laser treatment, with interstitial small-vessel proliferation and tissue cell hyperplasia after 6 weeks of treatment [23]. The laser rapidly promotes local elastic fiber and collagen proliferation, increasing local tissue thickness and elasticity [24], so in turn, it relatively increases the stability and reduces the mobility of the urethra [15, 24,25,26].
Current status of domestic and international studies and innovations of this study
In recent years, foreign scholars Dabaja H [27] and Lauterbach R et al. [28] have published studies on the use of lasers for SUI in females, and although the number of cases and follow-up time are small [29], they have initially suggested that vaginal laser treatment for SUI is safe and effective. The largest sample size was reported by Gonzalez et al. [23] in a prospective study of 161 postmenopausal patients with mild SUI, in which patients received four treatment sessions with intervals of 30–35 days and then additional maintenance sessions at 12, 24, and 36 months, with symptomatic improvement lasting for 36 months, suggesting definite efficacy in patients with mild urinary incontinence. James W Alexander et al. [30] conducted a participant-blinded, sham-controlled, randomized controlled trial in 2 hospitals,in which they compared the effects of CO2 vaginal laser vs. sham therapy for treating stress urinary incontinence. Results show that there was no difference between the groups in subjective or objective stress urinary incontinence. They concluded that CO2 vaginal laser therapy cannot show an improvement in stress urinary incontinence, which is different with other studies. The results of our study suggest that the vaginal CO2 laser was effective in improving urinary leakage in the treatment of mild to moderate SUI with no significant serious complications. The inconsistencies of current studies suggest that high-quality and large-sample studies are needed in the future.
In addition, this study found that some patients did not respond well to treatment. In this paper, through multi-factor logistic regression analysis, we found that the amount of leaked urine, which was valued by pad test (in grams), was a factor affecting the efficacy, i.e., the more severe the leakage, the less effective the treatment. It is suggested that laser treatment is only suitable for patients with mild and moderate urinary incontinence, and it is not effective for those with severe urinary leakage, which needs to be selected carefully in clinical practice.
This study found that age was not a factor affecting efficacy, suggesting that laser may be a good option for middle-aged and elderly females with SUI, especially since this group often cannot effectively cooperate with pelvic floor muscle training in the clinic or have difficulty in adhering to coming to the hospital for pelvic floor electromagnetic stimulation and biofeedback. Ivan Fistonic et al. [31] performed a prospective cohort study, which recruited 85 patients in 2016; they found that age is one of the independent significant predictors of Er:YAG laser treatment efficacy for SUI, which was also found in C. Tamer Ere et al. [32] research. The two studies mentioned above both suggest that younger women showed a better response, although Ogrinc et al. [33] could not show any relationship between patient age and success of the Er:YAG laser treatment, which is similar to what we found. In Ivan Fistonic et al. [31] research, they found that the critical age for Er:YAG laser effect is 47.5 years, but, in our study, the mean age was 40.59 ± 10.83 years; this may be the reason for the difference in our conclusions.
Our study suggests that the efficacy is not related to the URA. URA is the difference between the tilt Angle of urethra at rest and that of Valsalva. The tilt Angle of urethra is the angle between the central axis of the proximal urethra and the central axis of the human body. Normally, URA should be less than 45°, and its increase is one of the ultrasonic manifestations of SUI [34], as well as one of the important indicators of urethra activity and diagnosis of SUI [20]. Based on the above considerations, the author substituted it into the regression equation, and the final results suggested that it had little relationship with the therapeutic effect, which might be because there was inconsistency in the studies on whether URA itself was related to the severity of SUI [35, 36]. Subsequently, our research group could consider increasing the sample size to compare the changes in the relevant parameters of B-ultrasound before and after treatment in the next study, which may explain the mechanism of laser treatment for SUI.
There are some limitations in this study. The follow-up time is short, and its long-term curative effect is unknown. Whether it recurs, whether it needs intermittent consolidation in the follow-up, and whether it will cause local mucosal damage after multiple treatments still need long-term and large-scale research. In addition, to reduce bias, the author chose only three factors affecting the efficacy of the study under the premise of an extensive literature search, and it is still necessary to expand the sample and increase the potential risk factors in the future. These are also the parts that need to be further explored by our group in the future.
In conclusion, this study showed that transvaginal carbon dioxide laser treatment for mild and moderate SUI is safe and effective, the treatment effect is not affected by age, and there are few complications and significant improvement of patient’s symptoms in a short period, which provides a basis for laser treatment for patients with SUI and provides a relevant reference for clinical diagnosis and treatment of SUI.
References
Imamura M, Abrams P, Bain C et al (2010) Systematic review and economic modelling of the effectiveness and cost-effectiveness of non-surgical treatments for women with stress urinary incontinence. Health Technol Assess 14(40):1–188, iii–iv. https://doi.org/10.3310/hta14400
Committee U (2018) Conservative management of urinary incontinence. J Obstet Gynaecol Can 40(2):e119–e125
Okeahialam NA, Dworzynski K, Jacklin P et al (2022) Prevention and non-surgical management of pelvic floor dysfunction: summary of NICE guidance. BMJ 376
Palos CC, Maturana AP, Ghersel FR et al (2018) Prospective and randomized clinical trial comparing transobturator versus retropubic sling in terms of efficacy and safety. Int Urogynecol J 29(1):29–35
deTayrac R, Deffieux X, Droupy S et al (2004) A prospective randomized trial comparing tension-free vaginal tape and transobturator suburethral tape for surgical treatment of stress urinary incontinence. Am J Obstet Gynecol 190(3):602–608
Wein AJ (2005) ICIQ: a brief and robust measure for evaluating the symptoms and impact of urinary incontinence. J Urol 173(3):908–909
Gynecological Pelvic Floor Group of the Obstetrics and Gynecology Branch of the Chinese Medical Association. Guidelines for the diagnosis and treatment of female stress urinary incontinence (2017). Chinese J Obstet Gynecol, 52(05):289-293
Li FG, Maheux-Lacroix S, Deans R et al (2021) Effect of fractional carbon dioxide laser vs. sham treatment on symptom severity in women with postmenopausal vaginal symptoms: a randomized clinical trial. JAMA 326(14):1381–1389
Gao L, Wen W, Wang Y et al (2022) Fractional carbon dioxide laser improves vaginal laxity via remodeling of vaginal tissues in Asian women. J Clin Med 11(17):5201
Mothes AR, Runnebaum M, Runnebaum IB (2018) An innovative dual-phase protocol for pulsed ablative vaginal Erbium:YAG laser treatment of urogynecological symptoms. Eur J Obstet Gynecol Reprod Biol 229:167–171
Nalewczynska AA, Barwijuk M, Kolczewski P et al (2022) Pixel-CO2 laser for the treatment of stress urinary incontinence. Lasers Med Sci 37(2):1061–1067
Ruffolo AF, Casiraghi A, Marotta E et al (2021) Does the time of onset of urinary symptoms affect microablative fractional CO2 laser efficacy in postmenopausal women? Lasers Surg Med 53(7):953–959
Geisser ME, Clauw DJ, Strand V et al (2010) Contributions of change in clinical status parameters to Patient Global Impression of Change (PGIC) scores among persons with fibromyalgia treated with milnacipran. Pain 149(2):373–378
Schüssler B, Alloussi S (1983) Ingelman-Sundberg classification of stress incontinence. Gynakologische Rundschau 23(3):166
Palacios S, Ramirez M (2020) Efficacy of the use of fractional CO2RE intima laser treatment in stress and mixed urinary incontinence. Eur J Obstet Gynecol Reprod Biol 244:95–100
ElSheemy MS, Fathy H, Hussein HA et al (2015) Surgeon-tailored polypropylene mesh as a tension-free vaginal tape-obturator versus original TVT-O for the treatment of female stress urinary incontinence: a long-term comparative study. Int Urogynecol J 26(10):1533–1540
Abdel-Fattah M, Ramsay I, Pringle S et al (2011) Evaluation of transobturator tension-free vaginal tapes in management of women with recurrent stress urinary incontinence. Urology 77(5):1070–1075
Dietz HP, Hansell NK, Grace ME et al (2005) Bladder neck mobility is a heritable trait. BJOG 112(3):334–339
Ashton-Miller JA, Howard D, DeLancey JO (2001) The functional anatomy of the female pelvic floor and stress continence control system. Scand J Urol Nephrol Suppl 207:1–7
Turkoglu A, Coskun ADE, Arinkan SA et al (2022) The role of transperineal ultrasound in the evaluation of stress urinary incontinence cases. Int Braz J Urol 48(1):70–77
Chen HY, Huang YL, Hung YC et al (2006) Evaluation of stress urinary incontinence by computer-aided vector-based perineal ultrasound. Acta Obstet Gynecol Scand 85(10):1259–1264
Xiao T, Chen Y, Gan Y et al (2019) Can stress urinary incontinence be predicted by ultrasound? AJR Am J Roentgenol 213(5):1163–1169
González Isaza P, Jaguszewska K, Cardona JL et al (2018) Long-term effect of thermoablative fractional CO2 laser treatment as a novel approach to urinary incontinence management in women with genitourinary syndrome of menopause. Int Urogynecol J 29(2):211–215
Gaspar A, Brandi H, Gomez V et al (2017) Efficacy of Erbium:YAG laser treatment compared to topical estriol treatment for symptoms of genitourinary syndrome of menopause. Lasers Surg Med 49(2):160–168
Salvatore S, Leone Roberti Maggiore U et al (2015) Histological study on the effects of microablative fractional CO2 laser on atrophic vaginal tissue: an ex vivo study. Menopause 22(8):845–849
Zhang L, Lai Y, Pan W et al (2021) Application of ultra pulse CO2 lattice laser in the treatment of female urinary incontinence. Transl Androl Urol 10(6):2471–2477
Dabaja H, Lauterbach R, Matanes E, Gruenwald I, Lowenstein L (2020) The safety and efficacy of CO2 laser in the treatment of stress urinary incontinence. Int Urogynecol J 31(8):1691–1696
Lauterbach R, Aharoni S, Justman N et al (2022) The efficacy and safety of a single maintenance laser treatment for stress urinary incontinence: a double-blinded randomized controlled trial. Int Urogynecol J 23:1–6
Mortensen OE, Christensen SE, Løkkegaard E (2022) The evidence behind the use of LASER for genitourinary syndrome of menopause, vulvovaginal atrophy, urinary incontinence and lichen sclerosus: a state-of-the-art review. Acta Obstet Gynecol Scand 101(6):657–692
Alexander JW, Karjalainen P, Ow LL et al (2022) CO2 surgical laser for treatment of stress urinary incontinence in women: a randomized controlled trial. Am J Obstet Gynecol 227(3):473.e1–473.e12
Fistonić I, Fistonić N (2018) Baseline ICIQ-UI score, body mass index, age, average birth weight, and perineometry duration as promising predictors of the short-term efficacy of Er:YAG laser treatment in stress urinary incontinent women: a prospective cohort study. Lasers Surg Med
Erel CT, Inan D, Mut A (2020) Predictive factors for the efficacy of Er:YAG laser treatment of urinary incontinence. Maturitas 132:1–6
Ogrinc UB, Sencar S, Lenasi H (2015) Novel minimally invasive laser treatment of urinary incontinence in women. Laser Surg Med 47:689–697
Ying T, Li Q, Xu L et al (2012) Three-dimensional ultrasound appearance of pelvic floor in nulliparous women and pelvic organ prolapse women. Int J Med Sci 9(10):894–900
Al-Saadi WI (2016) Transperineal ultrasonography in stress urinary incontinence: the significance of urethral rotation angles. Arab J Urol 14(1):66–71
Sendag F, Vidinli H, Kazandi M et al (2003) Role of perineal sonography in the evaluation of patients with stress urinary incontinence. Aust N Z J Obstet Gynaecol 43(1):54–57
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics approval
Approved by Ethics Committee of Affiliated Hospital of Nantong University
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Wang, Y., Ye, Q. & Zhang, YQ. Effect evaluation and influencing factor analysis of vaginal carbon dioxide laser in the treatment of stress urinary incontinence. Lasers Med Sci 38, 153 (2023). https://doi.org/10.1007/s10103-023-03776-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s10103-023-03776-4