Abstract
The aim of this study was to evaluate the safety and efficacy of combined 1060-nm diode laser and 635-nm low-level laser therapy (LLLT) device for non-invasive reduction of the abdominal and submental fat. Forty-two healthy subjects received single laser treatment on both the abdomen and submental area. Ultrasound images measuring the thickness of abdominal and submental fat were taken at baseline, follow-up at 4, 8, and 12 weeks after treatment. Waist circumference and body weight were also measured at all visits. Adverse events were recorded at all visits. Subjects completed a satisfaction questionnaire at the end of the trial. Twelve weeks after a single treatment with the investigational device, ultrasound images showed statistically significant (P < 0.0001) reductions in abdominal and submental fat by 18.62 and 26.4%, respectively. In addition, significant (P < 0.0001) reduction in waist circumference was observed. Ninety-six percent of subjects rated that they were satisfied. Noted side effects were transient mild to moderate tenderness which subsided within 1 to 3 weeks. No serious treatment-related adverse events were reported. The dual wavelength device combining 1060-nm diode laser with 635-nm LLLT was safe and effective for non-invasive reduction of both abdominal and submental fat.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Currently available treatment options for excessive localized subcutaneous fat include liposuction, cryolipolysis, radiofrequency (RF), high intensity focused ultrasound (HIFU), and low-level laser therapy (LLLT). Liposuction effectively removes the excess subcutaneous fat from the target area but a high risk of post-operative pain, bleeding, infection makes it a less elegant treatment option for moderately obese persons. In contrast, non-invasive procedures including RF, HIFU, and LLLT deliver energy to the target area, causing either refirming of the fibrous tissue supporting the subcutaneous layer or inducing apoptosis of the adipocytes that constitute the excess subcutaneous fat. These have been previously demonstrated to effectively reduce localized body fat with minimal risk of side effects.
Localized fat destruction using the 1060-nm wavelength has been previously evaluated for its efficacy and safety [1]. This particular wavelength efficiently delivers laser energy to the subcutaneous adipose tissue with minimal affinity for other potential chromophores. Hyperthermic damage to the adipocytes, induced by laser therapy, causes disruption of the cell membrane leading to cell death, consequently resulting in reduced volume of adipose tissue in the treated area. LLLT is another modality for localized fat reduction and its efficacy has been previously evaluated by Caruso-Davis and colleagues [2]. Unlike other non-invasive options, fat reduction using LLLT does not involve catastrophic hyperthermic damage to adipocytes. Instead, it has been demonstrated that LLLT causes significant release of fat from adipocytes, resulting in volumetric reduction of the fatty tissue [3].
Under the background described above, we hypothesized that a novel medical laser beam scanner combining 1060-nm diode laser and 635-nm LLLT could demonstrate a synergistic effect in reducing localized subcutaneous fat. This prospective, multi-center clinical trial was designed to demonstrate the clinical efficacy and safety of this dual wavelength device in reducing subcutaneous fat in the abdominal and submental areas.
Patients and methods
This two-center study was approved by the Institutional Review Boards (Asan Medical Center, Seoul, Korea; Soon Chun Hyang University Hospital, Bucheon, Korea) and informed consent was obtained from all study subjects.
Study subjects
The inclusion criteria consisted of healthy volunteers aged over 19 years, with a body mass index (BMI) ≤ 30 kg/m2 and unwanted localized fat deposits in the abdomen and submental area measuring ≥2.5 cm and ≥1 cm, respectively, with a skinfold caliper. All study subjects agreed to neither take medication nor receive any kind of dermatologic or surgical procedures aiming at reducing body fat during the study period. Exclusion criteria included pregnant or breastfeeding status; photosensitivity or use of photosensitizing drug; uncontrolled chronic diseases; presence of malignancy and any condition which, in the opinion of the investigator, may represent significant risk to patient health, confound study results, or interfere with patient participation.
After standard health assessment and medical history, investigators determined the treatment areas at baseline. A horizontal line was drawn 2 cm below the center of the umbilicus and the exact areas to be treated were delineated with a surgical marker so that the applicators could be aligned horizontally with minimal space between each. Ultrasound images were serially taken on these predetermined locations.
Study device
The combined 1060-nm and 635-nm laser device used in this study employs 4 standard applicator heads and one small-sized applicator head. The standard applicator heads are joined to create a rectangular zone of radiation of approximately 112 cm2, or 28 cm2 per applicator. The small-sized applicator also creates a rectangular zone of radiation of approximately 5.8 cm2. The standard applicator emits a total energy of 0.9 to 1.4 W/cm2, of which the energy from 635-nm irradiation is fixed at 21.5 mW/cm2. The small-sized applicator emits 0.9 to 2.35 W/cm2, of which a fixed energy of 36.3 mW/cm2 is from 635-nm wavelength. Each applicator contains a water-cooled sapphire window that makes direct contact with the skin, keeping the skin surface cool throughout the treatment. Treatment time is set at 20–30 min for all patients.
Study protocol
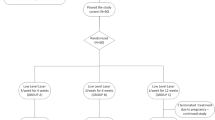
Subjects received a single treatment with the study device on both the abdomen and the submental area. Power density of the treatment was 0.9–1.4 W/cm2 and 0.9–2.35 W/cm2 for the abdomen and submental area, respectively. The treatment was set at maximal tolerable energy level. Treatment-related pain was recorded using a 10-point numerical rating scale (NRS). Adverse events were assessed at each treatment and follow-up visit. After treatment, aftercare instructions were given to the subject. Patients were instructed to maintain their current weight and not to change their diet or exercise routine. If a subject experienced any discomfort, the application of ice packs or taking acetaminophen was permitted, along with gentle massage.
Efficacy evaluation
Ultrasound imaging of the treated areas, body weight and abdominal circumference measurement were performed at 4, 8, and 12 weeks after treatment. The rate of subcutaneous fat reduction at 12 weeks after treatment compared with that of the baseline was set as the primary efficacy endpoint. The secondary efficacy endpoints included the following:
-
1)
Subcutaneous fat reduction rate at 4 and 8 weeks after treatment compared with baseline
-
2)
Amount of subcutaneous fat reduction at 4, 8, and 12 weeks after treatment compared with baseline
-
3)
Change in weight loss and abdominal circumference at 4, 8, and 12 weeks after treatment compared with baseline
-
4)
Subjects’ satisfaction assessed by General Aesthetic Improvement Score (GAIS) for each treatment area at 4, 8, and 12 weeks after treatment
Safety evaluation
All subjects completed the questionnaire addressing adverse events at each follow-up visit. Safety of the tested treatment was based on the incidence of treatment-related adverse events, subjects’ vital signs and laboratory tests. Blood samples were collected at baseline, 4 and 12 weeks after the treatment and were tested for the following complete blood cell counts, routine blood chemistry and lipids.
Statistical analysis
For the statistical evaluation of change in the subcutaneous fat thicknesses measured by ultrasonography, paired T-tests were performed to compare baseline values with 12 weeks post-treatment, and Wilcoxon signed rank tests were performed to compare baseline values with 4 and 8 weeks post-treatment. The choice of statistical technique was based on the results of Kolmogorov-Smirnov test for normality. Paired T-tests were used to evaluate differences in efficacy endpoints and treatment-associated pain between the abdomen and the submental area. Spearman’s rank-order correlation analysis was performed to determine correlation between the fat reduction rates of the abdomen and the submental area. All statistical analyses were performed using a statistical software package (SPSS, version 22.0; SPSS Inc., Chicago, IL, USA). Differences were considered statistically significant when P < 0.05.
Results
A total of 48 participants were enrolled. Among them, 44 participants completed the study protocol and were included in the analysis. Of the four participants who did not complete the study, three withdrew their consent during the study period and one participant was excluded due to change in body weight exceeding 5% of the initial weight. The characteristics of the study group are illustrated in Table 1. On blood sample analysis and physical examination, no subject had significant comorbidities. Review of medication revealed no concomitant use of both local and systemic drug that could interfere with this study.
Reduction of subcutaneous fat
Table 2 summarizes the reduction of subcutaneous fat after single treatment with the dual wavelength device. Mean subcutaneous fat reduction rate for the abdomen at 12 weeks after the treatment was 18.62 ± 12.23%, which was statistically significant (P < 0.0001, Fig. 1A). For the submental area, the mean subcutaneous fat reduction rate at 12 weeks after treatment was 26.40 ± 14.65%, which was also statistically significant (P < 0.0001, Fig. 2). These changes corresponded to a decrease in thickness by 5.91 ± 4.33 mm and 1.66 ± 1.35 mm for the abdominal fat and the submental fat, respectively. The reduction rates of abdominal fat at 4 and 8 weeks after treatment were 11.36 ± 8.45% and 16.31 ± 12.63 %, respectively. This corresponded to an absolute decrease of 3.60 ± 2.90 mm, 5.21 ± 4.34 mm in abdominal fat thickness at 4 and 8 weeks after the treatment, respectively. For the submental area, the mean reduction rate of subcutaneous fat at 4 and 8 weeks after treatment were 14.94 ± 12.14% and 22.61% ± 13.77%, respectively. This corresponded to an absolute decrease of 0.97 ± 1.17 mm, 1.43 ± 1.26 mm in submental fat thickness at 4 and 8 weeks post-treatment, respectively. For both areas, the rate as well as the amount of decrease in subcutaneous fat thickness were statistically significant at all tested time points (4, 8, and 12 weeks post-treatment) compared to baseline (P < 0.0001). Also, the decrease in subcutaneous fat thickness between consecutive time points (4 weeks vs. 8 weeks and 8 weeks vs. 12 weeks) was statistically significant for both treated areas. (P < 0.01) Fig. 3 illustrates the morphological changes in the submental and abdominal areas before and after the treatment in a representative case. The ultrasound images demonstrated a notable decrease in the abdominal fat thickness at week 12. We observed a positive correlation between the reduction rate of the abdominal fat and that of the submental fat at 12 weeks post-treatment on Spearman’s rank-order correlation analysis (P < 0.01).
Representative case showing both abdominal and submental fat reductions after treatment with the dual wavelength device. Twelve weeks after the treatment, this 56-year-old female participant showed 14.7 and 22% decrease in fat thickness of the abdomen and submental area, respectively, from baseline. Decrease in the abdominal fat thickness is seen in the ultrasound images
Changes in waist circumference and body weight
The changes in waist circumference and body weight 4, 8, and 12 weeks after the treatment compared to baseline are presented in Tables 3 and 4, respectively. While there was no significant difference in mean body weight of subjects after the treatment compared with baseline, the treatment with the dual wavelength device resulted in a significant reduction in waist circumference starting from 4 weeks post-treatment and lasting until the last follow-up visit at 12 weeks post-treatment. (P < 0.0001, Fig. 1B and C)
Subject satisfaction
Subject satisfaction was assessed according to the 5-point GAIS reported by the participants for each treatment area at 4, 8, and 12 weeks after treatment. (0: much worse, 1: worse, 2: no change, 3: improved, 4: much improved). The mean GAIS for the abdomen at 4, 8, and 12 weeks after treatment were 2.23 ± 0.42, 2.45 ± 0.66, and 2.48 ± 0.66 points, respectively. For the submental area, the mean scores at 4, 8, and 12 weeks after treatment were 2.32 ± 0.52, 2.61 ± 0.72, and 2.59 ± 0.73 points, respectively. Although the reported scores varied from 1 to 4 points, no subject gave a satisfaction score of 0 point (Fig. 4).
Treatment-related discomfort
The mean NRS pain score during the treatment was 5.23 ± 2.81 for the abdomen and 3.25 ± 3.13 for the submental area. After classifying NRS scores by severity (no pain: 0, mild: 1 to 3, moderate: 4 to 6, severe: 7 to 10), there were 19 (43.2%) subjects who reported severe pain, 11 (25%) subjects who reported moderate pain, and 10 (22.7%) subjects who reported mild pain. Four (9.1%) subjects reported no treatment-related pain. For the submental area, 10 (22.7%) subjects reported severe pain, 8 (18.2%) reported moderate pain, 13 (29.5%) subjects reported mild pain, and 13 (29.5%) subjects reported no pain during treatment.
Adverse reactions
A total of 15 (34.1%) subjects experienced at least one adverse event, and 6 (13.6%) of them experienced a total of 8 adverse events related to the medical device. Six (13.6%) cases of application site pain and 2 (4.5%) cases of subcutaneous nodules on application were found. None of these lasted to the last visit. There were no subjects who experienced serious anomalies or adverse events that resulted in subject drop-out.
Discussion
A number of body sculpting devices based on low-level laser therapy (LLLT) and laser therapy have been manufactured and tested for their clinical efficacy and safety [1, 2, 4]. Although the degree of subcutaneous fat reduction varied from one device to another, most LLLT and laser devices demonstrated moderate success with good safety profile. Other modalities, including cryolipolysis, high-intensity focused ultrasound, radiofrequency and whole body vibration, also demonstrate efficacy in reducing subcutaneous fat [5,6,7]. Interestingly, there have been reports on the synergistic fat-reducing effect obtained by combining these modalities [8, 9]. In light of these previous reports, the possibility of combining laser treatment and LLLT to maximize subcutaneous fat-reducing efficacy has been postulated. The dual wavelength device investigated in this study combines 1060-nm diode laser with LLLT to reduce localized subcutaneous fat.
The primary efficacy endpoint of this clinical trial was the rate of subcutaneous fat reduction rate at each treated area at 12 weeks after the treatment compared with baseline, determined by serial measurements of subcutaneous fat thickness with ultrasonography. The results indicate a significant reduction of subcutaneous fat thickness after the treatment for both the abdomen and the submental area. The submental area showed a greater reduction compared to the abdomen (P < 0.001). This could be the result of higher treatment energy level of the submental area as the smaller applicator could reach a higher energy output. Also, because the subcutaneous fat thickness of the submental area is relatively thin, it is possible that a higher proportion of subcutaneous fat was exposed to sufficient laser and light energy compared to the abdominal area. Previous study evaluating the efficacy of cryolipolysis for submental fat reduction reported an average absolute decrease in submental fat thickness of 2 mm at 12-week post-treatment [10]. Although the modality chosen to treat submental fat differs from ours, the dual wavelength device demonstrated superior submental fat reduction by more than twofold.
The rate of fat reduction at 4 and 8 weeks after the treatment compared to baseline was evaluated as a secondary efficacy endpoint. A significant decrease in subcutaneous fat thickness was observed at 4 weeks after the treatment and onwards. This suggests that the inflammatory process leading to apoptosis of adipocytes occurs within the first 4 weeks. Compared to a previous study using the 1060-nm diode laser treatment that reported significant change in subcutaneous fat thickness at 6 weeks after treatment, earlier onset of significant fat reduction was observed in this study [1]. Further decrease in fat thickness was seen at 8 and 12 weeks after the treatment, indicating that the inflammation in subcutaneous adipose tissue lasts longer than 4 weeks after treatment.
In this study, we observed a positive correlation between the rates of fat thickness reduction on the abdomen and the submental area (P = 0.0002), suggesting that certain subjects respond better to the dual wavelength treatment. However, we could not identify demographic factors that are associated with higher fat reduction. In this regard, future studies to assess clinical factors that affect the efficacy of this device seem necessary.
Other secondary endpoints included the absolute change in subcutaneous fat thickness, changes in body weight and abdominal circumference. The onset as well as the general trend of absolute reduction of subcutaneous fat was comparable to that of the fat reduction rate. Body weight showed no significant change in all subjects during the entire study period. This suggests that treatment with the dual wavelength device is intended to reduce localized subcutaneous fat, rather than to promote weight loss, making it a ‘body-contouring therapy’. But this observation could have resulted from the participants’ effort to maintain their initial body weight as informed at the time of enrollment and the exclusion of one subject whose body weight increased by more than 5% of the initial weight during study period in order to rule out the effect of body weight change on the subcutaneous fat thickness. Dual wavelength treatment on the abdomen resulted in a reduction in abdominal circumference, which was noted at 4 weeks post-treatment and lasted through the entire study period.
The participants reported a moderate satisfaction score of 2.48 and 2.59 on a scale from 0 to 4 for the abdomen and submental area, respectively. Although this difference was not found statistically significant (P = 0.23), slightly higher satisfaction for the submental area may be correlated to the more pronounced fat reduction in the submental area than in the abdomen. The satisfaction score was initially expected to be higher, but only a small number of participants gave a score of 3 or 4. This discrepancy could be attributed to the high expectation of participants, which is often unrealistic as observed in any aesthetic procedure. In addition, treatment-related discomfort could have negatively affected the overall satisfaction since most subjects reported localized pain of a certain degree during the treatment. Nonetheless, when compared with other similar studies, the fact that only one (2.3%) subject reported to be unsatisfied with a score of 1 for both areas suggest positive rating by the subjects in general [11, 12].
The degree of discomfort was higher on the abdomen compared with the submental area (P = 0.001). Moderate to severe treatment-related pain was anticipated as the treatment energy was set at the highest tolerable level. Pain on the treated area is considered to reflect the amount of heat energy delivered to the target tissue, thus the degree of adipocyte injury. However, while the subjects reported more severe pain on the abdomen, the rate of fat reduction was more prominent on the submental area. Therefore, the intensity of pain and degree of fat reduction do not seem to be directly correlated.
In this study, about one-seventh of the subjects experienced treatment-related adverse reactions, where the most frequently reported adverse reaction was localized pain on the treated areas. Also, formation of tender subcutaneous nodules was observed in two subjects. Considering that the incidence of pain and nodules on the treatment area was reported to be 56.6 [13] and 12% [1] in previous related studies, the dual wavelength modality portends a lower risk of such adverse events.
Certain limitations need to be addressed regarding this study. First, owing to the nature of this study, strict control of both dietary habit and physical activity was not possible. Nevertheless, we tried to minimize the effect of weight loss on the subcutaneous fat thickness by regularly checking subjects’ body weight and dropping out one subject whose body weight increased by more than 5% of baseline. Second, the ultrasound measurement of the subcutaneous fat thickness is subject to measurement error and potential bias. Although measurements were performed by one trained physician in each study center in order to minimize inter-observer variation, a double-blinded study seems necessary to overcome potential bias. Finally, the fact that 88.6% of the study subjects were Asians, with only five (11.4%) Caucasians, makes it difficult for this study’s results to be generalized to other races. However, it has been previously demonstrated that skin of color is more vulnerable to adverse effects such as pigmentary changes caused by laser treatments [14, 15]. Considering that more than 70% of the subjects were of Fitzpatrick skin type III/IV and that no serious treatment-related adverse effects were observed, treatment with the dual wavelength device is expected to be safe in fair skin.
Conclusion
The results of this study suggest that a single treatment with the novel dual wavelength device combining 1060-nm diode laser with 635-nm LLLT can be a safe and effective modality for the reduction of localized subcutaneous fat on the abdomen and submental area.
References
Katz B, Doherty S (2018) Safety and efficacy of a noninvasive 1,060-nm diode laser for fat reduction of the flanks. Dermatol Surg 44:388–396. https://doi.org/10.1097/DSS.0000000000001298
Caruso-Davis MK, Guillot TS, Podichetty VK et al (2011) Efficacy of low-level laser therapy for body contouring and spot fat reduction. Obes Surg 21:722–729. https://doi.org/10.1007/s11695-010-0126-y
Neira R, Arroyave J, Ramirez H et al (2002) Fat liquefaction: effect of low-level laser energy on adipose tissue. Plast Reconstr Surg 110:912–922; discussion 923-915. https://doi.org/10.1097/00006534-200209010-00030
Decorato JW, Chen B, Sierra R (2017) Subcutaneous adipose tissue response to a non-invasive hyperthermic treatment using a 1,060 nm laser. Lasers Surg Med 49:480–489. https://doi.org/10.1002/lsm.22625
Choi SY, Kim YJ, Kim SY et al (2018) Improvement in abdominal and flank contouring by a novel adipocyte-selective non-contact radiofrequency device. Lasers Surg Med 50:738–744. https://doi.org/10.1002/lsm.22808
Ingargiola MJ, Motakef S, Chung MT, Vasconez HC, Sasaki GH (2015) Cryolipolysis for fat reduction and body contouring: safety and efficacy of current treatment paradigms. Plast Reconstr Surg 135:1581–1590. https://doi.org/10.1097/PRS.0000000000001236
Coleman WP 3rd, Coleman W, Weiss RA, Kenkel JM, Ad-El DD, Amir R (2017) A multicenter controlled study to evaluate multiple treatments with nonthermal focused ultrasound for noninvasive fat reduction. Dermatol Surg 43:50–57. https://doi.org/10.1097/DSS.0000000000000918
Ferraro GA, De Francesco F, Cataldo C, Rossano F, Nicoletti G, D'Andrea F (2012) Synergistic effects of cryolipolysis and shock waves for noninvasive body contouring. Aesthet Plast Surg 36:666–679. https://doi.org/10.1007/s00266-011-9832-7
Savoia A, Landi S, Vannini F, Baldi A (2013) Low-level laser therapy and vibration therapy for the treatment of localized adiposity and fibrous cellulite. Dermatol Ther (Heidelb) 3:41–52. https://doi.org/10.1007/s13555-013-0026-x
Kilmer SL, Burns AJ, Zelickson BD (2016) Safety and efficacy of cryolipolysis for non-invasive reduction of submental fat. Lasers Surg Med 48:3–13. https://doi.org/10.1002/lsm.22440
Shek SY, Yeung CK, Chan JC, Chan HH (2016) The efficacy of a combination non-thermal focused ultrasound and radiofrequency device for noninvasive body contouring in Asians. Lasers Surg Med 48:203–207. https://doi.org/10.1002/lsm.22406
Shek SY, Yeung CK, Chan JC, Chan HH (2014) Efficacy of high-intensity focused ultrasonography for noninvasive body sculpting in Chinese patients. Lasers Surg Med 46:263–269. https://doi.org/10.1002/lsm.22232
Kennedy J, Verne S, Griffith R, Falto-Aizpurua L, Nouri K (2015) Non-invasive subcutaneous fat reduction: a review. J Eur Acad Dermatol Venereol 29:1679–1688. https://doi.org/10.1111/jdv.12994
Kang HJ, Na JI, Lee JH, Roh MR, Ko JY, Chang SE (2017) Postinflammatory hyperpigmentation associated with treatment of solar lentigines using a Q-Switched 532-nm Nd: YAG laser: a multicenter survey. J Dermatol Treat 28:447–451. https://doi.org/10.1080/09546634.2016.1254330
Eimpunth S, Wanitphadeedecha R, Manuskiatti W (2013) A focused review on acne-induced and aesthetic procedure-related postinflammatory hyperpigmentation in Asians. J Eur Acad Dermatol Venereol 27(Suppl 1):7–18. https://doi.org/10.1111/jdv.12050
Acknowledgements
This research was partially supported by the Ministry of Health and Welfare of Korea (grant number: HR20C0026) and the Soonchunhyang University Research Fund (grant number: 20200040).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Moon, I.J., Choi, J.W., Jung, C.J. et al. Efficacy and safety of a novel combined 1060-nm and 635-nm laser device for non-invasive reduction of abdominal and submental fat. Lasers Med Sci 37, 505–512 (2022). https://doi.org/10.1007/s10103-021-03288-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10103-021-03288-z